Introduction
In Japan, the absolute and relative shortage in the number of physicians has become a serious social problem. The number of doctors ranks in the lowest group in the OECD – 2.3 doctors per 10 000 population – and shows a shortage of about 140 000 doctors as compared with the OECD average1 In addition, many doctors are concentrating on convenient urban areas, and the shortage of doctors working in rural areas is more serious. This problem has been an important social and political issue for several decades in Japan. Other western countries, such as Australia and USA, have similar problems and much research is being done to develop the recruitment and retention of rural practitioners2.
According to findings that community-based education is very effective in fostering health personnel who respond to community needs3,4, the community-based clerkship has been started in many medical schools around the world5-7. In Japan, in 2007, the model core curriculum was revised by the Ministry of Education, Culture, Sports, Science, and Technology8 and, in 2016, the revised model core curriculum was proposed again. It was shown that ‘acquiring the ability to contribute to community healthcare by understanding the way of community healthcare and regional hygiene, current situation and problems’ and ‘learning the necessity and importance of community-based integrated and regional comprehensive care system through activities such as hygiene, medical, welfare, nursing etc.’ is done through community-based medical training9. However, the study only investigated the change in participant views before and after the clerkship10; few studies focus specifically on exploring the characteristics of medical students that will predict their intention for rural practice11-14. In western countries some studies have been done to explore rural-oriented attitudes among medical students15,16. Thus, identification of these relationships between various characteristics and their intent for rural practice will assist Japanese medical schools to effectively recruit and foster future rural physicians.
This study involved a cross-sectional survey among medical students in Japan to develop questionnaire items that measure self-efficacy of intent for rural practice based on the portfolio of the students who experienced community medicine clerkships.
Methods
Participants
This study was designed as a cross-sectional survey. The authors conducted a survey of 1st–6th year medical students from one Japanese regional university school of medicine. Every May, a five-page entry questionnaire was administered in a class within the first 4 weeks of the start of medical school. (In Japan, the academic year begins in April.)
Questionnaire development
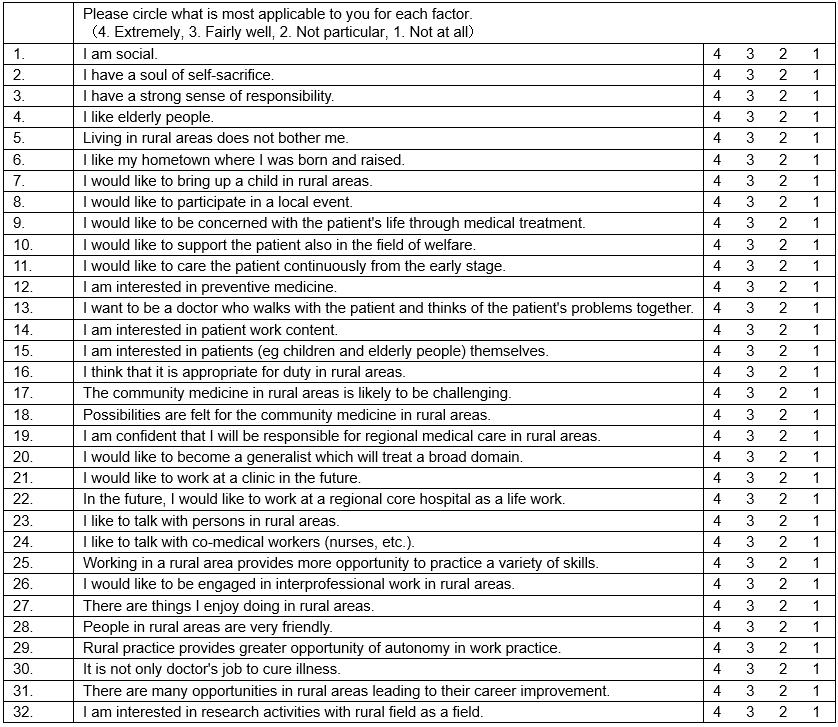
The authors extracted candidate items that measure self-efficacy of intent for rural practice based on the portfolio of Ehime University School of Medicine 5th year students who experienced community medicine clerkships. They experienced 1-week community medicine clerkships by interprofessional cooperation in two rural areas. They were obligated to record their clerkship experiences on a daily refraction sheet. All reflection sheets were analyzed to understand how the students learned during their clerkships. The authors extracted all points considered to be examples of learning from the students’ descriptions, and classified them by content, and also extracted examples of learning about rural practice17. Also examined was deepening of levels in community medicine to present ‘expressing experience’, ‘impressions’, ‘general experience’ and ‘future specific actions’. In addition, the authors referred to variables used in studies by Takeda et al.18-20 proposing a model of self-efficacy measuring intent for rural practice. Finally, 32 items were selected that included family and personal issues, professional issues, interprofessional practice, community and social issues, and learning skills (see Appendix A).
