Introduction
Rural acute care nursing is a generalist specialty that is as diverse as it is complex.1 Newly graduated registered nurses (RNs) who choose to work rurally will need to care for clients of all ages, most with unrelated diagnoses, while rotating between several focal points of care, including medical–surgical, emergency, labor–delivery, palliative, and constant care.2-4 They will also be expected to work autonomously and to fulfill additional duties when other professionals are off site or off duty.2-4 Developing and maintaining this array of skills will take time on the job and the support of seasoned colleagues; however, predictions about the numbers of senior RNs who will be available for this supportive role, based on Canadian RN workforce trends spanning the last 14 years, are alarming.5-11
For the purposes of this article, the term RN will refer to individuals with either a baccalaureate- or diploma-level nursing education.
Background
In response to a dearth of full-time jobs in 2002, many new Canadian RNs migrated to the USA to find work.5 In 2003, the last year for which data was published, only 22% of Canadian rural communities were successful at retaining new RNs during their first year of practice.6 Data about retention rates in acute care in general are alarming. In 2011, turnover intention rates among Québec new acute care RNs were high at 49%7 and in 2015, new RN turnover intention rates across Canada were reported to be as high as 57%.8 These findings are not surprising since transition has been reported as the most stressful time in new Canadian RNs’ careers and the main reason they leave the profession.9
Recent reports indicate that the future of the Canadian rural RN workforce appears bleak. While the percentage of RN positions across Canada increased by 18.5% between 2006 and 201510, the rural and remote RN population plummeted nearly 10%.11 Additionally, 2014 Canadian nurse workforce demographic information pointed to high RN retirement rates.11 Will new RNs choose to work in rural acute care and will there be senior RNs to support their transitions?
Literature review
A systematic integrative review12 of the extant qualitative and quantitative literature about new RNs’ transitions into acute care was conducted in 201113 and updated in 2017. Canadian literature specific to rural settings was sparse, necessitating the inclusion of studies from Australia, New Zealand, the UK, and the USA. Of the 38 studies included, only eight were specific to rural settings; none were Canadian. The other 30 studies involved urban or mixed rural–urban settings. Themes about transition arising from this review include theories, internal influences, and external influences.
Theories: While theories of transition into acute care have been generated over the past 42 years, none are specific to rural acute care settings. Three Canadian theories, Duchscher’s ‘A process of becoming’14 and ‘Transition shock’,15 and Nour’s ‘Becoming alive’,16 are based on urban acute care settings. Two UK theories, Kelly’s ‘Hospital nursing: It’s a battle!’17 and ‘Preserving moral integrity’,18 and one US theory, Kramer’s ‘Reality shock’,19 only incorporate mixed samples of rural and urban acute care RNs. Notably, all paint transition as a predominantly negative and shocking experience.
Internal influences: Internal influences on transition included role stress, moral integrity, and doubt in knowledge. Overall, these influences negatively impacted new RNs’ transitions into Australian rural settings20-22 and Australian,23-25 Canadian,7,26-34 New Zealand,35 UK,17,18 and US36-38 mixed rural–urban acute care settings.
External influences: External influences on transition included relationships with the other (i.e. RNs, nurse managers, and clinical nurse educators), working conditions, residency programs, mentorship programs, transition to practice programs, and certification courses.
