Introduction
The growth in the number and intensity of disasters has drawn global attention to human, material and environmental destruction and the related social and economic consequences. Hydrological disasters (floods and wet mass movements) made up the largest share of natural disasters in 2013, affected 32 million people and accounted for 46.5% of the total deaths1. In Brazil, this situation has become worrying, as the country has experienced many floods and slides2.
Although the current global rural population of approximately 3.4 billion is expected to decline to 3.2 billion by 20503, there is growing concern regarding their health conditions because, in the rural context, natural resources are decreasing, poverty is common and access to healthcare services is precarious. In Brazil, the unexpected transition after natural disasters by flood has impacted family routines and resulted in difficulty accessing public health services caused by lack of transportation due to poor road conditions4. This context demands actions to mitigate these consequences with measures to preserve the environment and prepare health professional teams.
When this type of disaster occurs in rural communities, the demand for health services increases, especially in primary health care (PHC)5. PHC services play an important role in the management of disasters caused by floods, especially in the response and recovery phases. These responses depend on the synchronized actions undertaken by a multidisciplinary team of whom a series of competencies are expected in order to ensure quality and priority care6. Competence in this context is related to performance when facing situations of unpredictability and complexity and solving problems in a specific cultural context as they arise7.
The study of health professionals’ performance in certain types of natural disasters has contributed to the identification of these competencies. The professional emergency preparedness skills among the health professionals who worked during hurricanes Katrina and Rita8 and the skills, knowledge and attitudes required of the nurses who worked after earthquake-type disasters9 have been studied.
Competencies for nurses and health professionals practicing in rural areas have been studied. Excellence in clinical decision making and functioning in a more independent, generalized fashion were identified as important components of good nursing practice in critical access hospitals10. Public health nurses’ level of competency has been assessed in a rural area11. In Brazil, a set of competencies for a rural medical education program has been developed12.
A significant number of disaster competencies have been published over the past decade for different professional sectors, with nursing being the most targeted discipline13. This article describes the results of an investigation developed to identify PHC nurses’ competencies when responding to hydrological disasters in rural areas.
Methods
Study design
A descriptive, exploratory, qualitative study was developed in 10 rural municipalities located on the coast of the Uruguay River in Rio Grande do Sul, Brazil, an area frequently affected by storms and floods.
The critical incidents technique was adopted14,15, as it has been successfully used in research to understand the activities of various professional groups and to describe the roles and functions of health professionals such as nurses14.
Selection of participants
The method was chosen for its properties of providing rich qualitative content by reflections on situations and actions in the profession14. Participants were public health nurses with a direct or indirect role in providing care to the rural population in the response and recovery phases of the 2014 and 2015 hydrological disasters. The sample was selected intentionally in order to obtain representation from different locations and experiences.
Data collection
Data were collected through semi-structured interviews with 20 nurses15. This number was considered sufficient based on the theoretical saturation of the data and the objectives of the study.
Nurses were asked to provide a detailed report of a situation when health care was necessary after the floods of 2014 and 2015, specifying exactly what the situation was, who was involved in it, what was done and what occurred after the response. A pre-test of the interview script was carried out with two PHC nurses.
Data analysis
The interviews were initially recorded, transcribed in full and thoroughly reviewed by the first and last authors. Data were organized to identify the significant narratives, groups and categories14. Critical requirements of the nurses were derived from the situations, critical behaviors and consequences identified.
The critical behaviors and requirements provided the necessary criteria to build the competencies. For each competency statement, the following format criteria was followed: every competency title should be consistent with a verb, a noun, and could include one or more qualifiers. Competencies were classified according to five frameworks6,7,16-18.
Ethics approval
Human research ethics approval number 1.455.248 was obtained from the Institutional Review Board of the Universidade Federal do Rio Grande do Sul. Written informed consent was obtained from all subjects.
Results
Sample characteristics
Of the practicing nurses (n=20), 14 worked as PHC nurses, and the others held positions as coordinator of health programs (n=3), were responsible for health surveillance (n=2) and provided psychosocial services (n=1). The nurses had been employed in their current positions for up to 5 years (n=7), 6–10 years (n=6) or more than 11 years (n=7). Their educational backgrounds included specializations in public health (n=7), PHC (n=5) and emergency care (n=2). Most of the nurses (n=16) referred to previous experiences in disaster situations.
Primary health care nurses’ competencies
Within the critical incidents (n=84), 78 situations, 8 behaviors, 10 consequences to the population and 9 consequences to the nurses were identified. These incidents and the critical requirements supported the development of 30 competencies, which were classified into eight domains as summarized in Table 1.