Questionnaire content
A self-administered questionnaire was used, enquiring about background factors and intent for rural practice. Sociodemographic questions regarding gender, age, academic year (1–3, 4–6), admission from hometown, graduation from public high school, combined junior high and high school graduation, have failed entrance exam, experience in admission to another university, parents as doctors, encounter with a doctor as a role model, scholarship for regional duty (chiiki-waku), admission by school recommendation, size of hometown of residence until age 18 years (eg capital city, regional, rural) and general medicine orientation were included. Influence of the responses to the candidate item extracted by the pilot survey was rated on a four-point Likert scale (4=’extremely well’, 3=’fairly well’, 2=’not particularly’, 1=’not at all’). Participants were asked whether they were willing to practice in a rural area (1=’positively motivated’, 2=willing to work for a certain period of time’, 3=’would rather avoid it’, 4=never’, 5=’other’).
Statistical analyses
Statistical analysis was performed using the Statistical Package for the Social Sciences v21 (IBM; http://www.spss.com). Results were shown by gender because Japanese medical students have dichotomized some motivations for their practice preference based on gender21. Data are presented as mean±standard deviation (SD) unless otherwise specified, and in the cases of parameters with non-normal distributions the data have been log-transformed for analysis. Differences were analyzed by student t-test or χ2 test. From 32 candidate items measuring self-efficacy of intent for rural practice (Appendix A), items were selected that were significantly related to intent for rural practice in the future. The factor analysis was conducted with SPSS using a maximum likelihood method and promax rotation. In each item, mean±SD was calculated, and items showing a ceiling effect (≥3.2) or floor effect (<1.2) were excluded from the analysis. In order to decide the number of factors, a scree plot, which shows the eigenvalues on the y-axis and the number of factors on the x-axis, was generated, and a cut-off of eigenvalue was set to be greater than 1. Item retention was based on coefficient values (factor loadings ≥0.35), and those showing a similar factor loading in more than two factors were excluded, then the factor analysis was repeated. Cronbach’s α coefficient was calculated for each factor to determine its scale reliability, as well as a mean score and SD. Logistic regression analysis (backward elimination method) was used to evaluate the contribution of each confounding factor for the participants’ intent for rural practice. In addition, multiple linear regression analysis using rural self-efficacy score as an objective variable, adjusted for confounding factors as explanatory variables, was performed. A value of p<0.05 was considered significant.
Ethics approval
The study was approved by the ethics committee of the Ehime University Graduate School of Medicine (IRB1507004), and informed consent was obtained from all subjects.
Results
Characteristics of medical students
Table 1 shows characteristics of medical students who participated in the study. The subjects comprised 166 women aged 22±2 (range 19–34) years and 243 men aged 23±3 (range 18–41) years. The participants were from academic years 1–3 (60.9%) and 4–6 (39.1%). In male participants, prevalence of the following factors was significantly higher than for women: academic years 1–3, from hometown, graduation from public high school, have failed entrance exam, experience in admission to another university and scholarship for regional duty. Combined junior high and high school graduation and admission by school recommendation were significantly lower. There were no gender differences regarding age, prevalence of doctors in parents, encounter with a doctor as a role model, hometown size until 18 years or general medicine orientation.
