Introduction
Korean public health doctors (PHDs) are required to provide public health services in medically underserved areas in accordance with Article 34(1) of the Military Service Act (2016) and Article 2(1) of the Act on Special Measures for Health and Medical Services in Agricultural and Fishing Villages, etc. (2016). All male citizens of South Korea aged between 18 and 35 years have to undertake national service duty by serving in the military or other public service duties, such as serving for 3 years as a PHD. PHDs in South Korea consist of medical doctors, dentists and oriental doctors.
Before 2000, PHDs were deployed only in public health subcenters (located in every si and gun – equivalents of large and smaller cities) and public health subcenters (located in most eups and myeons – equivalents of towns and districts) of medically underserved areas1 Later, in addition to working in public health subcenters, PHDs were also deployed in national health centers and county hospitals, private hospitals, correctional facilities, public health and medical research institutes operated by national and local governments. However, the number of medically underserved areas in South Korea has steadily decreased due to economic growth, an increase in the total number of doctors, and development of transportation2. Also, there has been a steady reduction in the number of PHDs since 2005 due to a change in the medical education system from undergraduate medical school to graduate medical school3,4, leading to licensure of doctors who completed the national service duty before they acquired their medical license. In the past, medical school was a 6-year course in the undergraduate system (directly into medical school after secondary school). Most opt to obtain a medical degree before undergoing military service to become PHDs or military doctors. Therefore, there was a need to efficiently utilize PHDs during their 3 years of service1,3.
Previous studies focused on the appropriateness and validity of placement of PHDs based on improvement of transportation and communication systems, development of rural areas (leading to a reduction in medically underserved areas) and reduction of the number of PHDs5. More specifically, the regulatory standards for the placement of PHDs were found to be very inadequate6. For example, some PHDs were placed in private hospitals for the purpose of maintaining emergency departments in medically vulnerable areas. However, within the hospitals, they were ‘relocated’ to outpatient clinics for more financial benefit of hospitals7. Most studies concluded that the regulations for placement of PHDs should be analyzed first, and that the appropriateness of tasks of PHDs be re-established5,8.
The change in socioeconomic and medical accessibility status of South Korea led to a reduction in the need for primary care provided by PHDs. For this reason, many Korean public healthcare professionals argue that the work paradigm of PHDs should shift from primary care to preventive medicine and health care8-11. They also argue that the core role of PHDs should not be to compete with the private clinics8,9, and should be more geared towards public healthcare policy and patient education for the general public8. Based on these previous studies, the purpose of this study is to survey PHDs to investigate the appropriateness of tasks of PHDs.
Methods
This study was a collaborative work between the Korean Association of Public Health Doctors and the Research Institute of Healthcare Policy under the Korean Medical Association. A quantitative survey study was used to investigate the hypothesis.
Participants
Participants included were current PHDs as of January 2017. The Korean Association of Public Health Doctors has a secure database of demographics of current PHDs. Only medical doctors were included, excluding dentists and oriental medical doctors since the tasks of medical doctors are unique. The total number of eligible participants was 2138.
A similar survey study was performed in 2011. Based on the survey questionnaires, questions were modified and added that would focus more on the appropriateness of tasks of PHDs. These questions focused on placement, task, education and satisfaction of PHDs. There were 35 major. For some questions, a series of logical questions were asked based on the response to the previous question. The survey was performed electronically through Naver Form and provided de-identified personal information to the researchers. The pre-survey was performed on eight participants and the survey questionnaires were subsequently modified based on their opinion. The survey was performed for 2 weeks from 16 January to 31 January 2017 by contacting participants electronically (text messages). The researchers had complete independence in the survey design, collection and analysis of the results, and writing of the manuscript.
Statistical analysis
Of the 2138 eligible participants, 1024 (47.9%) participated in the survey. Of those who participated, one was ineligible and eight were duplicate participants. Thus, 1015 participants were included in the statistical analysis. Participants who did not answer some questions were excluded from analysis for those questions. Quantitative data underwent unified coding and strict logical examinations. A Likert five-point scale ranging from 1 (‘very invalid’) to 5 (‘very valid’) was used. Statistical analysis was performed through SPSS v23 (IBM International; http://www.spss.com). Data were expressed as number (n), percentage (%) or mean and standard deviation (±SD).
