Introduction
A global diabetes epidemic is underway1. The main contributor to the epidemic is an increasing prevalence of type 2 diabetes, due to an increasing incidence2 associated with the disease burden of 'overweight and obesity'3, an increase in age-specific prevalence rates4, an aging population in whom there is a higher age-specific prevalence rate of type 2 diabetes5, and increased survival for both type 1 and type 2 diabetes6.
Highland Region, in the north of Scotland, is an area of 26 500 km2 covering one-third of the total Scottish landmass. The region is sparsely populated with 208 000 people, only 4.1% of the Scottish population, with a proportion of elderly that is growing more quickly than the Scottish population as a whole. Due to the higher age-specific prevalence rate of type 2 diabetes in older age groups, aging populations alone will inevitably lead to an increase in the prevalence of diabetes7.
The Scottish Indices of Multiple Deprivation indicates that there are pockets of marked deprivation within Highland but, in terms of access to services, 40% of electoral wards in Highland region are ranked in the lowest 10% for Scotland. The delivery of health-care services in rural areas is affected by geographical distances and inadequate transportation; people with diabetes are known to be responsible for 6.4% of all out-patient attendances8.
The number of people with diabetes in Highland in 2003 was 6042, a prevalence rate of 2.8% of the whole population, or 3.3% of those aged over 15 years; of these 128 were children, one of whom has type 2 diabetes9. The region was served by one consultant diabetologist for adults and a paediatrician who specialises in diabetes based in a regional diabetes centre in the Highland capital Inverness.
The increasing prevalence of type 2 diabetes, accentuated by rural demographic changes and the difficulties of access to services in remote areas, contributed to unacceptable waiting times of over 90 weeks for some people with type 2 diabetes9. At the time of these local pressures, three major national guidance documents were published: the Scottish Diabetes Framework for service development, new Scottish Intercollegiate clinical management guidelines and revised clinical standards. The complexities of the local implementation of these central policies were magnified by the effects of rurality in terms of geography, access to health-care services, a need greater in people with diabetes, and the aging of rural populations, leading to an inevitable increase in the prevalence of diabetes. Such policies are known not to necessarily translate well to rural policy10.
The public health department in NHS Highland, the regional health authority, was asked to undertake a review of diabetes services by engaging health-care professionals and people with diabetes and their carers, including those from the remote and rural areas. The aim of the review was to describe the current service provision identifying areas for improvement, develop solutions and make recommendations for change and to design a new service configuration to meet the needs of people with diabetes in the region.
Methods
The key to the success of this initiative was the inclusive involvement of everyone with an interest in the care of people with diabetes, representative of all disciplines, professions, geographical locations and patients and carers. To consolidate this approach as the underlying philosophy, the redesign methodology, as advocated by the Scottish Executive, was adopted11 and is outlined below.
A preliminary workshop with the regional diabetes service group, consisting of primary and secondary medical, nursing and managerial health care professionals and patient representatives identified all stakeholders. To ensure inclusion and ownership, workshops were organised throughout the region. These included remote areas, as well as the diabetes outpatient service, the retinopathy screening service and two workshops in a Diabetes UK awareness event for patients and carers.
Teams of facilitators undertook the workshops and over 160 health-care professionals with an interest in the care of people with diabetes, including GPs, consultants, nurses and allied health-care professionals from diverse disciplines participated in 14 workshops across the region randomly selected. A further 40 patients and carers attended the workshops held during the Diabetes UK awareness day and this information was supplemented by 27 written submissions.
Participants were asked to consider the patient's journey from diagnosis through initial management, use of secondary care diabetes services, tertiary services and eventually death. At each stage areas of good practice, service deficiencies and suggestions for service improvement were identified. The journey was mapped in a large flow chart with the identified stages, areas of good and deficient practice and the suggestions all recorded in a different colour. This information was reproduced as a pictorial patient journey map and forwarded to the participants and also to those unable to attend, for comment and corrections and thereby further enhancing ownership.
The views of patients and carers were considered essential to the effectiveness of the review of services. To supplement the two workshops, patients attending the outpatient clinic were also requested to submit written views on eight previously identified distinct stages of the patient journey. This was considered necessary to gain the opinions of people in the areas of poorer access to the regional Diabetes UK event.
