Introduction
The number of cases of diabetes continues to rise globally. Diabetes prevalence in Scotland is 5.3%, with type 2 diabetes accounting for 86.7% of all cases of diabetes in the National Health Service (NHS) Highland health boards area and 85.7% in the Western Isles1. Good management of type 2 diabetes reduces long term complications and increases quality of life, and is most effective when people take responsibility for managing their own condition. Giving people access to knowledge of nutrition, exercise, glucose monitoring and medication that they can apply in their day-to-day lives is a key factor2-5.
All people in Scotland with type 2 diabetes should have access to both standardised education within 6 months of diagnosis and to quality assured structured education programs6. Structured education is increasingly offered in group formats; however, there is little evidence on patient preferences for mode of delivery and access in either urban or remote and rural areas. Group sessions are less feasible in lower-population non-urban environments due to distance, participant numbers and access to appropriately trained healthcare professionals. Face-to-face group education may also be less attractive in small communities, where people tend to have close day-to-day contact. In practice, attendance at such group sessions is low and even when people have agreed to participate, non-attendance is often high. To ensure equity of access and healthcare quality, a solution needs to be developed for provision of structured education to remote and rural communities in Scotland7.
Three levels of education are provided for people with type 2 diabetes in Scotland8,9: at diagnosis (level 1), ongoing throughout life (level 2) and structured group education (level 3). Level 1 is delivered on a one-to-one basis by healthcare professionals (HCPs), while level 2 is delivered either on a one-to-one or group basis as needed or requested by individuals. Level 3 refers to education programs delivered to groups of people and is the focus of this study.
NHS Highland employs the Conversation Maps type 2 diabetes education program10, which uses a series of tabletop images as a facilitation tool for HCPs to engage groups of people in conversations about diabetes. Availability of trained staff for delivery and low attendance are ongoing challenges both in the community and secondary care. Access to the program is currently by invitation to a session held centrally, usually in Inverness or occasionally during monthly meetings of the Fort William area local support group. The geography of the Highlands means that these options are available to only a small proportion of the nearly 16 000 people with type 2 diabetes who are likely to benefit from the program.
While not structured education, the NHS Scotland interactive website MyDiabetesMyWay provides public access to a range of diabetes topics as well as access to blood test results for registered users Scotland-wide11,12. Confirmation of registration requests is required by the individual’s local diabetes care team. In 2015, 2.6% and 4.3% of people with type 2 diabetes in the NHS Highland and the Western Isles respectively were registered with the site1. UK-wide, the charity Diabetes UK also provides online information for people living with type 2 diabetes13.
Centrally provided materials may not allow for differences between urban and rural communities in terms of access to health services, opportunities for physical activity and availability of food choices. Diabetes education programs for rural areas may thus need to consider local context. Understanding current access barriers to education, identifying modes of delivery most likely to be successful in engaging rural dwellers and involving them in the shaping and development of any new system would ensure they feel relevant. This work is part of a study aimed at eliciting the views of people with diabetes and encouraging their active involvement in co-creating an approach to delivering diabetes education appropriate for the Highlands and Islands of Scotland.
Background
The Highland council region in the north of Scotland covers a land mass of 25 657 km2. With a population of 234 110, the population density is 9 people/km214. Twenty one per cent of the population is over the age of 65 years15. The Western Isles (also known as the Outer Hebrides) is an island chain off the western coast of mainland Scotland. Fifteen of the islands are inhabited, with a combined population of 27 40014. The combined land is mass 3071 km2 and the population density is also 9 people/km2. Twenty four per cent of the population is over the age of 65 years15.
Health service delivery in this geographical context is challenging, with limited resources for face-to-face contact with specialist services and long travelling distances for patients and staff. Adult health services in the Highlands and Islands are delivered by two separate health boards: NHS Highland and NHS Western Isles. Approximately 65.5% of the NHS Highland board population live in areas classified as ‘remote and rural’16, while the whole of the Western Isles is classified as either ‘very remote small town’ or ‘very remote rural’16. People with type 2 diabetes in the Highlands and Islands tend to receive their care in the community through the primary care system.
