Introduction
According to the European Union’s rural development policy, the regions within every country can be classified as either urban or rural. Bosnia and Herzegovina (BiH) is one of the most rural countries in Europe, with the OECD’s definition placing it fourth, after Finland, Ireland and Montenegro1. The rural regions encompass small towns (several thousand inhabitants) and villages that are notably dissimilar to and disadvantaged compared to the urban areas2. The available data suggest that the percentage of the population living in rural regions has been nearly constant over the past 30 years, showing a minor rise from 60.5% to 60.8% from 1991 to 2007, and then declining to 60.4% by 20102.The levels of outmigration to the urban areas or abroad as well as the unemployment rate are high2. Rural regions are predisposed to have a more aged population and therefore contribute significantly less to the national budget than their urban counterparts.
A World Bank survey conducted in 1999 found that appropriate health care is available to only 28% of the rural population in Bosnia and Herzegovina, while 13% have a pharmacy in close proximity. Lack of qualified physicians/nurses and equipment in rural regions was also reported3. The most important priority for study participants was health care, with 73% of households identifying the need for essential changes to the healthcare system4. In a reform of the healthcare sector, the government proposed the development of a new primary care model in 2001, oriented toward family medicine5. The reform focused on strengthening the gatekeeping system of primary care, providing continuity of care, increasing the autonomy of choices to patients and establishing an improved primary healthcare infrastructure6. The emphasis was placed on family medicine teams, consisting of one family physician and one or two nurses, responsible for providing primary care to a certain number of patients (1500–2000). At the beginning of reform, the majority of physicians practising in rural areas were specialty physicians (pediatricians, dermatologists, internists and gynecologists). Certified family physicians, however, were few. To overcome the workforce shortage, distance, time and cost of traveling to urban health centers, the capacity of rural physicians to deliver comprehensive care was planned to be expanded in the course of additional training or residency in family medicine. The curricula included public health issues, clinical procedures, various encounter situations, emergencies and palliative care.
Bosnia and Herzegovina is divided into two entities. The smaller entity, the Republic of Srpska, has a centralized healthcare system, financed by the entity government through entity insurance funds. The second entity, Federation of Bosnia and Herzegovina, has a separate system of financing and a decentralized cantonal system, with each of 10 cantons being responsible for its healthcare administration. Primary care centers are owned by municipal governments within the cantons. Family physicians are mostly employed by primary healthcare centers, while less than 1% practice in private family medicine clinics6.
Previous studies showed that medical education can play an important role in the recruitment and retention of rural physicians7-10. In Bosnia and Herzegovina, there are six faculties of medicine. The Faculty of Medicine Foca was founded during the civil war, in a small town and rural municipality of the Republic of Srpska entity, placed near the border with Montenegro, by a group of professors who wished to provide the opportunity for medical education in the region. Hardships that were overcome during the founding and first years of the faculty were a lasting motivation for achieving goals in the future. Currently, the faculty is integrated into the University of East Sarajevo, along with 16 other faculties. It is one of few rural faculties of medicine in Europe. Academic study programs include medicine, dentistry, speech language pathology and nursing.
The literature indicates different factors influencing recruitment of health professional students to work in rural areas. In developed countries, characteristics of students11, growing up in a rural location12, financial incentives13, professional/personal support14, exposure to rural practice during training15,16 and spouse’s occupation17 have been identified as being important determinants of intent for rural practice.
Recent systematic review, analyzing medicine students’ motivation to practise in rural regions of low-income and middle-income countries suggests that rural location of a medical school could influence students’ work choice 18. However, data to indicate whether determinants of rural career decision making found in international research could be applied to Bosnia and Herzegovina is limited.
The purpose of this study was to explore the willingness of health profession students in the Faculty of Medicine Foca to work in a rural area following graduation and the factors influencing incentives to pursue a rural career.
Methods
Study design and participants
The cross-sectional study was carried out in November 2017, at the beginning of the winter semester during the first required lecture for each year and study program class. The study included first-year through sixth-year students aged 18 years or more and enrolled in one of three study programs at Faculty of Medicine: medicine, dentistry and nursing. Research assistants comprehensively introduced objectives of the study to the students and explained that rejection to participate would have no scholarly consequences. Each student received a paper-and-pencil questionnaire. Verbal affirmation of study procedure and consent to participate in research were obtained before questionnaire completion. Written informed consent was not requested. The survey took about 10 minutes to complete. All personal data were anonymized. The questionnaires were numbered and analogized for data analysis. Neither financial nor non-financial compensation were provided.
