Introduction
Children residing in areas outside major metropolitan centres may be at higher risk of injury incidence and adverse outcomes as they are routinely exposed to environmental hazards, travel long distances to receive medical care in emergencies and are reported as more likely to receive inadequate supervision1. High injury mortality rates of children aged less than 5 years in rural Australia, compared to urban children, are concerning2. The incidence of hospital admissions due to injury is significantly higher in rural/remote Australian children than those who live in metropolitan areas, and children residing in rural areas are 2.4 times more likely to die from unintentional injury than children living in metropolitan areas1. This has been attributed to the unique combination of home and workplace on rural/remote properties1.
The leading cause of injury or death to children in rural/remote areas in Australia is transport incidents3. One significant subclassification of these is low-speed vehicle run-over (LSVRO), defined as ‘an incident where a pedestrian – usually a child – is injured or killed by a slow moving vehicle travelling forwards or reversing’3. Since being first identified as an important contributor to paediatric injury in 19644 a growing body of evidence shows LSVRO events as an area of increasing concern in various countries, including the USA5-8 UK9 Austria10, Brazil11 and New Zealand12-15. To date, research suggests that those most at risk are children aged 0–4 years, especially boys13,16,17. Recent Australian data collected by the authors indicate that the incidence of LSVROs among children aged 0–15 years is increasing, and that rates in Australia (particularly of non-fatal LSVROs) are among the highest in the world16.
A recent statewide, population-based 11-year retrospective study conducted by the authors of fatal and non-fatal LSVRO events in Queensland, Australia, suggests that children residing outside major cities may be at greater risk for LSVRO events than children residing in metropolitan areas18. However, the true extent of LSVRO events in rural/remote Australia is unknown. Until the magnitude of the problem is identified, and the risk factors explored, initiatives to prevent these events are unlikely to be effective.
The aim of this article is to describe incidence rates of LSVRO events for various areas of remoteness in children aged 0–14 years in Queensland, from 199 to 2009, and to describe the associated patterns of injury, with respect to gender, age group, severity, characteristics (host, vehicle and environment), and trends over time.
Methods
This study was a population-based retrospective, cohort study of LSVRO events, aiming to obtain the most comprehensive estimate of the magnitude of the mechanism as a function of geographical remoteness. A case series was undertaken to determine the nature of LSVRO events. This study adopted the LSVRO definition from the Queensland Commission for Children, Young People and Child Guardian (CCYPCG, now named Queensland Family and Child Commission) and Queensland Injury Surveillance Unit (QISU)19 where a pedestrian, usually a child, is injured or killed by a slow-moving vehicle (<30 km/h) in both traffic and non-traffic areas. To avoid potential incident identification, the authors have attempted to be as sensitive as possible with these data; hence, where counts were less than five, data were not described.
Data were collected (and linked to one unique identifier) on LSVRO events that occurred among children aged 0–14 years in Queensland from 1999 to 2009 from five relevant data sources:
- prehospital – patient care records regarding patients attended by Queensland Ambulance Service
- emergency department (ED) – information on patients treated at EDs in Queensland
- hospitalisation – Queensland Admitted Patient Data Collection (all children admitted to any hospital for 24 h or longer in Queensland)
- injury surveillance data – QISU, sourced from various (but not all) hospital EDs in Queensland
- fatality data – information pertaining to any childhood death, including coroners’ findings, police reports and hospital information from the CCYPCG-Child Death review.
The data extraction process has been described in detail elsewhere16,18,20.
For each case, the Areas of Remoteness Index of Australia+ (ARIA+) code was used as a measure of remoteness21. This was based on the postcode of the child’s place of residence. ARIA+ was developed by the National Centre for the Social Applications of Geographic Information Systems. Each geographical area is allocated a score between 0 and 15, based on the (road) distance to nearby towns that provide services. Scores are then allocated to the following categories: ‘major city’ (0.0–0.2), ‘inner regional’ (0.21–2.4), ‘outer regional’ (2.41–5.92), ‘remote’ (5.921-10.53) and ‘very remote’ (≥10.53). For the purposes of this article, ARIA categories 4 and 5 (‘remote ‘and ‘very remote’) were combined.