Staff nurses and nurse managers were both supportive and unsupportive of new RNs’ transitions into rural settings in Australia20-22 and mixed rural–urban acute care settings in Australia,23-25 Canada,7,26-34 New Zealand,35 the UK,17,18 and the USA.36-38 Recently in Canada, it was reported that nurse managers who acted as authentic leaders played a significant role in creating positive working conditions for new RNs, which in turn reduced reports of new RNs’ burnout and poor mental health.39 Previously, the erosion of the clinical nurse educator role in acute care settings in Alberta, Canada, was reported by researchers as negatively influencing new RNs’ transitions.27
In 2016, researchers indicated that working conditions of new RNs in Canadian mixed rural–urban acute care settings were generally positive and stable over time, but that workplace mistreatment was a significant issue warranting change.40
To adequately orient and support new RNs transitioning into US rural and urban acute care environments, three program reviews recommended residency programs be used to increase new RNs’ confidence and competence levels, and to reduce turnover rates.41-43 To support new RNs’ transitions into Australian rural environments, researchers recommended implementing mentorship programs44-46 or rural transition to practice programs.47 To support new RNs’ transitions into rural and urban hospitals in British Columbia, Canada, a transition to practice program was developed.48 A review of this program completed in 2015 indicated that orientation for new RNs should be at least 4 weeks in length and new graduates should work at least 49 hours in 2 weeks.49 Based on province-wide research about educational needs of rural nurses in British Columbia, a rural-focused nursing certificate program was developed.50 A review of this program indicated that rural RNs’ competence, confidence, and job satisfaction increased. Most recently (2017), an online rural certification course was developed in Ontario, Canada, to support educational needs of rural nurses.51
While it is well documented that transitioning from the role of student to new RN in urban acute care settings is often stressful, leaving new RNs discouraged, frustrated, and disillusioned,7,14,15,25-38,52 it is unknown how transitioning into rural acute care hospitals is similar to or different from urban environments. Although the supports and challenges surrounding new RNs’ recruitment and retention in urban environments have been addressed,14,15 they remain unclear in relation to rural environments.
Purpose of the study and guiding question
The purpose of this study was to identify, understand, and explain how new RNs perceive the experience of transitioning into the rural acute care environment and the supports and challenges surrounding their recruitment and retention.53 The central questions guiding this study were ‘What are the experiences of new RNs transitioning into the rural acute care environment’ and ‘How do these experiences influence recruitment and retention?’53
Methods
An interpretive description design54 was used for this study. This approach facilitated interpretation of new RNs’ perspectives about (a) the phenomenon of transition in relation to the rural acute care hospital environment without losing sight of individual variations within that group, (b) the supports and challenges to rural recruitment and retention, and (c) strategies to inform future directions in rural acute care nursing at practice, policy, educational, and research levels.53
Setting
This study was conducted in 14 rural communities across the province of Alberta, Canada. The Alberta Health Services definition of rural acute care hospital was used to situate this study (acute care hospitals other than suburban or regional hospitals located in rural communities), in which emergency, medical, palliative, pediatric and, in some, surgical, obstetrical, or constant care services are provided.55
Participants
The College and Association of Registered Nurses of Alberta provided support for this study by distributing recruitment information to prospective participants. Inclusion criteria consisted of RNs with full-time, part-time, or casual employment of more than 1 month and less than 2 years in one or more Alberta rural acute care hospitals.53
Data generation
Over the course of 10 months, 16 semi-structured face-to-face, audio-recorded interviews were conducted and transcribed verbatim. Twelve new RNs were interviewed; four participated in second interviews guided by emerging categories; two of these four had changed job sites, hence the difference between number of settings (14) and number of participants (12). Notes to capture contextual data were audio-recorded following each interview. Pseudonyms were used to protect participants’ privacy.
Data analysis
The data analysis process was inductive and iterative.53 In keeping with the Interpretive Description56 approach, various techniques borrowed from other research domains were used to complete data analysis: data immersion from Hermeneutic phenomenology,57 unitizing and categorizing from naturalistic inquiry,58 and constant comparative analysis and memoing from grounded theory.59
Ethics approval
Ethics approval was received from the Athabasca University Research Ethics Board #CNHS-12-01.53
Results
Transition into the rural acute care setting involved participants learning and enacting the role of the rural generalist RN. Most described it as a huge learning curve that placed them on an emotional roller coaster. The few who felt well supported by interdisciplinary teams and with educational resources reported minimal fluctuations in their emotions; those who were not reported extreme fluctuations. Participants’ experiences ultimately impacted their decisions to remain in their current jobs or to seek work elsewhere, be it in rural nursing or not.