Historically, access to broadband is limited; however, it was expected that 84% of Highlands and Islands premises would have access to high speed fibre network services by the end of 201617. Mobile phone network coverage is patchy, with some areas having little or no coverage.
Methods
The study used a mixed methods approach. Focus groups and questionnaires were used to elicit the views of service users in remote and rural areas of the Scottish Highlands and Islands.
Participants
Eligible participants were defined as having type 2 diabetes, aged 18 years or more and living in a remote or rural area in the Highlands and Islands of Scotland as defined by the Scottish eight-fold urban/rural classification18. Eligible classifications were 4, 5, 7 and 8, ranging from remote small towns (population 3000 to 9999, drive time 30–60 minutes to settlement of 10 000 or more) to very remote rural (population less than 3000, drive time greater than 60 minutes to settlement of 10 000 or more). Accessible rural areas were excluded. Participants either took part in focus groups or completed a questionnaire.
Focus groups
Focus groups were designed to (1) explore service user experiences of the Conversation Maps method of delivery, (2) identify features of delivery that are important to users, (3) explore how the types of technologies already in use are being used and (4) explore how commonly used technologies could deliver structured education. Focus groups were held in Highland and in the Western Isles. Audio recordings of focus groups were made and transcribed. All focus group participants provided written consent for participation and for use of anonymised data.
Questionnaire
A questionnaire was used to elicit the views of a wider range of service users than those who were willing or able to participate in focus groups. The questionnaire was designed to explore perceptions of diabetes knowledge, diabetes education and use of technology, covering similar topics to those explored in focus groups.
Recruitment
Focus groups: A number of different strategies were used for focus group recruitment including handing out study invitation letters and information packs at hospital-based diabetes clinics, sending letters of invitation and information packs to members of local diabetes support groups, distributing posters and flyers to general practitioner surgeries with information about the study, and displaying posters in public places such as post offices, libraries and community centres.
Questionnaire: A total of 321 postal questionnaires were distributed to people with type 2 diabetes in the Highlands who were on the Scottish Diabetes Research Network (SDRN)19 database and whose postcode identified them as living in urban rural classification 4, 5, 7 or 818. This equates to approximately 4% of people with type 2 diabetes living in these areas1,20. There were no people with type 2 diabetes on the SDRN database for the Western Isles. The questionnaire was also sent to people who contacted the study researcher with an interest in taking part in the study but who were either unable or unwilling to take part in focus groups.
Ethics approval
The study was approved by the North of Scotland Research Ethics Committee, reference 12/NS/106.
Results
Focus group participants
Three focus groups were held, two in Fort William (Highland) with six participants and one in the Western Isles with three participants. Focus groups were held over lunchtime in Highland to facilitate participation, and mid-morning in the Western Isles. Two of the participants were currently in employment with the remainder either retired or not in employment. All but one participant had been living with diabetes for more than 5 years. Focus group participants were from remote small towns, remote rural and very remote rural urban/rural classifications (classifications 4, 7 and 8). Where quotes from focus group participants are provided below, AF1, BF1 and so on are used as identifiers.
Recruitment into focus groups took considerably longer than had been anticipated, in spite of the number and range of different approaches that were taken. This may mirror a general reluctance of the wider diabetes community in remote and rural areas to participate in group based education.
Questionnaire respondents
Of the 321 questionnaires distributed, 158 (49.2%) were returned complete. The characteristics of respondents (Table 1) appear to reflect the overall type 2 diabetes population in Scotland. A greater proportion of respondents were male (55.8%), identical to the proportion for Scotland1. The mean age of respondents was 65.9 years, with 57.1% ≥65 years, compared with the Scottish percentage of 57.4%1. The proportion of respondents living with diabetes for >5 years was 73.7%, compared with 66.8% living with the condition for ≥5 years across Scotland1.
