Introduction
The ongoing crisis in primary care in the USA is attributed to two main concerns: (1) medical students are increasingly choosing specialties other than primary care, and (2) medical knowledge is expanding faster than ever before, making it difficult for busy primary care providers (PCPs) to keep up.1,2 Maintaining a working level of expertise in dermatology is of particular concern for PCPs, recognizing that 36.5% of patients seeking primary care also had at least one skin problem, making dermatologic conditions highly common among primary care patients.3
For rural patients, primary care may be the only access to healthcare services. Studies on access to care found that patients would likely not travel to receive care if they had to travel more than about 30 km (20 miles), even if the care was free.4,5 In addition, available timely evidence-based care in the USA is inadequate; it is estimated that patients receive recommended care only 50% of the time.2,6-8. For patients with skin disease, the current maldistribution of the dermatology workforce further aggravates the problem of access, as does the fact that a growing number of dermatologists focus on surgical procedures rather than medical dermatology care.9,10
Objective
The objective of this observational study was to identify practical applications and utilization of telemedicine videoconferencing technology designed to deliver a guided practice model for treatment and management of various skin conditions. Dermatology Show-Me Dermatology Extension for Community Healthcare Outcomes (ECHO) is a telementoring project at the University of Missouri, created to improve access to dermatology expertise by educating participating PCPs in best practices in dermatology, thus addressing the shortage of dermatologists in Missouri.
Methods
Project ECHO
Over the past two decades, teledermatology has become one of the major tools used to bridge the gap of medical expertise and access in the care of skin disease by using innovative technologies for both live interactive and store-and-forward applications. While policymakers and healthcare leaders recognize the value of applications such as teledermatology, more work is needed to remove barriers to utilization that still exist, such as reimbursement, legal and regulatory challenges.11 One groundbreaking approach that has successfully overcome these barriers, while at the same time improving patient outcomes, is Project ECHO.
Project ECHO was initially developed in 2003 at the University of New Mexico Health Sciences Center to help with inadequate access to care for rural patients in management of chronic infections due to hepatitis C.2,6,7 Rural PCPs often struggle to keep up with the most current evidence-based medical practices typically exhibited at large urban academic centers, mostly due to geographical limitations.2 Project ECHO uses telemedicine technologies to provide case-based learning opportunities, with the aim of overcoming geographic restrictions.2,6,7 It facilitates the teaching of current evidence-based care guidelines, and creates a strong peer-learning environment.2,6,7
The initial ECHO model for management of hepatitis C showed that serious adverse events occurred less commonly in patients treated at ECHO sites compared with patients treated at the academic medical center (6.9% vs 13.7% respectively).7 These somewhat surprising yet important findings tend to validate observations that health care is often best when delivered locally or regionally. Local providers recognize the available resources for their patients, may understand the local culture better, and have established provider–patient relationships, all of which are important for increasing patient compliance and reducing adverse reactions.7
Project ECHO has since expanded to involve many other medical disciplines, including the treatment of complex regional pain syndrome, HIV/AIDS, substance use disorder, endocrinology, autism, and many other common, complex, costly, and chronic conditions in 30 US states and 15 countries.2,6,7
Dermatology ECHO
The Department of Dermatology at the University of Missouri (MU Derm) has been an innovative leader in teledermatology, offering two weekly clinics for patients at more than 80 telehealth sites in 50 Missouri counties since 1994. In 2015, MU Derm, supported by the Missouri Telehealth Network (MTN), implemented the first non-military Dermatology ECHO in the United States as part of a larger ECHO implementation, Show-Me ECHO.
The MTN provides operational, technical, and recruitment support for both telehealth clinics and Show-Me ECHO. With the mission of increasing access to care for rural and underserved patients in Missouri, MTN delivers expertise in legal, regulatory, and policy changes.12 The MTN also supports rural Missouri providers connecting via telehealth to participate in various departmental grand rounds and other educational opportunities at MU for which they receive continuing medical education (CME) credits at no cost.12 The MTN ensures Dermatology ECHO complies with the fidelity to the ECHO model. This means that all presented cases are de-identified, all participants are introduced before they speak, and the hub team ensures case presentations and didactics stay within allocated time.