The domain of leadership and management included competencies that contribute to the articulation and integration of health services and organizations. In this process, an important step is planning, which affects nursing behavior, because it needs continuous updating during disaster response and recovery.
We tried to plan, but when we got there, sometimes we were faced with a situation that our planning did not take into account. So we had to be planning our action all the time. (nurse 17)
Provision of supplies was identified as a need by nurses considering some situations that resulted from the disaster.
And then we even took the material to make a bandage and had, because when we took it one helped the other, you know? [...] took a lot of places and there was a bandage, a referral to take the [vaccine], tetanus, who had been cut. (nurse 8)
Many people had to rush out of their homes and forgot or lost prescriptions and chronic medications. The nurses showed an interest in ensuring that these people had their medications and used them appropriately.
She did not take her medication when she left the house and could not go back there to get them. (nurse 1)
The inclusion of additional personnel created new demands. Volunteer participation was described as an immediate action in the population affected by the flood and in the planning meetings.
All this work was done and it was not only the professionals who did it, because as we did the planning meetings in the morning and in the afternoon, we guided all those who were working, all the volunteers who were working at that time. Then, we would advise them how to proceed, how to act. (nurse 1)
Nurses’ behaviors included conducting a risk assessment with community health agents, who are the professionals in permanent contact with the community. Mapping of risk areas included the identification of vulnerable populations such as pregnant women.
Then, we already knew where the pregnant women were, we already knew where the hypertensive patients were, where the older ones were, the more vulnerable patients. (nurse 1)
The community health nurse’s most unique challenge is building a network of relationships and partnerships with a variety of relevant groups, communities and organizations.
A great emphasis was placed on teamwork. Some interviewees recognized the importance of the nurses’ behavior when managing and organizing the teamwork process during the post-disaster flood response and recovery phases.
Look, I think a team like that is fundamental at those times. Team is everything. We have a very good team here. Nutritionist, psychologist. So, we always tried to work together; we tried to help in the best way possible. (nurse 11)
Health care presupposes prevention, promotion, protection and rehabilitation practice. In disaster situations, a new scenario is presented for professionals who have to work in different locations.
Sometimes we would go to the shelters where there were more people. We would see patients, advise them in a small corner, check their vital signs and refer them to the unit. I had a little pad for that. (nurse 19)
Community oriented competencies were extracted from situations using the perceived behavior of the nurses, whose commitment to the community and their needs were assessed by the knowledge of the community they served.
And this is one of the things that help you to see just how important it is to know the area where you are working. We already knew where the pregnant women were, we already knew where the hypertensive people were, where the older and most vulnerable people were as well as the kind people who directed them. (nurse 1)
For public health professionals, effective communication demands the use of tools to promote interpersonal relationships between the community and the health team. In disaster situations, the communication regarding exposure to risks was identified as a competency for the nurse.
[...] we came to look at the water level. There was a whole house down in the middle of the river and the guy got into a boat [...] we saw those guys leaving without any safety equipment, no vest, nothing, nothing, nothing, and the water bringing trees, a lot of dirt. (nurse 1)
The communications from the health team to the population were facilitated by the community health agent, who was told to try to reach the families, offer help and see if the nurse or a physician was needed.
I would say, ‘No, I will not be able to go to such a residence, so you, the health agent, will go there, see how it is and there you will report to us to see if we need to send something or go there to provide some service or not’. (nurse 1)
Psychological support implies the identification of psychological needs and implementation of supportive nursing interventions to assure the wellbeing of health workers by meeting their basic human needs during such stressful times.
Nurses demonstrated the ability to be caring and sensitive and to sympathize with the populations’ necessities, creating a humane relationship and becoming a resource for patients who needed individual or collective care.
[...] then we did the psychological part. Let's wait, and when the river recedes, we'll see what's going to happen, but at the moment, while the river was swollen, we talked, tried to calm them down, did the psychological part. (nurse 5)
Health surveillance was developed to determine major disease risks, collaborate on developing plans to reduce identified risks, and assist in the development of surveillance systems related to disease outbreaks. In one municipality, diseases were related to the flooding due to the environment in which the population lived and the lack of a sanitary system. Thus, when the floods occurred in 2014 and 2015, the situation became more complicated.