The information gathered was collated and a regional flow chart, or service level map of the patient journey was constructed. The information also provided common themes where the service could be improved. Findings were analysed in terms of the Scottish Diabetes Framework considering the effects of rurality on these centrally driven directives, enabling the information gathered to be focused into a series of questions, representing the service needs for people with diabetes.
These questions were presented to a regional solutions conference to generate discussion and determine sustainable solutions to the issues raised as areas of system improvement in the mapping process. Invitations to attend this conference were distributed to all general practices, all secondary care personal involved in the care of people with diabetes, and to all patient and carer groups in Highland. Delegates were divided into small facilitated groups and, for each, the discussions and solutions to the questions posed were recorded.
The solutions were corroborated by the service planning group consisting of health board and primary and secondary care senior management and the director of public health using a modified Delphi technique12, and amalgamated to form the basis of a new service configuration for the region that reflected the national framework and the issues of rurality.
Results
From the workshops undertaken, 15 local patient journey maps were constructed, reflecting the wide geographical area, diverse professions and patient and carers' viewpoints.
Current service provision
The maps were amalgamated to form a service level map (Fig 1), the current service provision revealed that there is a dichotomous service for people with diabetes in Highland. Most patients present through their GP, and then enter into a cycle of care within primary care. There are numerous and varied referral criteria which, when reached, lead to the patient being moved into a cycle of care within the secondary care setting.
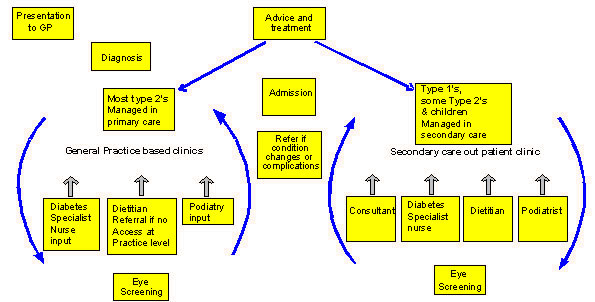
Figure 1: The current patient pathway represented in a service level map for people with diabetes in Highland.
In the region's 72 administratively distinct general practices there was a great variety in the nature of services. This in part reflects the variable geography of Highland, with small single-handed practices by necessity not having structured care, and the larger practices having organised care for people with diabetes.
A single-handed consultant managed care in the secondary care setting with four diabetes specialist nurses. Dietetic and podiatry services were provided in both the secondary and primary care setting but were inequitable in distribution. Eye screening was available in a variable format in both settings, a central call/recall system coordinated the screening; due to the small numbers in the remote settings there were issues over quality assurance.
Areas for system improvement
Four main themes, shown (Fig 2), were highlighted as areas for system improvement: (i) the need to reduce waiting times for secondary care out patients; (ii) an improvement in communication between health-care professionals; (iii) further education for both health-care professionals and patients, and (iv) the use and role of allied health professionals. From the mapping exercise, 10 distinct questions arose (Fig 2), and these were posed to the regional solutions conference.
Figure 2: The four main themes to emerge from the mapping exercise and a summary of the questions posed at the regional solutions conference.
Solutions
The solutions conference was attended by 97 health-care professionals, patients and carers and provided 17 solutions for the enhancement of services in Highland and are shown (Fig 3).
Figure 3: The seventeen solutions to the four themes identified in the mapping process developed in the regional solutions conference.
New service configuration
From the information gathered at the solutions conference a proposal for a new service configuration was possible and this is shown (Fig 4).
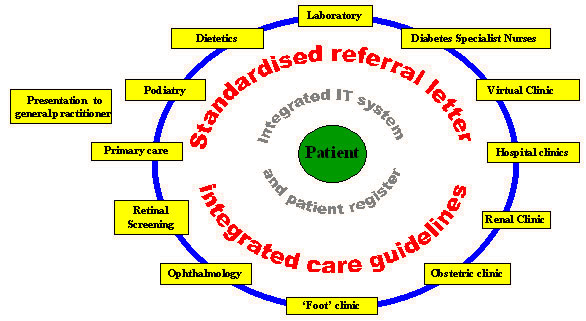
Figure 4: The proposed new service configuration derived from the planning process.