The context
The contextual factors influencing transition included the facilities in which participants worked and their educational preparation, other work experiences, and reasons for choosing rural nursing (Table 1).53
The hospitals where participants worked were of two different types: urban and generalist models. The services available and the participants’ transition experiences in these two different models of hospitals varied markedly.
The urban-model rural hospital was organized into separate medical, surgical, obstetrical, pediatric, and emergency units. A new RN was only expected to work on one unit and was well supported with an extended orientation and onsite clinical nurse educator. Learning was described as safe and manageable, but slow and frustrating.
Generalist-model hospitals were organized into two or three units (emergency department (ED), operating room, and acute care, which included a combination of medical, surgical, palliative, and obstetrical patients). Eleven of the 12 participants transitioned into this type of facility and were expected to work on the different units. They described their transitions as exhilarating, but overwhelming and frightening.
When asked what she would say to a new nurse transitioning into a rural generalist-model hospital, Mia candidly remarked:
I would tell them, ‘It’s a really awesome job, and you’re really going to love it. But you’re going to be scared shitless every day. So make sure that you are willing to walk in and have your mind open to … learn everything and understand that … you’re going to get all that responsibility put on you. Are you going to be able to deal with that? Because you’re going to get a wicked experience, but you’re also going to be really overwhelmed all of the time.
Table 1: Contextual factors influencing transition53 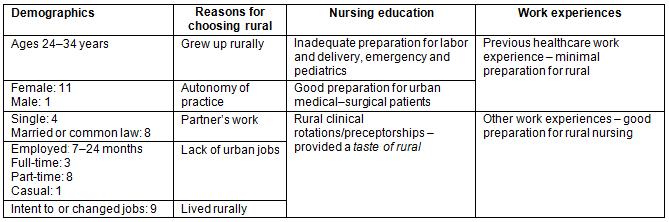
The consequences
Decision to stay or go: Alarmingly, 9 of the 12 participants had changed jobs or sought other employment within their first 2 years of practice. Three had moved to urban units, three to another rural acute care facility, and three had applied for positions in another area of their current workplaces.
Reasons to stay in the job included liking the people, small-town feeling, work schedule, and scope of practice; preferring rural living; feeling supported by staff and physicians; and supporting a significant other’s need to work rurally.
I like the staff. A lot of the girls are super nice to work with, and it’s fun. I guess growing up in a small community I missed that small-town feeling and … I got that … feeling working there. (Tina)
Reasons to leave the job included fear of critical incidents, desire for a different specialization, or feeling undervalued and bullied. For Kelly, critical incidents involving the unsafe practices of older senior RNs left her worrying about picking up bad habits and losing her licensure.
Tina sought work in an urban labor and delivery unit because she thoroughly enjoyed maternity nursing. Betty sought work in an urban ED because she loved trauma and everything like that and caring for the many awaiting placement patients in the rural hospital was not what she had signed up for.
Notably, John anxiously awaited a different position in the same hospital so that he could get away from his bullying manager. Xeno felt so undervalued by her nurse manager and unwelcome by senior RNs that she sought a job in a different rural hospital. Christina moved to another rural hospital because of the frequent bullying she was subjected to by senior RNs.
An explanatory model of transition: a double whammy!