[...] parasitic disease, as I said, fever, gastroenteritis, diarrhoea, children with verminosis; there is a lot, especially in this region that has these high intensity floods of short duration, leading to a lot of onions and animal waste from pig sties. The water stays on the ground, the mud comes, and the children play. At the level of primary health care, we mainly saw verminosis, fevers, and stomach diseases [...]. (nurse 9)
Educational competencies allow nurses to take on a leadership role in the development and implementation of training programs for nurses and other healthcare providers. According to one nurse, after the flood of July 2014, the need for training all health professionals emerged.
In 2014, as it was very serious, the need arose for them to enable us to work. Not that we were not trained, but we had never faced such a situation, and every day a new problem arose. The flood increased, the situation worsened even more, and then we did not know what to do. Then, the need for better training of all professionals arose. (nurse 17)
These domains help to elucidate in which areas nurses should prioritize their practice when a disaster occurs. If some sort of stratification would be proposed, it should take into account the greater number of competencies in leadership and management and health care, indicating the need for investment in preparing for this type of practice.
Table 1: Primary health care nurses’ competencies in rural disasters caused by floods, by domain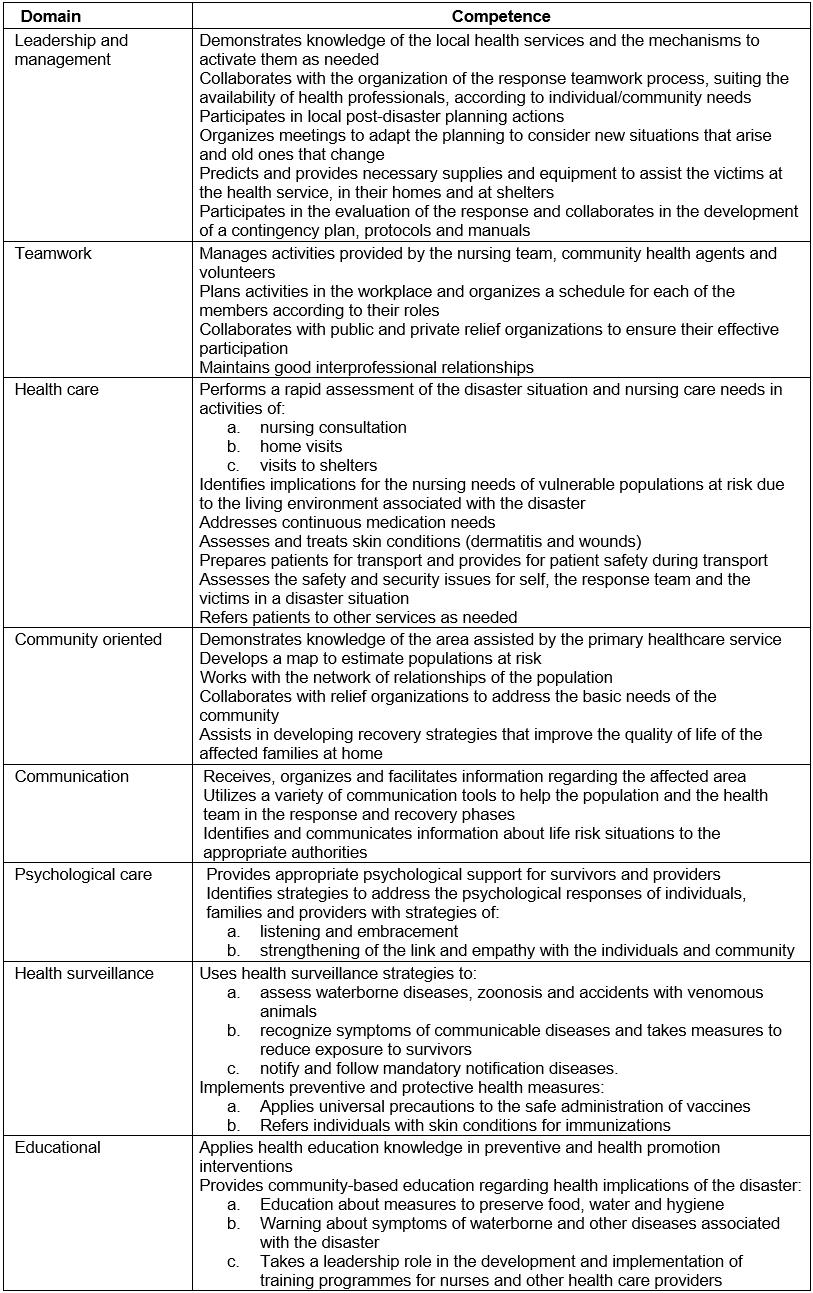
Discussion
In Brazil, PHC nurses serve as first responders, triage officers and care providers, coordinators of care and services, providers of information and education, health promoters, supervisors and counsellors. The nurses’ activities are directed towards the individual, the family and the community7.