The child or adult with diabetes will usually present within primary care, and becomes the centre of the system. Access to health-care professionals will be possible, on referral, within a non-hierarchical and integrated managed clinical network of services.
The new configuration encourages the sharing of care between health-care professionals, coordinated by an integrated IT system and patient register, regulated by a standardised referral letter, with agreed integrated care guidelines.
The flow of information on a need-to-know basis, represented by the blue line (Fig 4), between relevant health-care professionals will prevent duplication, history repetition, and improve the continuity of care. The IT system allows for the integration of the retinal screening call/recall service, as well as contributions to audit, national data surveys and clinical governance.
Discussion
Over 300 health-care professionals patients and carers contributed to a consultation process inclusive of remote areas in Highland. Current services were demonstrated to be dichotomous in nature, variable in standard and inequitably distributed. The major areas for service improvement for people with diabetes were identified as: a reduction in waiting times, better communication, professional and patient education, and more equitable provision of allied health professionals. The process identified 17 solutions to solve these service issues and a new service configuration was proposed, with the patient at the centre of a managed clinical network, supported by a remotely accessible integrated information system and a patient register.
Transparency was of great importance throughout the information-gathering process to enhance ownership and to steer the way through numerous political sensitivities; all maps and processes were made available on the health board website13.
Solutions that were suggested were filtered by the steering group and interpreted in the light of the Scottish Diabetes Framework. To confer rigour to the process, the solutions and new service configuration were processed through several meetings and two separate committees. Similar modified Delphi techniques have been used to determine diabetes policy in other localities14.
The development of managed clinical networks is similar to other regional service developments in Scotland and to support these a suitable integrated IT system is available. Financial backing for IT development is available from the Scottish Executive, and a minimum core-dataset is already published. The development of agreed integrated care guidelines will help develop a more seamless service. The care of uncomplicated diabetes in the primary care setting has been shown, by randomised controlled trial, to be appropriate15.
The National Institute for Clinical Excellence has recommended that structured patient education is made available to all people with diabetes at the time of initial diagnosis, an ideal that is to be adopted within Highland.
The development of a virtual consultation clinic will be an innovative advance overcoming the issues of access to service in the remote setting. Interactive health technologies have helped to address some of the challenges in diabetes care16. Virtual health networks have been developed for other chronic diseases in remote regions and are effective in improving clinical indicators17.
The practical recommendations to the secondary care services of increasing the interval between review appointments and auditing the existing people on the waiting list are similar to other initiatives to reduce waiting times in other areas of health care. Reviewing consultant diabetology resources reflected an element of local political difficulties.
Representatives of Diabetes UK deemed the clarification of badges a very important issue. This is only a small change that will make a big difference to the patient.
In the Tayside region of Scotland, similar work has been undertaken to resolve the increasing burden of diabetes18. The drivers for change were similar to those in Highland and included an increasing diabetic population, variability of access to services, increasing outpatient waiting times, and government directives.
The proposed service configuration focuses on the patient as the centre of the system but uses a population-based diabetes clinical information system. Such a system will help to manage and monitor the increasing burden of the care for people with diabetes19.
Several outcomes have developed from the work. Local agreement, reflecting the unique rural situation of Highland was reached to take forward the Scottish Diabetes Framework, with the formation of a managed clinical network. Integrated care guidelines are being developed among the professions involved. The outpatient waiting list has been audited with a view to discharging patients. Local agreement has been reached on the adoption of the Scottish Care Information Diabetes Collaboration IT system, underpinning the new service configuration. Accreditation for a multidisciplinary diabetes training course is being sought for Highland. The Scottish National Patient Information Pack is to be made accessible. Group sessions are being delivered by allied health professionals. Funding has been secured from the Scottish Executive Health Department for a telephone consultation service.
Conclusions
This work was driven by the rising trend in the number of people with diabetes, and centrally directed reforms of services for people with diabetes accentuated in areas of rurality. The WHO indications that there is a growing burden and a need for service changes in the care of people with diabetes1,20 apply to the remote and rural setting. The solutions to the factors that are driving change need to undergo rigorous local processes to ensure local ownership and success, confirming that different ways of working are even more critical in remote areas in the determination of service planning21.
