Introduction
Constipation is not a disease; it is a subjective symptom, the interpretation of which can vary from person to person, and which adversely affects daily life. Constipation is defined as failed or lengthy attempts to defecate, and hard and painful defecation that is distressing to family and child. Delay or difficulty in defecation that continues for 2 weeks or longer is also defined as constipation. Constipation, which is most frequent in childhood, affects 0.5–29% of the child population worlwide1-5.
The etiology of childhood constipation is generally divided into two groups: organic and functional. Organic constipation is when the defecation disorder is related to causes such as anatomical malformations, metabolism, neuropathies, bowel nerve or muscle disorders, abdominal wall anomalies, connective tissue diseases, and drugs. Functional constipation, without objective evidence, is the voluntary holding of stools by a child who wants to avoid painful defecation and is much more common than organic constipation6,7. In functional constipation type, familial, cultural and social factors play an important role6. The pathophysiology of constipation has not been fully elucidated, and many mechanisms play a role in the progression of constipation.
Constipation in childhood occurs as a result of multifactorial causes, and dietary habits, physical inactivity, gender, lower socioeconomic and psychological parameters, medications etc., have all been implicated as risk factors for constipation7-9. In addition, urban and rural areas exhibit some differences in the risk factors for constipation. Genetics, insufficient physical activity, and obesity are among the risk factors for constipation in rural areas, while stress and lifestyle affect those in urban areas1,7,9.
Constipation in childhood starts as a simple complaint, but, if it is not treated adequately, it can become so serious that it can affect the growth and development of the child7. In the study by Sahin et al, it was seen that 10% of children with a constipation complaint suffered from growth and developmental delay10. Constipation is a health problem that is being encountered more frequently in society. However, it is not regarded as a serious problem by families, so they do not consult health institutions7,8.
Individuals in rural areas try to manage their illnesses by traditional methods due to cultural beliefs and practices as well as the distance to health centers and the lack of staff at such health centers. Also, the opportunity to access healthcare services is reported to be limited in rural areas. The range of healthcare services provided by the government in rural areas is quite limited compared to in urban areas. The outcomes of this study will make a contribution to the determination of the prevalence of constipation in infants aged 0–12 months and provide mechanisms for decreasing constipation in society.
Research questions
• What is the frequency of constipation in infants aged 0–12 months in the area where the study is conducted?
• Is there any connection between the sociodemographic characteristics of babies and constipation rates?
• Are there any differences between the defecation characteristics and the rate of constipation of the infants and their families?
Methods
Research design and settings
The study, which was planned as a descriptive and relational type, consisted of babies aged 0–12 months who were registered with family health centers in rural areas.
Participants
A schedule recommended for ‘predicting a rate in society with particular accuracy’ was used for the identification of the size of the research sample11. Since this was a finding related to the prevalence of the examined incident (rate of incidence of constipation) in society, a rate (4.7%) reported by van Tilburg et al was used12. In a table proposed by Lemeshow et al, the reported rate was established as 5% with a confidence level of 95% and a relative accuracy of 3%, and the sample size reported in the table was 20311. A simple random sampling method, one of the probability sampling methods, was used in the selection of the sample. Between April and June 2016, infants aged 0–12 months and their parents were chosen from those who applied to the family health center ; those who complied with the criteria for inclusion in the study were included in the sample. The research consisted of 685 children. The number of infants involved in the sample was 203, and the sample was selected using a random numbers table.
If a parent did not want to participate in the research or couldn’t be accessed, the next infant on the list was selected.
The sample selection criteria was as follows: no chronic disease, no congenital aganglionic megacolon disease, no 1-month hospital stays, and no neurological disease.
One definition of rural areas in Turkey is communities with a population density of <150 people/km2. The city of Karapnar has an area of 8924 km2 and 28 people/km2. This population includes those who live in districts and those who live in the countryside. The town known as Karapnar mound conforms to the definition of a rural area in terms of population, education, transport and social life. The population growth rate of rural Turkey is 4%, the fertility rate is 2.65%, the perinatal care ratio is 57.7%, the mobile internet access rate is 26%, and the Gini index (a standard economic income inequality measure) is 0:36 (where 0 is the sum total and 1 is inequality). The unemployment rate in rural areas of Turkey is 5.9%13,14. In this region, agriculture and animal husbandry is the main source of income. The town is about 99 km from the city center. In Karapnar, health services are provided by a district hospital and 11 family physicians.