In the response phase of a disaster, nurses function in leadership roles, managing and coordinating health care and caregivers. The knowledge of services in the region of a disaster and the organization of networks of health care services have been recognized as nurses’ competencies in Brazil in the context of hospital care6.
Managing logistics and human resources (including training and exercises) are actions planned to be developed by the nurse19. These competencies include participation in planning to meet healthcare needs in a disaster and can contribute to the development, assessment and modification, if any, of the community disaster plan16.
In the recovery phase, public health professionals are expected to assess and plan for future disasters. Competencies, including evaluation and management planning after a disaster, have been defined for nurses16. Nurses respond and practice during the disaster and collaborate with nursing organizations to solve problems and improve responses16.
The allocation and distribution of resources during a disaster is considered a skill of the public health nurse19, who manages the resources and supplies necessary for community care16. Lack of access to medications can have immediate repercussions on health; this lack of access can be life-threatening or lead to permanent disability20.
The possibility of having to work with limited or damaged resources18 was verified in this study in a municipality where resources such as survival kits were not available as planned.
As recommended for public health professionals, the establishment of protocols improves the capacity to respond in emergencies21. This need was expressed by nurses and others in Brazil for whom the use of protocols streamline work; this streamlining is important in disaster care, when actions need to be developed without delay6.
Disaster scenarios challenge effective interprofessional working practices. Maintaining a good interprofessional relationship is a skill expected of the generalist nurse22 and was found to be important for nurses in disasters in this study.
In Brazil, PHC nursing is developed by a team of nurses and nursing allied professionals. Within this team, community health agents play an important role as health promoters. Nurses are responsible for both these groups’ practices. Due to this experience, the management of the activities of volunteers was added to the nurses’ responsibilities.
For policy development and planning, nurses describe the role of government and organizations in disaster planning and response. In such situations, the nurse ‘collaborates with other health professionals, community organizations, governments, and community leaders to develop risk reduction measures to reduce the vulnerability of populations’(p. 50)16.
Health care of individuals and families demands that the nurse ‘conducts a health history and age appropriate assessment that includes physical and psychological responses to the disaster’ (p. 56)16. Nurses conduct consultations and/or referral of users to other healthcare providers in any line of continuity of care when the user's condition is not within the scope of the nurse's practice or the individual nurse's competence23. Knowing the network for possible referrals facilitates the sequence of health care of the affected populations.
The nursing role in various disaster assignments (eg shelters, emergency care sites, temporary healthcare settings, disaster coordination and management units)16 was described by a nurse who reported having performed this type of evaluation in the shelters, using a 'notebook' as a resource for recording and referral of cases.
Nurses valued home visits to prioritize the care and control of multiple situations and to adapt nursing practice standards, as necessary, based on available resources and patient care needs16. This context is close to what is recommended for community health nurses in Canada, where the home visit is a strategy that nurses use to ensure access to support services for vulnerable populations (people who are sick, elderly, young, poor, recently immigrated, isolated or have communication barriers)22.
Care for vulnerable groups in flood situations has been described in the competency ‘directs nursing actions to meet specific needs, considering the risks of vulnerable populations associated with the living conditions resulting from the disaster’. The need to direct the nursing team’s actions was recognized by hospital nurses for the response of disaster situations in Brazil6.
The special needs of vulnerable groups must be addressed in disasters to reduce the harmful effects on the health of the population and the number of deaths. PHC nurses are in a privileged position to understand the risks and needs of these populations in their service area and to prepare to support them during a disaster23.
There are few publications on access to medicines needed for people with chronic diseases. Lack of access can have immediate repercussions on health that can be life-threatening or lead to permanent disability20. The most commonly used health services and medicines were not available to residents in flood-affected areas in urban and rural communities24.
Some nurses may abide by the idea of saving lives without thinking about their own safety first, since they are more confident in their abilities if they are willing to take on more risk6. In this study, this situation was reported by nurses who, similar to the riverside residents accustomed to the Uruguay River floods, are exposed to unnecessary risk.
Helping to shape public policy that will decrease the consequences or potential effects of a disaster is an important role because of the nurse’s knowledge of the community and the areas of vulnerability16. Competency levels in relation to community dimensions of practice skills have been associated with rurality, as measured by district population density11.
