Introduction
The Solomon Islands is an archipelago in the Oceania-Melanesia region and has a population of 595 0001,2. The female population is 250 000 and there is a relatively high proportion of child-bearing age women, numbering approximately 180 0003,4. Although more than three-quarters of the population are rural dwelling1, specialist services are concentrated in the capital city of Honiara, where all seven of the country’s obstetricians and gynaecologists are located. Generalist medical officers service the provincial hospitals, and women who require specialist obstetric and gynaecological services are referred to Honiara. Obstacles presented by limited transport and financial costs can have an indirect negative impact on health outcomes for these women2,5.
Gizo is located within Western Province, geographically the largest province of the Solomon Islands. Western Province has the third largest population and comprises approximately 37 000 women3. Western Province has a higher percentage of the population with primary school education and an equivalent percentage of the populace with secondary and tertiary education as compared to the rest of the country3. Outside the city of Honiara, Western Province has the largest English speaking population in the Solomon Islands3. Western Province enjoys the highest female employment participation rate, after Honiara3. Despite this, women in the Western Province commonly report difficulties accessing medical care as a result of treatment-related costs5.
There is limited data on the maternal and reproductive health profile of women in Western Province, particularly concerning specific diagnoses and respective modes of treatment. Local data of this type are critical to effectively guide resource allocation and foreign aid, and to direct the training needs of doctors6. Information of this type also enables upskilling of the local workforce, which contributes to capacity building and increases options and level of care available for women in the Solomon Islands. A recent report by WHO described a median age at first birth of 22 years, a fertility rate of four births per woman and a contraceptive prevalence of around 35% within the Solomon Islands7. Unmet family planning needs in Western Province are thought to be around 9%5. In Western Province around 95% of women receive some antenatal care and 92% deliver in a healthcare facility5. During the 2007 Solomon Islands Demographic and Health Survey more than 30% of women aged 49 years reported being menopausal5.
The present study describes the gynaecological presentations occurring in Western Province during a 6-day visit by volunteer gynaecologists from Australia to Gizo Hospital. Gizo Hospital is the only hospital in Western Province and comprises 52 inpatient beds, three wards, an emergency department and a labour ward. Local medical staff at Gizo perform uterine curettage, removal of intra-uterine devices, caesarean sections and mini-laparotomies for tubal ligation or treatment of ectopic pregnancies, and 195 such cases were performed in 2017. Patients who require more complex surgery are referred to the National Referral Hospital in Honiara. Histopathology is not requested for all excised tissue; however, if there is clinical concern for malignancy or need for specific tissue diagnosis, samples can be sent via commercial flight to Brisbane, Australia (Queensland Health Pathology and Scientific Services, Royal Brisbane Hospital, Queensland) and reviewed in clinic at Gizo. Histopathology results are typically obtained within 6–9 weeks.
Volunteer gynaecologists were working on behalf of Doctors Assisting in Solomon Islands (DAISI), a non-profit organisation that has been operating since 2014. The organisation donates medical equipment to hospitals in the Solomon Islands and collaborates with local doctors to increase operating capacity and the surgical skills of local providers both in Honiara and in provincial centres. Donations to DAISI are used to provide medical equipment, and all team members fund their own travel and accommodation costs8. Gizo Hospital has collaborated with DAISI on multiple surgical programs. The gynaecology program is new to DAISI and Gizo, and the first collaborative program occurred in 2017.
This study addresses a gap in the literature by profiling gynaecological presentations occurring in Western Province during a 6-day visit in 2017 by volunteer gynaecologists from Australia. Demographic information for each type of presentation and descriptions of all gynaecological surgeries performed and their associated short-term surgical outcomes are provided.
Methods
The study describes a case series of surgeries performed at Gizo Hospital in Western Province, Solomon Islands. The planned arrival of gynaecologists was broadcast on regional radio stations and newspapers, following which women travelled from neighbouring islands to attend surgical screening. Screening was performed in the outpatient department of Gizo Hospital on 28 and 29 June 2017 by the gynaecology consultant and registrar from Honiara. Patients who were identified as surgical candidates were reviewed by an Australian gynaecologist on 30 June and surgeries booked as clinically indicated. Data were collected for all women who subsequently received surgery during 3–7 July 2017. The gynaecology team comprised two Australian gynaecologists, a specialist obstetrician-gynaecologist from the National Referral Centre in Honiara, Solomon Islands, two registrars (one Australian, one from the Solomon Islands), two Australian anaesthetists, three Australian medical students, and four theatre nurses from Gizo Hospital.
