Introduction
Difficulties recruiting and retaining healthcare providers in rural areas have resulted in a persistent shortage and maldistribution of primary care physicians1. Rural populations are also vulnerable to recent trends seen among medical students, including declining student interest in primary care careers, less medical students expressing interest in rural practice, and an increasing proportion of women medical students who have historically been less likely to provide care in rural areas1,2. In fact, US matriculating medical school classes are now equally balanced between men and women3, making the recruitment of women physicians to rural areas of utmost importance, in order to address the well-documented rural–urban physician disparity4.
Much has been published about physician recruitment to rural areas, with most of this work coming from Australia, Canada, and the USA. Students from rural backgrounds or those with strong ties to rural areas are more likely to choose rural practice sites5-9. Physicians trained in multi-faceted, rurally focused educational programs are more likely to practice in rural communities10-14. Other reported recruitment strategies include financial incentives and professional support15-18. While financial incentives are used most frequently, there is evidence that rural physicians are responsive to other incentives as well, including positive aspects of the work environment, improved work life balance, inter-professional collaboration, and professional autonomy16.
Some studies have reported specific recruitment strategies used to attract women physicians to rural settings. One study of women physicians in the rural Northwest region of the USA reported these women professionals valued flexible schedules, spouse or partner opportunities, role boundaries and professional or personal support networks19. Women physicians, as compared to their male counterparts, are also more likely to value both flexible scheduling and positive interpersonal communication during the recruitment process20,21. While this information begins to describe the recruitment preferences of women physicians, all studies have included relatively small samples of respondents from localized regions of the USA.
Recruitment is important, but retention of those physicians who choose to practice in rural communities is equally important. In the USA, federal and state programs have been established to link obligated service to scholarships and loan repayment, and studies have shown longer rural retention among those physicians receiving financial support17,22. Several factors that support recruitment to rural practice also predict physician retention. These include participation in an educational program designed to produce physicians who choose rural practice, completion of a rural preceptorship, rural background and rural college location23,24. Interestingly, resilience as a personality characteristic has also been shown to contribute to retention of rural physicians25.
Unfortunately, there is some evidence that women in rural practice are less likely to be retained for long careers26. International studies have reported that women in rural practice have unique challenges, including managing both patient and family responsibilities, responding to patients after hours, identifying quality child care, and identifying rewarding work for spouses19,26,27. Because women are also under-represented in the rural medical community, they may find it more difficult to cultivate professional support28. However, no previous studies have specifically focused on the retention of rural women physicians, and none have qualitatively explored the factors that contribute to women’s success in rural family medicine.
In order to effectively recruit women who practice rural medicine and make rural practice a viable and longstanding career option, hospital systems and rural communities need to better understand what makes rural practice desirable (or not) for women physicians. To inform rural stakeholders as well as women physicians contemplating rural practice, the authors qualitatively explored the viewpoints of women family physicians currently practicing in rural communities across the USA, specifically focusing on practice, personal, and community characteristics that contribute to (or detract from) successful long-term rural practice. This report depicts the attributes of practice and employment that impact women physicians’ professional satisfaction and rural longevity. A previous publication described respondents’ personal strategies for work–life balance29.
Methods
Twenty-five women family physicians were recruited electronically through the email contact lists of various rural healthcare organizations, listservs of the Society of Teachers of Family Medicine and the American Academy of Family Physicians, newsletters, and snowball sampling. Participants were included if they were associated with an active rural medical practice and had practice zip codes that corresponded to a Rural-Urban Commuting Area level of seven or higher30. Participants received a US$50 gift card to Amazon.com. The interviews were completed between January and June of 2012.
Interview questions were developed by the research team, which included an experienced qualitative researcher. Each participant was interviewed by a member of the research team in a semi-structured format. The interviewers included two medical students, a Masters-level public health student, two family physicians, and an experienced medical educator, the majority of which were women. All interviewers described themselves to participants as ‘researchers’, and all had some working knowledge of contemporary primary care practice. One family physician investigator had experience in rural practice. Interview questions were pilot-tested with physician colleagues, and refined with feedback. In order to maintain consistency between interviewers, each interviewer used the same script; however, interviewers also asked neutral follow-up questions to solicit further information from the interviewees (eg ‘Tell me more’). Table 1 includes sample interview questions pertinent to rural practice and employment characteristics.