Instruments
The Infant and Family Data Collection Form containing 47 questions generated by the researcher was used to collect the data, the Rome III criteria was used to diagnose constipation in newborn and infancy periods, and the Bristol stool chart (BSC) was used to evaluate stool consistency15,16. The heights and weights of the infants were measured with a digital baby scale and an infant meter calibrated in the family health center. The infants’ heights were measured by measuring the distance between their heels and the end of their head with an infant meter, after they were placed on the exam table. The infants’ weights were measured when they were wearing lightweight clothes after they were placed on a digital baby weight. The data were collected by the researcher from the mothers of the infants using the face-to-face interview technique between April and June 2016.
Rome III criteria
Rome III criteria consist of six criteria: two or fewer stools per week, stool leakage at least once a week, excessive stool retention, painfully stiff stools, rectal stool mass detection, and stool large enough to clog the toilet. At least two criteria must be present for a diagnosis of constipation17.
Bristol stool chart
The BSC is used to determine constipation. On this scale, there are seven visual forms of stool for designating feces. The first form describes a stool as ‘separate hard lumps, like nuts’ and the scale continues to the seventh, which describes a stool as ‘watery, no solid pieces, entirely liquid’16.
Statistical methods
The data of the study were analysed using number, percentage, and mean and standard deviation to create descriptive statistics; a χ2 analysis (Fisher’s exact test and tetra-eyed Pearson and multi-eyed Pearson χ² analyses) was made to compare the incidence of constipation according to the variables. The Kolmogorov–Smirnov test, the skewness-kurtosis values and the histogram were used to evaluate the normality of the distribution. Logistic regression (enter) analysis was completed to evaluate all variables together that have an effect on the incidence of constipation. The statistical significance level was accepted as p<0.05.
Ethics approval
Ethics approval was obtained from the Necmettin Erbakan University Faculty of Medicine Ethics Committee (approval number 2016/452) on 16 February 2016. Written permission of the Public Health Directorate of Konya (799-E.476/00021013330) to conduct the research in the relevant institutions was obtained on 22 March 2016. Verbal consent was given by the families participating in the study to the researcher, who explained the research ethics.
Results
It was observed that 53% of the infants who participated in the research were male, 88.2% were born in the 38th week or later, the birth weights of 93.6% of the infants were ≤2500 g, and 91.6% were looked after by their mother. The infants’ average age was 4.8 months, the mean height was 62.58 cm, and the average weight was 6.58 kg.
According to the body mass index (BMI) percentile groups, it was determined that 25.6% of the infants were underweight (below 15%), 56.2% were normal weight (15–85%), and 18.2% were obese (86% and over). It was found that 86.2% were breastfed as their first food, 31.5% took in breast milk half an hour after birth, 47.3% took supplementary food, and 55.2% started to take in supplementary food before the 24th week. It was determined that 24.1% of the infants’ mothers had a constipation complaint. Meconium excretion was determined in 1.5% of the infants 48 hours after birth. It was determined that 15.3% of the infant defecated every two or three days; 13.3% defecated every four days or less frequently, and had hard stools; 12.3% had hard stools; and 4.9% of the infants had stools that were like goat droppings. While the prevalence of constipation in infants was found to be 17.7% according to the Rome III criteria, 19.7% of the infants’ mothers said that their infants had a constipation complaint. Sixty-five percent of the infants’ complaints were found to have continued for 1–4 weeks, and 35% of the infants’ complaints were found to have continued for 5 weeks or longer.
It was determined that 2.5% of the infants had bleeding during defecation, 25.1% of the infants had pain during defecation, 20.2% exhibited continence behaviour, and 31.5% had abdominal pain and trouble defecating.
It was determined that 9.9% of the infants were given medicine to treat the constipation, and 75% of the medicines used was glycerin, In 12.8% of the infants, an application was performed at home to get rid of constipation, and 84.6% of the infants were given olive oil to drink.
The most frequent complaints seen in the infants was defecation twice or fewer times per week (21.2%), painful and hard defecation (17.2%), excessive continence behaviour (16.3%), and rectal fecal mass (1.5%). According to the BSC, 4.9% infants defecated in the shape of dispersed nodules as hard as a nut (hard to defecate), and 7.4% defecated in the shape of sausage but tubular.
The complaints of infants with constipation were found to be painful defecation (94.4%), having difficulty during defecation (91.7%), abdominal pain (86.1%), continence behaviour (80.6%), nausea and vomiting (33.3%), anal fissure (16.7%), and the presence of blood during defecation (11.1%).