All four urban/rural classifications targeted were represented. The small number (7.1%) from classification 5 reflects that fewer people on the SDRN register live in very remote small towns, most likely due to the small number and reducing populations of such towns. Although the study focused on rural areas, with 67.8% of respondents living in remote rural or very remote rural areas, 60.9% of respondents lived within 3.2 km (2 miles) of their GP. Of those living in remote small towns, 87.2% lived within 3.2 km of their GP. The percentage was 72.7% for very remote small towns, 52.7% for remote rural areas and 46.0% for very remote rural areas.
Table 1: Characteristics of questionnaire sample population 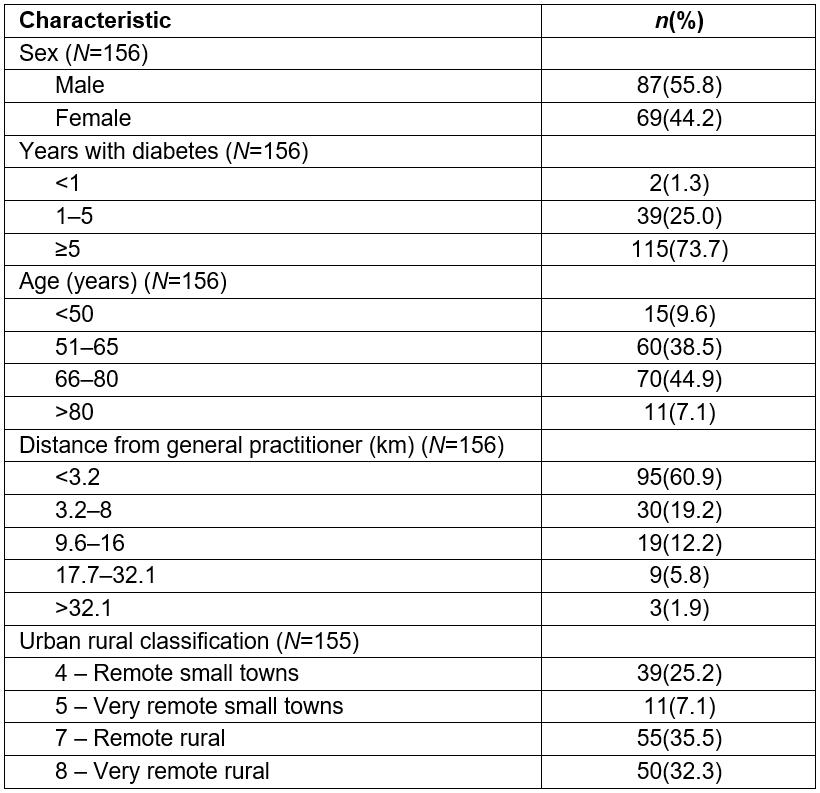
Current access to structured education
Prior experience of structured education by focus group participants was limited, with only four participants in Highland having attended Conversation Maps sessions run at their local support group. Other participants either had no experience or had not heard of Conversation Maps.
Participants had most valued two aspects of the sessions: the opportunity to talk to other people with diabetes about their experiences and delivery of the program by a local HCP.
I was amazed at how little some people knew and how things came up that I hadn’t even read about because people were further on and I hadn’t thought about it so I thought it was good being in a group because if you just done a one-to-one you’re only going to ask questions that you can think of yourself whereas something can crop up from somebody else. (AF3)
A group’s good to get to discuss things. … here we’re talking about things but some people don’t want to say anything about anything. … but does that matter if they’re still learning I mean I could have kept quiet and I could have learned things. (BF1)
The other thing is that people who are quiet. … we did have a chance to write questions and just throw them in the table, there was no names on them so you didn’t know who’d asked them or anything – yeah that was good. (AF2)
Participant use of other educational resources was limited. No participants were aware of or had used MyDiabetesMyWay16. Two participants thought that they might have been told about a website but were not sure which one.
Only one questionnaire respondent (0.7%) had any experience of Conversation Maps. No respondents were aware of or had any experience of other structured education programs. The questionnaire did not specifically ask about MyDiabetesMyWay as a resource.
Barriers to participation
Travel: Although there was a general acceptance by focus group participants that there had to be some travel involved for attendance at group sessions, different views were expressed about the impact this has and the ease with which people can travel. Participants felt that holding sessions in local communities would enable greater participation, but recognised that this was not feasible due to low numbers and staff resources.