The implementation of government directives presented a considerable workload for a relatively small health board; further investigation is needed to examine the impact of government directives on remote and rural communities and organisations. Success was dependent on the integration of connections, remote communities and culture22 among health-care professionals, patients and their carers though empowering people to influence and to see the results of change.
It is the lack of services and the inappropriateness of approach, not poor compliance, that leads to poor diabetes control23. Following the implementation of guidelines and organisational improvements, changes primarily occur in process outcomes24. Improvements in patient reported outcomes following the introduction of service level changes have been reported in a rural setting25. An evaluation of the process outcomes and improvements in the wellbeing of people with diabetes, resulting from the implementation of the solutions and the adoption of the new service configuration, is essential to establish the success of service changes in the remote and rural setting.
References
1. WHO. Diabetes. (Online) 2003. Available: http://www.who.int/hpr/NPH/docs/gs_diabetes.pdf (Accessed 18 March 2005).
2. Gatling W, Budd S, Walters D, Mullee MA, Goddard JR, Hill RD. Evidence of an increasing prevalence of diagnosed diabetes mellitus in the Poole area from 1983 to 1996. Diabetic Medicine 1998; 15: 1015-1021.
3. Must A, Spadano J, Coakley EH, Field AE, Colditz G, Dietz WH. The disease burden associated with overweight and obesity. JAMA 1999; 282: 1523-1529.
4. Newnham A, Ryan R, Khunti K, Majeed A. Prevalence of diagnosed diabetes mellitus in general practice in England and Wales, 1994 to 1998. Health Statistics Quarterly 2002; 14: 5-13.
5. Neil HA, Gatling W, Mather HM et al. The Oxford Community Diabetes Study: evidence for an increase in the prevalence of known diabetes in Great Britain. Diabetic Medicine 1987; 4: 539-543.
6. Stovring H, Andersen M, Beck-Nielsen H, Green A, Vach W. Rising prevalence of diabetes: evidence from a Danish pharmaco-epidemiological database. Lancet 2003; 362(9383): 537-538.
7. Wild S, Roglic G, Green A, Sicree R, King H. Global prevalence of diabetes: estimates for the year 2000 and projections for 2030. Diabetes Care 2004; 27: 1047-1053.
8. Currie CJ, Williams DR, Peters JR. Patterns of in and out-patient activity for diabetes: a district survey. Diabetic Medicine 1996; 13: 273-280.
9. NHS Highland. Improving care for people with diabetes: Epidemiological needs assessment for people with diabetes in Highland. (Online) 2003. Available: http://www.show.scot.nhs.uk/nhshighland/Health%20Services/Diabetes/Reports/epidemiological%20needs%20assessment.pdf (Accessed 14 January 2005).
10. Moore A. Out in the field. Health Service Journal 2003; 113(5867): 10-11.
11. Scottish Executive Publications. Beyond boundaries: a development approach to improving inter-agency working. (Online) 2002. Available: http://www.scotland.gov.uk/library5/health/bbex.pdf (Accessed 8 March 2005).
12. Jones J, Hunter D. Qualitative research: consensus methods for medical and health services research. BMJ 1995; 311(7001): 376-380.
13. NHS Highland. Report of the Highland Diabetes Redesign Project. (Online) 2003. Available: http://www.show.scot.nhs.uk/nhshighland/Health%20Services/Diabetes/Reports/Full%20report.pdf (Accessed 18 March 2005).
14. Gallagher M, Bradshaw C, Nattress H. Policy priorities in diabetes care: a Delphi study. Quality in Health Care 1996; 5: 3-8.
15. Forssas E, Keskimaki I, Reunanen A, Koskinen S. Widening socioeconomic mortality disparity among diabetic people in Finland. European Journal of Public Health 2003; 13: 38-43.
16. Piette JD. Enhancing support via interactive technologies. Current Diabetes Reports 2002; 2: 160-165.
17. Celler BG, Lovell NH, Basilakis J. Using information technology to improve the management of chronic disease. Medical Journal of Australia 2003; 179: 242-246.
