Introduction
Preventing maternal deaths depends significantly on the presence of skilled birth attendants at child delivery1. To reduce maternal mortality, the Kenyan Government is promoting skilled birth attendance, for example by prohibiting births solely attended by traditional birth attendants (TBAs)2. To further lower barriers, the government has abolished user payment for maternal delivery at public health facilities. The Beyond Zero campaign aims to promote access to skilled delivery through the provision of equipped mobile clinics. Caulfield et al. found that, despite these strategies, many Kenyan women, particularly in remote areas, continue to give birth at home attended by family members or TBAs2. They only resort to formal healthcare services in the event of complications, often when it is too late for effective intervention.
For rural residents, who have a greater difficulty in traveling to primary, preventative, prenatal and emergency care providers3, access to health care overall is a challenge. The use of reproductive health vouchers is one approach that can help reduce financial barriers to healthcare access, stimulating client demand for services, and giving clients the purchasing power to seek care from the full range of available providers4. According to Obare et al.4 significant reduction in financial barriers is achieved through subsidizing the cost of services, providing transport to accredited providers, or both.
In the past few years, Information and Communication Technology for Development (ICT4D) has become a buzz term for developing technological solutions to support rural development for remote and low-resource settings. In the context of the rapid mobile phone penetration in developing countries, mobile technology is currently considered to be particularly important for development5. In many developing settings, access to mobile phones exceeds the availability of paved roads, clean water, bank accounts or electricity6. The wide availability and relative simplicity of mobile phones make them a promising instrument for delivering a variety of development interventions, among others in the health sector. Mobile health (mHealth) initiatives developed for low-resource and remote settings include interventions for treatment and disease management, data collection and disease surveillance, health support systems, health promotion and disease prevention, communication between patients and healthcare providers, and medical education7. The scale of implementation, however, remains heavily dependent on its adoption by potential users.
In June 2013, M-PESA Foundation launched a project aimed at improving maternal and newborn health outcomes in Samburu, Kenya, where the maternal mortality rate is 360 per 100 000 live births8. The project was conducted in partnership with PharmAccess Foundation, Safaricom, AMREF Flying Doctors and the Ministry of Health of Kenya through the Samburu County Health Management Team. A baseline study among 385 women and girls aged 15–49 years was carried out to assess the status of utilization of maternal healthcare services and facility deliveries, the role of community units in promoting maternal health, health worker training gaps and mobile phone availability (Samburu Maternal Neonatal Health Project Phase II baseline report, unpublished, 9 November 2015). The survey established that home deliveries were common if not the norm (ie 66% of the sampled respondents). Those who went to hospital mainly did so because of complications during delivery. Distance to the facility was the biggest barrier to facility delivery, reported by 64% of the respondents. Ownership of mobile phones was reported by 72% of respondents across three sub-counties in Samburu. To address the poor physical access to health facilities, PharmAccess Foundation tested the use of mobile money-based transport vouchers to pay for transport to the health facility. The vouchers were implemented using the Safaricom closed-loop wallet, Surepay. Surepay is built on top of the M-PESA mobile money transfer system. It allows funds to be placed under restrictions on where and how the money can be used. The experiment was carried out in two remote areas of Samburu County: Barsaloi and Suguta Mar Mar. The transport voucher was to be used for ambulance transport services to the health facility.
The objectives of the experiment were first to test if facilitation of transport to healthcare facilities would result in increased numbers of enrolled mothers opting for skilled delivery at a health facility, as opposed to delivery at home. The second objective was to investigate the technical usability of the Surepay wallet as a transport voucher, and the third to identify user experience.
Community health volunteers (CHVs) were instrumental in purposively selecting women and girls in their third trimester of pregnancy. Participants were recruited while in the health facility, at the marketplace and at their homes. A total of 86 women and girls were enrolled into the study from Suguta Mar Mar and Barsaloi (Fig1). The mothers were recruited from either the remote villages where they live or from the health centers where they seek antenatal services. Walking is the main mode of transport for those who opt to deliver at a health facility. Walking distance can range from 2 km, for those who live close to the town centers, to 20 km, for those who live further away. Those with financial resources can use motorcycles or public transport (ie minivans) to travel to the health facility. However, those who use public transport must walk a considerable distance from their homesteads to the main road to board a vehicle. Mothers who had used the county ambulance indicated that they did so in emergency cases.