Ethics approval
Current work is exempt based on American Association for Public Opinion Research 45 CFR 46.101(b) requirement criteria based on category 2, ‘research involving survey procedures, involving de-identified personal information’, and category 3, ‘survey of public officials’.
Results
The result of the general characteristics of participants is summarized in Table 1. The number of specialists was highest (55.2%), compared to general physicians (42.6%) and interns (2.3%). PHDs were distributed relatively equally between first and third year of service. Most were placed in inland villages (74.6%), with the rest located in inland cities (14.3%), connected islands (4.5%), and remote islands (6.6%). The most common type of workplace was public health subcenters (67.7%), followed by public health centers (12.2%) and national health centers and county hospitals (7.8%). PHD cited the presence of private hospitals and clinics within 5 km as 45.2% and 72.7%, respectively. In remote islands, there were barely any nearby hospitals (7.5%) and clinics (23.9%). Most public health subcenters had nearby hospitals (91.9%) and private clinics (98.4%).
PHDs’ validity of placement score was above midpoint (mean 3.4±1.1; Fig1a). PHDs working in national health centers and county hospitals (3.5±1.0) and public health subcenters (mean 3.4±1.1) scored the validity of placement as relatively high, while those in public health centers (mean 3.1±1.0) gave relatively low scores (data not shown). Based on the presence of nearby medical facilities (private clinics and hospitals), the validity of placement scored lower (means 3.3±1.1 and 3.2±1.0). The validity of number of PHDs placed was above midpoint (mean 3.4±1.1; Fig1b). PHDs working in inland villages gave high scores (mean 3.6±1.0), while those on remote islands gave low scores (3.2±1.2). PHDs working in public health centers (mean 3.0±1.0) and correctional facilities (mean 2.9±1.3) gave low scores, while those in public health subcenters gave high scores (mean 3.6±1.1).
Most PHDs performed, on average, 3.6 types of work (Table 2), mainly primary care (96.8%) and vaccination (85.8%). Less than half worked in public health care (35.7%), home-visit care (36.9%), patient consultation and education (36.0%), and diagnostic examinations (32.3%). Less common tasks included emergency care (19.8%), administrative duties (16.2%) and research (3.7%). PHDs on remote islands had the greatest number of types of workload (4.7 types of work), mainlyt primary care (100%), emergency care (89.6%), public health care (43.3%) and administrative duties (34.3%). PHDs working in public health centers also had many types of work (4.1 types). The proportion of public healthcare work in public health centers was higher than the overall average (50.0% vs 35.7%).
The validity of each task as perceived by the PHDs is shown in Table 3. The validity scores of primary care (3.5±1.1), vaccination (3.5±0.9) and patient education/counseling (3.4±1.0) were generally high. However, based on geographical location and type of workplace there were some discrepancies. For example, validity of primary care is higher than the average on remote islands (3.7±0.9), in public health subcenters (3.6±1.1) and in areas where there are no medical facilities within 5 km (3.6±1.1). Public health centers’ validity in providing primary care (3.2±1.1) is cited lower than that of remote islands. In general, emergency care (2.4±1.1), diagnostic exams (2.6±1.1), home-visit care (2.4±1.1), research activity (2.3±1.0) and administrative duties (1.9±0.9) were considered as less valid tasks for PHDs.
In the form of a multiple choice questionnaire, PHDs were asked their reasons for or against provision of primary care. The most common reason for supporting primary care was ‘provision of basic medical care’ (67.5%), followed by ‘lack of nearby medical facility’ (53.3%), and ‘medical care for specific population group’ (30.0%) (Fig2a). The most common reason against provision of primary care was ‘presence of nearby medical facilities’ (87.1%), followed by ‘not main purpose of public health facility’ (55.6%) and ‘need for efficient use of physicians’ (23.5%) (Fig2b).