Figure 1 shows the prevalence of intent for rural practice by gender. A total of 83.5% of participants had positive intent for rural practice. There was no difference in gender with and without intent for rural practice.
Table 1: Characteristics of medical student study participants by gender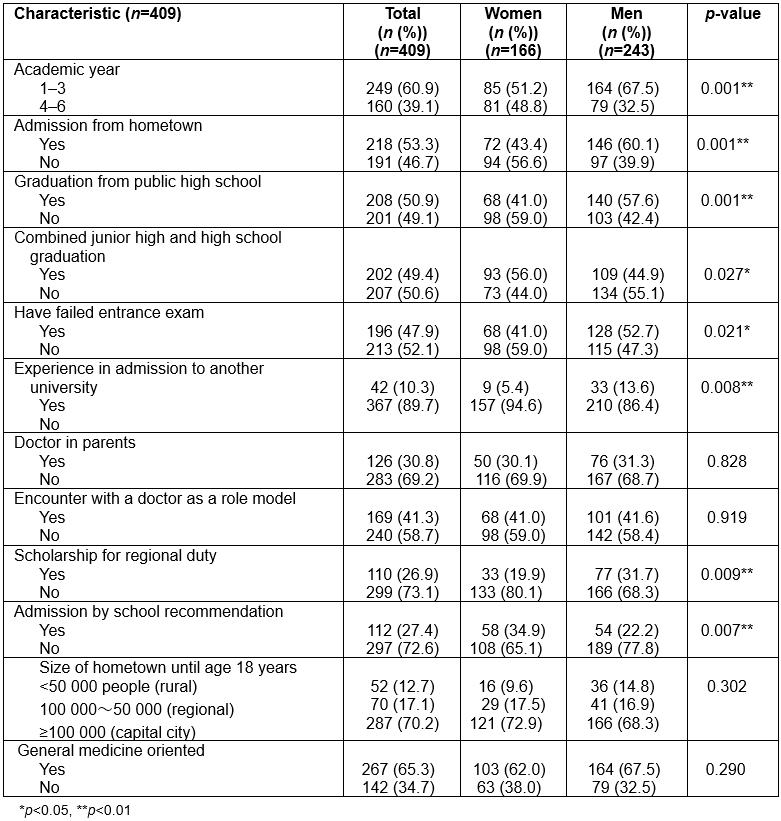
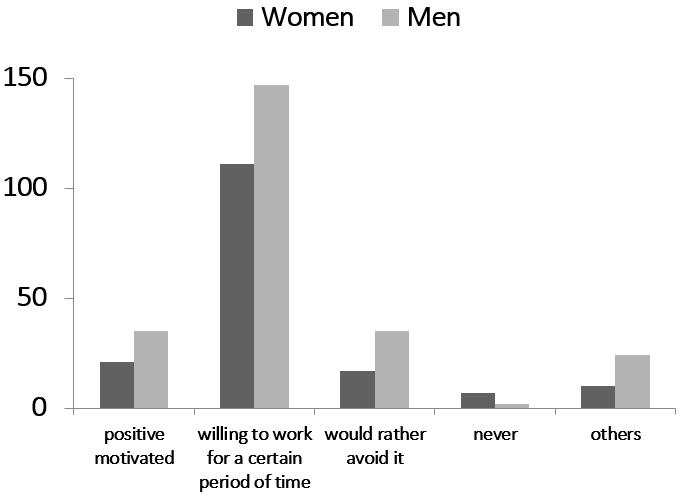 Figure 1: Prevalence of intention for rural practice by gender.
Figure 1: Prevalence of intention for rural practice by gender.
Factor analysis of rural self-efficacy items
Factor analysis yielded four factors that included 15 of the 32 items listed (Table 2); two items were excluded due to the ceiling effect; 15 items were excluded because of low loading factors (<0.35). The following four factors were defined based on the types of items that grouped together (Table 2).
- work preferences
- evaluation of rural practice
- evaluation of rural living
- personal character.