All interviews were recorded and professionally transcribed. The research team analyzed interviews with an immersion and crystallization approach31, conducted regular conference calls to discuss findings, and inductively created a list of consensus codes. Each interview was coded in detail by at least two researchers. NVivo software v9 (QSR International; http://www.qsrinternational.com/nvivo) was used to establish codes and create an audit trail. Codes were cross-checked, and in the few instances where disagreement existed, the team discussed the discrepancy until consensus was reached. Codes were iteratively discussed, and sentinel findings were organized into emergent themes. The emergent themes were critically examined to identify new discourse, and data collection continued until saturation of themes was reached. A large number of themes emerged; this article explores, in particular, the practice and employment characteristics that emerged as important contributors to participants’ professional satisfaction and desire to remain in rural practice.
Table 1: Sample interview questions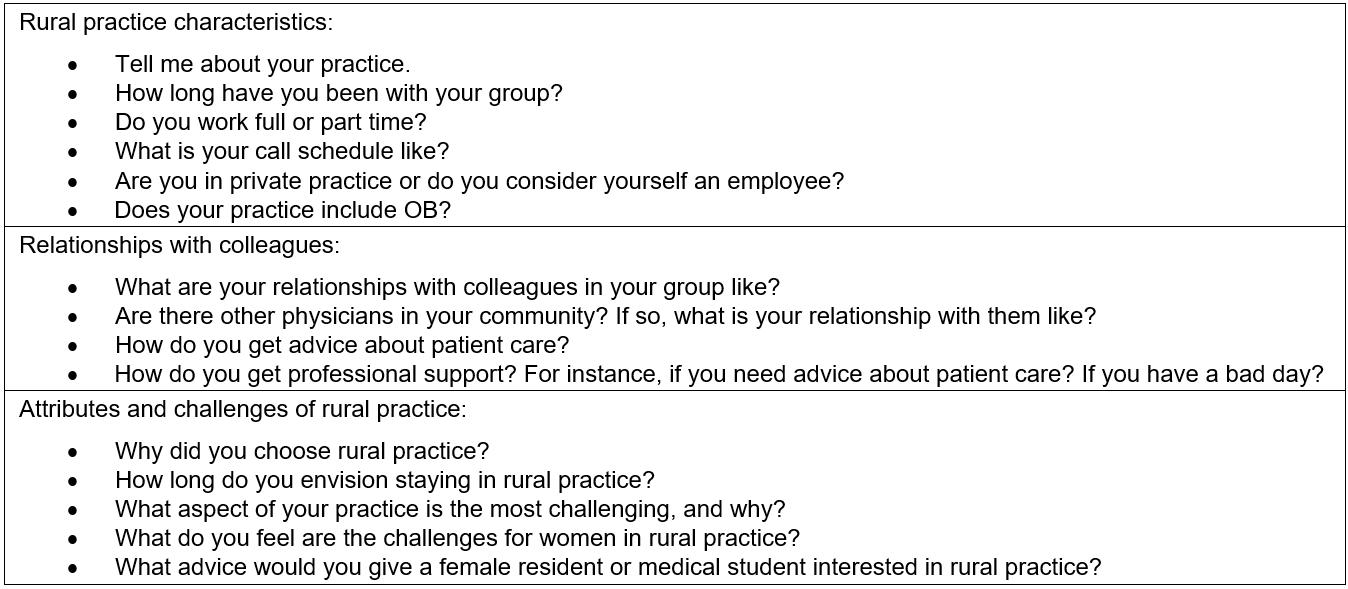
Ethics approval
The study was approved by the Columbia University Institutional Review Board (IRB) (Protocol #IRB-AAAI5401), the Michigan State University IRB, and University of Kentucky Office of Research Integrity.
Results
Participants came from 13 states and represented all regions of the continental USA; a map displaying their states of origin has been published previously29. Table 2 contains participants’ personal characteristics and Table 3 shows practice characteristics. The majority of participants were married or had a domestic partner, had children living in their home, and worked full-time. About half included obstetrics in their scope of practice. Seven of twenty-five (28%) of the participants’ practices were subsidized by the US government, either as federally qualified health centers, rural health clinics, or Indian health service practices. In the USA, federal subsidies are a strategy to support practices in the most underserved communities; subsidies increase payments received for patients with government-sponsored insurance plans, including those with very low income and the elderly.
