Introduction
Type 2 diabetes is a lifelong disease that affects many people in urban and rural areas. Diabetes has significant social and economic effects on individuals and societies. It also has negative effects, which result from high healthcare expenditures for medical care. The cost of supportive measures for preventing the acute or chronic complications that occur in type 2 diabetes patients has a negative effect, too.1-4 Extended lifespans, urbanization, a sedentary lifestyle and changes in nutritional habits following medical and technological developments have increased the prevalence of diabetes,4,5 making it a significant public health problem worldwide. WHO considers diabetes to be pandemic.1,3 Prevalence differs by age, gender, race, nutritional patterns, and genetic and environmental factors.6 In addition, the risk factors for diabetes display some differences between urban and rural areas. Genetics, smoking, insufficient physical activity and hypertension are among the risk factors for diabetes in rural areas while stress and lifestyle affect those in urban areas.7
Diabetes is an important concern among healthcare professionals and researchers. This concern focuses on complications, treatment and prevention. Treatment of diabetes is a long-term and comprehensive process, and it includes the control of risk factors.8 Thus, diabetes is accompanied by a need for lifelong care and management. Since diabetes requires a change in lifestyle, individuals have a central role in their care.9 Individuals’ ‘belief of sufficiency’ or ‘self-efficacy’ for performing self-care behaviors is important for a successful personal disease management. According to social cognitive theory, self-efficacy is an important factor in facilitating behavioral change and ensuring health control. Self-efficacy is accepted to be the direct determinant of beliefs and behaviors.10
Individuals should be addressed considering their biological, physical, psychological, sociocultural and economic aspects. Their self-efficacy status should be evaluated for performing care. Studies on self-efficacy mostly address chronic diseases.11-16 Self-efficacy level is reported to be affected by socioeconomic status, education level,17 residence and income level.18 A study on self-efficacy in diabetes indicated that self-efficacy level is affected by problem-solving and self-management.19 In addition, enhanced self-efficacy positively affected the glycemic level of blood.20 It was negatively correlated with HbA1c levels,21 and effective in overall diabetes management.11,17,22-27
An important limitation concerning many studies on diabetes is that these studies focus mostly on urban areas. As a result of the migration of young people from rural areas to urban areas for economic reasons, an elderly and vulnerable population is left in rural areas.28 Therefore, studies on chronic diseases, diabetes in particular,29 should be expanded to cover rural areas. Individuals in rural areas try to manage their diseases using traditional methods due to cultural beliefs and practices and the lack of medications and equipment.30,31 In addition, the opportunity to access healthcare services and health attitudes is reported to be limited.32 The range of healthcare services provided by the government to rural areas is quite limited compared to that in urban areas.33 For these reasons, this study aims to determine the self-efficacy level of type 2 diabetes patients living in rural areas on disease management and the factors that affect that level.
Research questions were as follows:
- What is the self-efficacy level of diabetes patients who live in rural areas?
- Do the self-efficacy levels of diabetes patients differ by their sociodemographic characteristics?
- Do the self-efficacy levels of diabetes patients differ by their disease characteristics?
- Do the self-efficacy levels of diabetes patients differ by their metabolic control parameter characteristics?
- What are the determinants of the self-efficacy level of diabetes patients?
Methods
Research design and settings
This descriptive study was conducted in a hospital located in a rural area of Turkey that has an internal medicine polyclinic. In addition to checking up and examining patients, this polyclinic provides education and counseling via a diabetes nurse in the internal medicine service. The diabetes-education nurse also works as a service nurse.
Participants
The number of independent variables examined in this study was 22. Considering this number, the minimum sample size was found to be 195 at 90% power, 0.05 significance level and 0.15 effect size.34 The upper number, which corresponds to 216 individuals, was reached.
The inclusion criteria included the following:
- 18 years of age or older
- type 2 diabetes diagnosis displaying symptoms for at least 1 year
- no loss of mental ability.
