Introduction
Australian health and aged care policy is undergoing rapid change as a result of current reforms1-3, which include dramatic changes to aged care advocated in the Productivity Commission report Caring for older Australians. Recently, these reforms have advocated an approach to service provision that emphasises a more holistic model of health; consequently, recent policy has emphasised wellness4, a multidimensional concept that includes aspects such as physical resilience, emotional wellbeing, social connectedness and spirituality5, as an optimal outcome for older adults. This policy perspective promotes the achievement of wellness as a means of enhancing the independence of older people, improving quality of life, ensuring the continued contribution of older people to society and reducing demand for expensive and ongoing services1-3,6.
However, the capacity of older adults to maintain their wellness is problematic in rural contexts. It is generally reported that rural older people experience poorer health outcomes than those in urban areas, specifically related to increased mortality. In Australia, as in many other countries, rural areas have a much higher proportion of older people than do metropolitan areas7,8. Demographic ageing is more dramatic in rural Australia, where the numbers of older people residing in rural communities are growing rapidly as a result of two concurrent trends: young people relocating out of rural areas for education and employment and older people migrating to rural areas in retirement9. These changes reduce the capacity of rural communities to adequately cater for the growing numbers of older people. In particular, demand on local services is increasing at a time when many rural communities struggle to provide the types of health and community services likely to sustain older people’s health and wellbeing10.
Whilst the focus remains on the promotion of wellness in the policy agenda, there is a lack of systematic rigorous evidence examining wellness in older people, particularly those who live in rural areas. Such knowledge is essential if policymakers are to understand how to respond to the needs of older people across the diversity of Australia’s rural areas. In view of the gap in knowledge, the present article seeks to test a predictive model of wellness of rural older people. In doing so, it will draw on cross-sectional data collected via a telephone survey utilising a community saturation strategy across six rural case study sites in two Australian states: Queensland and Victoria. The intent was to build a diverse sample of both case study sites and individual respondents in order to best represent the experience of ageing in a rural Australian community.
The concept of wellness
The concepts of wellness, quality of life (QoL) and wellbeing are commonly used in research and in policy. The choice between the terms has been somewhat arbitrary and there exist gaps and inconsistencies in the measurement tools of each of the three. Thus, for example, QoL has been extensively conceptualised and theorised, and WHO has both defined and provided an appropriate measure11. Despite this, the research literature includes many different ways of measuring QoL, including the CASP-19 measure12, the Satisfaction with Life Scale13 and the Philadelphia Centre Morale Scale13, as well as numerous unvalidated and self-devised questionnaires. While there are many definitions of wellbeing and different measurement tools, they are remarkably similar in their components, emphasising both current happiness or satisfaction and an expectation of future happiness14,15.
Wellness is considered a broader term and according to the WHO recognises the ‘realisation of the fullest potential of an individual physically, psychologically, socially, spiritually and economically’, recognising the breadth of factors that lead to positive health and wellbeing16. Thus wellness is considered the optimal state of health of individuals and groups, encompassing the maximum potential of which the individual is capable.
However, there is a surprising paucity of research that uses wellness as the central measure. Instead, research examining older people’s health has tended to use ‘wellbeing’ and ‘quality of life’ and ‘life satisfaction’ measures interchangeably, making comparisons between the studies difficult. In recent studies of older people’s health, Gana et al17 used wellbeing as the central measure of a longitudinal study; Pinto, Fontaine and Neri18 used life satisfaction; and Prieto-Flores et al19 used QoL measures. This use of different terms and measurement tools might explain why the evidence about the ‘wellness’ of rural older people is somewhat mixed.
The Perceived Wellness Survey (PWS) developed by Adams et al20 provides a measure of wellness across six domains: physical, spiritual, social, intellectual, emotional and psychological20. A number of studies have been conducted to validate the PWS in measuring wellness, including Adams et al20, and Harari, Waehler and Rogers21. The PWS has been used to investigate wellness in a variety of contexts, including persons with traumatic brain injury22, consumption of organic foods23, fitness courses24 and burnout rates25. A limited number of studies have utilised the PWS for measuring wellness in older adults. One Australian study demonstrates the strong correlation between wellness and physical and mental aspects of health26.