Data analysis
Crude incidence rates for LSVRO events were calculated separately for the four remoteness categories. The Australian Bureau of Statistics provides population data for each single year of age, for each remoteness category, from 1901 until 2006. After 2006, population data are only available for each remoteness category for age groups (not single year of age), and not for every calendar year. The summary data on age groups per remoteness category from 2006 were compared with the population data provided per age year, for calendar years up until 2006. There were no marked differences relating to the age group of interest in this study (0–14 years).
To calculate incidence rates across the categories of remoteness for children aged 0–4 years, the estimated population at 2006 for the age group 0–4 years was used as the population denominator for this age group for every year from 1999 to 2009. While there are inaccuracies using this approach, it was the most valid of all available approaches. This process was repeated for the age groups 5–9 years and 10–14 years. Incidence rates for LSVRO events (number of LSVRO events in relevant remoteness category divided by population in relevant remoteness category) were calculated separately for males and females, for males and females combined, for fatal events, non-fatal events (hospital admissions and non-admissions, respectively), and for all LSVRO events. In addition to incidence rates, risk of LSVRO events in each geographical region relative to metropolitan region (incidence of LSVRO events in inner region divided by incidence of LSVRO events in metropolitan region), together with 95% confidence interval (CI), were calculated using the Statistical Package for the Social Sciences v21 (SPSS; http://www.spss.com). Epi Info v7.0 (Centers for Disease Control; https://www.cdc.gov/epiinfo/index.html) was used to calculate χ2 tests for trend to determine trends over time in incidence rates.
Descriptive analyses were used to examine the patterns of injury in children across the various remoteness categories. Where variables were categorical, χ2 analysis was used. (Where expected cell counts were less than 5, Fisher’s exact method was used.) For continuous variables, t-tests or analysis of variance (ANOVA) were used. Where data were not parametric or group sizes were less than 30, Mann–Whitney U-tests or Kruskal–Wallis tests were used.
Ethics approval
Ethics approval for this study was sought and granted from the Children’s Health Queensland Human Research Ethics Committee (HREC/09/QRCH/79), University of Queensland Medical Research Ethics Committee (2009001464) and Director General, Queensland Health Public Health Act (RD002327).
Results
Over the 11 years from January 1999 to December 2009 a total of 1506 children aged 0–14 years for whom data on ARIA were extracted were involved in an LSVRO event. Figure 1 shows LSVRO incidence rates over the 11-year study period as a function of remoteness. Just over half of LSVRO events occurred in major cities (n=826, 13.8/100 000/annum). During the 11 years, 45% (n=680) of LSVRO events occurred outside major cities. Compared with children aged 0–14 years living in major cities, incidence of LSVRO events was 3.08 times higher (95%CI=2.70–3.51) in children living in outer regional areas, 1.70 times higher among children living in inner regional areas (95%CI=1.48–1.95), and 2.12 times higher among children living in remote/very remote areas (95%CI=1.69–2.65). Overall, the highest incidence rates were observed in outer regional areas (n=315, 42.5/100 000/annum; 95%CI=42.37–42.56), and rates were highest in these areas for 9 of the 11 years of the study. Among children aged 0–14 years generally, no significant changes were observed in the incidence of LSVRO over time, except for those living in inner regional areas, and remote/very remote areas. For children living in inner regional areas, LSVRO incidence increased significantly over time (p<0.001), and this was true for males (p<0.001) and females (p<0.05). However, this is likely to be influenced by a peak that occurred in 2008 in inner regional areas (46.6/100 000; 95%CI=46.31–46.83; 56 events occurred in 2008, compared with between 10 and 29 events for all other calendar years). In contrast, incidence of LSVRO events decreased significantly over time among children living in remote/very remote areas, by approximately 1.3% per annum (p<0.05).