When discussing rural practices with these physicians, several key themes emerged, the strongest being the importance of professional relationships. These included relationships with colleagues within the practice, other medical professionals in the region, and role models and mentors. In addition, participants valued specific characteristics of rural practice, such as expanded scope of care. As rural physicians, these women also described common difficulties that they have faced in their practices, especially challenges during times of practice transition. Participants described these themes as contributing to, or detracting from, their success and expected longevity in rural practice.
Table 2: Participant demographics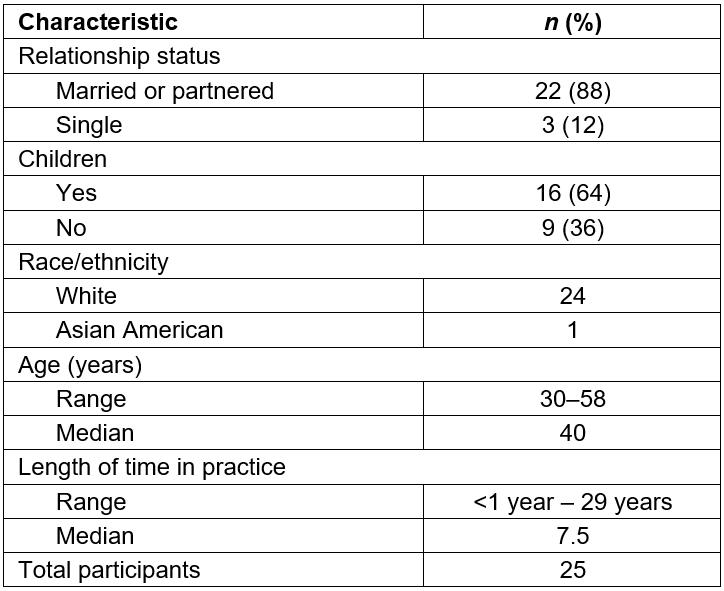
Table 3: Practice characteristics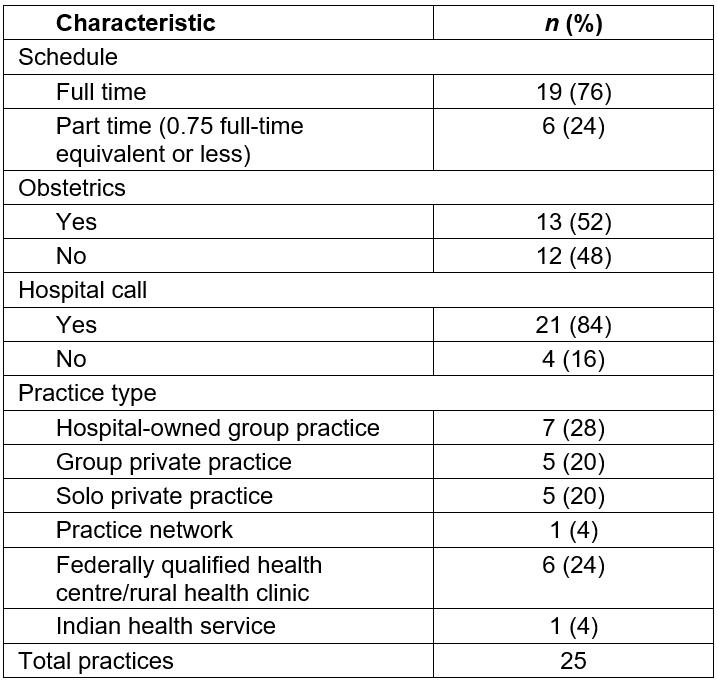
Importance of professional relationships in rural practice
Relationships with colleagues within the practice: Study participants expressed a deep regard for their relationships with colleagues, both those within and outside their own practice. This theme emerged from a large number of interview segments that described how having supportive colleagues drew physicians to the practice and contributed to a healthy workplace environment. With these colleagues, women rural physicians often established effective practice teams so that the demands of patient care were shared equitably. The quality of these relationships promoted a feeling of loyalty to colleagues, such that the interviewees believed they could remain in rural practice indefinitely.
