Introduction
The scope of physiotherapy practice in rural and remote areas is changing. Rural and remote physiotherapists are commonly regarded as ‘specialist generalist’ practitioners with clinical skills enabling them to work across a wide variety of conditions and across the lifespan1. In addition, rural and remote practice may include population health and primary healthcare approaches such as health promotion and community development1,2. Allied health rural generalists can now undertake tertiary-level training tailored to their practice context and there have been calls within the physiotherapy profession for recognition of this high-level expertise through advanced practice standing2. There is also increasing recognition of the potential for better utilisation of the rural and remote allied health workforce through extended scope roles3. Extended scope of practice involves an advanced clinical specialist undertaking further training in tasks usually undertaken by doctors, nurses or other health professionals. Extended scope, advanced practice and full scope of practice are recognised elements of expanded scope of practice3. There are few published examples of the implementation of extended-scope physiotherapy roles outside metropolitan areas4.
There is strong evidence that expanded-scope physiotherapy roles in the emergency department (ED) can improve service performance. These roles have been shown to reduce length of stay and waiting time compared with usual care by a physiotherapist5 and medical staff6, reduce treatment time5, have higher levels of patient5,7 and staff satisfaction7 and result in a positive patient experience8 without any adverse effects5,9. The percentage of people who present to the ED with conditions classified as semi-urgent (Category 4) or non-urgent (Category 5) according to the Australasian Triage Scale10 is higher outside major cities11. Assuming that these semi-urgent and non-urgent presentations will include musculoskeletal conditions that can be safely and effectively managed by an expanded-scope physiotherapist, these roles may have benefits for regional hospital EDs.
Rural and regional sites present particular challenges in implementing new workforce models. Lack of a career pathway to advanced roles, limited access to professional development and postgraduate education, and the time and cost of attending training courses can make it difficult to attract and retain qualified physiotherapists12. Documenting the implementation of expanded-scope physiotherapy models of care in a regional hospital ED can be beneficial in gaining a better understanding of the challenges and potential benefits for implementation of these new roles outside of major cities. The current project is one of eight expanded-scope-of-practice physiotherapy projects funded by Health Workforce Australia (HWA), a former Commonwealth statutory authority, to enable local implementation and evaluation of expanded-scope physiotherapy models in several sites across Australia13. The national evaluation of all of the funded projects has been published elsewhere14.
The aim of this article is to describe the redesign of a physiotherapy service in a regional hospital ED from a week-day service provided by an existing advanced physiotherapist role to an extended-hours, 7 day expanded-scope service provided by an advanced and a senior physiotherapist and to discuss the lessons learnt for sustainable expanded-scope physiotherapy practice in regional hospitals.
Methods
Setting
The study site is a 571-bed regional hospital that provides 24-h emergency care for people living in the surrounding areas. The nearest equivalent-level public hospital ED is 344 km away.
Service redesign
In the existing ED model of care, patients presenting with musculoskeletal conditions were referred by medical or nursing staff to an advanced physiotherapist. X-rays were ordered and reviewed by medical officers. Fractures were managed in conjunction with a medical officer and all cases were reviewed by a medical officer prior to discharge. The service redesign involved: (1) the advanced physiotherapist undertaking a postgraduate diploma and on-the-job training in extended scope skills; and (2) a senior physiotherapist role. A professional development package was developed locally to facilitate the senior physiotherapist progressing to an advanced level. The package included a log book in which the physiotherapist recorded knowledge gained and skills demonstrated in advanced musculoskeletal management as assessed by members of the ED multidisciplinary team. The service was increased from 5 to 7 days and hours extended from 7 (0800–1600 hours) to 10 (0800–1800 hours). The purpose of the senior physiotherapist role and the professional development package was to achieve an extended-hours roster and create a pathway for the senior physiotherapist to advance their skills and experience so that they would be eligible for advanced and extended scope roles in the future. These measures would all help address recruitment and retention issues experienced in regional areas.
Service evaluation
Design: The study was a descriptive observational design using mixed method data collection techniques. Data mining of ED administrative and clinical data sets included the number of primary and secondary contacts per shift, mean waiting time to be seen, proportion of patients discharged home within 4 h and mean length of stay in ED. Patient and staff satisfaction surveys were also conducted. An ‘issues log’ of challenges and how they were addressed derived from discussions at project implementation and steering committee meetings was maintained by the project officer.
Procedure: The patient satisfaction survey was based on a validated questionnaire14 adapted by the national evaluation team13 and answered on a Likert scale from 1 (strongly agree) to 5 (strongly disagree). The advanced physiotherapist informed patients of the study at the conclusion of treatment and gave them information sheets. Patients who agreed to participate in the study either placed completed surveys in a locked box in the ED or returned them via a prepaid envelope.