The second criterion of selection of mothers was based on owning or having access to a mobile phone with a Safaricom SIM card. Those without phones stated that they had access to their husband’s phones. Once enrolled, the mothers were trained to make payments using the wallet. Ambulance drivers from Suguta Mar Mar health facility, Barsaloi Public Health Center and Barsaloi Mission Hospital were trained to process payments using the Surepay wallet. When childbirth was imminent, the mothers were to contact the CHVs or the ambulance drivers. The ambulance driver would then transport the mothers to the hospital and bill them using the Surepay system before transporting them home (Fig2).
The billing process involved the ambulance driver initiating the Surepay payment process by phone. Subsequently the expectant mother received a pop-up message requesting her to enter her PIN to accept the billing. In the case of a failed transaction the ambulance driver would make the payment request again.
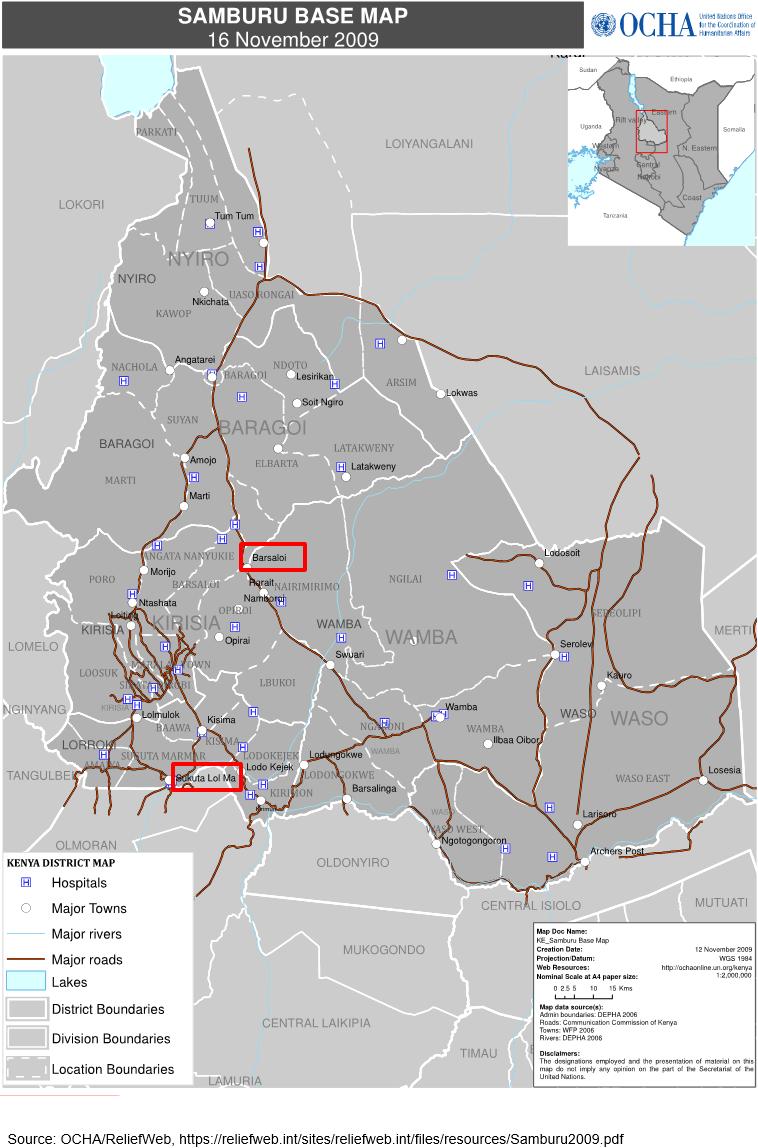 Figure 1: Barsaloi and Suguta Mar Mar town in Samburu County, Kenya.
Figure 1: Barsaloi and Suguta Mar Mar town in Samburu County, Kenya.
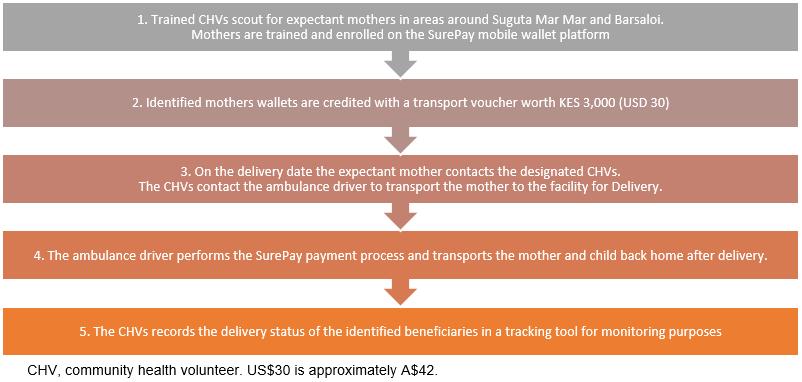 Figure 2: Mobile transport voucher process flow.