The four factors and the items that load on these factors are illustrated (Table 2). There were good factor loadings on all factors (0.424 to 0.890). This four factor (15 items) solution explained 46.8% of variance in responses. Cronbach's α coefficients demonstrated internal consistency: 0.813 for work preferences, 0.731 for evaluation of rural practice, 0.702 for evaluation of rural living and 0.747 for personal character. Overall score was 0.849, which is considered acceptable for newly developed scales. The lowest score was 27 points and the highest was 59 points, with higher scores indicating stronger intent for rural practice. The intercorrelations between the four factors are shown in Table 2; all interfactor correlations were significantly positive.
Table 2: Factor analysis of rural self-efficacy items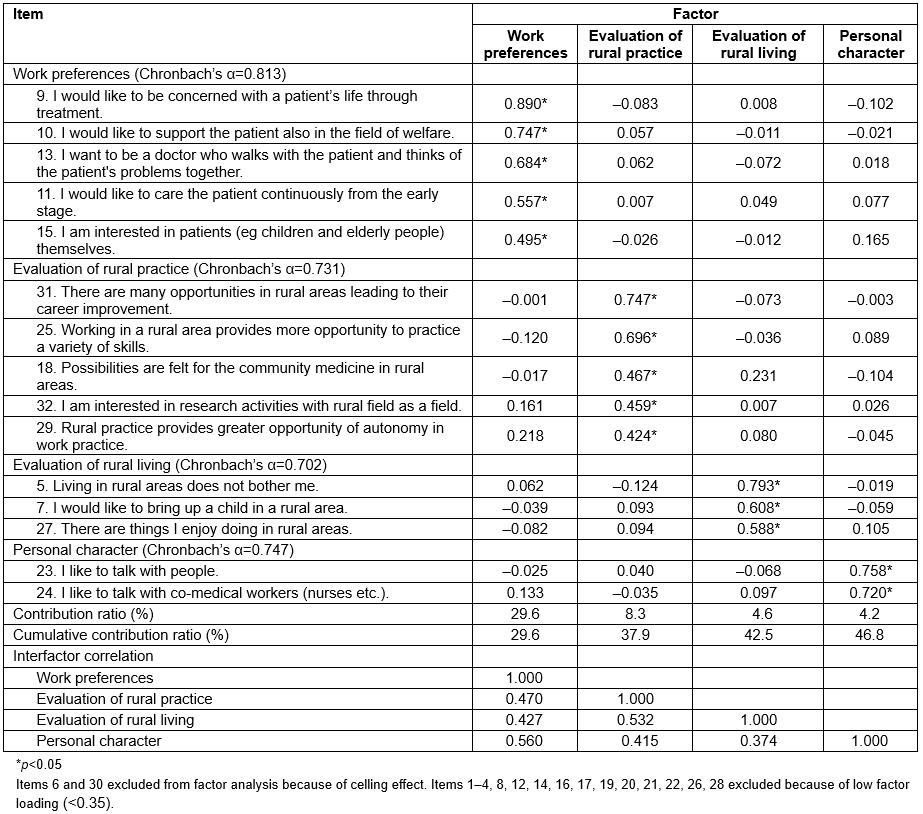
Score distribution of rural self-efficacy items by gender
Table 3 illustrates score distribution of various items constituting the rural self-efficacy scale. ‘I would like to be concerned with a patient's life through treatment’, ‘I want to be a doctor who walks with the patient and thinks of the patient’s problems together’, and ‘I am interested in patients (e.g. children and elderly people) themselves’ were significantly higher for women than for men, but ‘living in rural areas does not bother me’ and ‘there are things I enjoy doing in rural areas’ were significantly higher for men.