The staff survey was developed by the national evaluation team13 and answered on a Likert scale from 1 (strongly agree) to 5 (strongly disagree). There was one open question for additional comments. Staff satisfaction surveys were completed online.
Survey data were analysed using descriptive statistics for quantitative data and content analysis of qualitative data. Adverse event and complaint reporting were monitored through normal procedures. Clinical activity data were extracted from the ED clinical data set and transferred to an Excel spreadsheet for analysis.
Ethics approval
Ethics approval for this study was obtained from the Far North Queensland Human Research Ethics Committee (HREC/12/QCH/94-813).
Results
Service redesign description
The 7-day, extended-hours roster commenced with the advanced and senior physiotherapist working an ‘overlap’ day to enable training and supervision of the senior physiotherapist and for project administration. A senior ED medical consultant provided clinical oversight for the advanced physiotherapist. The advanced physiotherapist had many years of experience and was able to work to their full scope of practice. The changes to clinical practice achieved by the advanced physiotherapist included credentialing to independently order and interpret plain film X-rays, autonomous discharge decision-making, independent management of patients with simple closed manipulation and plastering and direct referral to orthopaedic and fracture clinics.
The advanced physiotherapist recorded a total of 517 primary contacts with ED triage Category 3, 4 or 5 patients with musculoskeletal injuries. An average of eight patients per day were seen on weekdays, compared with 10 patients per day on weekends.
Education and training
The advanced physiotherapist completed a 12-month postgraduate Diploma of Extended Scope Physiotherapy, which involved four separate week-long residential blocks in Canberra. External grant funding was sought and obtained to cover course costs and travel. The senior physiotherapist commenced the locally developed professional development package. There were a number of challenges associated with this component of the redesign. Due to clinical workload and off-site study leave, there was limited time for the advanced physiotherapist to supervise the senior physiotherapist. There were limited inter-professional networks in ED to support the senior physiotherapist in the absence of the advanced physiotherapist. Due to resource constraints, the professional development package was not available until 10 weeks after commencement of the role. To address these challenges, rosters were changed so that the advanced and senior physiotherapist rosters overlapped for two half-days, supervision was provided on seeking referrals and screening patients and joint working and education sessions with nurse practitioners and medical staff were organised to increase awareness of the senior physiotherapist role and facilitate working with other ED staff. The senior physiotherapist resigned before the professional development package was completed and was replaced by a base-grade physiotherapist after an unsuccessful recruitment campaign.
Service evaluation
For the advanced physiotherapist, the average proportion of patients discharged within 4 h (the National Emergency Access Target (NEAT) introduced into Australian hospitals in 2012) was 97.44% compared with an average ED discharge rate of 73.76% (Table 1). Wait time to be seen by the advanced physiotherapist decreased from 39 to 19 min (Table 2). Treatment time (time left waiting area to time left ED) remained stable, with a decrease of 6 min over the project (Table 2). No adverse events or patient complaints were recorded.
Survey responses (30% of total ED staff) showed a high level of staff satisfaction with the expanded-scope role. Staff reported an improved quality of care for musculoskeletal conditions (82% strongly agree) and the ED team was more effective (80% strongly agree). Staff commented on the improved quality of care for patients ('Hugely beneficial to patients') and the contribution to the multidisciplinary team ('the ED primary contact physio is a huge asset to this ED. Physios have a much better understanding of musculoskeletal injury'). The main concern expressed was the impact on junior doctors ('My only concern … is that our junior medical officers may not get as much exposure to this group of presentations').
Of the 104 patient satisfaction surveys that were distributed, 99 were completed. For the expanded-scope role, patients reported that the physiotherapist seemed comfortable dealing with their problem (94%), understood what was wrong with them (86%) and told them what to do to prevent further problems (72%). They also reported that the treatment prescribed was effective (76%), and the physiotherapist made them feel less worried about their problem (82%).
Table 1: Number and percentage of Category 3–5 patients seen by the advanced physiotherapist in a primary contact capacity who were discharged within 4 h compared with all-hospital emergency department (ED)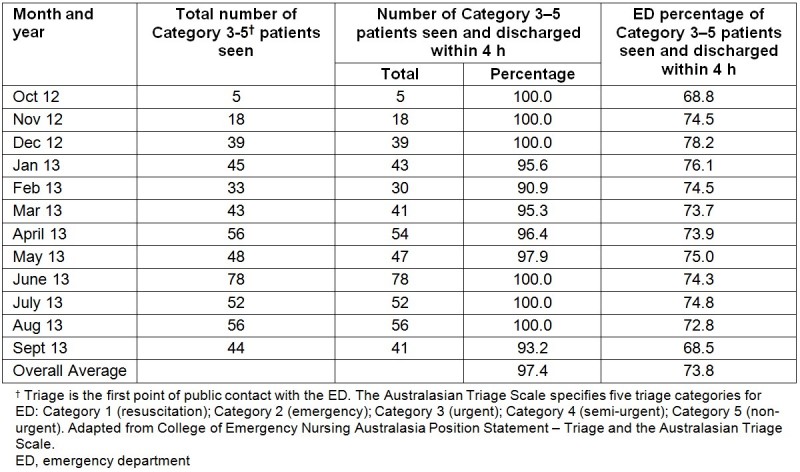
Table 2: Wait time and treatment time for primary contact patients seen by the advanced physiotherapist
Discussion
This study describes the redesign of an existing experienced physiotherapy role to an expanded scope of physiotherapy service. Findings demonstrate that it is feasible to implement a safe and efficient extended-hours physiotherapy service and staff training in expanded-scope practice in a regional hospital. There were high levels of staff and staff satisfaction with the role and no adverse events were recorded during the study period.