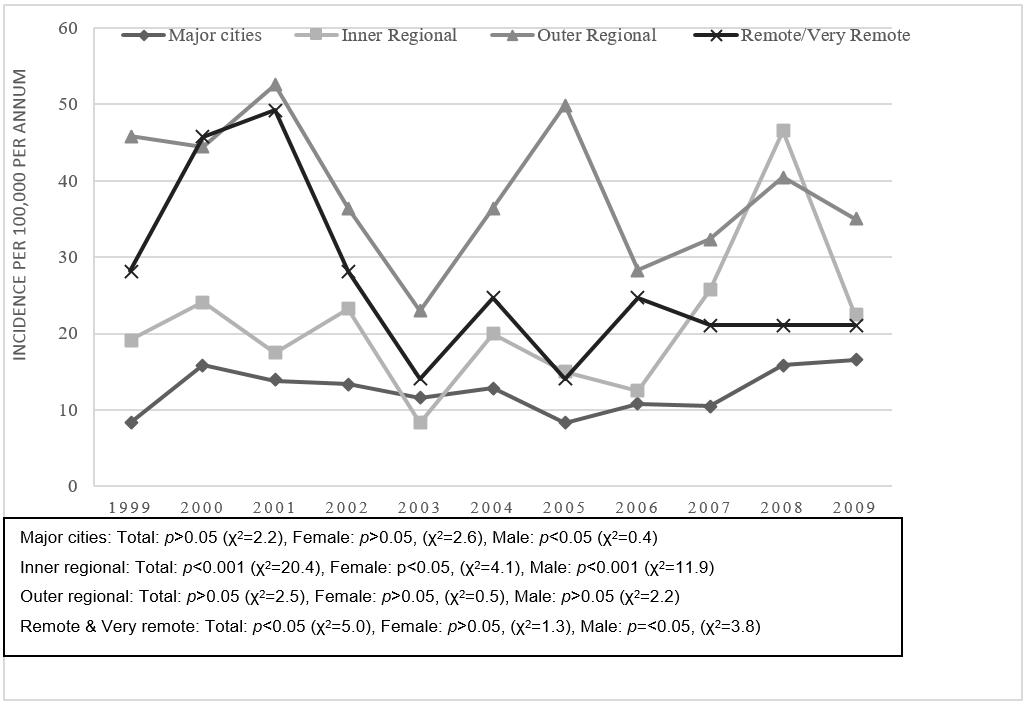 Figure 1: Crude low-speed vehicle run-over incidence by Remoteness Area category, and incidence rates by Areas of Remoteness Index of Australia status and gender, Queensland, 1999–2009.
Figure 1: Crude low-speed vehicle run-over incidence by Remoteness Area category, and incidence rates by Areas of Remoteness Index of Australia status and gender, Queensland, 1999–2009.
Age group
Overall, the age group most at risk of an LSVRO event was 0–4 years (n=605; 40.1%); however, the age group of children involved in an LSVRO event varied significantly by remoteness (χ2=14.62, degrees of freedom (df)=6, p<0.05). For outer regional and remote/very remote areas, LSVRO events were significantly more likely to occur among young children aged 0–4 years, but this was not true for major cities. Approximately half the events that occurred in remote/very remote areas involved young children (n=43, 49.4%; Table 1). Incidence was 2.68 times higher than among children in this age group living in major cities (95%CI=1.95–3.69). Almost half the events that occurred in outer regional areas (n=140, 44.9%) involved young children aged 0–4 years, and LSVRO incidence was 4.03 times higher than among children in major cities (95%CI=3.32–4.91). In inner regional areas, 40.4% (n=122) of events involved this age group; incidence was 2.07 times higher than children living in major cities (95%CI=1.67–2.55; Table 2).