My colleagues are amazing. And especially as being someone young in practice, [my colleagues] were one of the biggest things that drew me to this job. (Participant 23)
And I think that’s just super valuable that we have that relationship here because then if something does come up, we all just try and figure out, ‘Okay, that came up, what are we going to do about it? How are we going to handle it?’ And nobody feels like anybody’s out to get them or game them. (Participant 19)
That's the main reason I stayed. This is just an extraordinary medical staff … The leadership here is just quite unusual … [the leaders are] the ones that pitch in the first and the hardest, and the rest of us just don't mind pitching in … That's the main attraction here. (Participant 8)
Within their practice, this support was most evident when respondents knew they could contact partners for help with difficult patients or circumstances. Often interviewees stated their colleagues were invaluable when family issues arose, call responsibilities became unmanageable, or patient care volume was unusually high.
It didn't matter what time of day or who was on call, if you needed help, you called and your partners came. That’s just the way we work, we have a very collegial working relationship. (Participant 25)
So I think one of the things that I like about them is that everybody has their own things with family, and so we switch call or cover for each other. If my kids are sick or one of the guys has to go to the science fair, for example. (Participant 7)
Several participants stated that it was important to have colleagues who shared their passion for rural medicine and were committed to high-quality patient care. Colleagues who valued providing reliable, unconditional assistance to patients were particularly important. Supportive colleagues reinforced a physician’s commitment and loyalty to her practice over the long term.
It’s the 35th year of the clinic. I’ve been here 26 years ... a very cohesive group of doctors working together to give good care to the community, good care to our patients. (Participant 2)
Well, we want the best outcome for our patients, so our decisions are based on that; decisions we make as a business and decisions we make based on what our patients need for the clinic. (Participant 21)
Some of the respondents spoke about their disappointment and frustration with colleagues in their practice who were not collegial, as evidenced by their unwillingness to share hospital call or participate in practice management tasks. Participants also described instances when collegial support was missing due to conflict, apathy, and avoiding assigned responsibilities, and how this challenged their own commitment to rural medicine.
It’s pretty challenging, there’s lots of conflict in terms of call responsibilities and division of labor, essentially. (Participant 13)
[It’s hard] now that half of the providers are employed and don’t really have any interest in the decision-making part of things … They want to do their work and get their paycheck, and call it a day. (Participant 20)
A lack of support was particularly striking when describing maternity leave policies within small practices. For example, some women were pressured to take very short maternity leaves or to make up call time missed during their maternity leaves.
The big challenge I’m working on right now is maternity leave, and they really don’t want to cover my call, and expect me to make it up, and I find that to be a pretty big challenge. (Participant 14)
Relationships with colleagues outside the practice: Rural women physicians also spoke about the value of good working relationships with physicians outside of their own practice. Such relationships brought about beneficial options for rural physicians, such as coverage for patients during vacations, access to specialty care and the opportunity to share call responsibilities.
I have lots of collegial support from the folks in my community. I have call partners, I have OB [obstetrics] backup, I have good people. (Participant 19)
Both remote and local specialist colleagues were vital for the care of highly complex patients. Typically, rural physicians communicated with these specialists via telephone when assistance was needed. Locally, the degree of support by specialist colleagues could also impact practice scope. Participants described supportive specialists as a resource that allowed them to provide more complex care to patients locally, but also expressed frustration when community specialists interfered with their intended scope of practice.
We have a pretty good working relationship with a lot of different specialists in the area, so if I have a specialty question, I can either call one of the specialists that comes here … or I'll just call [the larger hospital] and talk to one of the specialists. (Participant 7)
If there is a difficult case or we have a question, that there's certain docs in each specialty that I feel comfortable I can call and run the question by them, but without necessarily transferring the patient or having them assume care. (Participant 17)
The obstetricians that were here were so unsupportive of us doing OB that it was going to be a big battle to fight. (Participant 4)
Presence of role models or mentors: New rural women physicians spoke positively about senior colleagues who helped with the transition from residency to practice. While several respondents did not have this type of support, those who did stated that it made a significant difference, especially in the first several months of practice. The participants described these mentors’ willingness to share their expertise when needed.