The service redesign contributed to efficiency and effectiveness with a consistent rate of discharge within 4 h of 97.4%, well above the hospital’s ED average for Category 3, 4 and 5 (73.8%) and the overall 2013 hospital NEAT target for all categories (77%). This result addresses one of the perceived barriers to introducing expanded-scope physiotherapy roles in EDs, which is that they tend to provide a more in-depth service that is less cost-effective7. This result also improved on the 4 h discharge rate of 91% reported in a study of a primary contact physiotherapy role in a metropolitan hospital6. Wait time to be seen by the advanced physiotherapist decreased by 20 min over the course of the study. Studies in metropolitan areas have shown that wait times to be seen by primary contact physiotherapists are shorter than for doctors6. Time taken to treat remained fairly constant throughout this study. A comparison of wait times and time to treat for the advanced physiotherapist and doctors in regional areas is warranted because both of these factors may influence patient satisfaction in the ED5,7
Patient and staff satisfaction surveys showed strong support for the expanded-scope physiotherapy role. Staff was supportive of the contribution to the multidisciplinary team and valued the knowledge and expertise of the expanded-scope physiotherapist. This is consistent with a previous study that found high levels of ED staff satisfaction with the role on the basis of their knowledge and skills5. Patient experience is an emerging area of expanded scope of physiotherapy research. The results of this study support those of Harding et al.8 who found that in both metropolitan and remote areas, patients valued the confidence, skills and attributes of the expanded scope physiotherapist, making them a suitable alternative to a doctor for treatment of musculoskeletal conditions. Further investigation of patient experience in regional hospitals is warranted.
The challenge of recruitment and retention of experienced physiotherapists was addressed in this study by training a senior physiotherapist in advanced ED skills in addition to up-skilling the advanced physiotherapist in extended scope of practice. No other study has addressed this issue as part of an expanded scope of practice model of care. Comparable studies in a remote location8 and major regional city6 were staffed by multiple physiotherapists in the expanded scope role. Alternating staff across a 14-day period with one day per week of overlap was an effective method for providing a 7 day service with only two staff members in the short term but long-term viability is limited. The resignation of the senior physiotherapist meant that the training package for the senior physiotherapist was not completed. Time away from service delivery by the advanced physiotherapist to complete a postgraduate qualification and a delay in availability of the package were additional constraints on completion of the professional development package by the senior physiotherapist. The findings support work reported by Harding et al15 to develop a standardised clinical education framework and pathway for physiotherapists undertaking advanced musculoskeletal physiotherapy roles. The findings of the present study support the conclusion that a preferred model for education should be affordable, require minimal time off work and be based in the workplace so that it is tailored to meet the needs of the local population15.
Conclusions
The findings of this descriptive observational study indicate that expanded scope of physiotherapy roles have the potential to improve performance of regional hospital emergency departments. A limitation of the study is that other factors not studied may have influenced the overall ED performance and that of the advanced physiotherapist in achieving time targets. No comparisons were made with similar patients managed by medical staff. Nonetheless, the findings are consistent with a growing body of research that supports the contribution of expanded-scope physiotherapy practice in providing safe, acceptable, timely and high quality care in ED. However, greater availability of physiotherapists with advanced skills, more advanced practice roles, affordable training programs with flexible delivery options and adequate resourcing for on-the-job training are required to support these roles in regional hospital EDs. As these roles develop to include additional expanded-scope tasks, including independent prescribing and injecting for the purpose of joint aspiration and administration of local anaesthesia, further evaluation is warranted.
Acknowledgements
This project was possible due to funding made available by Health Workforce Australia as an Australian Government Initiative. The postgraduate course completed by the Extended Scope of Practice Physiotherapist was funded by a Services for Rural and Remote Allied Health Nursing and Allied Health Scholarship and Support Scheme post graduate scholarship. The authors acknowledge the physiotherapists who performed the advanced and senior ED physiotherapy roles.
Portions of this article were presented at the Services for Rural and Remote Allied Health National Conference, 17–24 September, 2014, Kingscliff, New South Wales.