The nurse assesses the community to determine pre-existing health problems, disease prevalence, chronic illness and disability, and community healthcare resources16. Sometimes the nurse needs the help of people close to the victims. By working together with the community, the nurse strengthens the health system's ability to respond and recover from a disaster16. Besides health needs, considerable emphasis was placed on the nurse’s role in social assistance, collaborating with relief organizations to address the basic needs of the community.
Disaster response demands effective communication with the application of principles of interpersonal relationships by PHC nurses. As recommended, nurses maintained records and documentation, provided reports as needed, coordinated information with other members of the disaster response team, and provided up-to-date information to the disaster response team regarding health issues and resource needs6,16.
Disasters require communication to be developed through the use of specialized communication equipment and a variety of communication tools to reduce language barriers16. Communication tools (pamphlets, booklets) and vocabulary accessible to users were reported by nurses, with educational lectures addressed to vulnerable groups.
Nurses were made aware of life-threatening situations because of their direct contact with the affected population in their territory. When reporting to the competent bodies the identified life-threatening situations, the nurse collaborates with the disaster response team in order to reduce risks in the affected area6.
It was reported that psychological shock arose in both the disaster affected populations and the people who provided care. Internationally, the need to develop relevant skills in health professionals is recognised, so that the mental health needs of people who have had experiences with floods can be met25.
In the case of nurses, they provide adequate psychological support for survivors, practitioners and volunteers who responded to the disaster, as well as identifying individuals' behavioral responses to the disaster and providing appropriate interventions as needed (eg psychological first aid)16. Intervening in the medium and long term to indicate to public health authorities the necessity of provision of health services to individuals with post-flood mental health problems may be necessary26.
In this regard, the competence of psychological evaluation and therapeutic counselling for professionals and victims in situations of stress was identified by the community nurses25. Along with psychological problems, an increase in the occurrence of cases of dengue fever and transmissible diseases has been reported in Brazil after the floods27.
Health surveillance demands recognition of the symptoms of communicable diseases and taking measures to reduce the exposure of survivors16. The identification of associations between gastrointestinal, skin and eye diseases28 is important for nurses to reduce the risks related to person-to-person transmission of diseases16.
Prevention and protection principles must be adapted to a repertoire of activities, such as to implement universal precautions for the safe administration of vaccines29. In this study, nurses carried out vaccinations in homes, shelters and in health units.
Educational competencies were directed towards health surveillance of the environment. As recommended, the population was encouraged to boil or lightly chlorinate the water if the sources of supply were contaminated. In addition, guidance was provided on how to prevent physical damage and exposure to flood waters or contaminated property during cleaning26.
However, it was difficult to intervene in these situations due to environmental conditions and the lifestyle of the people living in these places. Guidelines offered by the nurses often do not influence attitudes because of people’s low education level and because structural conditions do not allow for their implementation.
Health professionals must be trained accordingly to offer the correct answer. Previous disaster response experience and appropriate disaster education appear to be essential ingredients in providing a prepared and confident workforce. When an emergency plan predicts skills nurses do not possess, competencies are important tools to educate them about new techniques and forms of organization to address casualties6.
Conclusions
This study allowed the identification of PHC nurses’ competencies to be performed in rural areas when a disaster by flood occurs. These competencies were extracted from situations, behaviors and critical requirements identified with the Critical Incidents Technique, and they reflected existent and preferred skills, since they were derived from their lived experience and conclusions on what would be best for every circumstance.
These competencies could be related to the established international nurse competencies in disasters. Some of them were described only in this study, which demonstrates their contribution to the PHC nurse's performance in flood-type disasters in rural areas. Although developed in a specific region with specific characterizations and a history of occurrences of natural disasters, there is a potential for them to be adopted in other regions of Brazil and even internationally. This finding helps to give consistency to the need for the preparation of the nursing workforce, due to the increase in the occurrence of disasters by flood.
Some limitations of this study related to the critical incidents technique were the use of facts that occurred 1 or 2 years before the research and the psychological impact reported by some nurses at the time of the disaster, which may have interfered in their ability to remember the facts in full.
The development of competencies contributes to improving and streamlining nurses’ actions, positively influencing their practice and the health of the rural population. In addition, they constitute a reference and support for the preparation and performance of nurses in PHC, allowing them to adapt their practices to the affected population or in areas at risk.
Acknowledgements
The authors thank Coordenação de Aperfeiçoamento de Pessoal de Nivel Superior/CAPES of Brazil for financial support.