Table 3: Score distribution of rural self-efficacy items by gender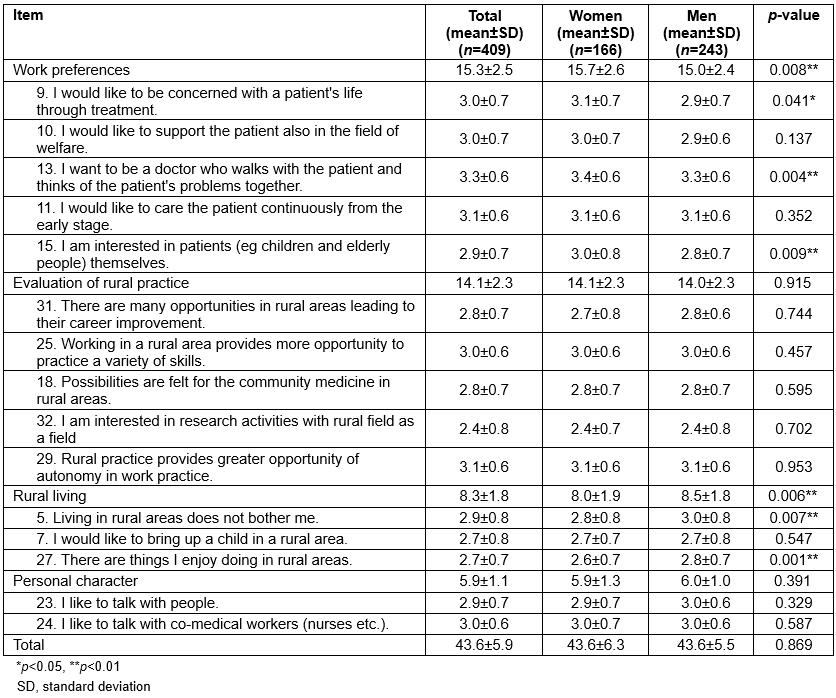
Relationship between intent for rural practice and rural self-efficacy score by gender
The relationship between the intent for rural practice and rural self-efficacy score by gender is shown in Figure 2. The average score was 43±6 in women and 44±6 in men. There was no difference for gender. A relationship between rural self-efficacy score was significantly increased with stronger intent for rural practice in both men and women.
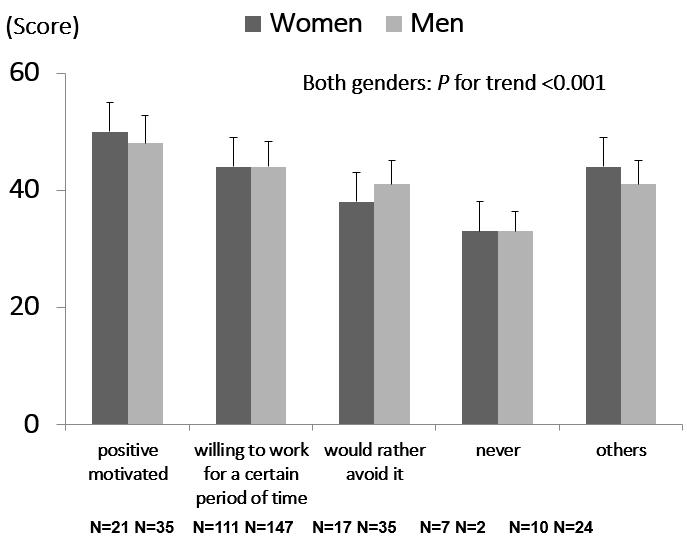 Figure 2: Intention for rural practice and rural self-efficacy score by gender.
Figure 2: Intention for rural practice and rural self-efficacy score by gender.
Simple relationship between rural self-efficacy score and the intent for rural practice by gender
Table 4 illustrates the odds ratios for the total and each of four factors of the rural self-efficacy score by simple logistic regression analysis. All factors were significantly associated with positive intent for rural practice in both men and women.
