Context
For quite a long time, patients in rural areas have considered the Chinese medical care system to be inaccessible, as well as unaffordable1,2. The major cause is that the medical resources, such as advanced equipment, pharmacies and qualified specialists, are usually concentrated in major hospitals in cities. Therefore, patients from towns and villages go to these major hospitals for medical care even for minor illnesses3,4. As a result, most rural hospitals and clinics cannot maintain their medical practices due to an ongoing decrease of both patients and financial and professional resources5,6. The expected medical services thus become inaccessible for patients with minor illnesses. On the other hand, major hospitals in cities have excessive patient numbers every day and exhaust their medical resources. Doctors have excessive caseloads, and may be unable to devote their expertise to management of complex diseases. The cost of medical services can be far too high for patients from towns and villages.
Government efforts towards a tiered medical scheme
The central government of China has put great effort into medical reforms to address these issues in previous decades1,7-9. The decentralisation of medical resources to make medical services affordable and easily accessible for rural populations is one of the major goals for the government. In the twelfth 5-year plan, primary care provision was addressed and community health centres and stations are required by the policy to enhance the medical service quality for both urban communities and rural areas10,11.
The tiered medical scheme (TMS) was introduced by the Chinese State Council in 2015 to try to redistribute medical resources and provide accessible medical care for rural areas12. The TMS policy divides the medical service providers geographically into three different tiers: (1) major hospitals serving counties, (2) community hospitals serving towns and (3) clinics serving villages. Four principles are suggested by the TMS policy to optimise the medical care provision: the initial diagnosis should be made by a local medical service provider, a bidirectional patient referral should be executed to provide optimal medical services, acute and chronic diseases should be treated distinctively by appropriate channels in hospitals at different tiers, and medical resource optimisation should be carried out within the three tiers rather than in an individual hospital.
Issues
Challenges for the implementation of TMS
While a promising direction is provided by the TMS policy, it has not been easy to implement. Although the coverage of community health centres providing primary care has been significantly increased11, rural areas with developing economies and less health funding still suffer from a lack of accessible primary care13. Additionally, the service quality of township community hospital and village clinics is still worrisome due to lack of human resources and hence struggling GP practices11; accordingly, these providers cannot efficiently serve more patients in rural areas, even with the success of the New Rural Cooperative Medical Scheme14. While the bidirectional referral mechanism has long been addressed by government policies10,12,15, barriers still exist between providers, preventing close collaborations due to different service qualities and financial interests16,17.
The inefficient financial management model is, in the authors’ opinion, the key reason for the challenges of implementing the TMS policy and decentralising medical resources at the grassroots level. Traditionally, government health funding (the New Rural Cooperative Medical Scheme) is managed by the provincial health authority and allocated to each medical service provider according to the volume of services it provides. Such a funding model has multiple challenges:
- unsustainable development of primary care: Most government funding goes to major hospitals in urban areas and counties, which treat an overload of patients. Being underfunded, the town and village clinics are unable to provide quality primary care, nor do they act as the gatekeeper to provide first diagnosis as encouraged by the TMS policy.
- barriers among service providers: Because funding is allocated according to the number of patients each provider treats, medical collaborations and resource sharing among providers are not facilitated. The providers would rather compete with each other for their own financial interests. Additionally, the bidirectional patient referral mechanism would not be easily implemented, because a referral decision could be influenced by financial incentives instead of professional judgement18.
- biased pricing structure: High pharmaceutical prices is one of the issues with the Chinese medical care system, and is the main cause of the unaffordability problem for patients. Although reducing the proportion of drug sales in hospital income has been addressed as a goal of the Chinese medical care reform, most providers, especially those in townships and villages, still consider drug sales as their main source of income due to lack of government funding19,20.
These challenges resulting from the previous financial management model prevented the medical resources from being decentralised. As such, a financial reform approach that can effectively support the implementation of the TMS policy is imperative.