The MTN and MU Derm partnered with Missouri primary care clinics in 2015 to start the Dermatology ECHO in order to address the need to facilitate management of various dermatological conditions by PCPs at distant sites across Missouri. Over a period of 6 months, they worked closely together on identifying and recruiting the hub team members, signing PCPs from rural and underserved areas to participate in upcoming sessions, surveying PCPs on needs and expectations, and developing a didactic curriculum.
The Dermatology ECHO hub team consists of seven providers: two general dermatologists, two pediatric dermatologists, a dermatopathologist, a clinical psychologist and an advanced practice nurse (Fig1). They meet with 7–15 PCPs once a week during an hour-long ECHO session, every Friday between 12 and 1pm (Fig2). There is no limitation on the number of cases each PCP can present, and typically each ECHO session consists of three to five de-identified case presentations. Occasionally, more than five cases are received at a time, in which case the hub team prioritizes and decides which cases will be discussed the following week and which cases need to be discussed immediately. Case presentations are discussed with the Dermatology ECHO hub team, which then gives the diagnosis and recommendations for further management of each case. Each case presentation and subsequent discussion and telementoring takes 5–15 minutes, depending on complexity and intricacies of the diagnosis. In addition to case presentations, each ECHO session also consists of a brief 10-minute CME-approved didactic presentation (Fig3).
Dermatology ECHO uses Zoom software to connect participating providers and the hub team during the video-guided practice and telementoring session.13 Participating providers connect using desktop computers or mobile devices. The PCPs take still images of the affected area using the ECHO tele Missouri Dermatology Image Database mobile app, specifically developed at MU for MU teledermatology clinics.14 It allows PCPs to take photos that are automatically downloaded to a secure dermatology image database at MU, which can then be accessed by consulting dermatologists.14 The app has a built-in feature that deletes images from the far-site mobile device once the PCP has closed the app, without storing them on the device itself.14 Automatic deletion is essential for maintaining confidentiality, noting that previous studies of store-and-forward telemedicine found that transmitting sites sometimes forget to manually delete patient photos from devices.14 The TeleMDID app has been adapted for the Dermatology ECHO project, and the ECHO TeleMDID app now allows providers to share patient photos in a de-identified manner using only the patient ECHO ID numbers and no other patient identifiers.14 The Dermatology ECHO hub team meets at a conference room in MU Derm that is equipped with a smart TV that has Zoom access and a high definition camera.
Prior to Dermatology ECHO implementation, many rural and underserved patients had no or only limited access to dermatologists. Most dermatologists in Missouri practice in four major urban areas – St Louis, Kansas City, Columbia, and Springfield. Patients from other areas, such as an extremely remote south-eastern area of the state, may have up to a 5-hour one-way drive to see a specialist, which they are often not able to make due to financial hardships, lack of transportation means, or work constraints. In addition, some of the skin conditions they may encounter have a complexity that most PCPs are not adequately equipped to treat. Forgoing treatment, or receiving an incorrect diagnoses and treatment, are common occurrences resulting in high morbidity and increased healthcare costs.
Before Dermatology ECHO implementation, numerous patients have been seen repeatedly by their PCP for the same condition, often taking various medications and undergoing unnecessary ancillary testing, before being presented to the Dermatology ECHO team. A case is offered to illustrate.
 Figure 1: The Dermatology ECHO multidisciplinary hub team.
Figure 1: The Dermatology ECHO multidisciplinary hub team.
 Figure 2: A telementoring ECHO session.
Figure 2: A telementoring ECHO session.
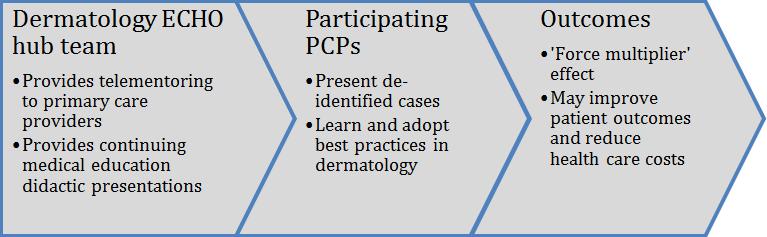 Figure 3: Dermatology ECHO structure.
Figure 3: Dermatology ECHO structure.