Table 4: Simple relationship between rural self-efficacy score and intent for rural practice by gender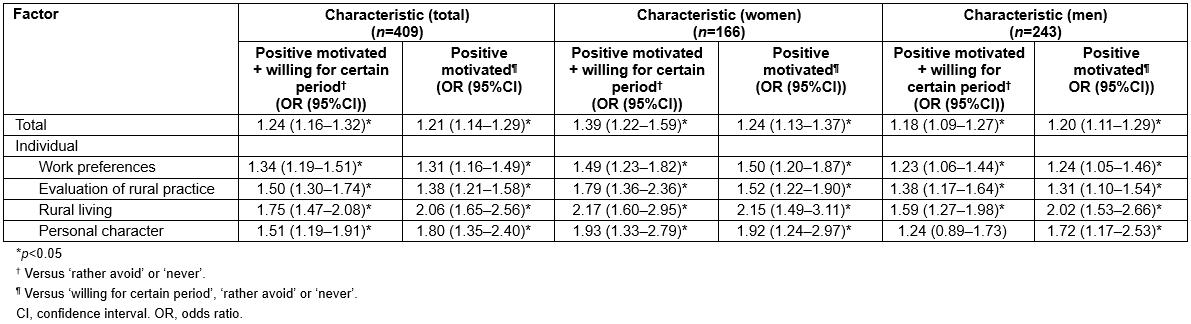
Characteristics of participants and rural self-efficacy score by gender
A relationship between characteristics and rural self-efficacy is shown in Table 5. Significantly higher rural self-efficacy scores were shown in for encounter with a doctor as a role model and general medicine orientation, for both men and women; and academic years 1–3, graduation from public high school and regional to rural hometown in men. Male students with combined junior high and high school graduation had significantly lower scores than other students. There were no relationship between the score and other characteristics.
Table 5: Characteristics of participants and rural self-efficacy score by gender
Multivariate-adjusted relationship between rural self-efficacy score and intent for rural practice by gender
Table 6 illustrates the odds ratios for the four factors of rural self-efficacy by multivariate logistic regression analysis using the intent for rural practice, adjusted for all confounding factors. The overall rural self-efficacy score and the scores for work preferences, evaluation of rural practice and evaluation of rural living showed a significant and independently positive association with the intent for rural practice.
Table 6: Multivariate-adjusted relationship between confounding factors including rural self-efficacy score and intent for rural practice by gender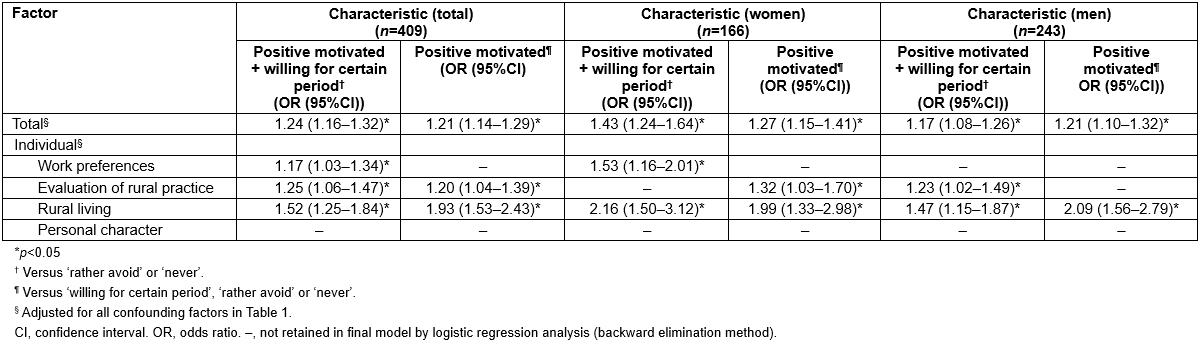
Multivariate-adjusted relationship between confounding factors and rural self-efficacy score by gender
In Table 7, multiple linear regression analysis using rural self-efficacy score as an objective variable, adjusted for confounding factors as explanatory variables, showed that, for women, encounter with a doctor as a role model and general medicine orientation and, for men, lower grade academic year, graduation from public high school and not failed entrance exam were also significantly and independently associated with rural self-efficacy score.