Medical service unity
The medical service unity (MSU) approach, as shown in Figure 1, is an approach for the implementation of the TMS policy to decentralise the medical resources. The key philosophy of the MSU is to organise medical service providers from all three tiers in a region as a unity. The tier 1 hospital takes charge of the MSU to provide unified management. All tier 2 hospitals are affiliated to the tier 1 hospital and each tier 3 clinic is affiliated to a tier 2 hospital. Each medical service provider in the MSU plays a part in sharing medical knowledge and experience, expertise and equipment. In particular, a new financial management model is promoted in the MSU, in which the government finding is shared and managed by the unity rather than allocated to each individual provider. Accordingly, three flows can be defined – funding flow, patient flow and medical resource flow – to effectively integrate the medical services amongst the three tiers. The three flows are enabled by the following three mechanisms, in which the financial decentralisation is a radical but fundamental reform.
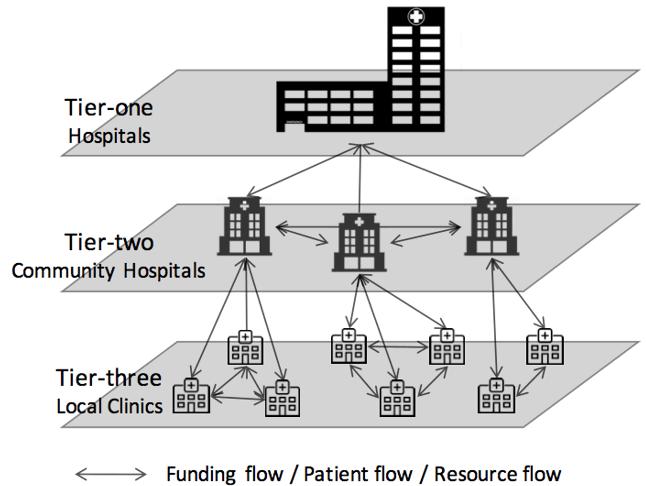 Figure 1: The medical service unity model.
Figure 1: The medical service unity model.
Financial decentralisation: With respect to the previous funding model, a radical change is proposed by the MSU to overcome the challenges already discussed. In an MSU, the management of the government health funding (New Rural Cooperative Medical Scheme) is taken over by the tier 1 hospital from the health authority. The budget is determined by the government according to the population within the specific MSU on a standard rate per capita. The funding is allocated to the MSU seasonally in advance and the government evaluates the usage of the funding at the end of each year. Importantly, any funding surplus can be kept by the MSU for the development of all the members; over-spending is not supported unless there are justified reasons. As a consequence, the government roles within the health funding system change from provider, distributor and manager to just provider and supervisor. The MSU manages the funding, and allocates it to each provider according to the need instead of workload with an adaptive manner.
Such a decentralised financial management mechanism has great potential to improve the medical care provision in rural areas, and also facilitate the implementation of the MSU. The developing service providers from the lower tier can get more funding to improve their service qualities so that they can play a better role in the MSU. Sharing the same financial interests promotes the real collaboration among the unity.
Bidirectional patient referral: The MSU promotes a patient flow to provide each patient with adequate medical services and also distribute the patients to lower tiers where possible. A patient referral facilitates the patient flow in two directions, from lower to upper tiers, and vice-versa. Based on the severity of a disease, a decision can normally be made on either treating locally or referring the patient to upper-tier providers. Bidirectional referrals could happen even for a single patient. For example, a patient can be referred to an upper-tier hospital for surgery and referred back for recovery. With such a mechanism, the patient does not need to suffer high costs and the upper-tier hospital does not have to exhaust its medical resources if the patient can be treated locally. Additionally, the patient can be referred to another provider in the same tier if necessary, subject to the availability of expertise and equipment.
Such a bidirectional referral mechanism mutually benefits medical providers and patients. If patients are treated locally where possible, upper-tier hospitals can devote their resources to the treatment of more severe illnesses, while the lower-tier providers are able to fulfil their medical responsibilities and gain experience. Accessing medical services locally can significantly lower the cost for patients as shown in Table 1, and thus the inexpensive medical services are made accessible to patients.