He really taught me how to run my practice, how to take care of patients, and just all kinds of things … When I came I had never been a solo physician, I had never run my own practice, I had only been employed … I didn’t know things like how to pay my employees, how to make sure I got taxes to the government, or how to track practice management. I didn’t understand anything. And he definitely mentored me for years on how to do that sort of thing until I felt like yes, I know what I’m doing. (Participant 19)
For many, mentoring was synonymous with collegial support. New women physicians often identified and valued senior members of the practice as mentors and advisors about patient care issues, but also as role models and sources of inspiration. Mentors were often male physicians.
He is the best apple ever. He’s been here 18 years. He’s definitely one of my mentors. I still ask him questions about things, and boy, I’m sure the first year I just drove him crazy with, ‘Can you look at this X-ray,’ and ‘What do you think about this case’. And he really taught me how to run my practice, and how to take care of patients, and just all kinds of things. (Participant 19)
[My colleague] took care of myself and my sisters and my mom … he was our doctor all through when we were growing up. And he was who I wanted to be. (Participant 1)
Rural practice characteristics
Although relationships with colleagues were salient, respondents also identified and appreciated the opportunity to practice full-spectrum family medicine in rural practices. A broad scope of practice, including obstetrics and inpatient care, was what drew many of them to rural medicine. Many described this aspect of rural practice as unique and defining.
It's one of the few places you can do full spectrum family medicine. When I tell people what we do here, there are people that just don't believe that we can do all of that. So it's a unique place. (Participant 25)
The nature of rural medicine is that you get to do urgent walk-in care, emergency medicine, inpatient care – the ability to do so much was a great opportunity, a great challenge, especially coming right out of residency. I felt like I was able to broaden my skill set rather than have to narrow it right off the bat. I just get to do a lot of unique and challenging things. (Participant 22)
I wanted to practice medicine like the doctor that I had when I was a kid growing up in a small town. I wanted to practice basically from womb to tomb, cradle to grave medicine. (Participant 3)
Loan repayment also surfaced as a reason for choosing a rural site in which to practice. This was cited by several respondents as a financial advantage.
The first four years that I spent in [rural town] paid back all of my med school loan debt. And that’s just huge. And I definitely think that that impacted where I wound up after med school. I think the fact that I just love practicing in a rural area is why I stayed. (Participant 19)
I think if you know you want to go to a rural area or an under-served area, there are so many ways that you can think outside the box about that and get employment contracts and signing bonuses and loan repayment. If I knew I wanted to do primary care, especially if I knew I wanted to go to an underserved area, I would go into it thinking some of these issues will probably get solved for me. (Participant 4)
The most common advice the interviewees gave for women contemplating rural practice was to carefully explore opportunities prior to relocating. Many respondents had spent a month or more in their rural community during training, and felt this contributed to confidence in their choice of rural practice and commitment to their specific rural site.
Try it out first. Find an opportunity to go [short term] to a practice without committing long term. Filling in for another female physician who needs to go on maternity leave or needs a break is a way of trying it out and seeing if it fits before you commit to a whole patient population who then almost immediately sees you as their doctor and all the responsibilities that come with that. There are a lot of opportunities for people to do that, and I think it's pretty smart to do. (Participant 13)
[Before committing to a practice] I would really try to get a sense of what their group dynamics are like. I would find out what their maternity policy is before you even decide to go there. Look closely at the call requirements and assess whether you think you can manage them. (Participant 14)
Difficulty during practice transitions
The study respondents described many different rural practice models, including private practices, government or hospital-subsidized practices, and solo and group practices. Most were satisfied with their practice model, but some voiced concerns about balancing workload and financial obligations, and some practices experienced financial struggle. These challenges seemed of biggest concern for interviewees during times of practice transition. Some practices experienced difficulty recruiting physicians, which created stress for the practice and the study physicians. For those rural physicians in private practice, recruitment of partners often represented a personal financial burden as well as the stress of balancing an additional workload during the transition.
It’s been a real challenge to keep things going ... if we hire new people, it means we have to cut our salaries. (Participant 20)
All the big hospitals are trying to buy up the little clinics, and just trying to compete in that kind of environment as one of those little clinics who thus far hasn’t sold our soul; trying to figure out how long can we do that. And then the logistics of a partner who's retiring and nobody stepping up to buy his practice, and what that means to me. (Participant 17)
Discussion
Specific practice characteristics and professional relationships impact the success of women physicians in rural practice, both positively and negatively. Rural communities, practices, and hospital systems that understand the needs of these professionals – and work to build professional networks that support their rural practices – may improve both recruitment and retention of women physicians to rural areas.