LSVRO incidence was consistently higher in areas outside major cities for every year of the study in children aged 0–4 years (Fig2). In this age group, the highest incidence rates were observed in children living in outer regional areas, for almost every year of the study (Fig2). Significant reductions in LSVRO incidence were observed during the 11 years of the study among children aged 0–4 years living in outer regional areas (χ2=11.01; p<0.001), inner regional areas (χ2=8.18; p<0.01) and in major cities (χ2=16.58; p<0.001). A reduction in incidence was also observed among children aged 0–4 years living in remote/very remote areas, although not of the same magnitude (χ2=3.09; p>0.05). Incidence rates were higher in all regions outside major cities for children aged 5–9 years. Incidence was highest for children living in outer regional areas (38.65/100 000/annum; 95%CI=38.51–38.81) – this was 2.73 times higher than among children living in major cities (95%CI=2.16–3.44). Incidence was 1.49 times higher for children in inner regional areas (95%CI=1.16–1.90), and 1.76 times higher for children in remote/very remote areas (95%CI=1.16–2.68). LSVRO incidence increased significantly over time in this age group, among children living in remote/very remote areas (χ2=10.65; p<0.01), whereas incidence decreased during the study period among children living in outer regional areas (χ2=6.25; p<0.05). No significant changes over time were observed for children aged 5–9 years in major cities or in inner regional areas (p>0.05).
Among older children aged 10–14 years, LSVRO incidence was higher in all areas outside of major cities, with incidence being highest in those living in outer regional areas (relative risk=2.73; 95%CI=2.16–3.44; incidence rate is per 100 000, per annum). Incidence increased significantly during the study period for those living in inner regional areas (χ2=8.8, p<0.01), outer regional areas (χ2=19.34, p<0.001) and major cities (χ2=29.3, p<0.001). While incidence increased among those living in remote/very remote areas, this was not significant (χ2=0.82, p>0.05).
Table 1: Low-speed vehicle run-over incidence (per 100 000 per annum) by Remoteness Area, age group and gender, 1999–2009, Queensland 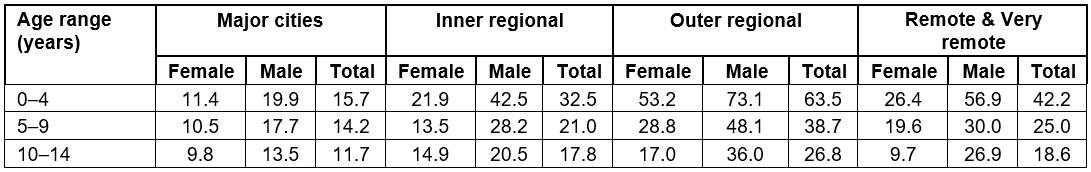
Table 2: Relative risk of low-speed vehicle run-over by Remoteness Area, age and gender, Queensland, 1999–2009†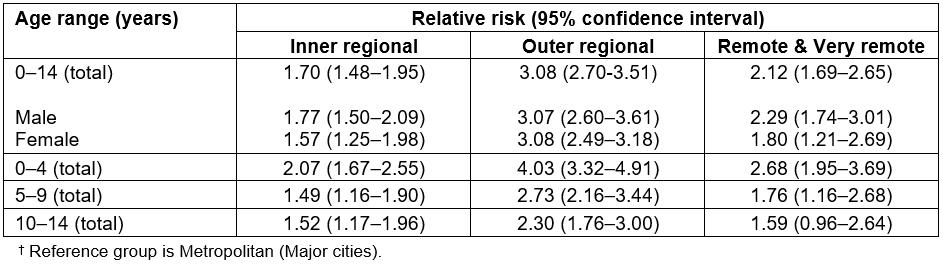