The findings in this study revealed that participants’ transitions into the rural acute care environment constituted a double whammy consisting of two simultaneous non-discrete experiences of I’m a generalist! and I’m it! (Fig1).53
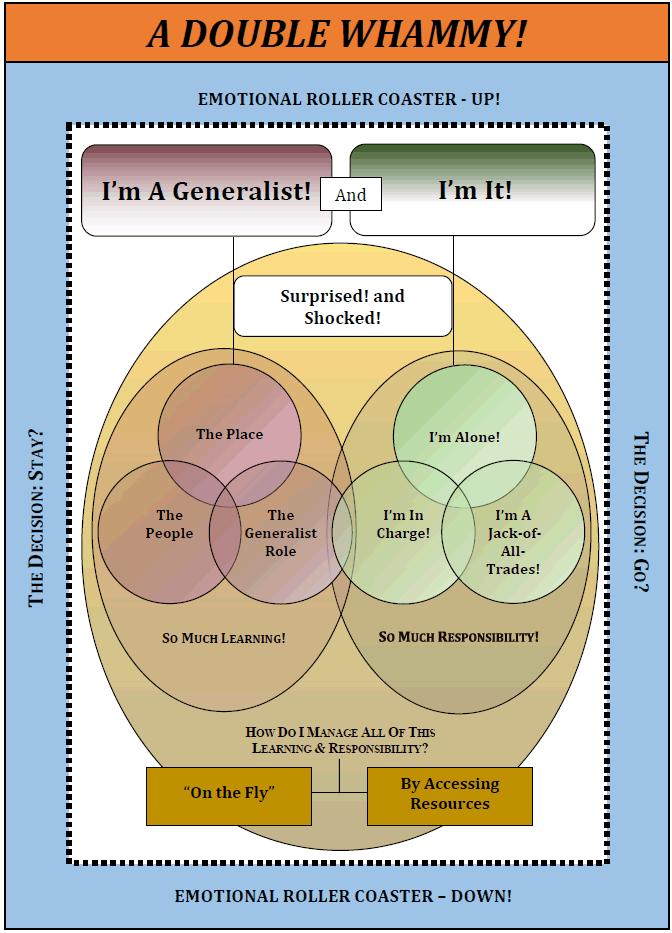 Figure 1: Illustration of the double whammy.53
Figure 1: Illustration of the double whammy.53
I’m a generalist!
For participants, I’m a generalist! involved learning about the people, the place, and the generalist RN role.
Participants learned about the people (staff and physicians who worked in the rural hospital and the patients and family members who accessed the hospital). For example, they reported that the staff and younger physicians who worked in the rural hospital were generally very supportive of their learning. Madeline highlighted:
She’s a phenomenal nurse because she gets you right in there. It’s her personality. She’s not overly intimidating, but she’ll push you enough and ask questions to make you understand what you’re doing, and it’s her attitude. She doesn’t make you feel stupid when you have questions …
Oprah expressed:
It’s like I’ve never worked in a better place. You’re a team. We all hang out after work, and its first-name basis all around … you follow through with them [physicians] about things. You can call down to the clinic. It’s so open; they’re all fantastic.
However, participants also reported that their personal and professional values were sometimes challenged due to senior RNs performing tasks the way they had always been done, rather than based on evidence. In most facilities, there was at least one person (RN, older physician, or nurse manager) who was impatient, unwilling to teach, and used negative communication techniques that consisted of yelling, passive aggressiveness, name-calling, telling not asking, or intimidation. Betty described the behaviors of some older physicians as follows:
There are certain situations where they would yell at you, and not really teach you. [Some] had no patience and were mad that inexperienced nurses were put in Emerg. So instead of showing us how to do something right, they would yell at us and walk away.
Participants learned that many patients and their families were friendly, encouraging, and appreciative, but that it took time to be accepted and trusted. Initially, most patients were uncertain about participants’ knowledge levels and abilities and trusting the new RNs was significantly influenced by the word of others, which travelled fast in the rural community. For Xeno, the candour of many rural people was shocking and created challenges when she tried to maintain nurse–client boundaries:
Everybody wants to know everything. So then you really have to guard what you’re willing to share. They’re helpful, but they’re a hindrance too because they … challenge what you’re supposed to say.
The environmental dynamics of the place wherein there could be a lack of onsite pharmacists and physicians left a few participants feeling overwhelmed and unsafe because of the responsibility to make high-level decisions about medication work60 and medical care. While lack of an onsite clinical nurse educator negatively affected participants’ learning and confidence levels, they also recognized this as a greater systems issue:
She’s supposed to be at our hospital once a week, but we never see her. She’s based out of the city, and she’s in charge of all the rural acute care hospitals in our area. So it’s sometimes tough. In her defense, she’s not a full-time position, and then spread quite thin between all of us. (Betty)
Enacting the generalist RN role required participants to learn on the fly and to skillfully change hats. They learned how to care for a variety of clients representing a mixture of ages, life stages, diagnoses, and cultures. They learned a broad range of clinical skills, as well as how to be flexible, undertake high levels of responsibility, and manage any kind of contingent or emergent situation, prioritizing care, and using anticipatory planning to access human and educational resources.