Figure 2: Mobile transport voucher process flow.
Methods
The design for the research component of this project was a combination of quantitative and qualitative methods. Quantitative data collection methods included a baseline survey to find out the number of children the mothers had and the place where they last delivered, Surepay data on the number of transaction attempts before successful billing, and a user experience survey of those who enrolled in the project. The user experience survey relied on a sample size of 50 beneficiaries, of whom 46 were actually interviewed (34 from Suguta Mar Mar and 12 from Barsaloi). Systematic random sampling was used to select the mothers to be interviewed from the list of 86 participants enrolled in the project.
A structured questionnaire with closed questions was used to collect the survey data. Due to the remoteness of the study area, the researchers relied on phone-based interviews as the main data collection method for both study areas. Respondents who were selected and not available during the phone-based interviews were replaced by those who were available. Qualitative data was collected through in-depth face-to-face key informant interviews with CHVs and the ambulance drivers using an open-ended interview guide. These interviews were to find out the technical usability of the Surepay wallet by investigating if the participants understood the training on use of the transport voucher, their ability to carry out transactions without the assistance of the ambulance driver and the CHVs and challenges experienced while implementing the project.
The researcher conducted a thematic narrative analysis of the qualitative data. Descriptive statistics such as percentages and frequencies were conducted on the quantitative data collected from the baseline and user survey. The results were presented using bar charts and tables. Due to the small sample size of this study, no attempt was made to analyse data beyond descriptive statistics.
Ethics approval
For this project no approval by an institutional research review board was needed, because it was a quality improvement of existing services and no samples were required from human subjects.
Results
Effect of Surepay transport vouchers on skilled delivery
In both Suguta Mar Mar and Barsaloi, the transport voucher proved instrumental in aiding mothers to access healthcare facilities for skilled delivery (Fig3). Sixteen of the 53 (30%) enrolled mothers in Suguta Mar Mar reported previous delivery at a health facility. After the introduction of the mobile transport voucher, this number increased to 52 (98%). Only one participant from Suguta Mar Mar did not use the transport voucher. This was because the ambulance driver was not available when she was ready to deliver. In Barsaloi, 18 (55%) of those enrolled had their previous delivery at home. Ten (30%) had their previous delivery at the Barsaloi public health facility or mission hospital. These women and girls resided close to Barsaloi town. The remainder (5, 15%) were expectant for the first time.
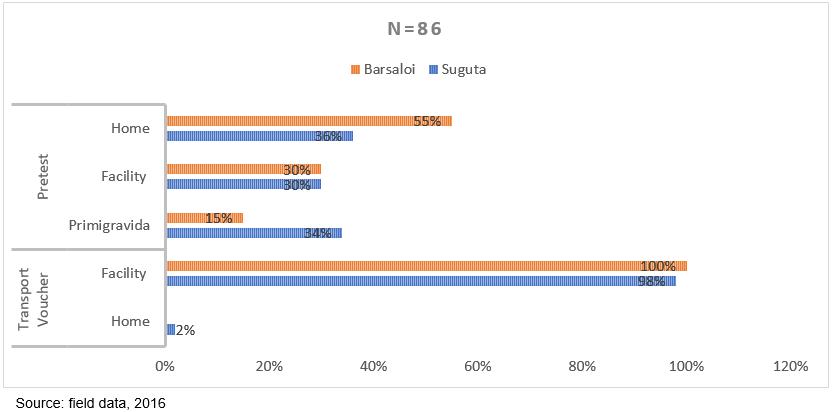 Figure 3: Place of delivery pre-test and during test period.
Figure 3: Place of delivery pre-test and during test period.
Technical usability and challenges of the Surepay transport voucher
The Surepay voucher transaction process, where the ambulance driver initiated the payment process and the expectant mother was to enter her PIN, proved challenging to more than half of the mothers. There were several cases where participants did not remember their PIN, or did not enter it quickly enough. Also, there were fluctuations in network availability in a few instances, resulting in transaction failure (Table 1).