The proportion (77.4%) of questionnaire respondents who viewed not having to travel as a benefit of using a technology approach for education delivery suggests that travel was perceived as a barrier.
Timing: People in employment found that holding sessions during working hours was difficult. It was accepted that the date and time of sessions needed to be within the working day of the HCP leading the group. For some participants an overnight stay would be required for attendance if sessions started early in the morning or late in the afternoon.
Being able to learn when they wanted was a preferred option of 72.8% of questionnaire respondents suggesting that timing of sessions is important and may be perceived as a barrier.
Appropriateness of content: One focus group participant, recently diagnosed when they attended a group session, felt uncomfortable with discussions about long term complications. This deterred them from returning. This participant felt strongly that separate sessions should be held for those who have recently been diagnosed. Conversation Maps are designed with different options for people at different stages of diabetes; however, due to the small numbers attending in the Highlands, they are usually delivered to mixed groups.
Lack of confidence in accessing reliable information: Participant use of online educational resources was limited. Although an interest in using the internet to get more information about diabetes was expressed, there was uncertainty about where to find reliable information. With the increasing amount and type of information about diabetes available on the internet, there was a desire for signposting to trusted sources of information.
Only 27% of questionnaire respondents used the internet to look for information about diabetes. Other sources of information were GP/nurse (86.1%), diabetes specialist nurse or dietitian (58.9%) and books/magazines (40.5%), suggesting that these were more trusted than online sources.
Belief that already have the knowledge needed: When questionnaire respondents were asked if they felt they had already learnt enough about their diabetes and how to manage it, 45.6% responded ‘yes’, 29.1% ‘no’ and 25.3% were not sure. However, all focus group participants were interested in learning more.
Desired access
Focus group participants wanted to have timely access to diabetes education and were open to the use of technology. All but one of the participants currently used the internet, and discussions quickly focused on the use of a website.
A website would solve those problems[the need to travel and when sessions are held]. (AF7)
I think if I knew it was a genuine website and it was controlled I’d feel more inclined to use it. (AF5)
Some participants felt that access to a HCP through a live website would be a good option. Other participants felt that this would be restrictive and would take away the benefits of using a website. Frustration that internet access/speeds were unreliable, and an acceptance that this was how it would remain, led to a preference for users to be able to choose when they accessed a website.
You don’t have a specific time, you can do it when you like. Your answers aren’t so quick but I would be happy with using that. (AF7)
One participant suggested the use of short pieces of video with an online forum or chat room facilitated by a HCP for discussing the content. Participants felt that this approach within a website format might work well. Users could watch the videos in their own time and ask questions of each other and the facilitator, with questions and responses visible to all. Participants also felt that using a web-based approach would allow users to be more in control and choose to participate when appropriate to their current needs.
With a chat room … I suppose that … I could go on and ask the questions I want to ask the dietitian. (AF1)
You do feel sometimes like you’ve got nobody to talk to that they don’t realise what you’re going through. (AF6)
Just that you had … somebody that’s been through it like when you come to the group you’re talking to people you know and you’re … picking up wee bits and pieces. (AF2)
Concerns were raised about unsolicited emails if an email address was needed for set-up, logging in and the need to register on a website.
When questionnaire respondents were asked where they would like to access their diabetes education, preference was expressed for either home (69%) or GP practices (65.8%), compared with in the community (20.8%) or from the workplace (7.3%). Access from both home and GP was preferred by 40.5% of respondents.
The internet was used by 68.6% of questionnaire respondents, with 73.6% using a computer for access (Tables 2,3).