Data were collected on the medical history of the patients: age, gravidity, parity, mode of delivery, menstrual history, contraceptive use, history of sexually transmitted infection, history of cervical screening and past medical and surgical history. Examination findings included body mass index, abdominal examination and vaginal examination. Investigations performed included urine and blood tests and abdominal/pelvic ultrasound. Surgical data included type of surgery performed, anaesthetic used, estimated blood loss, intra-operative complications, surgical findings (including gross description of the pathology following excision and whether a specimen was sent for formal pathological assessment) and postoperative data (including instances of any postoperative complications, amount and type of analgesia used and length of hospital stay). Descriptive analysis of demographic and surgical data was undertaken.
Ethics approval
Ethical approval for the project was granted by the Solomon Islands Health Research and Ethics Review Board (HRE023/17).
Results
Patient demographics
Twenty-three patients were reviewed for gynaecological presentations between 30 June and 6 July 2017, and booked for surgery. Of these, 20 patients underwent surgery during 3–7 July 2017. Patient demographic details are displayed in Table 1.
The patients presented with a variety of problems (Table 2). The most common complaint was pain (n=20, 86%), including pelvic and abdominal pain, dysmenorrhoea and dyspareunia. The second most common complaint was abnormal uterine bleeding (n=19, 83%), including irregular bleeding, heavy menstrual bleeding and post-coital bleeding. Sixteen women (70%) presented with both pain and dysfunctional bleeding. No patients reported symptoms of anaemia. Four women presented with infertility.
Twenty patients (87%) had pre-operative trans-abdominal ultrasound performed by local sonographers in the hospital. Pre-operative haemoglobin was assessed on full blood count in 21 of the 23 patients (91%). The mean haemoglobin was 116 g/L (range, 70–144 g/L. No patients required pre-operative blood transfusion.
Table 1: Patient characteristics (n=23)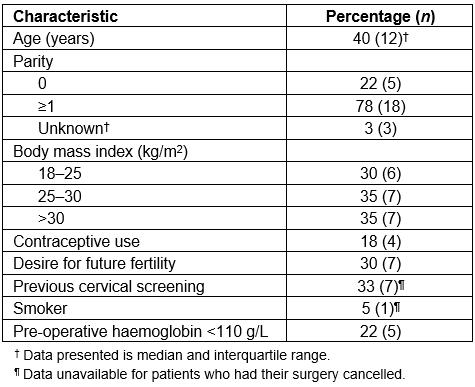
Table 2: Gynaecological presentations of patients (n=23)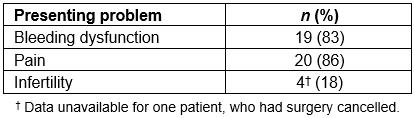
Surgeries performed
Twenty-nine surgeries were performed on 20 patients during the study period. Figure 1 summarises the types and frequency of surgeries performed. Diagnostic laparoscopy was performed in six patients, and operative laparoscopies were performed in two patients: adhesiolysis and diathermy, and excision of grade 2 endometriosis. Veress needle entry was attempted in all laparoscopies. Entry failed in one case due to a large uterine fibroid; Hasson technique was subsequently used. Minor procedures included dilatation and curettage of uterus (n=8), diathermy to cervix (n=2), diathermy to vaginal warts (n=1) and excision of a vaginal lesion. Six oophorectomies were performed; two of these were for ovarian cysts and were not accompanied by hysterectomy. Of the nine laparotomies, two were performed with midline vertical skin incisions and seven were performed with Pfannanstiel incisions.
All laparoscopies were performed under general anaesthetic. The vaginal cyst excision was performed under local lignocaine injection. The remaining surgeries were performed under spinal block.
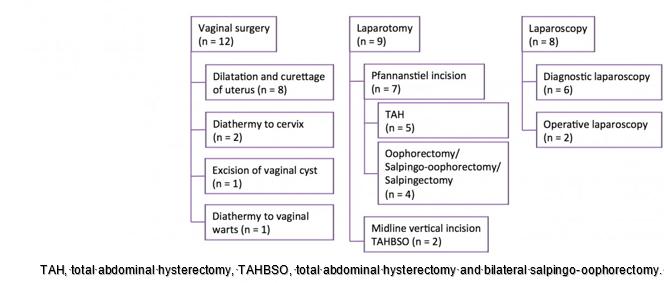 Figure 1: Types and frequencies of reviewed surgeries performed.
Figure 1: Types and frequencies of reviewed surgeries performed.
Surgical cancellations and complications
Three patients had their surgical booking cancelled. One cancellation was due to patient preference. Two cases were cancelled due to the patients having dengue fever with associated thrombocytopenia. One patient was known to have dengue fever at the time of booking and thus surgery was intentionally booked for the end of the operating week; however, repeat platelet count had dropped to 31×109/L. She was instead scheduled for follow-up in Honiara for a cone biopsy and uterine curettage for known cervical intraepithelial neoplasia. The second patient was booked for a hysterectomy for heavy menstrual bleeding secondary to a fibroid uterus and her surgery was cancelled because she developed dengue fever whilst awaiting surgery.