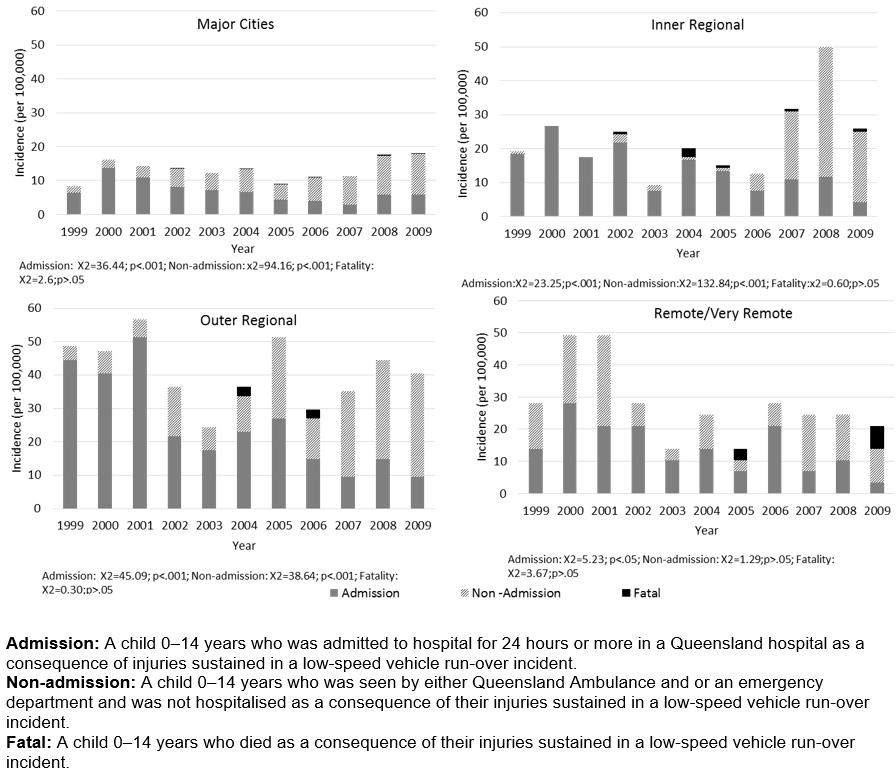 Figure 2: Crude low-speed vehicle run-over incidence (per 100 000) by severity (fatal, admission and non-admission) by Remoteness Area, Queensland, 1999–2009.
Figure 2: Crude low-speed vehicle run-over incidence (per 100 000) by severity (fatal, admission and non-admission) by Remoteness Area, Queensland, 1999–2009.
Gender
Incidence was higher in males than females (Table 1) for every region, across all age groups, for every year of the study. For both males and females, incidence was greatest in outer regional areas (males: 51.8/100 000; 95%CI=51.67–51.99; females 32.5/100 000; 95%CI=32.42–32.63). Relative risk was consistently higher for males in each region (Table 2).
Severity
Incidence of LSVRO events resulting in fatalities, hospital admission and non-admission are shown separately in Figure 2, by remoteness and calendar year. Mortality was highest in remote/very remote areas (1.06/100 000/annum; 95%CI=1.05–1.06). Incidence of fatal LSVROs was highest among young children aged 0–4 years, for every category of remoteness, and higher among girls than boys for every category of remoteness except for those living in outer regional areas The highest recorded incidence of fatal LSVROs during the study was in boys aged 0–4 years living in remote/very remote areas (3.79/100 000; 95%CI=3.76–3.82; n=2). The number of LSVRO fatalities in each remoteness category were n=7 for ‘major cities’, n=6 for ‘inner regional’, n=4 for ‘outer regional’ and n=3 for ‘remote/very remote’. Over time for children aged 0–14 years, mortality varied most in remote/very remote areas (from 0 events to 2 events in 2009). Analyses of trends over time were not completed for mortality incidence due to small numbers.
Incidence of LSVRO events resulting in hospitalisation decreased significantly during the study period, for every category of remoteness (Fig2). Incidence was higher in young children aged 0–4 years than older children for every category of remoteness; the highest incidence in this age group occurred in outer regional areas (46.1/100 000; 95%CI=45.91–46.28) and remote/very remote areas (30.32/100 000; 95%CI=30.14–30.50). Similarly, incidence of hospital admission was higher in boys than girls for every category of remoteness; the highest incidence for boys aged 0–14 years was observed in outer regional areas (32.19/100 000; 95%CI=32.01–32.37). In contrast, incidence of events not resulting in admission increased over time; this was significant for every category of remoteness except ‘remote/very remote’.