The study was conducted according to the principles of Helsinki Declaration.
Instruments
Age, gender, place of birth, year of study, study program and place of living were surveyed for social background.
The seven-step process, described in guide 87 of the International Association for medical education, was used to design and develop the self-administered questionnaire19.
Prior to implementation of the full study, pilot testing was conducted to identify potential problem areas and deficiencies in the questionnaire. The respondents selected for the pilot testing were representative of the students to be surveyed in the main study from Bosnia and Herzegovina (25 students) and Croatia (36 students). Members of the representative population completed the survey in the paper-based format. The final version of the questionnaire consisted of 19 items. The response options to be used for each item were selected. The first item was the dichotomous (yes/no) question ‘When you complete your studies, would you be inclined to accept a job in a rural region?’. Eighteen items exploring the reasons for accepting or not accepting a job in a rural setting were rated according to a five-point Likert-type scale. The students were asked to complete the task by circling the answers that best applied to them on the scale ‘strongly disagree’ (1), ‘disagree’ (2), ‘neutral’ (3), ‘agree’ (4) and ‘strongly agree’ (5). The reliability analysis was conducted by calculating a Cronbach’s alpha coefficient. Its value of 0.859 was found to be satisfactory. The questionnaire was in Bosnian but, for the purpose of the current article, the questions were translated into the English language.
Statistical analysis
Statistical analysis was performed using the Statistical Package for the Social Sciences v20 (IBM; http://www.spss.com). Means (± standard deviations) for continuous variables, and numbers and percentage for categorical variables, were used to present responses. The differences between means were analyzed using student t-test or analysis of variance when appropriate. Categorical variables were tested using the Kruskal–Wallis test. Factors significant in the univariate analysis were entered into a multivariate logistic regression model predicting willingness to practice in rural area. P-values less than 0.05 were considered significant.
Ethics approval
The research protocol was approved by the Ethical Committee of the Faculty of Medicine Foca, University of East Sarajevo, under the registration number 01-190 /17.
Results
Out of the total 588 invited students, 519 agreed to participate in the survey and completed questionnaires (response rate 88.3%). Among them, the majority were female (71%) and studied medicine (61%); the average age was 21.45±2.43 years (Table 1).
Seventy-seven percent (399) of participants responded positively to the question ‘When you complete your studies, would you be inclined to accept a job in a rural region?’ Statistically significant differences in response to this question were found by gender (p=0.027), rural upbringing (p=0.037) and study program (p=0.010), but not by year of study (p=0.458).
Health profession students’ opinions are summarized in relation to incentives affecting their choice to pursue a rural career (Table 2). Respondents indicated that getting into the residency program more easily (4.03±1.14) and opportunities to attend paid international courses (4.03±1.01) would be among the most important incentives to accept employment in rural practice. The highest mean was linked to ‘possibility to move from rural to urban practices in the future’ (4.08±1.08), and the lowest to the ‘opportunity to support actions and conditions conducive to health (3.37±1.29). In the students’ opinion, willingness to work in rural practice would increase if there was a possibility for admission to fully funded doctoral education (3.99±1.18). A salary higher than in urban areas (3.74±1.15) and free housing provided by employers (3.93±1.07) were considered as motivating factors to practise in a rural area, next to non-financial incentives, such as primary school (3.98±1.17) or after-school program accessibility (3.82±1.16) for children and the factors facilitating professional development.
Significant differences between medicine (4.19±1.09), nursing (3.58±1.19) and dentistry (3.89±1.16) students were found in relation to the opinion that willingness to work in rural practice depends greatly on the possibility of getting residency more easily (p=0.001). Compared to their peers, nursing students scored better opportunities to attend national courses cost-free (4.13±0.99, p=0.027) and to be involved in the education of new generations of health profession students (4.10±1.10, p=0.001). Getting a post in an urban area after a work period in a rural area was most valued as an incentive by dentistry students (4.21±0.94, p=0.037) (Table 3). Significant differences in students’ opinions were not found in relation to year of study, except for possibilities to attend national congresses cost-free (p=0.004), and job opportunities for spouses (p=0.034) (Table 4).