Table 1: Comparison between average costs of three selected surgeries in a tier 1 hospital (People’s Hospital of Funan) and a tier 2 hospital (Community Hospital of Chaiji) in Funan county 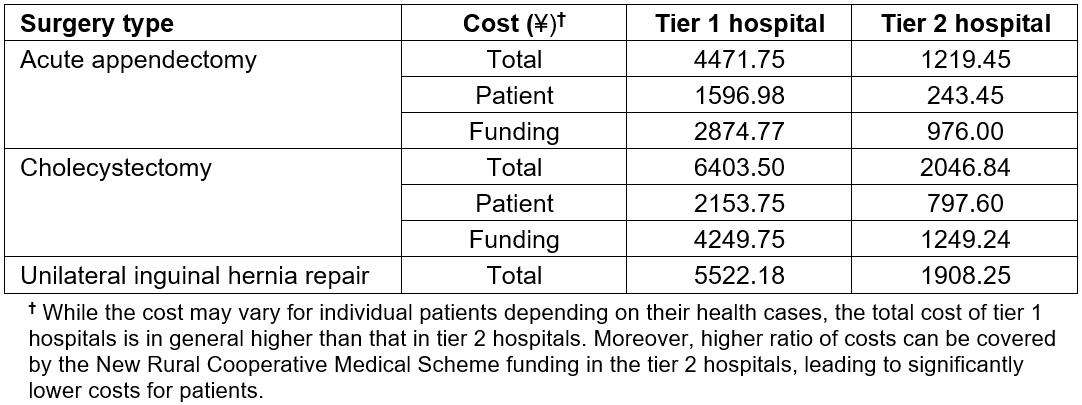
Medical resource sharing: The medical resource flow, consisting of doctors with expertise and experience as well as equipment, is enabled by the sharing mechanism. A doctor mobility scheme is promoted to allow highly qualified and experienced doctors from the upper-tier hospitals to support medical practices for their affiliated lower-tier members with financial incentives attached. For example, mobile doctors from the upper tier can obtain additional allowances when they provide services in the lower tiers. Doctors from the lower tiers can be assigned to upper-tier hospitals to work with experienced doctors in order to advance their skills.
The three flows are intercorrelated with each other. The funding flow fundamentally groups the providers in a unity and empowers the patient flow and resource flow. The patient flow distributes patients to lower tiers, which reinforces the funding flow. The resource flow improves the service capabilities of the lower tiers and in turn supports the patient flow.
MSU pilot in Funan
In response to the central government’s call, many cities and counties in China have tried to implement the TMS policy. The MSU is a particular approach adopted by different pilot projects, including Funan county in Anhui province. Since May 2015, Funan county established radical reform in terms of financial decentralisation to effectively support a two-tier form where the People’s Hospital of Funan at tier 1 leads the MSU and three community hospitals from Chaiji town, Zhuzhai town and Jiaopo town respectively constitute tier 221. No clinics were formally included in tier 3 because the clinics in the villages are only able to provide peripheral medical services. However, the Funan MSU encourages local clinics as well as village doctors to sign agreements with the tier 2 community hospitals so that they can in general participate in the unity.
Figure 2 shows that the three tier 2 hospitals have made changes through the implementation of the MSU from 2015 to 2016. For the period May–July 2016, the tier 2 hospitals have increased by 28.44% for outpatients, 8.93% for inpatients, and 33.53% for surgeries. The data demonstrate that tier 2 hospitals became more capable of providing services and, therefore, the income of these hospitals increased by 21.03%. Furthermore, while the government health funding has been allocated to the leading hospital of the MSU, a surplus of ¥26.19 million was made in 2016 in comparison with ¥10.49 million in 2015 because treating patients locally reduces costs. The surplus was then used to support the doctor mobility scheme. By doing so, the doctors received an average 40% increase in their salary. In summary, the MSU in Funan achieved, as reported by Finance China22, development for hospitals, benefits for patients and motivation for doctors.