Host factors
In addition to the age and gender differences already described, socioeconomic status (measured using the Socio-Economic Indexes for Areas, see note in Table 3) varied significantly by remoteness category (χ2=555.2; df=12; p<0.005,). Almost a third of LSVRO events in major cities occurred in children whose geographical residence reflected the two highest levels of relative advantage (n=257, 32.9%). By comparison, this was true for fewer than 4% of events that occurred outside of major cities. More than half of all events involving children living in remote/very remote areas occurred in areas reflecting an average level of relative advantage (n=43), whereas this was true for 15% (n=113) of events in major cities.
Table 3: Sample characteristics by Areas of Remoteness Index of Australia status 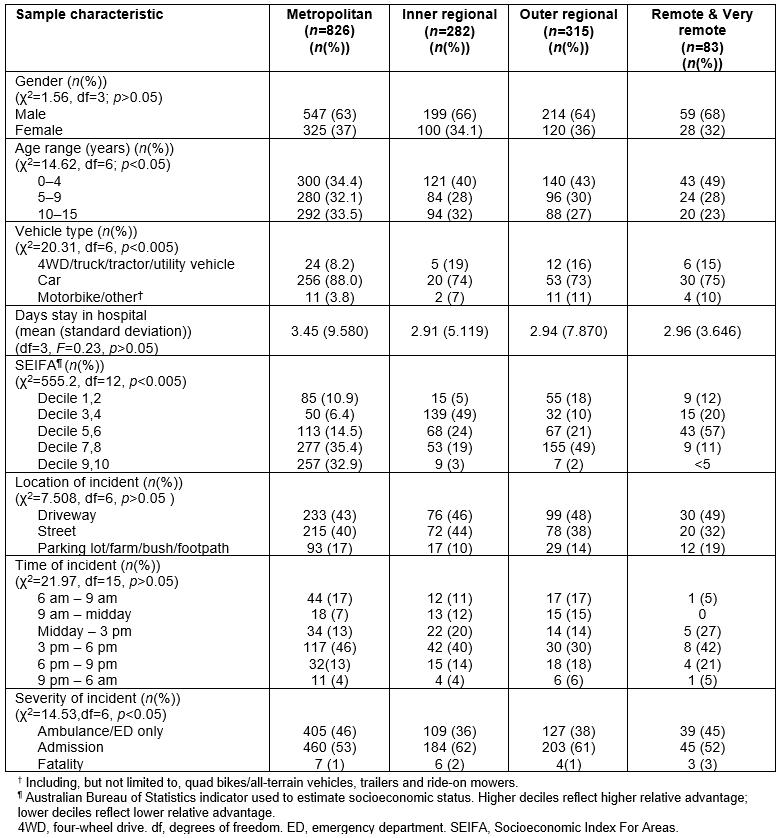
Environmental factors
No differences were observed in relation to time of day (χ2=7.508, df=6; p>0.05) or month of year (χ2=21.9, df=15; p>0.05), by remoteness category (Table 3). Events most frequently occurred between 3 pm and 6 pm across all of categories of remoteness, with one quarter of all events in remote/very remote areas occurring between 6 pm and 6 am (n=5, 26.3%).
Location of event did not vary as a function of remoteness category (p>0.05). The most common location for LSVRO events was the driveway (43–48.4%).
Vehicle factors
Data on vehicle type involved in LSVRO events was available from CCYPCG for fatal events, and from QISU for non-fatal events. (For these analyses, all cases captured in the QISU database are included, representing 260 children who presented for treatment to an ED only, and 178 children who were admitted to hospital.) Cars were the vehicle type most frequently involved in LSVRO events for all categories of remoteness (Table 3). For the purposes of analyses, vehicles such as motorbikes, quad bikes/all-terrain-vehicles, trailers and ride-on mowers were combined into one category (‘other’), and heavier vehicles such as four-wheel drives, trucks, tractors and utility vehicles/light trucks were combined into one group. Heavier vehicles, as well as ‘other’, were more frequently involved in LSVRO events that occurred outside of major cities (χ2=20.31, df=6; p<0.005).