Table 2: Current use of digital technology by questionnaire respondents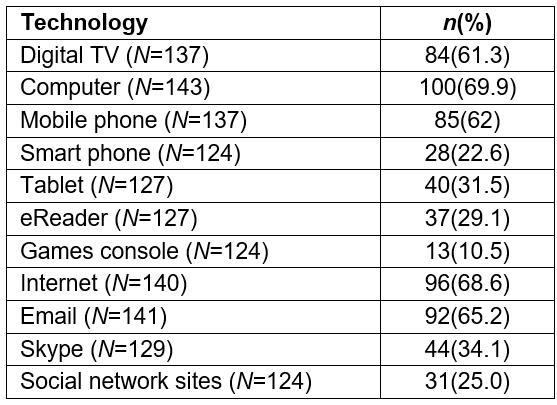
Table 3: Questionnaire respondent mode of accessing the internet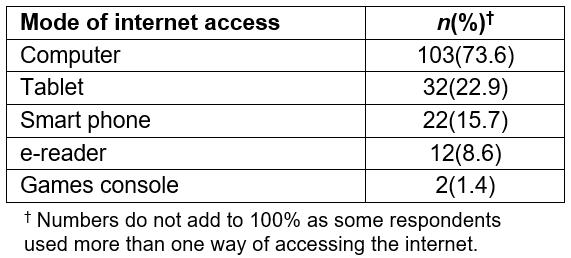
Perceptions of delivery modes
Face-to-face delivery: A face-to-face format was considered to be an important aspect of the current format for focus group participants. However, in the absence of face-to-face contact, as in a website option, focus group participants were comfortable with the use of an online forum or chat room as a substitute. This was viewed as separate to ongoing, one-to-one support from HCPs, which would still be face-to-face. Preference for one-to one sessions by questionnaire respondents was high (62.4%).
Group formats: The group nature of sessions was not viewed as a barrier to engagement by focus group participants. Three of the four users with prior experience felt that the group format had been very useful and they had valued the opportunity to share experiences. However, when questionnaire respondents were asked about face-to-face group sessions, only 27.2% indicated that this would be preferred over a technology approach.
Online formats: Focus group participants felt that they would be more comfortable with using an online system that had a local feel rather than something national such as MyDiabetesMyWay. They felt that this was particularly important when using chat room environments. With a local site, where users were invited to take part by a local HCP, they would know that all the people involved were local to the area, had type 2 diabetes, and were more likely to understand the context and challenges of living in remote and rural Highland.
A website was an acceptable way of accessing diabetes education for 74.6% of questionnaire respondents. Other technology approaches queried (with acceptability) were tablet apps (25.7%), video conferencing (18.3%), smart phone apps (15.5%), interactive TV (15.5%), interactive games (console based) (2.8%) and virtual world environments (1.9%).
Internet users and non-users
Further analysis was carried out to explore differences between internet users and non-users and identify preferences of those who are already engaged with technology.
The mean age of internet users was 63.6 years, and 44.8% were aged more than 65 years, compared with 70.4% and 66.7%, respectively, for non-internet users.
Analysis of data from both internet users and non-users showed that 60% of non-users appear to be happy as they are and don’t want to learn more, compared with 15.8% of internet users; 79.4% of users were comfortable with using technology, compared with 25% of non-users; 54.6% of internet users preferred a digital approach over face-to-face group sessions, compared with 37.5% of non-users; and 58.8% of internet users and 73.1% of non-users would prefer one-to-one (in person) sessions, rather than a digital approach(Table 4). A technology approach would not be intended to replace the current one-to-one support provided at ongoing appointments, so this preference would still be met.
Use of computers and tablets by non-internet users was 4.5% for both devices, and 6.8% used an e-reader. While 30% of non-internet users had a mobile phone, none used a smart phone.
Internet users indicated a preference for being able to learn at their own pace (87.8%), not having to travel (80.6%), learning when they want to (79.8%) and where they want to (76.3%). A preference for face-to-face group sessions was low (23.7%) (Table 4).
Internet user preferences were combined with focus group findings to identify the properties of a technology approach to diabetes education desired by people living in the Highlands and Islands (Table 5).