Table 7: Multivariate-adjusted relationship between confounding factors and rural self-efficacy score by gender 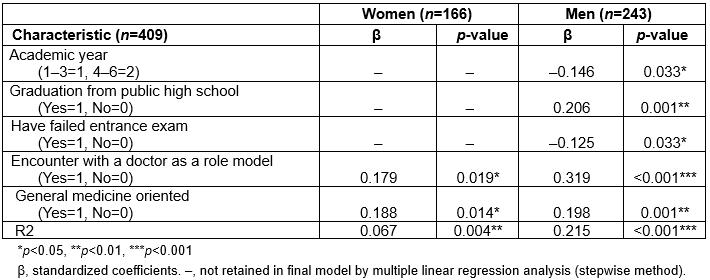
Discussion
In this current study, the authors developed a questionnaire that measures self-efficacy beliefs for intent for rural practice among Japanese medical students, and verified reliability and validity of the questionnaire. Four factors were identified as being associated with rural self-efficacy for rural practice: work preferences, evaluation of rural practice, evaluation of rural living, and personal character. Cronbach’s α coefficient for the questionnaire was 0.849, which is acceptable for newly developed scales. The present study suggests that medical schools might recruit medical students with higher rural self-efficacy scores and have to foster their rural-oriented attitudes in order to provide physicians to rural areas.
Many studies have focused specifically on exploring characteristics and identifiers of medical students that will predict their intent for rural practice. However, few studies have explored important components of medical students’ attitudes to future rural practice. Silagy and Piterman identified the factors that determine students’ choices of training location as education and training ( 20% of variance), personal and social (12% of variance), view of spouse and partner (8% of variance); and the factors that determine students’ choices of practice locations as professional (26% of variance), family (12% of variance) and community (9% of variance)22. Adams et al. identified four factors associated with student attitudes to living and working in rural areas: friendliness and support in rural areas (32% of variance), isolation and socialization problems associated with living and working in rural areas (14% of variance), enjoyable aspects of living in a rural area (9% of variance) and opportunities that working in a rural area provides (6% of variance)16. MacAuliffe and Barnett found that the influential factors identified in students considering rural employment included the rural location of their close family and friends, the overall occupational therapy program, good fieldwork experience and an inspiring fieldwork supervisor23. Henry et al. demonstrated that the most significant influencing factors for rural careers are professional support at national, state and local levels; career pathway opportunities; contentedness of the practitioner’s spouse in rural communities; preparedness to adopt a rural lifestyle; educational opportunities for children; and proximity to extended family and social circle24. In this study for Japanese medical students, four factors – work preference, evaluation of rural practice, evaluation of rural living and personal character in a rural area – were identified, and these factors were very similar to previous tools.
The four identified factors reflect the experience of living and working in rural area, demonstrating personal issues, professional issues, social issues and community issues. The other studies clearly support that these factors exist in rural practice and are interrelated, and the resulting factors provide a more integrated reflection of the rural experience16,25. In addition, the present study identified self-evaluation of personal character, which previous studies have not shown. Manahan et al. demonstrated that personal characteristics and experiences, as well as age and stage of life, rural background and location of family members, help shape personal values related to family, career, personal preferences and community, and that individual factors and personal preferences (eg need for adventure, wilderness and outdoor recreation) and community factors (eg people’s friendliness and a slower pace) also influence practice location decision26.
According to the reliability and validity findings, the rural self-efficacy score appears suitable for measuring students’ attitudes. The results show potential to measure change in students’ attitudes towards rural practice and life, and the authors are not aware of a similar tool in Japan. In future study, the authors need to develop the tool by re-analyzing the items to ensure new factors.
This study had some limitations. First, the cross-sectional study design does not eliminate potential causal relationships between characteristics of medical students and their intent for rural medicine. Second, this study was based on a limited number of students who belong to one regional university. Therefore, the demographics and referral source may limit generalizability. Third, the study measured students’ intent for rural practice but not their actual choice of practice because students’ intent was measured prior to residency. Fourth, this was a self-administered questionnaire developed for medical students in academic years 1–6, and some of the characteristics examined appeared to be suitable for upper grade students but not for lower grade students.
Conclusion
The present study identified four factors associated with rural-oriented attitudes to living and working in a rural area. Future research using longitudinal data collection will enable monitoring of the relationship between baseline rural self-efficacy score, community medicine clerkship and actual behavior.