Injury characteristics
Characteristics of LSVRO events are shown in Table 3. Among children who were admitted to hospital as a consequence of the LSVRO event, the mean number of patient days in hospital was highest among children residing in major cities (3.45 days, standard deviation (SD)=±9.58), with the lowest among children in inner regional areas (2.91 days; SD=±5.119); however, there was no significant difference in length of stay by remoteness category (p>0.05). Body region injured and nature of injury did not differ by remoteness category (p>0.05).
Differences in primary injury sustained as a result of the LSVRO event were observed (analyses were not completed due to the nature of the data). Among children living in remote/very remote areas, the most frequent primary injury was ‘intracranial injury’ (n=7, 8%), whereas this was ranked third for children living in major cities (n=44, 5%) and outer regional areas, (n=21, 6.3%) and fourth for children in inner regional areas (n=15, 5%). Fracture of the lower leg was the highest ranking injury for children in major cities (n=73, 8.4%) and inner regional areas (n=26, 8.6%), and second for children in outer regional areas (n=24, 7.2%).
Discussion
This statewide, population-based study is the first to specifically examine LSVRO events in relation to geographical remoteness in Australian children. A further strength of this study is that data across the continuum of care (prehospital to fatality) were linked to obtain the most comprehensive estimate possible of the magnitude and nature of LSVRO events to date.
These data show that incidence rates are higher for every age group, for children residing outside major cities, for each of the 11 years studied. Children aged 0–4 years are those most at risk for these events, regardless of geographical location.
This is consistent with previous research on the disparity of rural health outcomes2,22. The literature indicate that people living in more inaccessible regions of Australia are often disadvantaged with regard to education and employment opportunities, income, access to goods and services and in some areas access to basic necessities22. The authors propose that children involved in a LSVRO in rural and remote areas may be at higher risk of sequelae due to the discrepancy in health outcomes and distance to tertiary hospitals1.
To date, there is minimal published literature on how injury characteristics resulting from LSVRO events vary as a function of geographical location. However, the Child Death Review (Queensland) found that the average annual mortality incidence from unintentional injury was 2.4 times higher in areas outside major cities between 2004 and 200823. Furthermore, transport incidents were the leading cause of injury and death to children in non-metropolitan areas. Data from NSW indicate that childhood pedestrian deaths occur less frequently in rural regions than in urban areas, probably due to decreased exposure24. These results clearly demonstrate that incidence of LSVRO events is higher for children outside major cities.
Not surprisingly, vehicle type involved in LSVRO events varied with remoteness and involved larger vehicles such as four-wheel drives, trucks, tractors and utility vehicles. Previous research indicates that fatal LSVRO events more frequently involve larger vehicles25-27. People residing in rural and remote areas are attracted to these larger, more durable and multifunctional vehicles because of the harsh environment and/or work (agricultural or mining). The higher rates of severe injury and death from LSVRO events in non–metropolitan areas observed in this study could be attributable to the fact that, in rural children, these events are more likely to involve heavy vehicles. This, combined with the possibility that vehicles tend to be older in rural areas, might result in delays in safety vehicle modifications compared with major cities28. A potential prevention strategy is to provide incentives to ensure compliance with vehicle safety in rural areas. Raising awareness regarding this type of event and the type of vehicles frequently involved will promote safer use of heavy vehicles, and vehicles such as quad bikes/all-terrain vehicles and motorbikes.
Limitations
Some limitations associated with this study include the lack of availability of population data by single year of age, for every calendar year of the study period. However as described in the methods, no marked differences were observed in population data when comparisons of age groups per remoteness category from 2006 were made with the population data provided per single year of age. This was the most valid of all available approaches. Another limitation is that incidence rates were calculated based on geographical residence of the child involved in the LSVRO event, and thus may not reflect the actual geographical location of the event in some instances. Also, analyses were limited by availability of data, especially for non-fatal events; however, as discussed in the methods article20, this was the only available data where such cases could be found at the time of data extraction. Data on children who sought treatment at an emergency department is less complete. It is likely that this study’s estimations of non-fatal LSVRO events that did not result in hospitalisation are conservative because data on these events are less complete than fatal events and hospitalisations. (The databases from which non-fatal cases were extracted are present at most but not all emergency departments in Queensland.) Also, databases accessed for this study (except for QISU) are administrative databases, therefore they do not consistently or routinely record information about circumstances leading to the event that are important for injury prevention.