Mia described on the fly in two different ways based on having to manage the entire ED with only 10 days of orientation, a minimal number of certification courses, and without the direct back up of senior RNs. She assumed the responsibility of learning procedures or protocols for the first time, at the bedside while providing patient care, or by paging overhead for help from the nurses in the acute care ward. When Xeno was asked what on the fly meant to her, she described it as:
Like being in a snowball downhill. You just go. You roll with what comes in, and you use your critical thinking as best as you can. My first chest pain [I] didn’t really know what to do, [I] took cues. Second one [snaps fingers], I had it better and just kept going.
To change hats participants had to move from room to room, area to area, or unit to unit, frequently all within one shift (obstetrics to emergency, to paediatrics, to palliative, etc.). It was particularly challenging for most participants because it was new and very different from what they had learned during their baccalaureate nursing programs and involved prioritization, anticipatory planning, and delegation skills. Betty described it as:
Managing all those different clients, a surgical, post-partum, medical, or geriatric patient, all in one day, was a big learning experience because you constantly have to switch your thinking – change hats. There was a lot of learning … with prioritization, and I did have a bigger patient load. … There was a lot of making sure I was delegating so that everything got covered, and being responsible for anything serious …
I’m it!
For participants, I’m it! involved tackling even more responsibility in addition to learning to be generalist RNs. It included working alone, being in charge, and being a jack-of-all-trades. Christina found that:
You do everything. You do palliative one minute, you deal with a jaundiced newborn the next, the next minute you’ve got a mom walking in, in labour. Half an hour later, you’re on the phone to a family talking about transition services because you don’t have a transition services nurse – you’re it. You are handing out taxicab vouchers to folks who need to get across town but can’t afford it, so you’re working in a social work role because you don’t have a social worker. At four o’clock in the morning, you’re the unit clerk, entering clients’ demographic information into the system, so you can give them care because you’re it.
Working alone for Xeno meant that she was the sole RN on shift with only one licensed practical nurse (LPN) for onsite support. She described her first code alone as follows:
My LPN is my only other person there until the doctor gets there – so once he gets there, then I can delegate to the LPN to find somebody else [to come in]. But to keep all of that straight, and to not panic when you need more hands, but you can’t get them because you can’t send up a flare. Everything else I was taught how to deal with – the medications and compressions and the intubating. That isn’t actually what scared me. It was that I didn’t know how to get help. [I felt] alone, incredibly alone.
In other situations, working alone meant there was no available physician, which required participants to be resourceful and self-reliant when trying to prioritize and manage critical situations. Sally described her emotions when delivering a baby alone without the backup of a physician:
[I was] scared out of my wits – I didn’t want to be there! But I’m glad I was there because she couldn’t do it by herself, so it’s overwhelming, and it’s because you don’t have much to draw from. Then it’s like [the baby’s born], Oh my gosh, thank God!
Being in charge was very manageable and empowering for the few participants who were provided structured support and were not expected to manage charge responsibilities until later in their transitions. Gretta described being in charge as:
I actually really liked it … It was really good because she didn’t just [say], ‘Oh, you’re in charge now’. We had about an hour and a half meeting; we went through the charge nurse manual and responsibilities. So I wasn’t just thrown to the wolves, there was a lot of support.