Despite these challenges, 28 (61%) of participants stated that the transaction process was very easy. The CHVs and the ambulance driver, however, felt that participants needed more training on how to use the wallet. This was because they were trained in different periods of their third trimester. Those who used the mobile voucher a few weeks after training had fewer challenges than those who used it months later. Furthermore, several PIN resets had to be carried out later in the project. CHVs and ambulance drivers had the opinion that the platform should be PIN-less to allow those who had difficulty remembering their PINs to accept transactions.
Table 1: Number and cause of failed Surepay transactions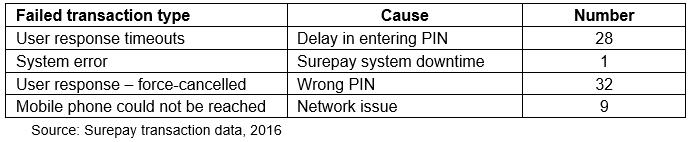
User experience
When asked if they would ever save money for transport to the health facility in the Surepay wallet, 43 (93%) of the mothers interviewed indicated that they were willing to do so. The mothers stated that compared to the usual mobile money they found the Surepay platform secure, thus they could not deviate funds for other uses. The 3 (7%) who were not willing to save indicated that they had difficulty in understanding the system due to illiteracy or indicated that the ambulance was unreliable thus were not willing to save up for transport they would not use.
Several limitations were experienced when implementing the transport voucher. This included lack of phone ownership, unavailability of the ambulance in a few instances, poor network and illiteracy. A total of 22 participants who did not own mobile phones were enrolled in the program. They were mainly from the Barsaloi area. The mothers were enrolled using their husband’s phone or those of other next of kin. Some husbands (three) were unwilling to have their phone used for billing during transportation even though the same phones were used to register the participants.
Discussion
The key assumption of the project was that because mobile technology has penetrated the remote Samburu County, payment for services using mobile phones would be relatively easy among participants and therefore Surepay mHealth vouchers would be readily adopted by pregnant women, because these involve fewer processes compared to existing mobile payments. This however appeared to be not straightforward. The project showed that the success of transport vouchers was merely due to the adoption and promotion of the technology by the ambulance driver and the CHVs. Resource challenges within the households, as well as illiteracy, were intervening variables that negatively impacted on the adoption of vouchers by participating women. The project also shows that technology diffusion in remote settings encounters visibility challenges. It is likely that the mothers recruited in the project rarely use mobile payment services and thus introducing the mHealth transport voucher was not compatible to existing practices and therefore considered complex.
Based on Jillo et al’s study on improving access to delivery and neonatal health care, mothers in remote pastoral communities only resort to formal healthcare services in the event of complications3. The mobile transport voucher changed this trend among mothers who were enrolled in the present study. This study builds consensus with Obare et al’s study on reducing financial barriers to accessing health care by use of vouchers4. The enrolled participants do not wait for an emergency case to use the Surepay transport vouchers – they willingly use it because it enables them to access a health facility at no cost.
Strength of the project was its rapid operational rollout and practical use, resulting in almost 100% of pregnant women and girls delivering at skilled facilities. The research design was focused on documenting this intervention, mostly qualitatively, in terms of operational feasibility and user experience. The quantitative data collected in this project are based on small numbers and should therefore be considered with caution.
Conclusion
Facilitation of transport to healthcare facilities for delivery using digital mHealth transport vouchers resulted in almost 100% of mothers taking up skilled delivery at a health facility. Technical usability was demonstrated and user experience was exclusively positive. It was demonstrated that, with access to safe transportation, mothers in the remote settings of Samburu were able to take up delivery in health facilities rather than only seeking delivery at a health facility in case of complications. Success in use of the Surepay transport voucher appeared to be due largely to the efforts by the CHVs and the ambulance driver, who are regarded as being the main communication channels or agents in the use of the mobile voucher technology.
For future policy, implementing mobile transport voucher programs in remote settings should involve the identification of the most effective communication agents so that technology can be adopted successfully. Moreover, due attention should be given to educating participants in the use of mobile phones for payment, particularly in areas with higher illiteracy rates. Involving women and girls at an earlier stage of pregnancy (first trimester) is recommended, in order to get acquainted with the new technological opportunities. Subsidization of transportation costs to the health facility remains a challenge.
References
You might also be interested in:
2015 - Re-orienting a remote acute care model towards a primary health care approach: key enablers
2014 - Sudden collapses in the heat in patients on angiotensin type 2 receptor blockers