Implications for prevention
Data from this study demonstrate that as well as increased incidence of LSVRO events in areas outside major cities, consequences from these events are worse possibly because, in addition to vehicle type involved, it takes longer for emergency services to be notified and reach the site, combined with the possibility that prehospital and emergency services are less well resourced in relation to treating major trauma28. There have been important systemic advances in Queensland over the last few years in relation to emergency and prehospital care for major trauma, since the adoption of a centrally coordinated trauma system following recommendations in the Trauma Plan for Queensland29. It will be imperative to monitor trends over time in relation to severity of LSVRO events to see whether these improvements translate to improved outcomes. While primary prevention strategies are optimal, secondary strategies are also important, especially in relation to LSVRO events outside major cities, to improve outcomes30. This means, in the rural setting in particular, coordination among all services is essential, improving provision of primary treatment, and more rapid notification and discharging of retrieval services. Healthcare providers in rural and remote regions need education on this increased risk of LSVRO injury and some of the main clinical injuries and characteristics surrounding LSVRO. The importance of early screening and treatment for post-traumatic stress disorder in young children is increasingly highlighted in literature31. Services are limited in rural and remote areas and this should be a serious consideration in discharge planning and transfer of care when patients are returning to their communities, as the first 2 years post injury have been identified as the at-risk time for both the patient and their families for traumatic injuries32.
A key environmental risk factor regarding injuries in children outside major cities12,28 is the unique combination of home and workplace on rural properties. Also important to consider is the variety of rural and remote areas settings in Queensland, including small towns, Aboriginal and/or Torres Strait Islander communities, island living, mining communities, hobby farms and very large, remote agricultural properties. All of these specific environments should be considered when developing an injury prevention strategy.
There should be particular focus on young children aged 0–4 years living in rural areas, as they are at greatest risk, and experience worse outcomes. Safe play areas are needed, with secure physical boundaries separating this area from hazards such as roadways, driveways and vehicles. While the safe play area concept has been comprehensively promoted in rural areas in Australia, there is evidence to suggest that this has not been widely adopted. One study of rural communities in Queensland found that one-third of respondents (primarily farmers with small children) did not have a fenced-off play areas separated from hazards1,2,28. Further research is needed about strategies to engage farmers and rural community groups, to establish what barriers to safety exist, and form collaborations to address these barriers. Comprehensive, targeted education strategies to improve awareness of LSVRO events and risk factors are recommended.
There are two critical elements authors can suggest to decreasing incidence and severity of outcomes of LSVRO events in rural communities. The first is to improve the commitment towards ongoing education for parents and communities, including safety programs, and area/culture-specific advertising (such as a social media campaign). Second, additional ongoing reviews and needs of the requirements of rural and remote areas will help to ensure high-quality trauma management systems and resources are in place.
Conclusion
Children residing outside major cities in Queensland have a higher risk of being involved in LSVRO events than children living in metropolitan areas, for both males and females, for every age group, for each of the 11 years studied. Risk was highest in young children aged 0–4 years living in outer regional areas, followed by remote/very remote areas. Further research is required to elucidate the causes of this increased risk among rural and remote children, but it is known that a variety of cultural, socioeconomic and environmental variables contribute. More research is required about causal factors of LSVRO events in both metropolitan and rural/remote areas. Additional research will determine barriers to safety promotion in rural communities, particularly in relation to children. A prospective data collection system utilising existing injury and trauma databases is needed to optimise the level of detail collected on characteristics of rural LSVROs. It is also crucial to collect information on the long-term outcomes of LSVRO events occurring in rural children to identify multidisciplinary opportunities to improve recovery. Prospective data collection is also imperative to compare the impact of any interventions implemented over a period of time. There is a need for rural- and age-specific strategies to prevent LSVRO incidents in children living in rural and remote areas.