Conversely, those who were immediately, and with little or no senior RN support or structured orientation, expected to be in charge, experienced emotions of exhilaration and panic. For some, this responsibility meant being in charge of the team of RNs, LPNs, and healthcare aides. For others, it meant being in charge of the acute care unit or ED and contingent or emergent situations (essentially every patient or family member who came through the door), which could be exciting, but also frightening. In some instances, it meant being in charge of the entire hospital:
The one night was absolutely horrible because it was me … and this travel nurse [who] had only been there a few days, and we had four women in labor [who] came in within two hours of each other. It was ridiculous! … Two of them delivered that night … and there’s me and her and an LPN, and the floor was full. (Ann)
Being a jack-of-all-trades required all participants to assume some of the responsibilities of other members of the interdisciplinary team (physicians, pharmacists, or respiratory therapists) and ancillary staff (unit clerks, medical records personnel, environmental services staff, maintenance workers, etc.) when these staff were off site or off duty.
Ultimately, participants’ transitions into the Alberta rural acute care environment constituted a double whammy! I’m a generalist! and I’m it! as described by Tina:
In the city hospitals, the units are so specific that you’re learning about heart clients or renal clients or maternity clients. Whereas in rural, you’re learning about all of them. You have to have a general basic idea of what’s involved with each condition and then learn the other things that are thrown at you, like charge nurse, janitor, pharmacist, and respiratory technician. ... When I went into rural it was a surprise … I didn’t think I would be in charge as soon as I was ... I didn’t think I’d be cleaning rooms. I thought those kinds of supports would just be there.
Discussion
Although this explanatory model of a double whammy is being proposed as providing a beginning understanding of transition into rural acute care nursing, the data suggest that comprehending the contextual factors influencing transition, as well as the I’m a generalist! and I’m it! components of the generalist role are foundational to rural new RN recruitment and retention.
Contextual factors
Notable is the finding that there are two models of acute care hospitals in Alberta deemed to be rural: the generalist model and the urban model. Participants who transitioned into generalist-model facilities experienced a wide range of emotional fluctuation, principally related to no onsite presence of physicians, pharmacists, or clinical nurse educators, and being expected to quickly enact the generalist role and be it. This finding speaks to the importance of researchers more clearly identifying a priori the type of rural hospital from which participants will be recruited.
Most participants felt inadequately prepared to work with maternity, emergency, and pediatric patients. Those who had participated in rural acute care clinical rotations or preceptorships during their nursing education had at least experienced a taste of rural, which they still considered insufficient for what was required of them.
A new contextual finding of this study was that the broader scope of practice of rural nursing, wherein autonomy is promoted, was a key reason for participants who had previously worked in health care under more limited scopes of practice to choose rural nursing as their first career choice. While autonomy has been identified by researchers as a hallmark of rural nursing,1-4,61,62 none have indicated this as a reason for new RNs to choose rural nursing.
The transition experience
Most of the findings in this study support and extend what has been reported in the literature.1-9,14-47,60-65 What sets this study apart from others is the fact that participants experienced fluctuating emotions that left them feeling exhilarated (pleasantly surprised) one minute and overwhelmed (shocked) the next. This finding contrasts with the results of many Canadian7,14-16,27,30-34,52 and international9,17-25,35-38,41-43 studies, wherein transition has been described as a predominantly negative, shocking experience.
Transition supports: Most participants identified feeling a strong sense of family or being a member of a supportive team, a finding well documented in the literature.1,4,62 However, a new finding in this study was that younger physicians provided significant support to participants during their transitions. While rural RNs’ positive interactions with physicians have been linked to increased job satisfaction, the dynamics of those relationships have not been delineated.1,4 In this study, some participants described their interactions with rural physicians as love–hate in nature, a description alluded to in the literature,4,63 but not specifically reported.
The fact that nearly half of the participants commuted is noteworthy, as they did not deal with issues related to lack of anonymity. Commuting participants felt accepted and supported by their rural patients despite not fully engaging in the community, as previously identified by researchers as integral to outsiders gaining acceptance in rural communities.1,4,63,64 Importantly, commuting participants did not link job satisfaction, and therefore retention, with community involvement, differing significantly from the findings of other researchers.4,63,64
Participants who appeared older and more mature found they were readily trusted and accepted by rural patients because they were perceived as possessing practice maturity. This is an interesting and new finding, although other researchers have discussed, in general, nurses’ acceptance into the community.1,4,63,64 It bears noting because many nursing programs in Canada are admitting students with previous education and life experiences.