The multivariate logistic regression model was used to analyze predictors of willingness to practise in rural areas. Students who had been raised in a rural community (p=0.042) as well as female students (p=0.016) were more likely to have intent for rural practice. Statistical significance at an alpha level of 0.05 was not reached in terms of study program and year of study (Table 5).
Table 1: Demographic characteristics of health profession students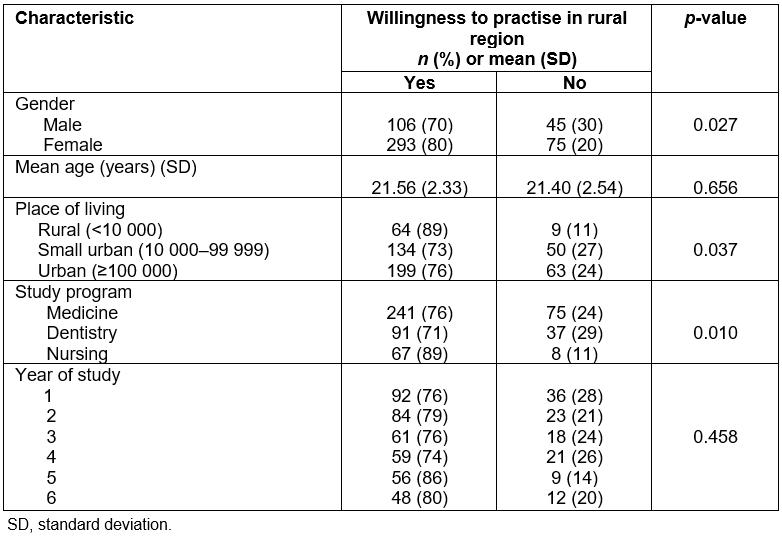
Table 2: Health profession students’ opinions of incentives to work in rural areas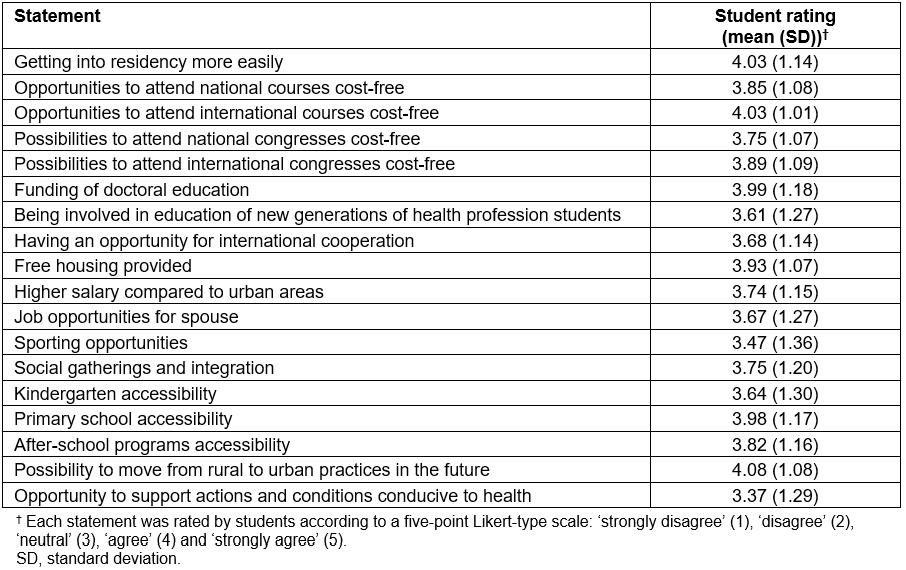
Table 3: Health profession students’ opinions of incentives to work in rural areas by study program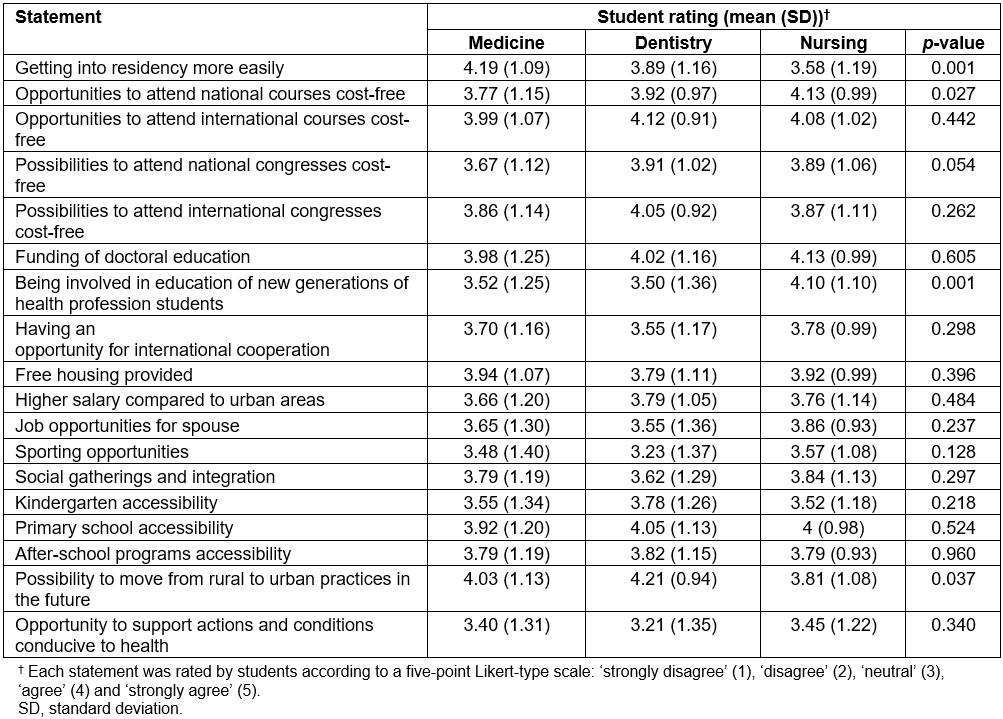
Table 4: Health profession students’ opinions of incentives to work in rural areas by study year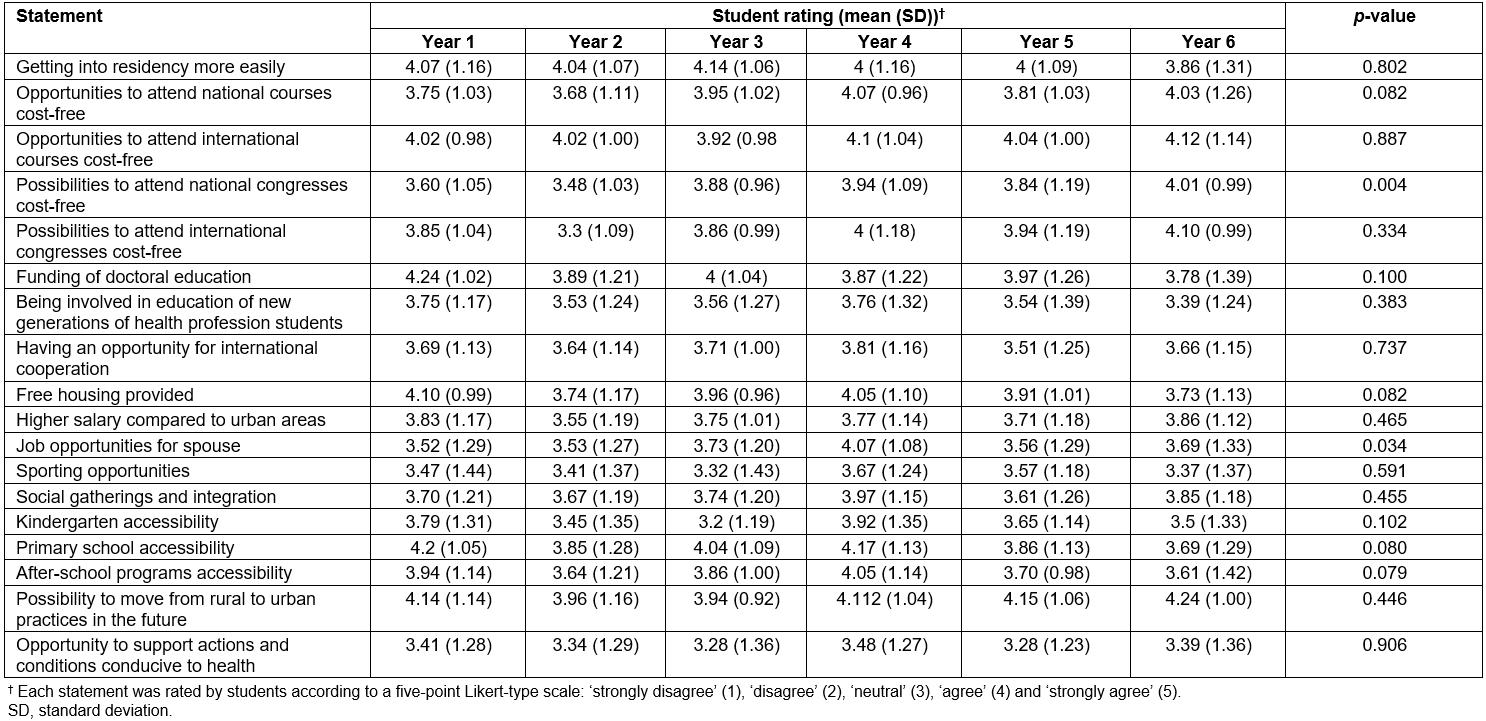
Table 5: Multivariate logistic regression analysis predicting willingness to practice in rural areas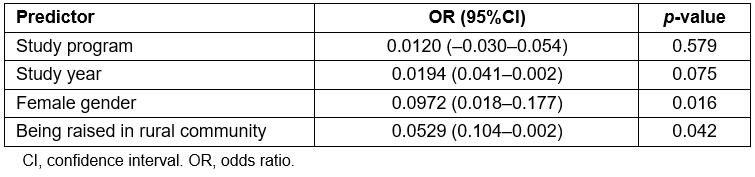
Discussion
This study demonstrates that the majority of health profession students at the Faculty of Medicine Foca are willing to work in a rural area following graduation. Alongside financial incentives, such as free housing or better salaries, various non-financial incentives for motivating students were identified. In line with previous studies, findings indicate that combinations of these incentives could improve the deployment of future health workers in rural settings13,20-24. A recent Chinese study found an association between satisfaction with educational scheme and positive attitude of the health profession students towards practising in rural areas25.