In Turkey, rural areas are determined considering population and settlements with populations fewer than 20 000 people. The region where this study was conducted had a population of 20 156, including its district, villages and remote settlements. This region displays the characteristics of rural areas in terms of population, education, transportation and social life. Turkey’s rural population growth rate is 4%, fertility rate is 2.65%, perinatal care rate is 57.7%, internet access rate is 14.2% and GINI index (a standard economic measure of income inequality) is 0.39 (where 0 is total equality and 1 is total inequality). Unemployment rate is 5.9% in rural areas.35 The region in which the study was conducted has similar health and demographic indicators. However, its economic indicators could not be identified. In this region, agriculture and livestock are the main sources of living. The region is located about 160 km from the city center. The district hospital generally serves the people living in the villages located in the vicinity. This hospital has many deficiencies compared to the hospitals in the city center in terms of technology and personnel. Of the study sample, 55.1% consisted of diabetes patients living in villages and 44.9% consisted of those living in districts.
Instruments
A questionnaire and the Self-Efficacy Scale for Type 2 Diabetes were used to collect data. The questionnaire form consisted of 10 questions on sociodemographic characteristics and some health characteristics, 10 questions on disease characteristics, and 7 questions on metabolic control parameters. Questions on sociodemographic characteristics and some health characteristics covered age, gender, marital status, educational level, occupational status, place of residence (for the longest period), regular income, family type, household and smoking status. Questions on disease characteristics included the year of diagnosis, the number of medications and doctor visits within the last year, existence of another diabetes patient in the family, education on diabetes, perceived diabetes management level, knowledge about diabetes complications and diabetes complications. Patients’ body mass index (BMI) and certain metabolic control parameters (fasting blood glucose, HbA1c (%), cholesterol, low-density lipoprotein, high-density lipoprotein and triglyceride values) were obtained from patient records. Researchers did not perform a measurement or make a request for laboratory test. The data were collected in April and June of 2015.
The Self-Efficacy Scale for Type 2 Diabetes was developed by Van Der Bijl et al. and tested by Kara et al. for validity and reliability in Turkish.36,37 The validity test indicated that the scale explained 55.2% of the variance. The reliability test demonstrated that the scale’s internal consistency and inter-item correlation were 0.89 and 0.91, respectively, and that the Turkish version of the scale was valid and reliable. The scale consists of 20 five-point Likert-type questions.36 The minimum and maximum scores to be obtained from the scale are 20 and 100, respectively, with a high score indicating high self-efficacy.36,37 Cronbach’s alpha coefficient was 0.82 in the present study.
Statistical methods
The data were summarized as number, percentage, mean values and standard deviation. The Kolmogorov–Smirnov test and skewness and kurtosis values were used to evaluate the normality of the distribution. The relationship between independent variables and self-efficacy level was evaluated with t-test and one-way ANOVA in independent groups. A multiple regression analysis was performed to identify the determinants of self-efficacy level. The statistical significance was found to be p<0.05.
Ethics approval
This study was approved by the Non-Interventional Clinical Research Ethics Board (2015/33-03) of Selçuk University. Written approval was obtained from the directorate of the hospital and patients gave written consent prior to the research.
Results
Diabetes patients’ mean age was 61.0±10.9 years. Of these patients, 68.1% were female, 79.2% were married, 50% had graduated from primary school, 31% were illiterate (unable to read or write), 67.1% were women performing home duties, and 55.1% had spent a significant part of their lives in a rural village. Patients who had health insurance constituted 95.8%. Of all patients, 82.9% had a regular monthly income and 87.5% considered their economic status to be moderate. Of the patients, 90.7% were part of a nuclear family, and 46.3% lived with their spouses. Half of diabetes patients were obese and 79.6% were not smokers. Half of diabetes patients had first- or second-degree relatives who had been diagnosed with diabetes. Among the patients, 57.9% were using oral antidiabetic medication for treatment, 70.8% had a co-morbid chronic disease, and 69.9% were using medications for other chronic diseases. The most frequently observed chronic disease was hypertension (54.3%). The rate of patients who had received education on diabetes was 65.7%, with 63.9% reporting lack of efficacy in disease management. The average length of time that had passed since the diagnosis of diabetes was 9.1±10.9 years. The average number of medications used was 1.9±0.8, and the average number of doctor visits within the previous year was 3.5±2.5.