Table 1: General characteristics of survey participants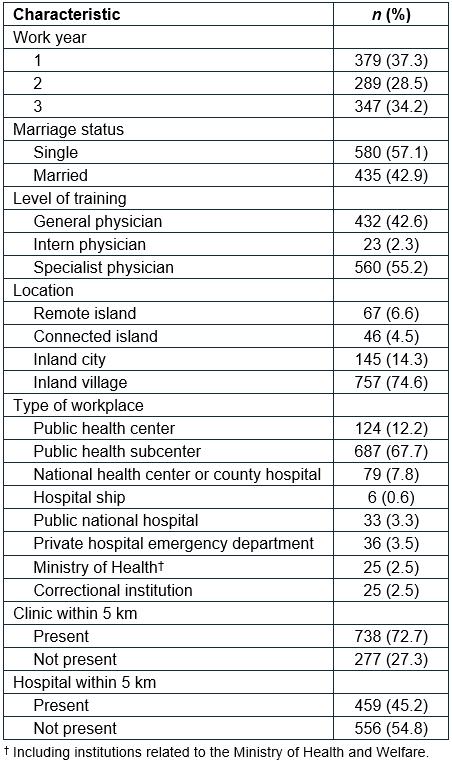
Table 2: Specific tasks performed by public health doctors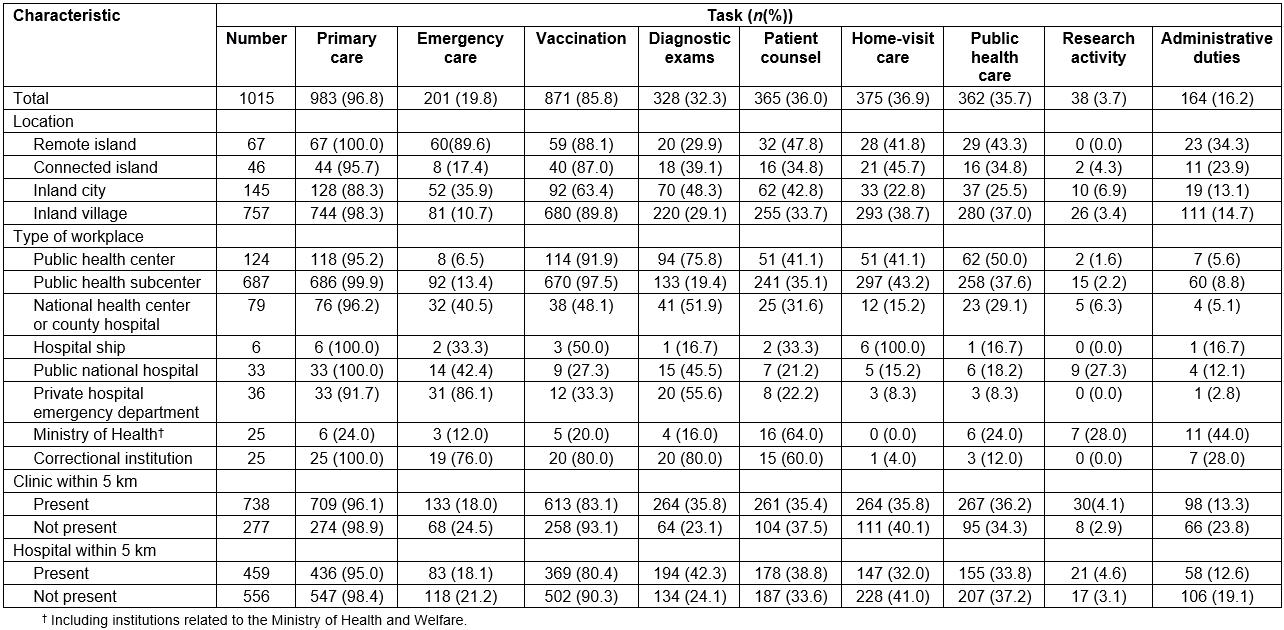
Table 3: Validity of specific tasks as perceived by public health doctors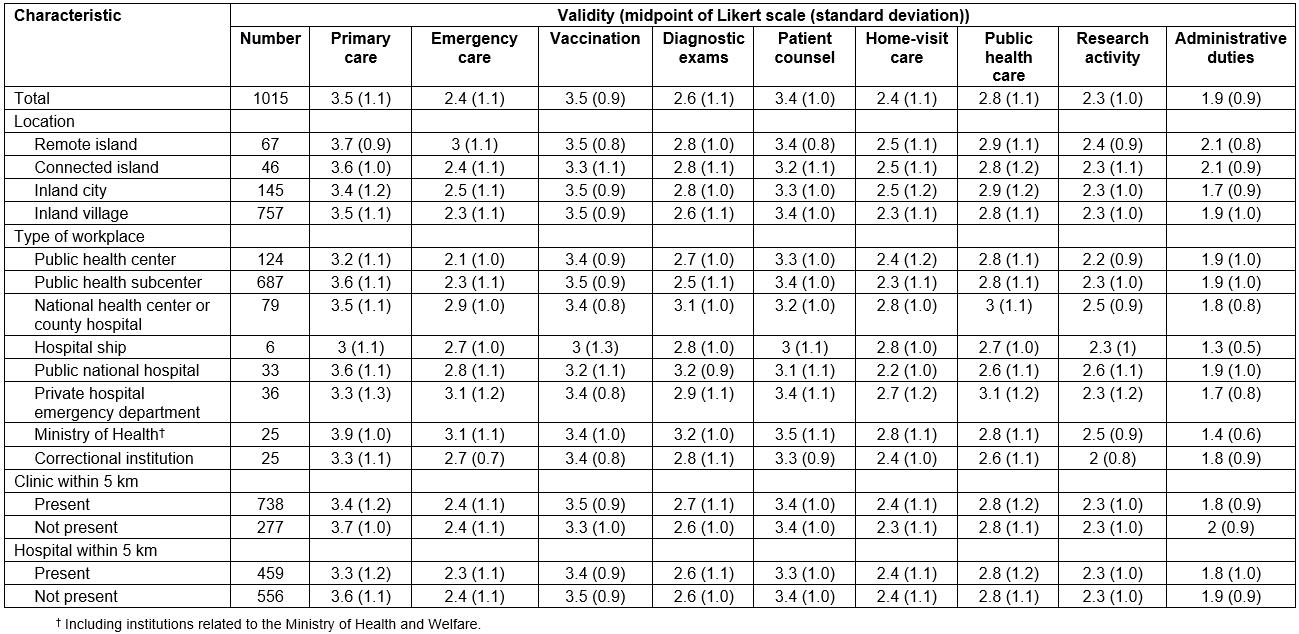
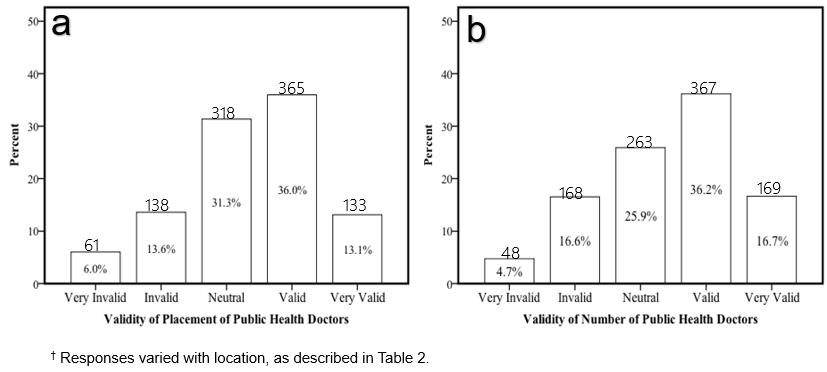 Figure 1: Public health doctors’ scoring for validity of placement and number of public health doctors.†