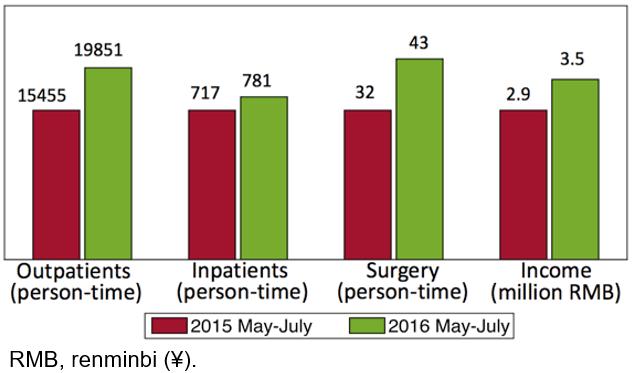 Figure 2: Comparison of tier 2 hospitals between two periods after the implementation of medical service unity in Funan county.
Figure 2: Comparison of tier 2 hospitals between two periods after the implementation of medical service unity in Funan county.
Lessons learned
Promising improvements have been achieved since the pilot project started, which displayed the value of the MSU approach. The three mechanisms played essential roles in the MSU project in Funan, which enabled the funding flow, patient flow and medical resource flow to implement the TMS policy. The financial decentralisation facilitated the successful implementation of the TMS policy. The medical service quality of the lower-tier providers can be greatly enhanced through effective collaborations within the unity, enabled by the financial decentralisation. From a long-term perspective, the financial decentralisation benefits the sustainable development of the medical system. A cost of treatment at a lower-tier hospital is normally less than at a higher-tier one (Table 1). Therefore, retaining patients locally can not only improve affordability to patients but also save the funding of the New Rural Cooperative Medical Scheme, leading to surplus. The surplus can then be used to improve salaries for those doctors who work at the lower tier in the MSU as well as favourably ameliorate the pricing structure. The mechanisms of bidirectional referral and medical resource sharing are made possible by financial decentralisation, and directly target the TMS policy, as such potentially improving accessibility and affordability for patients in rural areas. Bidirectional referral spreads the pressure to appropriate providers from different tiers, and the medical resources can thus be used much more efficiently. Localising patients as much as possible can also optimise the use of the New Rural Cooperative Medical Scheme funding. The sharing of medical resources can further improve the lower-tier service quality, hence rendering quality medical services directly accessible to patients in rural areas.
The potential value of the MSU approach shown by the pilot experience in Funan has been attracting significant attention from the central government and provinces other than Funan23-25. It offers inspiring insights to the healthcare provision for effective decision-making.
Future policies should address the financial management in health systems instead of only focusing on fixing the issues directly. The common perception is that the inaccessibility to and unaffordability of the healthcare service are the causes of the issues. While most previous policies, including the TMS policy, have been directed toward the improvement of accessibility and affordability on the surface without addressing the fundamentals, the MSU approach focuses on the root of the problem. The MSU deploys a strategy to deal with the vital point through the redefining and redistribution of financial responsibility. Accordingly, further adoption of the policy of finance reform will intensify all parties involved to be engaged more actively in the overall health reforms.
The MSU demonstrated a potential approach which can be adopted by other regions across China and even other countries to optimise the medical service practices. The tiered model could be tailored to suit different medical service settings in other regional medical systems. For example, the MSU model could begin with high tiers (province, city, and county). Village clinics can be added into the unity as the lowest tier at a later stage. In summary, to organise and motivate the providers from different tiers as a unity rather than let them operate separately will potentially help any medical system to enhance their service provision.
Acknowledgements
This work is partially supported by a key project of National Natural Science Foundation of China (NSFC) with grant number 71532002 and a key project of Beijing Social Science Foundation Research Base with grant number of 18JDGLA017.