Results
Atypical mycobacteria, such as M. chelonae, can be difficult to identify clinically. The clinical diagnosis of an atypical Mycobacterium infection is especially difficult for PCPs, who do not often see, or receive specific training to be able to recognize, this type of skin infection. This is a challenging diagnosis, since there can be a wide spectrum of presentations, from a non-healing ulcer to a cellulitis-like infection. This may lead to misdiagnosis and improper treatment with antibiotics that are ineffective against the infection. Improper treatment leads to a long-lasting infection, increased patient morbidity, and excessive healthcare costs, as in the following case report.
A 69-year-old Caucasian woman who had been spurred by a rooster initially presented to a rural medical clinic after 2 days with a red plaque on her right lower extremity proximal to the medial malleolus. She was prescribed cephalexin 500 mg quater in die for 10 days for presumptive cellulitis. When the patient presented to her PCP for follow-up she was found to have a 1 cm eschar over her right posterior leg with surrounding erythema. The patient noted improvement since the initial injury, but complained of residual pruritus. Tetanus, diphtheria, and pertussis toxoid were given and the patient was instructed to remain off antibiotics.
One month later the patient again visited her PCP. At that time, physical exam revealed a 2.5–3 cm erythematous plaque over the medial right lower leg, with central scabbing, tenderness, and fluctuance. The abscess was drained, packed with gauze, and the patient was prescribed levofloxacin 500 mg daily with instruction to repack daily. A 3-day follow-up was scheduled.
At the third visit a wound culture was found to be negative and the patient seemed improved as the wound now had moderate erythema and purulent exudate, but no surrounding fluctuance and only minimal tenderness. The patient was instructed to repack daily for 5 days and return for follow-up in 1 month.
At the fourth visit the patient noted that the wound improved with packing initially but redness and swelling returned. On exam the wound had 3–4 cm of indurated erythema with no fluctuance, but had become scaly. Ciprofloxacin 500 mg bis in die (BID) and metronidazole 500 mg BID were given for another 7 days for presumptive cellulitis.
At the patient’s fifth visit a week later the lesion was red, indurated, without fluctuance and minimally tender, but there was significant induration. The patient was prescribed amoxicillin/clavulanate 875–125 mg BID for 7 days. In addition, complete blood count (CBC), C-reactive protein (CRP), erythrocyte sedimentation rate (ESR), and second wound culture were ordered. CBC and ESR were normal, and CRP was elevated at 9.09 mg/L. A second wound culture was negative. Due to the ‘poor response’ to treatment, the case was scheduled to be presented at the Dermatology ECHO session. This case was discussed during an ECHO session once, and the hub team requested a follow-up case presentation 4 weeks after initial case presentation. Table 1 summarizes her PCP visits.
At the case session, the still images of the lesion were shared using the teleMDID app. The patient’s past medical history and current treatment plan were discussed, and the most recent digital images of the affected area were shared. Based on history, presentation, and photographs, the patient was diagnosed as having an atypical Mycobacterium skin infection by the Dermatology ECHO hub team. The diagnosis was specified on mycobacterial culture as M. chelonae. During this session, the dermatologists recommended that the patient take azithromycin 250 mg daily until her next follow-up appointment and apply a heating pad to the infection site 2–3 hours per day. Within 1 month the patient had dramatic improvement using heat and azithromycin as recommended (Fig4).
Table 1: Summary of patient’s visits to primary care provider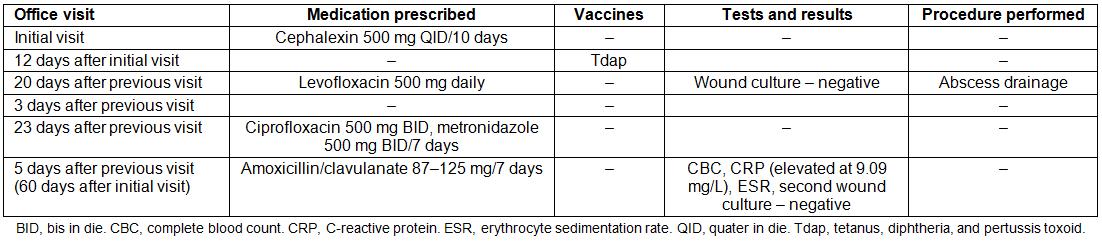
 Figure 4: Left: Patient’s lesion 2 months (left) after the patient was spurred by the rooster, during visit number 6, and 1 one month (right) after case presentation in the Dermatology ECHO clinic, when the more appropriate treatment was suggested.