One intra-operative complication was identified. This involved an air embolus, which caused a cardiac arrest. The surgery was stopped following incision of the skin and the patient was successfully resuscitated. The patient was aged 41 years, 12 weeks pregnant and booked for a mini-laparotomy for persistent pelvic pain and an 8 cm ovarian cyst. She was successfully resuscitated and discharged home after 4 days, with no ongoing sequelae. Foetal viability was confirmed prior to discharge.
The median estimated blood loss during the procedures was 10 mL (interquartile range (IQR), 245 mL). No patients required intra-operative or postoperative blood transfusion.
Surgical pathology
Specimens were excised from 18 patients. Eleven specimens from 10 patients (61%) were fixed, then sent to Australia for histopathology. These included seven uterine curettings, a pelvic biopsy thought to be endometriosis from a patient aged 26 years, a 12 cm right ovary with a presumed teratoma from a patient aged 21 years, and a 12 cm para-ovarian cyst with torted right ovary and fallopian tube from a patient aged 34 years. Figure 2 shows sections of a degenerating cystic uterine fibroid following a total abdominal hysterectomy and bilateral salpingo-oophorectomy performed on a patient aged 44 years. Dimensions of the first specimen were 27 × 16 × 14 cm and the largest fibroid was 10 × 9 × 7 cm.
Eight out of eleven specimens were appointed a diagnosis by Australian laboratories within 3 months of the surgery. Six specimens were uterine curettings, all of which were benign. The pelvic biopsy showed a benign mesothelial inclusion cyst with focal salpingosis. The ovarian teratoma was confirmed and the large fibroid demonstrated degenerative change without necrosis or evidence of malignancy.
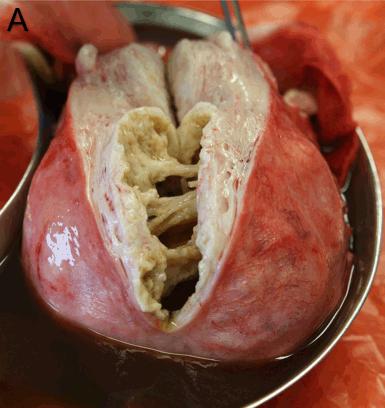

 Figure 2: Pathology specimens: (a) large multifibroid uterus with cystic degeneration (sent for histopathology); (b) large fibroid uterus (not sent for histopathology); (c) large ovarian teratoma with evident hair, cartilage and fat (sent for histopathology).
Figure 2: Pathology specimens: (a) large multifibroid uterus with cystic degeneration (sent for histopathology); (b) large fibroid uterus (not sent for histopathology); (c) large ovarian teratoma with evident hair, cartilage and fat (sent for histopathology).
Postoperative outcomes
No postoperative complications were identified. The available postoperative analgesia included paracetamol, non-steroidal anti-inflammatory drugs (NSAIDs, which were oral indomethacin or magnesium trisilicate) and opioids (subcutaneous injection of morphine or pethidine). Remarkably, 5 of the 20 patients did not use any analgesia, while six patients used paracetamol and/or a NSAID, and nine patients used opioid analgesia.
The median duration of postoperative hospital admission was 2 days (IQR, 1 day). One patient was discharged home on the day of surgery. The lengthiest post-operative admission was 4 days. All patients who had laparoscopies were discharged home the following day. The median length of stay for the patients who had laparotomies was 2.5 days; three patients who had hysterectomies were discharged home on day 2 postoperatively, and four were discharged after day 3.
Discussion
There are significant challenges in providing gynaecology surgery services in the Pacific Islands. This case series demonstrates the feasibility of volunteer gynaecology teams conducting surgery in the Solomon Islands, in partnership with the regional hospital facilities, and in accordance with the needs of the local population.
Case series population
The population of patients were mostly young, with only one postmenopausal woman booked for surgery. There were no adolescent presentations. The median parity of three in the cohort is lower than that reported by WHO6; however, 30% of patients reported a desire for future fertility. This is consistent with the lower contraceptive prevalence in this population, which is almost half that reported by WHO7. Furthermore, the high prevalence of obesity in this study is consistent with previous reports of Pacific Island patients9-11.