There has been limited research related to wellness in older people, and little is known about the broader systems in which rural older people live and the impact of personal and environmental factors. Recognising this interconnectedness of older people and place, the present study sought to test an ecological model of wellness. Brofenbrenner’s human ecology model recognises the importance of the environment at the microsystem, mesosystem, exosystem and macrosystem levels27. However, as early as 1988, McLeroy et al argued that models like Brofenbrenner’s lack the specificity to guide conceptualisations of health problems and subsequent interventions28. They instead proposed a variation of Brofenbrenner’s model that includes an examination of (1) intrapersonal factors – characteristics of the individual, (2) interpersonal processes and primary groups – formal and social network and social support systems, (3) institutional factors – social institutions, (4) community factors – relationships among organisations, institutions and informal networks and (5) public policy. In the present study, McLeroy et al’s ecological model28 provided the framework to developing a predictive model of wellness in rural older people.
A review of the literature of community-dwelling older people conducted by Yeom, Fleury and Keller identified the following intrapersonal factors: age, gender, socioeconomic status, marital status, mental health and physical health29. Other factors such as loneliness were also considered due to a body of research that has found loneliness in older people to be correlated with increased anxiety, increased depression30-33 and other physical health conditions. At the interpersonal level, social factors associated with presence of formal and informal ties and levels of social and community participation have been identified as potential factors impacting on older people’s wellbeing34. These factors are often associated with bonding forms of social capital, characterised by dense networks of support, reciprocity and engagement in participation35-37. At the institutional level, characteristics associated with the service environment, such as the availability of community amenities and health services, have been found to be associated with wellbeing in older people34,38. At the community level, factors associated with the personal and physical characteristics of the community were identified as impacting on older people’s wellbeing34,39. The present study, combining this set of factors derived from the literature, seeks to test this ecological model and its relationship to wellness in rural older people.
Methods
Research design
The present study draws on data from a multistage study to address the research question ‘What factors best predict wellness for older people living in diverse rural communities?’ In recognition of the diversity of both older people and their rural communities, the first stage of the study identified rural case study sites across two Australian states: Queensland and Victoria. Six sites were chosen to maximise community variability, using the Australian Bureau of Statistics Statistical Areas Level 2 (SA2) classification of key variables40. During the second stage of the study, a cross-sectional survey was designed and delivered to a diverse sample of rural older people.
Survey instrument
The key measure of this study was wellness as measured by the PWS20. The ecological model developed included the following intrapersonal factors: physical and mental health as measured by the Short-form 8 (SF-8) Health Status Questionnaire41, Loneliness Scale42 and social demographic characteristics (age, gender, marital status and financial capability). Financial capability was measured using a scale developed by Zaidi43. Interpersonal factors included a measure of social and community group participation44 and a series of questions designed to determine each respondent’s social network size. Questions were also asked on the characteristics of the support network related to the provision of assistance and care. Institutional factors were measured by a series of questions devised around the resource base environment and access to amenities and services. Specifically, participants were asked to rate their level of satisfaction with amenities that are available in their community. A Likert accessibility scale was developed for this purpose. Community factors were measured by a series of questions of perceptions of community (11 items) drawn from Dobbs’ study45.
A factor analysis was used to group the 11 community perception questions into two broader categories: personal characteristics of the community (eg ‘my community is a safe place to live’, ‘most people in my community can be trusted’ and ‘most people in my community have lived here a long time’) and physical characteristics of the community (‘the services in my community are easily accessible’ and ‘the community is an easy place to get around’).
Recruitment strategy
A community saturation approach46 was utilised to recruit a diverse sample of participants in relation to age, health status and location. The research team visited communities within the six case study sites in person to circulate information and elicit interest in the study. By working with health and aged care agency partners, the study endeavoured to include more frail and isolated older people. Inclusion criteria for the sample population was those aged 65 years or more and living within one of the six selected rural communities. Older people living in residential care or experiencing dementia were excluded. Study materials for participant recruitment were developed, including a flyer and an expression of interest postcard. A 1800 number was created and included in the study material to allow participants to contact staff toll-free. A detailed information sheet was supplied to all participants. A total of 266 older people from six rural townships within Australia took part in the current study. The sample consisted of 93 men and 172 women aged 63–100 years (mean=75.92, standard deviation (SD)=7.77), with 1.1% identifying as Aboriginal or Torres Strait Islander.