Figure 4: Left: Patient’s lesion 2 months (left) after the patient was spurred by the rooster, during visit number 6, and 1 one month (right) after case presentation in the Dermatology ECHO clinic, when the more appropriate treatment was suggested.
Discussion
Atypical mycobacteria, such as M. chelonae, can be difficult to identify both clinically and histologically.15,16 As in this case, PCPs not trained in dermatology may have difficulty identifying and treating rare conditions, leading to excesses in treatment, testing, and office visits.15 Reliable access to specialty expertise and education of PCPs who participate in the Dermatology ECHO can lead to high-value dermatology care by improving quality and controlling unnecessary cost.15,16
Like most states, Missouri has many rural communities that are separated from the few large academic centers. Many rural patients find it difficult to seek care in urban academic centers due to financial hardships, family obligations, or lack of transportation.
The Dermatology ECHO was initiated to help PCPs learn more about dermatology and provide better care for their patients locally. Weekly hour-long videoconferencing sessions occur where PCPs across the state present challenging dermatologic cases from their practice to the dermatology hub team of experts. History, presentation, workup, diagnosis, and treatment recommendations are discussed for these specific cases. Patient cases discussed during ECHO sessions are followed, and treatment outcomes are discussed at subsequent sessions.
In this report, the unusual case of a 69-year-old Caucasian woman with an M. chelonae infection of the leg was presented. Dramatic improvement in this patient’s condition is directly attributed to her PCP’s participation in a Dermatology ECHO teleconference to help guide diagnosis and treatment. In addition, participating providers at other sites gained considerably from the case discussion with the possibility that their future patients will likewise be positively impacted by the knowledge gained and expertise offered. This force-multiplier of Project ECHO is estimated to ‘exponentially increase workforce capacity’.6
Another illustration of the impact of the Dermatology ECHO project is the following comment, emailed by a participating PCP to the Dermatology ECHO hub team:
We changed our practice based on the derm ECHOs and started having men over 50 take off their shirts for their annual exams.
A couple of weeks ago [I] found an 'ugly duckling' on the back of a 61yo. This week I excised it and the path came back today: early in-situ melanoma.
I just thought I’d say thanks!
Conclusions
With the development of advanced telemedicine videoconferencing technologies, the age-old question about whether providers, other than board-certified dermatologists, should diagnose and treat skin conditions may be less pressing. The value of having specialists readily available is not debatable. Compared to PCPs, dermatologists have much greater accuracy in diagnosing skin lesions and are far superior at detecting melanoma.15 Knowing this, referrals to dermatology are frequent when the service is available. This, combined with the maldistribution and shortage of dermatologists, results in long delays in referral access. The August 2016 issue of Dermatology World reported that one in three physicians (32%) report having difficulty referring patients to dermatologists, but 84% of those surveyed still think it is important for their patients to have access to dermatologists.16
The American Academy of Dermatology (AAD) Special Positioning Work Group (SPWG) recently specified three core areas of impact for their specialty: (1) treating serious skin conditions that affect millions of patients, (2) using a team-based approach, and (3) adopting innovative initiatives such as teledermatology to increase access and reduce health disparities.17 Ongoing efforts are needed to close the urban–rural healthcare divide and improve access to evidence-based guidelines. The campaign by the AAD to improve access has a strong foundation on which to build a robust platform for comprehensive dermatology care and is consistent with the principles of Project ECHO.17-19
In addition, the SPWG found that non-dermatologists view dermatologists as ‘smart’, ‘thorough’, and ‘patient-friendly’.9 These perceptions further support the success of the first Dermatology ECHO project and facilitate recruitment efforts. More work is needed to educate PCPs about the Dermatology ECHO program and an in-depth outreach and recruitment campaign by MU Derm and MTN is underway.
The efficacy of the ECHO model in improving the health status of rural communities has been established in the literature.7 The case study presented here is one example of the effectiveness and benefits of the Dermatology ECHO Project at MU. The Dermatology ECHO project also aligns with the SPWG core areas by adopting innovative telemedicine technologies to engage a multidisciplinary team that uses the force-multiplier approach to reach a significant number of patients who would not otherwise receive adequate dermatology care.
Future investigation will assess pre- and post-Dermatology ECHO treatment outcomes for common dermatological diseases as well as pre- and post-participation referral rates to dermatology specialty clinics for specific conditions.