Table 4: Respondents’ opinions about technology use for diabetes education 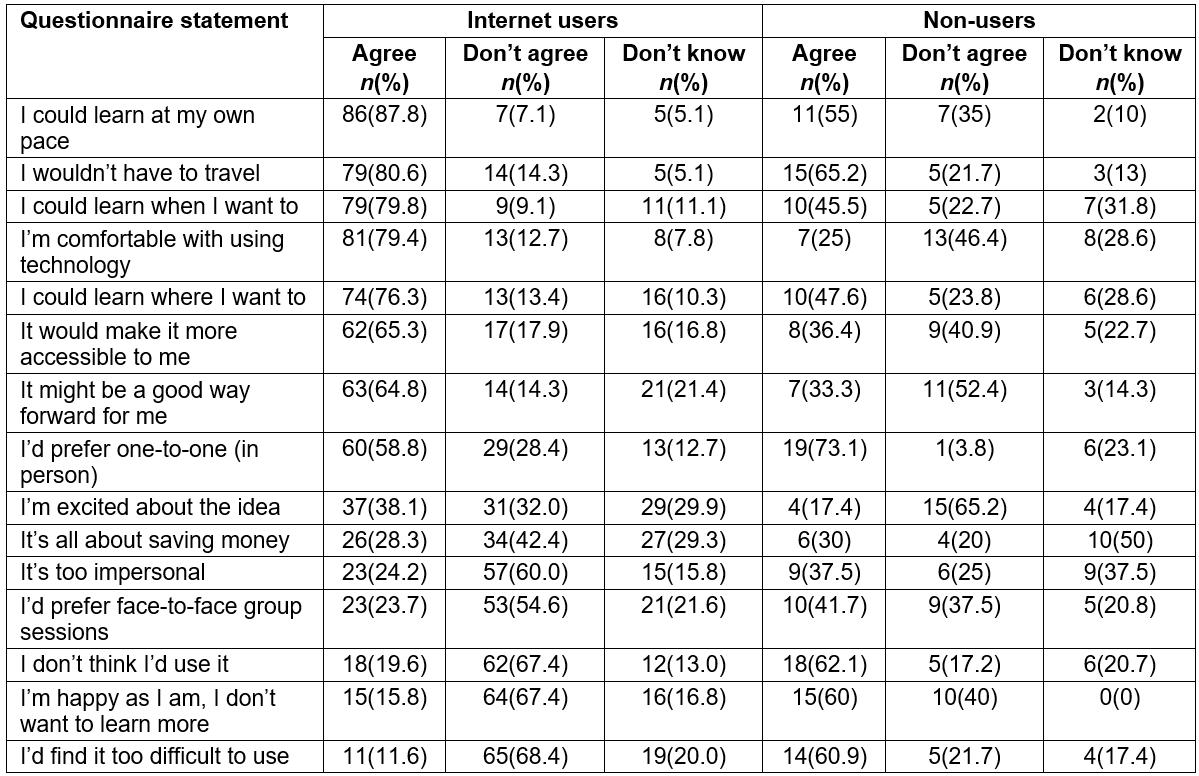
Table 5: Desired properties in the Highlands and Islands of a technology approach to diabetes education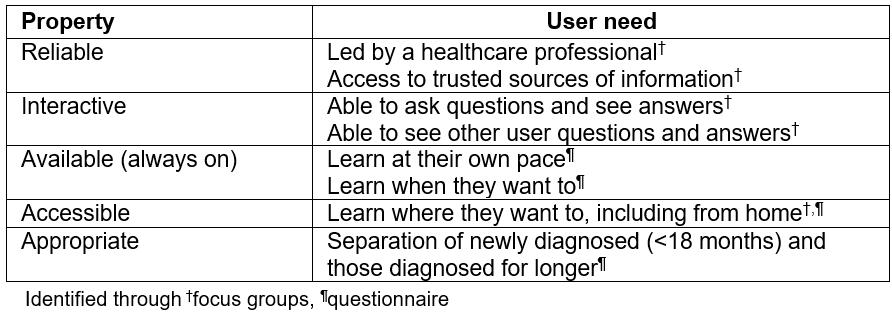
Discussion
This research provides insights into the views and needs of people with type 2 diabetes in the Highlands and Islands on structured education, the properties that are important to them and acceptability and access preferences of a technology approach to provision of education.