Procedures
The survey was administered by telephone, with the specific aim of reducing incomplete data, a significant limitation of self-administered questionnaires. Face-to-face administration of the questionnaire was offered to those participants who were particularly frail, had hearing problems or who had trouble with English language.
Statistical analysis
All data were entered into the Statistical Package for Social Sciences v22 (IBM; http://www.spss.com) for analysis. Data were checked for accuracy, missing values and outliers and cleaned, with out-of-range values recorded as missing. Missing values for the PWS subscales were replaced with means where more than 50% of the questions in the subscale were answered. Prior to examining hypothesised bivariate and multivariable relationships analysis, scores were calculated on key measures. Wellness scores were calculated (36 items), with means calculated for psychological, emotional, social, physical, spiritual and intellectual items. A wellness composite score was calculated, adhering to the guidelines provided. Total scores were calculated for SF-8 (physical and mental components) and the De Jong Gierveld and Van Tilburg loneliness measure42. The sizes of social networks were calculated, adding together the number of family, friends and neighbours. A total score for access to amenities was calculated, along with a total score for access to health services.
Prior to conducting multivariable analysis, the relationship between perceived wellness and several key variables was determined using Pearson product correlation coefficient (r). A one-way between-groups analysis of variance (ANOVA) was used to examine whether there were significant differences in wellness scores across the different sites. Hierarchical regression analysis was used to determine which factors in the model best predict wellness. A hierarchical regression involves predictors to a regression model being added in blocks, which allows the incremental contribution of these variables to be determined.
Ethics approval
Ethics approval was obtained from La Trobe University (HREC #14-051) and the University of Queensland (HREC # 2014001347).
Results
Descriptive data are provided in Table 1. On the SF-8 participants scored an average of 45.03 (SD=10.82) for the physical component score and 51.67 (SD=9.06) for the mental component score. The SF-8 has norm-based scoring (mean=50, SD=10), suggesting that the results obtained in the current study are relatively standard. Participants scored an average of 13.39 (SD=3.07) on the composite score for the PWS (range=6–36). While there are no validated cut-off points for the PWS, these results are similar to those obtained in other literature22,25,47,48, suggesting that these averages are again relatively standard. Participants scored an average of 1.11 (SD=1.27) on the six-item De Jong Gierveld and Van Tilburg loneliness measure (range=0–6). These scores are somewhat lower than those obtained from older adults in different countries47,48. Financial capability was relatively high with almost all participants (261; 98.1%) reporting an ability to afford to keep their home adequately warm or cool and 233 (87.6%) reporting an ability to pay for unexpected expenses through their own resources.
All participants excluding one were able to name at least one person in their social network, with most (84.6%) naming between 5 and 15 people. The mean size of this network was 9.33 people (SD=4.42). The majority of participants (96.3%) were satisfied or very satisfied with the contact they had with family, friends and neighbours. All participants excluding one attended at least one social or community group event semi-regularly, with the majority of participants (88%) attending at least three social or community types of services a year.
The majority of participants were fairly satisfied with their access to amenities and health care, with participants reporting access as easy 87% of the time for amenities and 66% of the time for health care. Participant ratings of transport options ranged from 1 (‘very poor’) to 5 (‘excellent’), with the mean rating of 2.37 (SD=1.23) sitting between the ‘poor’ to ‘fair’ response options, although most reported minimal effect of lack of transport on their ability to do specific tasks.
A bivariate correlation was conducted to assess the relationship between the measured variables (Table 2). Of note, wellness was significantly related to physical health, mental health and loneliness. However, wellness was not associated with access to services or the size of a participant’s social network.