Analysis of metabolic parameters indicated an abnormal fasting blood glucose and HbA1c level in 69.9% and 84.4% of the patients, respectively. Cholesterol level was abnormal in 48.5%, low-density lipoprotein level was abnormal in 60.2%, high-density lipoprotein level was not optimum in 55.4%, and triglyceride level was abnormal in 54% of the patients. Diabetes patients’ mean score on the Self-Efficacy Scale for Type 2 Diabetes was 65.4±11.7.
The mean self-efficacy scores were similar for the study groups in terms of marital status, regular monthly income, family type, household, BMI and smoking status (p>0.05). The mean scores of the groups were significantly different in terms of age, education level, occupational status and residence (for the longest period). Males (68.1±10.2), primary school or higher educational institution graduates (67.4±11.4), retired/working patients (68.6±10.4) and those living in a district (67.8±11.1) were found to have a higher mean score (p<0.05) (Table 1).
Diabetes patients’ mean self-efficacy score was not affected by the existence of a diabetic patient in the family or coexistence of another chronic disease. Patients who had received education on diabetes (67.8±11.6), diabetes management (73.7±9.1) and complications (68.5±11.6), and those who did not have diabetes complications (67.8±11.5) were observed to have a higher mean score (p<0.05). Tukey’s test indicated that patients who were taking both oral antidiabetics medication and insulin treatment (68.0±11.5) had a higher mean self-efficacy score than those who were administering insulin (62.7±12.4) or taking oral antidiabetic medication (64.6±11.5) (p<0.05). The mean scores of the groups on the Self-Efficacy Scale for Type 2 Diabetes were found to be similar in terms of type of medical treatment, metabolic control parameters and BMI values (p>0.05) (Table 2). The total score of the scale was not found to be related to the age of the patients with diabetes, the year of diagnosis, the number of medicines and doctor visits within the last year (p>0.05) (Table 3).
The determinants of the self-efficacy score were assessed using multiple regression analysis. The variables that were found to be significant in comparisons were included in the study, and the model was found to be significant (F=14.369, p=0.000). This analysis indicated that using oral antidiabetics or insulin (β= –0.122), lack of education on diabetes complications (β= –0.125), and insufficient diabetes self-management (β= –0.484) reduced the self-efficacy score.
Table 1: Relationship between self-efficacy levels and sociodemographic characteristics of patients with type 2 diabetes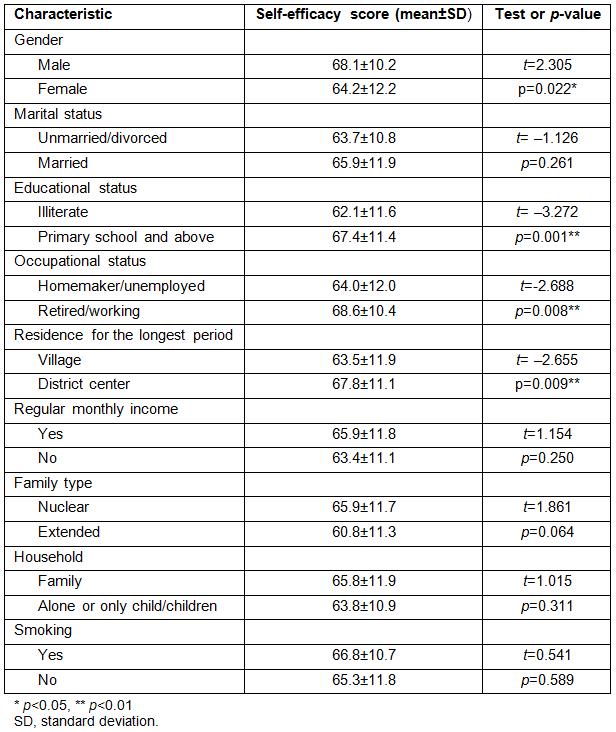
Table 2: Disease characteristics, metabolic control parameters and self-efficacy levels of patients with type 2 diabetes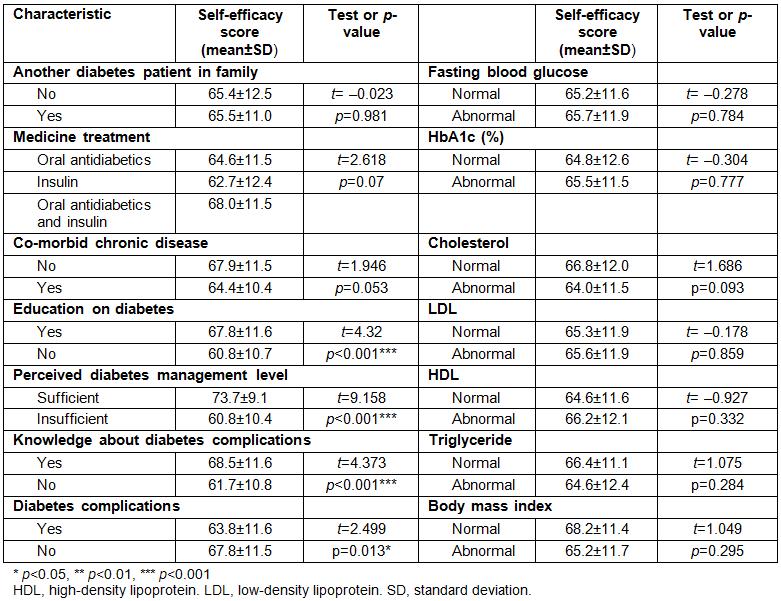
Table 3: Relationship between variables and self-efficacy levels of patients with type 2 diabetes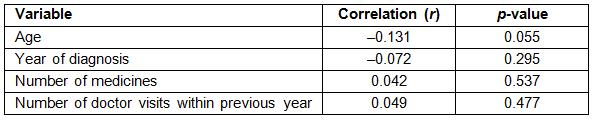
Discussion