Consistently the respondents stated that collegial professional relationships, both within and external to a practice, were important to women practicing in rural communities. This finding is consistent with previous studies showing that women physicians value positive relationships during the recruitment process20,21, but also underscores the importance of continued mentorship and collegiality to support rural practice. The importance of professional relationships was much stronger than other characteristics, and was a common thread for rural women physicians of all ages, career stages, and in all types of practices studied. Participants who did not benefit from stable collegial relationships questioned whether they would be able to remain in rural practice. Mentors and colleagues provided emotional support and practical assistance, and could be either men or women.
In a previous publication based on this data and focusing on work–life balance, the authors described the challenges that women physicians encounter in balancing family demands with patient care needs, and their personal strategies for coping with those challenges29. The themes explored in the present article focus on practice characteristics, and illuminate the importance of supportive colleagues in providing a sense of security, so that during times of increased workload or personal demands women in rural medicine have support from their practice partners. Those in cohesive within-practice and between-practice relationships describe loyalty to their colleagues, as well as to their communities. It is not surprising that participants without this cohesiveness felt the absence most acutely during one of the most stressful periods of many women’s’ lives – the weeks after they give birth. Previous researchers have described how an adequate supply of physicians, with a collaborative working dynamic, is essential to physician retention in rural communities6,32,33. In the present study, the authors affirm that this collaboration is also essential for women in rural primary care; previous studies have typically included mostly male physicians. Research in Australia has shown that women in rural practice, compared to men, are more likely to be in group practices, rather than solo practice26; this may be a response to this need for professional support.
Colleagues with a shared vision for the practice also reinforced the interviewees’ motivation to continue to practice rural medicine. Many women described ways that mentors and partners inspired them, and described a shared vision for the practice’s role in the community. In his theoretical model of physicians’ integration to rural places, Cutchin describes the importance of physician-to-physician mentorship, shared physician ideologies (particularly within practice groups), and a sense of unity, typically focused on community service31,34. Notably, women physicians indicated that male physician partners could be role models and mentors, suggesting that this tradition of inter-generational mentorship – often beginning in medical school or residency – has continued, even as the proportion of women in rural medicine has increased1.
Another important finding of the present study was the frustration encountered by these physicians during times of practice transition. This may be a reflection of the rural physician shortage, which makes recruitment or temporary coverage more difficult, and may support the finding that resilience is an important personality characteristic for rural physicians25. Practice transitions, whether temporary (maternity leaves) or more permanent (shifts in ownership structure or retirement), may be a high-risk time for burnout for all physicians in a rural practice. Rural physicians may benefit from increased professional, personal, and community support during these times.
Conclusions
Although much has been published about predictors of rural practice and the impact of educational programs on rural retention and recruitment of physicians, fewer studies have focused on practical strategies that rural communities or practices could employ to foster the satisfaction of their own physicians. These findings uncover potential strategies for these stakeholders. Recruitment efforts could include, at the onset, assurances of viable and supportive policies for maternity leave, practice coverage, and on-call obligations, as well as an identified practice mentor. Practices or health systems having difficulty with recruitment or retention might consider examining their culture and policies around interprofessional support, both within and between practices. Rural practices and communities should anticipate and acknowledge the stress that practice transitions will place on existing physicians, and explore tactics to mitigate the financial and personal burden these present.
The findings reported here may also be helpful for women medical students or residents contemplating rural practice. Knowing that practicing women family physicians place high value on collegial relationships will underscore the importance of identifying this support in any potential practice. Understanding office or system policies for support during leaves, times of practice transition, and after-hours coverage is also important when contemplating rural practice options.
This study was limited by the lack of racial or ethnic diversity in the sample. A more diverse sample may have uncovered additional challenges seen by under-represented minority women in rural medicine. Although the sample was not racially and ethnically diverse, it did include participants from geographically disperse regions, with a broad age range, a wide range of length of time in practice, and with varied practice types. Future work could further explore the experiences of other subpopulations.
Rural practice offers many unique joys and challenges. Understanding practice characteristics important to successful rural women physicians will help communities, practices, and physicians-in-training develop and evaluate opportunities that will best contribute to successful, long-term rural practice careers.