Figure 1: Public health doctors’ scoring for validity of placement and number of public health doctors.†
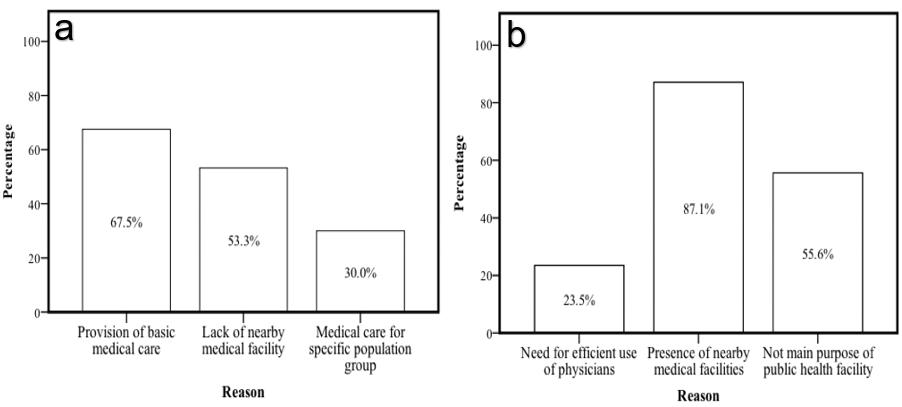 Figure 2: Public health doctors’ reasons for supporting or not supporting provision of primary care.
Figure 2: Public health doctors’ reasons for supporting or not supporting provision of primary care.