Disease characteristics of the patients living in a rural area of Turkey were defined in this study. Patient profile included displaying symptoms for approximately 10 years, using two medications on average, and visiting a doctor 3.5 times on average within the previous year. The majority had a coexistent chronic disease (hypertension in particular) and used medications for this disease. In addition, most of them had abnormal metabolic control value levels. Studies on diabetes management usually addressed patients displaying symptoms for 10 years on average.21,36,38-42 A high value in the time of displaying symptoms is important in terms of enabling a realistic evaluation for the self-efficacy levels of the patients. The literature also suggests that diabetes patients often have a coexistent chronic disease, which supports the findings of the present study.23,24,39 These findings indicate that patients living in rural areas have both poor disease management and more complex care requirements. Studies on diabetes report that metabolic control parameters and BMI values of diabetes patients are above normal levels.11,17,24,27,40-47 Metabolic control parameters reflect patients’ adherence and response to the treatment. Evaluation of these parameters provides information on treatment, care and effectiveness of disease management. This study’s findings indicate that diabetes patients living in rural areas take insufficient measures to control their diabetes, both in medical and lifestyle aspects, and are unsuccessful in disease management. It should be noted that, unlike metabolic control parameters, obesity is considered to be a result of diabetes and a risk factor.
The mean self-efficacy score of participants differed by age, gender, education level, occupational status, and residence (for the longest period) (p<0.05). Females, illiterate homemakers/unemployed patients, and those who had spent their lives in village had lower self-efficacy scores. Previous studies also reported that age,22 educational level,17,27,48,49 and occupational status50 affected self-efficacy levels. Higher self-efficacy levels of males (compared to females) living in rural areas may result from the fact that males have more opportunities for education, a higher level of autonomy, and more access to healthcare personnel. Patients with diabetes are expected to have a high self-efficacy level upon receiving education. In addition, easier access to information, increased awareness, and the ability to take responsibility for their own health problems, aligned with an increased education level, can positively affect patients’ self-efficacy level. The lower self-efficacy level of the unemployed/homemaker patients can be explained by their lower income level and fewer life opportunities. Bohanny et al. also reported that working patients had higher self-efficacy levels.51 The lower self-efficacy scores of the patients living in villages can be explained by the insufficient opportunities for education and income, and disadvantage in terms of personal development opportunities. In addition to those factors, difficulties in access to healthcare services and healthcare personnel play a role, too. Lepard et al. also identified limited healthcare resources and transportation problems in rural areas as factors that affect diabetes control52.