The aspect found to influence health profession students' willingness to practice in a rural setting was rural background. There is much international evidence of medical students with rural backgrounds being more likely to choose a rural career than students with urban upbringings13,18,24,26. This phenomenon is often called the rural background effect. Although the rural background effect is a strong, positive predictor of intent to enter rural practice, very little is known about its contributing factors. Almost half of the students enrolled in the current study have been raised and completed primary as well as secondary education in a rural area. The specific recruitment of students who live in a rural area does not exist at university level as found elsewhere27. Partnerships with secondary schools in rural communities, including presentation of university study programs every spring to senior students, are created. Over the past two decades, the government of the Republic of Srpska has been taking steps to ameliorate university attendance by offering free education, lowering tuition fees, scholarships, affordable dormitory housing and student restaurants, simultaneously making the recruitment of students with rural backgrounds less difficult. A high number of medicine graduates (from the Faculty of Medicine Foca) with rural backgrounds return to practise in rural communities and continue to practise in those areas for a long time. Several international studies on practice locations have found that medical students with a rural background continue to practise in rural regions for 10–16 years following graduation28,29. According to WHO recommendations, training health profession students with rural backgrounds in faculties of medicine located in rural regions, using rural health needs based curricula, increases the probability of graduates choosing to practise in rural areas22. Further research is needed to determine the level to which such interventions influence the motivation and retention of health professionals in rural areas.
Female students were more likely to choose to practise in rural settings compared to their male counterparts. Another study found that being male is related to a positive attitude toward a rural career30,31. In the past, male physicians mostly provided rural medicine, with the few female medicine graduates tending to practice in urban regions. Although the disproportion is still prominent for small and remote communities, the gap between male and female physicians has narrowed with time32. A recent study suggests that female medical graduates are more inclined to accept jobs in rural settings if the employees are flexible and supportive in regards to working hours33.