Discussion
Most PHDs were working in public health centers or public health center branches. Workplaces were mostly located in inland villages, with a minority located on remote islands (6.6%) or connected islands (4.5%). Work year was evenly distributed between 3 years, because the Ministry of Health and Welfare and Ministry of Defense coordinate the male graduates of medical school and residency programs in South Korea. PHDs are mostly general physicians (fresh graduates of medical school) or specialists (graduates of residency programs). The number of intern doctors consisting of doctors who have completed internships is small, mostly because these doctors are placed in military hospitals, instead of working as PHDs. Over 72% of all workplaces of PHDs had clinics within 5 km and 45% had hospitals within 5 km. In particular, over 90% of public health centers had nearby clinics or hospitals, whereas more than 92% of remote islands did not have nearby hospitals or clinics (76%). Of note, 98% of public health centers had nearby private clinics. Usually, private clinics have all the diagnostic testing equipment and personnel for an outpatient, ambulatory clinical setting. In Korea, the out-of-pocket expenses for medical service are less than for most OECD countries.
PHDs attested the validity of placement and the number of PHDs as being above midpoint. The validity of placement scored higher for those working on remote islands and in correctional institutions, while it scored lower for those in public health centers. However, the validity of number of PHDs was low among those working on remote islands and in public health centers. Currently, there are 54 remote islands, and most remote island workplaces have only two PHDs, leading to PHDs working over 84 work hours per week. This is above the government work-hour limit. PHDs in close proximity to private clinics or hospitals had a lower score of PHD placement and numbers. This suggests that more PHDs need to be relocated to true medically underserved areas, such as in remote islands.
Almost all PHDs perform primary care and vaccination. This suggests that, at present, PHDs are mainly working as primary care physicians. Generally speaking, public health facilities run by governments should be working for the wellbeing of society, for example in public health policy and infection control. However, South Korean PHDs currently working in public health centers are doing so as primary care physicians8. Validity of tasks performed by PHDs such as primary care, vaccination and patient education were scored above midpoint, while public healthcare, diagnostic tests, emergency care, home-visit care, research and administrative duties scored below midpoint.
The main reason for PHDs supporting provision of primary care was ‘provision of basic medical care’ (67.5%) and ‘lack of nearby medical facility’ (53.3%). The major reasons against the validity of tasks include ‘presence of nearby medical facilities’ (87.1%) and ‘not main purpose of public health facility’ (55.6%). Over 90% of PHDs with nearby facilities (92.6%) and public health centers (98.7%) selected ‘presence of nearby medical facilities’ as the reason against the provision of primary care task. Thus, it could be concluded that the validity of primary care depends upon the presence of a nearby medical facility. The most cited reasons for patients choosing their public health facilities were the cost of care and ease of access to specific drugs (data not shown). For example, in many public health centers, all elderly people aged 65 years or more are treated free of charge, and most public health subcenters in medically underserved areas provide a variety of medicines free of charge (data not shown).
Considering these factors, there is a need to re-establish the distribution of PHDs and the type of work they perform in order to efficiently use medical resources. For example, if the reason for choosing a public medical facility despite the sufficient number of nearby medical facilities is the low cost, there is a need to set the same cost for private medical institutions as for the patients except for the specific target (such as patients aged 65 years and over or disabled people or recipients of social security). Through this process, governments should reduce irrational care so that PHDs can focus more on public healthcare work.
Conclusions
PHDs should be deployed more efficiently depending on medical needs based on provincial needs and the presence or absence of nearby private medical clinics and hospitals. Currently, PHDs are mostly working in primary care. PHDs working in remote islands have a high workload and number of working hours. They believe that the validity of their work is high, yet the validity of number of PHDs is low. PHDs working at public health centers have a large amount of primary care work, but do not think their work type is valid. Public health centers are usually in the center of cities with abundant nearby medical facilities. Therefore, PHDs’ work type should be tailored to provincial needs, such as healthcare policy, chronic disease management, patient education, vaccination and infectious disease control. Public health centers should focus more on utilizing PHDs in performing public health duties, rather than working as primary care physicians, which is already done by nearby private medical facilities.
Contributions
Authors Dae Hyun Lee, Mid-eum Moon, Youngdoo Go, Jeehyun Song, Jemin Kim, Cheolsu Kim and Jaerim Kim contributed equally to this manuscript.