Table 1: Characteristics of study participants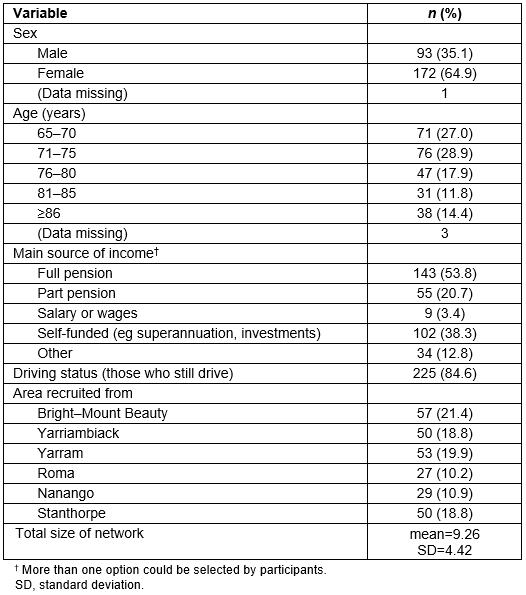
Table 2: Spearman correlations for demographic and outcome variable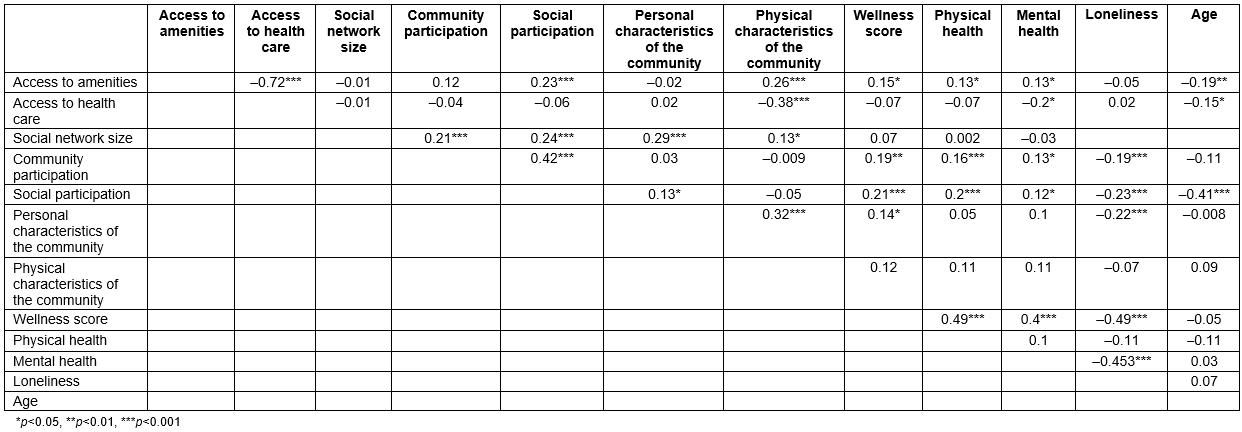
Differences in wellness scores across six case study sites
Comparisons between the six rural townships in wellness was conducted using ANOVA. The results were non-significant (F(5,245)=1.06, p=0.38, %u02732=0.02), indicating that the wellness levels are relatively similar in each of the six sites across Australia.
Predictors of wellness
A hierarchical regression was conducted to determine which variables in the model predict wellness. The ecological model determined the steps and how they were entered. Thus intrapersonal characteristic variables were entered at step 1 and explained 54.2% of the variance in wellness scores (R2=0.54, F(7,96)=16.24, p<0.001). At step 2, interpersonal variables were added to the regression and explained an additional 4.1% of the variance (R2=0.58, F(9,94)=14.54, p<0.001). At step 3, institutional variables were added to the regression, adding 1.7% of explained variance (R2=0.6, F(11, 92)=12.54, p<0.001). Finally, at step 4, community variables were added to the regression; however, they explained minimal additional variance (R2=0.601, F(13,90)=10.44, p<0.001). The results are summarised in Table 3.
The hierarchical regression revealed that the variables that contributed independently and significantly to perceived wellness were physical health, mental health, loneliness, financial capability, social network size and community participation.