Patients who had received education on diabetes and its complications, who considered their diabetes education to be sufficient and diabetes management to be good, who did not have complications, and who were taking both oral antidiabetics and insulin treatment had higher self-efficacy scores. In the literature, many studies found that receiving education on diabetes positively affected self-efficacy level.17,24-27,53 The present study’s findings indicate that diabetes education is an important variable for self-efficacy level. Additionally, these findings indicate that education enables patients to improve their ability to control their behaviors because they acquire the knowledge and skills for managing their disease, thereby increasing motivation to engage in effective health behaviors. It can be assumed that information positively affects characteristics such as self-esteem and self-confidence. Therefore, it can be said that increased knowledge of the disease leads to increased self-efficacy level. Another important finding is the significant relationship between level of perceived diabetes management and the total score of the self-efficacy scale. Patients who perceived their diabetes management to be good had higher mean scores on the self-efficacy scale. This finding is important because it suggests that self-efficacy level of the illiterate patients who live in rural areas can be evaluated using a single question instead of a scale.
Certain metabolic control parameters were not found to be statistically significant related to the total score of the self-efficacy scale (p>0.05). Although the present study did not find a relationship between these factors, some studies have revealed a relationship between diabetic people’s self-efficacy level and various metabolic control parameters.11,20,21,25,26,54,55 The main reason that a relationship was not found was attributed to the fact that the study group did not include an adequate number of diabetes patients, self-efficacy level was very high and metabolic characteristics were positive. More information can be obtained by determining groups in a rural area with normal and abnormal indicators and comparing these groups with one another.
No significant relationship was found between the total score of the scale and the variables of age, year of diagnosis, number of medicines, and doctor controls in the previous year (p>0.05) (Table 3). In the previous studies on self-efficacy, comparisons between age and self-efficacy levels yielded different results. Some studies demonstrated no relationship,11,17,40 whereas others reported that a relationship existed.15,53 The literature also indicates different results based on the year since diagnosis.11,12,17,18
Multiple regression analysis suggests that using oral antidiabetic medications or insulin (β= –0.122), lack of education on diabetes complications (β= –0.125), and insufficient diabetes self-management (β= –0.484) are determinants of the self-efficacy score (Table 4). Other variables found to be significant in analyses were not identified as determinants. This finding is important because it indicates that self-efficacy level of the patients living in rural areas can be increased regardless of gender and other characteristics if they are provided with sufficient health education including disease management. A systematic review, including studies conducted in rural areas, also revealed that diabetes education provided to the patients living in rural areas positively changed many indicators of diabetes.52
Table 4: Determinant factors of self-efficacy levels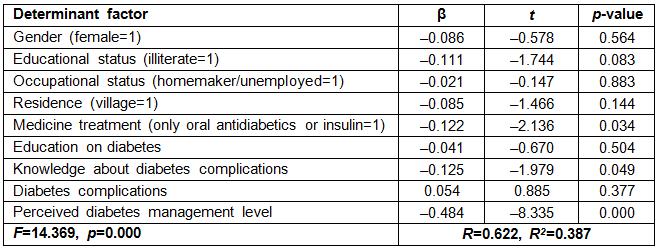
Study strengths
Self-efficacy perception of diabetes patients living in rural areas can be improved regardless of sociodemographic characteristics if patients receive education on the complications of their disease and improve their ability to manage the disease. This study contributes to the literature by suggesting that disease severity perception of patients living in rural areas has an effect on their disease control.
Study limitations
The limitation of this study is that it was conducted at a single center. This study should be conducted in different rural areas and cultures, and the results should be compared with one another. In addition, more studies should be conducted on diabetes in rural areas, and these studies should analyze the factors that affect self-efficacy levels. Risk groups should be determined in terms of self-efficacy levels, and studies should be conducted to analyze the relationship between self-efficacy level for diabetes and metabolic control parameters.
Conclusions
This study demonstrated that diabetes patients living in rural areas had a poor disease management level according to metabolic control parameters and a moderate self-efficacy level for diabetes. Female and unemployed patients, and those who had a low educational level, spent their lives in a village and thus received no education on their disease, constitute a risk group in terms of self-efficacy. Receiving education and taking responsibility regarding the disease process are the most important factors that positively affect self-efficacy level.
This study recommends that a diabetes education program be prepared for diabetes patients living in rural areas. Patients should be monitored and followed more frequently than those living in urban areas. A question on perceived self-efficacy should be used along with a scale during the evaluation of self-efficacy levels of diabetes patients living in rural areas.