Some participants embraced spirituality to cope with transition, a finding only alluded to in the literature as a spiritual tone.65 They incorporated prayer, faith, or nature into their work and or home lives to support their fitness to practice.
Transition challenges: To handle critical staffing shortages, many rural nurse managers contract agency RNs. The findings in this study highlighted how participants found it challenging and frightening to delegate work to agency RNs on night shift when no other senior RNs were available to support decisions. Previously, senior RNs had been integral to assisting new rural RNs with building the confidence needed to manage ambiguous situations and deploy human resources.4
Notably, a few participants were expected to assume the role of offsite pharmacists while in charge of clients, team members, and sometimes the entire unit or hospital, a finding not previously documented in the transition literature. This medication work60 was described by many participants as a huge learning curve, that was overwhelming, intimidating, and unsafe.
One participant was supported by a 3-month transitional graduate program similar to one48 created in British Columbia in 2013. She described the program as too generic and suggested she would have been better supported if the program had been tailored to her learning needs. She recommended weekly check-ins with the manager and preceptor to assist with identifying challenges and strategies to support those challenges. Interestingly, this program has since been discontinued in many Alberta rural hospitals, due to lack of funding.
Recommendations to support transition
At the policy level: It is recommended that funders consider the benefits of providing supports for new RNs transitioning into rural environments including onsite full-time rural clinical nurse educators, onsite transition to practice,48 certification,50,51 and mentorship programs,44-46 and new RN incentive scholarship programs.
At the education level: It is recommended that baccalaureate nursing students be exposed to rural learning opportunities including simulations of rural labor and delivery, emergency, and pediatric patient care; clinical practica in rural acute care hospitals; and final year nursing courses focused on the rural generalist role. It is also suggested that nurse educators collaborate with senior rural RNs and nurse managers to develop continuing education online leadership modules that include content about authentic leadership skills33 and how to support new RNs during transition into rural environments.
At the practice level: It is recommended that rural nurse managers provide longer structured orientation programs tailored to each new RN and his or her assigned mentor, but with check-in points to review progress.43 It is also suggested that rural nurse managers consider the benefits of providing incentives and onsite mentorship education for senior RNs who volunteer to mentor new nurses.
Limitations
The definition of the term rural was a significant limitation for two reasons. One, the classifications of rural previously referred to by researchers66,67 do not accurately address Canadian rural population growth and type of rural hospital. In this study, the populations of some communities deemed to be rural by Alberta Health Services exceeded the 10 000 population mark, a classification long used to delineate the upper end considered as rural in the Canadian literature.66 Two, the study was well under way before it was learned that the two different types of rural acute care hospitals obscured sample inclusion and exclusion criteria. Other limitations included that data were limited to one province of Canada, Alberta; participants self-selected, which resulted in a convenience sample;68 and males were not adequately included in the sample.
Implications for future research
The definition of rural and the different types of rural acute care hospital models must be considered a priori when researchers are investigating rural healthcare questions. Research examining current government policies and organizational structures related to recruitment and retention of new rural acute care RNs is warranted. Research exploring undergraduate educational methods and curriculum options related to preparing new RNs for employment in rural acute care environments is justified.
Conclusions
The explanatory model of a double whammy offers only one description of new RNs’ transition experiences into rural acute care, but may present readers with recognizable similarities about transition that resonate with their own learning and responsibilities.69 The supports and challenges to transition learned from this study can assist rural healthcare providers, policymakers, and educators in supporting and retaining new RNs in rural environments. Participants’ retention issues and current Canadian RN workforce demographics warrant further exploration of educational curricula and rural practice supports. While the findings from this study shed light on new RNs’ transitions into rural acute care, there are still many unanswered questions.
Acknowledgement
Jean Smith acknowledges Athabasca University, Red Deer College, and the Alberta Nurses Educational Trust for funding this study.