Table 3: Summary of hierarchical regression analysis for variables predicting wellness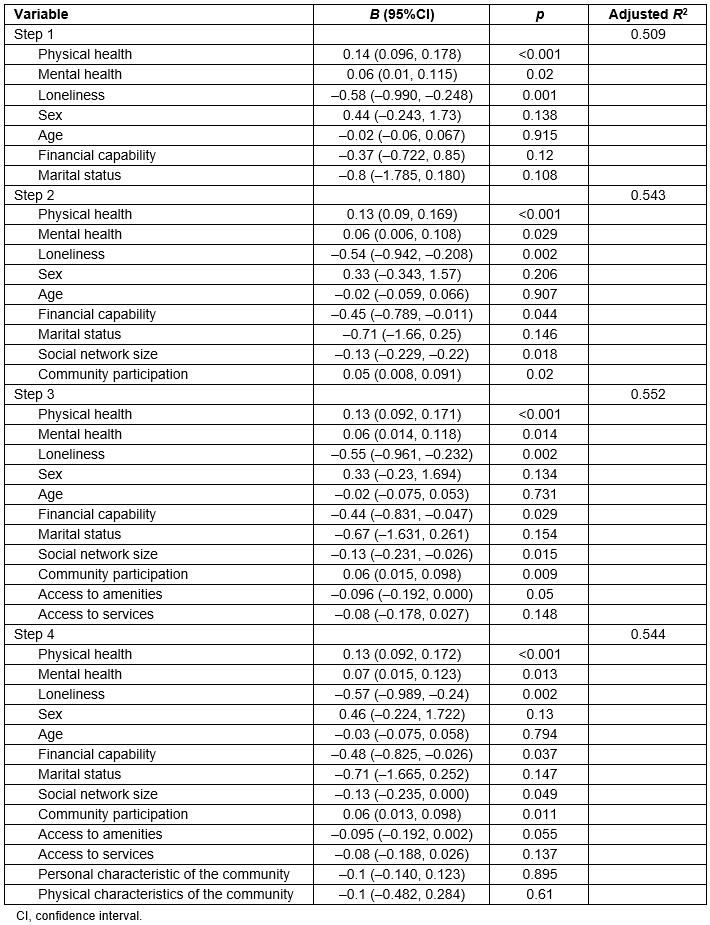
Discussion
This study, using an ecological approach, has indicated which factors best predict wellness for older people living in diverse rural communities. As prior research has focused on rural older people’s wellbeing and QoL and generally lacked conceptual clarity and consistency, the present study sought to make a unique contribution to knowledge through use of the multidimensional measure of wellness49. Use of this concept recognised the interrelated social, economic and physical influences that impact older people throughout the life course50.
The ecological model developed explains 58.8% variance in the wellness scores of rural older people. An examination of the independent variables highlighted that the intrapersonal factors were the strongest predictors of wellness: physical health, financial capability, the extent of loneliness experienced and mental health. Interpersonal factors – size of social network and extent of community participation – also contributed significantly to the variance observed. Institutional factors – the resource base environment and access to amenities and services – contributed only marginally to the model. Community factors – the personal and physical characteristics of community – only made a marginal contribution.
The means scores for the physical and mental components of health were close to the average score noted in the general population. However, this study did find that physical health made the strongest unique contribution to perceived wellness. Together, physical and mental health accounted for almost half the variance in relation to perceived wellness. This finding supports other research into wellness and older people using Adam’s perceived wellness measure20, such as Foottit and Anderson’s work26. From the results of their study Foottit and Anderson concluded that being physically able to do a number of activities (free of chronic pain), combined with good mental health, contributes to older people’s perceptions of wellness. Findings also support a body of work that has found rural older people experience poorer health outcomes than those in urban areas51,52. As there is a paucity of research using wellness as the central measure in older cohorts and across the lifespan53, the present study’s findings provide further supporting evidence.
The other key intrapersonal factor in the present study was loneliness. The impact of loneliness on physical health has been well documented, with evidence suggesting that through this and other mechanisms loneliness may be linked to multiple chronic illnesses54,55. It is also associated with poor mental health outcomes, such as increased depressive symptoms56, suicidal behaviours57, impaired cognitive performance58 and diminished executive control59. The findings here extend this body of work, by demonstrating a significant relationship to the broader concept of wellness.