Facilities for surgery
The facilities available at Gizo Hospital were sufficient for major and minor gynaecological surgery. Some investigations were readily available, including ultrasound and full blood count. However, because of the remote setting of the hospital, these resources were dependent on the availability of a few technicians. Further, there was no vaginal ultrasound probe and all ultrasounds were performed via transabdominal examination. Although no patients required blood transfusion, cross-matching facilities were available at Gizo Hospital. Beyond this, the specialised surgical equipment and laparoscopy stacks were made available through donations by DAISI, and may not be available at other facilities in the country. Laparoscopic surgery for gynaecology is a new procedure in the Solomon Islands and has been embraced with much enthusiasm by local gynaecologists. The advance of minimally invasive surgery in the Solomon Islands will allow common procedures that are currently done by laparotomy, such as tubal ligation and ovarian cystectomy, to be performed laparoscopically, resulting in faster healing, less pain and reduced hospital stay. Further, other procedures such as tubal dye studies and resection of endometriosis may become available to patients in the Solomon Islands for the first time.
Impact of dengue fever on surgery
An interesting and unexpected finding was the frequency of dengue fever in this small sample, leading to surgery cancellation due to thrombocytopenia and associated operative risks. Although there are no other published articles describing the rate of surgery cancellation due to dengue fever, doctors local to the Solomon Islands anecdotally identify this as a common problem. Further studies will be required to assess this secondary impact of dengue fever on healthcare provision and use of resources.
Surgical outcomes
Overall, surgical outcomes in this case series were equivalent to those in Australia. Use of spinal blocks as anaesthetic for all laparotomies provided effective analgesia and safely allowed a shorter duration of monitoring in the recovery bay. The only identified complication of air embolism was serious but reversible. Incident reporting was carried out for this instance and the Director of Medical Services was notified. As a result, recommendations to voluntary operating teams organised by DAISI now include on-site advanced life support simulation training.
Histopathological processing facilities continue to be limited. Careful consideration was needed when sending operative specimens for histopathological examination as this required specimen transportation to Brisbane, Australia. In the case of a huge multi-fibroid uterus with cystic degeneration, only part of the specimen was sent for histopathology despite the small risk of sarcomatous transformation in the specimen portion that was not sent.
Multiple options were available for postoperative analgesia, and combinations of different drugs were readily available for use. An increased length of stay was noted in this population – all patients were admitted 1 day prior to the day of surgery in order to ensure timely attendance and appropriate fasting. Laparoscopic patients were discharged the day after surgery. Patients in Australia who have diagnostic laparoscopies or minor operative laparoscopies would typically be discharged on the day of surgery. The increased length of stay in the Solomon Islands may be beneficial for a mobile population as the patient may not be able to easily access care if a complication became evident in the early postoperative period. The postoperative length of stay for the laparotomy cases was similar to the postoperative length of stay of open hysterectomy cases in Australian hospitals, which is 2.7 days12.
Integration with local health services
Collaboration with local doctors from the Solomon Islands was helpful in all aspects of care provided. This extends from the initial screening of patients, familiarity with available resources and hospital processes, to removal of a language barrier when seeing patients and increased rapport and trust between the patient and healthcare team. Also, postoperative follow-up of patients and histopathology can be provided by a member of the operating team in Honiara. In addition, the gynaecologists from Honiara can make arrangements for patients who had their surgeries cancelled to be reviewed and have the procedure rebooked.
Ongoing collaboration between Australian and Solomon Islands gynaecology specialists and specialist trainees can help to build sustainable gynaecology services that include minimally invasive surgery in both the National Referral Centre and provincial hospitals. The Pacific Islands Project, organised by the Royal Australasian College of Surgeons, has demonstrated that it is feasible to develop locally trained surgeons. This serves as a model for training in laparoscopy both for general surgery and gynaecology13. In such a way, the interaction between donor and recipient countries should be as equals – mutually beneficial and conducive to growth14.
Limitations
This study is limited by the small sample size, which means that the results may not be generalisable to the population of the Solomon Islands. Furthermore, there may be a selection bias as patients self-referred to the gynaecology service. Thus the population described may be more likely to be engaged with the health care service and to have had cervical screening, previous surgery, and be less likely to smoke.
Conclusion
This case series serves to demonstrate the feasibility of providing gynaecology surgery services to remote areas of the Pacific Islands, working together with local facilities and health workers. It additionally provides information, on cases encountered during a voluntary gynaecology operating visit, that will be useful in assisting future volunteer groups in preparing for surgery trips to the Pacific Islands.
Acknowledgements
The authors thank the patients who were included in this study as well as the medical and nursing staff of Gizo Hospital. In particular we would like to thank Dr Leeanne Panisi, Dr Dickson Boara and theatre nurses Joyce, Patricia, Viola and Clayton. We would also like to thank Dr Gary McKay and the team at DAISI for organisational support for the visit during which this study was performed.