The possibility to move to urban practice after a period of service in a rural area was highly rated as an incentive by all health profession students and was particularly important for dentistry students. The most commonly recognized indicator of long-term rural retention for dental practitioners was prior training in rural setting34, while identified negative factors influencing the decisions to leave rural areas included limited access to social activities35, limited access to continuing professional development36, poor access to education for children37, own or family’s dissatisfaction with rural lifestyle38, and difficulties earning a sustainable income and offering quality lifestyles in rural areas39. These locally relevant factors need to be considered by employers when planning and designing recruitment/retention country-specific interventions.
Getting into the residency program more easily and faster after graduation had important influences on medical students’ willingness to practise in rural communities. In Bosnia and Herzegovina, residency is not mandatory yet. To obtain an occupational licence granted by a specified government-approved professional association, medicine and dentistry students take a general exam following graduation and become authorized to practise the profession. A physician who would like to pursue the residency in family medicine needs to be employed full time by a primary healthcare institution. A primary healthcare center signs the contract with the resident, stating that all administration fees as well as the doctor’s salary will be regularly paid until the resident passes the board exam in family medicine. After the resident has completed the training, he or she is obliged to return to the primary healthcare center (who financed his/her residency training) and practise there for at least 3 years (or time spent in residency training).
Many primary healthcare centers in Bosnia and Herzegovina, particularly in rural areas, experience financial difficulties. In addition to paying a resident’s salary, primary healthcare centers are expected to hire locum physicians and compensate for their work – which ultimately leads to the reluctance of employers to offer vocational training. Facing many years of waiting to progress in their careers highly demotivates young physicians, and they leave rural practice. In order to yield results, strategies to improve residency training accessibility need to be grounded in management systems23. Nursing students rated opportunities to attend international courses cost-free as a very important incentive for rural career intent. The nursing profession is still underestimated in Bosnia and Herzegovina, and nurses have fewer opportunities and support from employers for professional development. Previous studies found that access to professional development is an important factor contributing to nursing retention in rural areas40,41. To support recruitment and retention of rural nurses, WHO recommends continuing professional development programs that meet their needs, as the nurse practitioners with an extended scope of practice could provide health service delivery in areas with a shortage of physicians22. The opportunity to be involved in the education of new generations of health profession students was also rated highly by nursing students; therefore, involving rural health professionals with student teaching could be another effective recruitment and retention intervention41,42.
Although their effectiveness is not yet established, incentives found among medicine, dentistry and nursing students need to be considered by policymakers when planning the implementation of recruitment and retention strategies, with information regarding the relevance of the interventions and the mechanisms by which specific interventions were effective in some contexts but not in others43,44. Multi-sectoral collaboration between rural stakeholders, Ministry of Health of the Republic of Srpska and faculties of medicine is required. Research on processes of implementation and long-term sustainability of strategies to improve recruitment and retention should be conducted in the future.
Study limitations
Several limitations need to be considered. The findings could be specific to the Faculty of Medicine Foca, located in a rural area, and therefore may be different than other faculties of medicine in Bosnia and Herzegovina. Undergraduate curricula of the study programs include rural health topics which may have biased the sample. The study analyzed students’ willingness to practise in a rural area, not the choice of practice. Longitudinal studies to further explore factors that may mediate the health profession students’ willingness and choice to pursue the rural career are needed.
Conclusions
This study showed a high willingness of medicine, dentistry and nursing students to work in rural areas. Female students and students who were raised in a rural community were more likely to choose a rural career. Opportunities to access residency programs more quickly and easily impacts medical students’ career decisions related to rural practice. Medical schools exposing undergraduate students to rural community experiences should increase the provision of health workers to rural areas, as this could have a positive influence. Financial incentives, professional development opportunities and involvement in teaching may motivate dentistry and nursing students to consider practising in rural areas. Stakeholders and rural healthcare center managers should be committed to strengthening the rural deployment of health professionals by creating a more attractive, rural environment.
Acknowledgement
The authors thank the health profession students for completing the questionnaire.