Focus group participants were unanimous in thinking that the current group session approach is a better alternative than a technology option, but felt that other issues such as travelling and timing might prevent people from attending. Questionnaire response data indicate that the group setting was less preferable than a technology option to the wider diabetes community surveyed. As the focus group participants were self-selecting, with no difficulty in participating in group sessions, relying on focus groups alone may have biased the results against further exploration of a technology approach.
A previous cross-sectional study of people with type 2 diabetes, at general practices and outpatient clinics across the Netherlands, found that most people with type 2 diabetes preferred not to receive diabetes education by means of a special diabetes course21. These findings are more consistent with the views of the wider type 2 diabetes community in the Highlands who responded by questionnaire.
The low participation in diabetes education found is in keeping with the literature. For example, in a study of US adults with type 2 diabetes, Lopez et al identified low participation in diabetes self-management programs and suggested that this underscores the need for strategies to improve patient engagement22. Although participation in diabetes education programs has been shown to result in better glycaemic control and slower disease progression for people with type 2 diabetes 23, the low uptake may reflect that the formats of such programs are not generally acceptable.
A strong preference by focus group participants for a HCP to be involved in education delivery is consistent with other findings. Gorter et al found that 6 out of 10 participants preferred either a nurse or a doctor to give diabetes education, with more than 80% of participants preferring to receive diabetes education during their regular face-to-face check-ups21. This compares with 62.4% of all questionnaire respondents in the current study who prefer one-to-one sessions.
Online education has become increasingly used and understood for medical students and HCPs. However, there has been less research on the appropriateness or value of online delivery of education for people with diabetes or other chronic diseases. A systematic review identified 20 publications with eligible computer based type 2 diabetes self-management interventions showing small benefits on glycaemic control24. Five of the studies identified were internet based. Peer support, identified as important in the present study’s focus groups, was not an inclusion criterion.
Peer support appears to benefit some adults living with diabetes, but the evidence to date has been too limited and inconsistent to support firm recommendations25. Nineteen of 25 studies included in this systematic review examined type 2 diabetes exclusively25. Two of 14 randomised controlled trials and one of 11 non-randomised controlled trials identified involved peer interaction over the internet. Further investigation was suggested on how to optimise the use and sustain the effectiveness of online peer support in diabetes.
Fisher et al suggested that peer support models must be ‘flexible so they can be tailored to widely varying settings, populations and social, cultural, organizational and economic contexts’26. This is in keeping with the findings of the present study, where participants felt they would have more confidence in the benefits of a website if users and HCPs were local to their area.
Strengths and limitations
The number of focus group participants was less than had been anticipated. As the majority of people with type 2 diabetes receive their care in the community, recruitment relied heavily on responses to posters and fliers. Identifying more personal face-to-face recruitment opportunities, for example at community based clinics, may have increased participant numbers and reduced the recruitment period.
Participation in group sessions was a potential barrier the study explored. Combining focus group and questionnaire findings has avoided potential skewing of results towards acceptance of group sessions if only self-selecting focus group participants had been considered.
Although the number of people surveyed with the questionnaire was small, the demographics of respondents appear to reflect the type 2 diabetes population in Scotland.
The findings are not generalisable to the rural type 2 diabetes community as a whole since the technology approach identified focuses on internet use, inevitably excluding non-internet users. However, it is anticipated that the size of this group will reduce as current internet users age and access to high-speed broadband increases.
Conclusions
People with type 2 diabetes living in remote and rural areas of the Scottish Highlands and Islands who already use the internet are receptive to the use of technology for diabetes education. They are interested in learning more about management of their condition and believe that a technology approach would provide more control over the pace of learning, and where and when this learning could take place.
Combining HCP facilitation of online education with online peer support could fulfil the user needs identified through the study and is likely to assist with better engagement and uptake in this geographically dispersed population.
Further research on the lack of awareness of existing reliable internet-based information, particularly MyDiabetesMyWay and Diabetes UK, may be warranted.
Acknowledgements
The authors are grateful to the Scottish Diabetes Group, who provided funding to support this project. Sincere thanks to those from the type 2 diabetes community in the Highlands and Islands who either gave their time to participate in focus groups or complete questionnaires.