The other intrapersonal factor that contributed significantly to the model was financial capability. Using Zaidi’s measure the present study was able to confirm that lower levels of financial capability were related to perceived wellness. Kimberley’s analysis of national Australian data demonstrates that 56% of Australians aged 75 years or more fall into the lowest income quintile and 22% into the second lowest60. In Australia, the aged care pension alone is widely recognised as inadequate60, yet in the present study nearly three-quarters of participants (74%) were reliant on full or part pension.
Perceived wellness was also predicted by interpersonal factors, in particular size of social network and degree of community participation. A detailed examination of support networks enabled the following to be captured: the mean size of participants’ network was over nine people, with 94.0–94.7% of networks containing a mix of ages and sexes and 90.9% including both kin and non-kin relationships. The majority of participants had regular contact with family, friends or neighbours and were involved in at least one social or community group. The social capital literature has highlighted the importance of bonding social capital, characterised by dense networks of social support61 in enabling people to ‘get by’35. Previous work by Heenan found evidence of strong reciprocal support between older people living in rural Northern Ireland62. Similarly, Australian research has found evidence of considerable reciprocal relationships between older people and their friends and neighbours63,64. The present study adds to the body of research on social capital, establishing a link to wellness in rural older people.
Somewhat surprisingly, both institutional factors and community factors did not significantly predict individual wellness. The institutional factors in the model, in particular access to amenities and health services, were not significant predictors, with the majority of participants satisfied with their access to amenities and health care. This is despite the literature highlighting the importance of the interactions between the resource environment on wellbeing and quality of life. This finding may be explained by a number of factors, including that rural older people see themselves as resilient and thus may have lower expectations of health care65.
The present study was not able to find support for community perception, either personal or physical. This was similarly surprising, as the study specifically set out to focus on rural communities with very diverse resource environments, including, for example, alpine areas, mining towns and farming regions. Despite this, the authors were unable to find any statistical difference in wellness based upon where participants lived, with surprisingly similar means in wellness scores across these areas. One potential explanation is that older people from a diverse range of rural communities tend to perceive themselves as having a rural place-based identity66.
Further explanations for this set of findings relate to the difficulties of recruiting hard-to-access populations, such as frail aged and socially isolated people from rural regions. Due to financial, ethical and practical constraints, it was not possible to recruit a random sample for this study. Instead, an attempt was made to maximise diversity among participants by utilising a community saturation approach. However, results suggest that there was both a gender bias and an overrepresentation of people from higher educational backgrounds in the sample. This limitation clearly needs addressing in future research, and the next stage of the study, in-depth interviews, draws on stratified sampling techniques to maximise diversity across the sample.
There are other limitations to the study, including its cross-sectional nature, which makes causality difficult to predict. Further, at the time of conducting the study, Adam’s perceived wellness measure20 was assessed as the best available tool, whilst acknowledging its lack of consistent application to older cohorts. Foster, Galjour and Spengel53 have since proposed that this measure fails to accommodate the impact of lifespan change on wellness and hence that older people tend to perceive wellness differently from the dimensions proposed by Adams20. In doing so they drop items from the established scale, drawing into question the validity of their tool. Strout and Howard have developed the Wellness Assessment Tool (WEL) designed specifically to measure wellness in older people living independently in the community and including other dimensions such as exercise and fitness, nutrition and social relationships67. There remains, however, only limited research measuring wellness in older people, suggesting that there is potential for future research development in this area.
Conclusions
This study set out to examine the predictors of wellness in rural older people. It did so by using a multidimensional concept that moves away from measuring descriptors of wellness, such as wellbeing and quality of life, to an integrated model of measurement. Using an ecological approach, the present study found wellness to be related to key intrapersonal and interpersonal factors. These factors should be considered when developing policy and subsequent strategies to increase the capacity of rural communities to facilitate wellness.
Acknowledgements
This study was supported by an Australian Research Council Linkage Grant (LP120200226), in conjunction with the Victorian Department of Human Services, Unitingcare Queensland, Southwest Queensland Hospital and Health Services, the University of Alberta, and the University of Queensland. Thanks are due to other ASPIRE research team members, particularly Rachel Winterton, Maree Petersen, and Turi Berg, who assisted with data collection.