18. Emslie-Smith A, Hunter K. Completing the jigsaw: Strategy and Implementation Plan for managing increasing demand in adult diabetes services. Dundee: Tayside Diabetes Advisory Group, 2004.
19. Morris AD. Considerations in assessing effectiveness and costs of diabetes care: lessons from DARTS. Diabetes/Metabolism Research Reviews 2002; 18(Suppl 3): S32-S35.
20. Gruber W, King H. The WHO national diabetes programme initiative. Diabetes Research & Clinical Practice 1996; 34(Suppl): S1-S6.
21. Clark J. Perhaps small is beautiful after all? Online (2003). Available: http://www.hsmc.bham.ac.uk/news/vol9iss2.htm#JMC-art (Accessed 17 February 2005).
22. Jensen GM, Royeen CB. Improved rural access to care: dimensions of best practice. Journal of Interprofessional Care 2002; 16: 117-128.
23. Simmons D. Impact of an integrated approach to diabetes care at the Rumbalara Aboriginal Health Service. International Medical Journal 2003; 33: 581-585.
24. Valk GD, Renders CM, Kriegsman DM et al. Quality of care for patients with type 2 diabetes mellitus in the Netherlands and the United States: a comparison of two quality improvement programs. Health Service Research 2004; 39: 709-725.
25. Maddigan SL, Majumdar SR, Guirguis LM et al. Improvements in patient-reported outcomes associated with an intervention to enhance quality of care for rural patients with type 2 diabetes: results of a controlled trial. Diabetes Care 2004; 27: 1306-1312.
Abstract
Introduction: The number of people with diabetes is increasing leading to a greater burden on health care services. The impact of the growing prevalence is accentuated by remote and rural demographic and geographic characteristics. Highland is a sparsely populated remote and rural area in the north of Scotland, characterised by poor access to health-care services and pockets of marked deprivation. Centralised policy developments demanding local implementation compounded the pressures on a system that already had waiting times of over 90 weeks for some people with diabetes. A regional review of services, engaging stakeholders from all disciplines and geographical locations was required to develop acceptable and sustainable solutions. This article describes the extensive mapping process involved, how solutions were derived, and suggests a new service structure to encompass remote health-care issues.
Methods: Health-care professionals with an interest in diabetes were identified and workshops were organised to include the remote areas of Highland. Patient and carers views were ascertained through workshops and supplemented by written submissions. Using the redesign methodology the patient pathway was mapped, noting service deficiencies and good practice. The information gathered was constructed into a service-level map representing the patient journey. A conference was organised to develop solutions to the issues raised during the mapping process. From these solutions a new service configuration was constructed.
Results: Over 300 health-care professionals patients and carers contributed. Fourteen workshops were held across the region including the remote areas, providing 15 local maps of the patient pathways subsequently amalgamated into a service-level map. The current patient pathway in Highland follows a traditional and dichotomous cycle of care in the primary and secondary care setting, partly reflecting the rural nature of healthcare in the Highlands. Four main areas for service improvement were identified: a reduction in waiting times for secondary care out patients; an improvement in communication between health-care professionals; further education for both health-care professionals and patients; and the use and role of allied health professionals. Seventeen solutions were recommended, including the introduction of a managed clinical network, use of an integrated IT system, use of a remote access consultation clinic, and web-based peer education and group sessions for allied health professionals. A new service configuration was proposed with the patient at the centre of a non-hierarchical system using standardised referral letters with a seamless flow of information.
Conclusion: Local processes for the implementation of government directives are imposing pressures on relatively smaller organisations. These pressures develop as a result of attempts to ensure local ownership and in overcoming the difficulties unique to the remote and rural setting. Further evaluation of the implementation of initiatives to solve the issues of service planning in remote areas is needed to clarify their level of effectiveness.
Key words: diabetes, mapping, redesign, rurality, service planning, sustainable solutions
You might also be interested in:
2018 - Lack of Medical Resources and Public Health Vulnerability in Mongoliafs Winter Disasters
2006 - Essential tips for measuring levels of consumer satisfaction with rural health service quality