No statistically significant difference was found between the infants’ postnatal age groups, delivery methods, and rates of incidence of constipation by gender (p>0.05). The rate of incidence of constipation in mildly obese and obese infants (according to the BMI percentile values) was found to be significantly higher than the rate in infants who were underweight and normal weight (compared to infants of normal weight) (p=0.035). No statistically significant difference was found between the rates of constipation in infants with meconium excretion within the first 24 hours and after 24 hours (p>0.05). The rate of incidence of constipation (36.7%) in infants whose mothers had a constipation problem was found to be significantly higher (11.7%) than in those whose mothers did not have a constipation problem (p<0.0001). The rate of incidence of constipation (26.7%) in infants whose fathers had a constipation problem was found to be higher (17.0%) than in those whose fathers did not have a constipation problem, but this difference was not found to be significant (p>0.05). The rate of incidence of constipation in infants who breastfed as their first food was found to be significantly lower than in those who did not breast feed as their first food (p=0.032). While the rate of incidence of constipation (20.8%) was higher (15.0%) in infants who did not take supplementary food than in those who did, no statistically significant difference was found between these two groups (p>0.05). The rate of incidence of constipation in infants who started to have supplementary food before the 24th week was found to be significantly higher than in those who started have supplementary food in the 24th week or later (p=0.041).
Logistic regression analysis was used to evaluate the effects of four variables that were found to affect constipation in infants. The presence of constipation was the dependent variable. The presence of constipation in the mother, the infant’s BMI, the circumstances of first breastfeeding, and the start time of the intake of supplementary food were included as predictor (influencing) variables in the model. The enter method was used for analysis. Logistic regression was applied, with standard deviation (SD) 1, χ2 25.219 SD 4 and p=0.000.
When the effect of some of the infants’ characteristics on the incidence of constipation was examined and the Wald test results with regard to the significance of the regression coefficients were considered, it can be said regarding the significance levels of variables included in the model that the presence of constipation in the mother had a very significant effect (p<0.0001), and the infant’s BMI (whether he/she is obese or not) had a significant effect (p=0.027). The effects of the circumstances of the first breastfeeding, and of the start time for the intake of supplementary food (p>0.005) on the incidence of constipation were not found to be significant (Table 1).
Table 1: Examination of variables affecting the presence of constipation in infants: logistic regression analysis results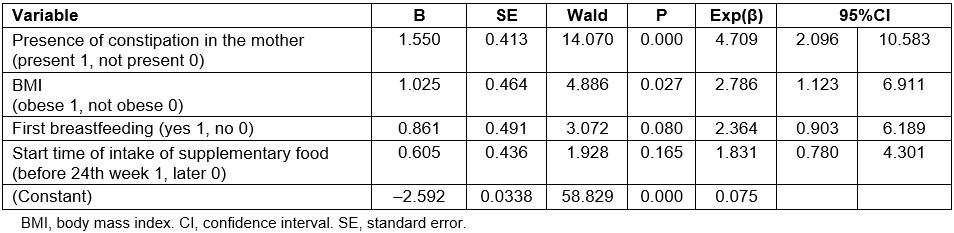
It was found that for infants whose mothers had constipation, the probability of the incidence of constipation was 4.7 times higher than for those whose mothers did not have constipation, the probability of the incidence of constipation in obese infants (mildly obese or obese) was 2.8 times higher than for those with normal BMI or those who were underweight. The effect of circumstances of first breastfeeding and of the start time of intake of supplementary food on the incidence of constipation in infants was not found to be significant (Table 1).
Discussion
This study was conducted to determine the prevalence of constipation in infants aged 0–12 months in a rural area of Turkey. In the study, the prevalence of constipation in infants aged 0–12 months was identified as 17.7% according to the Rome III criteria. In a study conducted by Loening-Baucke for children less than 2 years of age, the rate of the presence of constipation in infants aged 0–1 years was reported as 2.9%, and van Tilburg et al reported the rate as 4.7%12,17. Kocaay et al found the rate of incidence of constipation in infants aged 0–1 years as 2.13% in a study they conducted in Turkey18. The differences between the studies conducted may arise from constipation identification criteria, living in rural areas, and sociodemographic differences.
When an infant’s gastrointestinal system is covered with immunoglobulins as well as colostrum milk, a mucosal barrier is established. It allows the intestines to mature by means of the epidermal growth factor and other similar growth factors it contains and prevents the development of allergy and food intolerance. It facilitates the newborn’s meconium excretion with its mild laxative property19. While no evidence was encountered in the literature regarding the circumstances of the first breastfeeding and constipation, in the present study, constipation was seen in 15.4% of infants who were breastfed as their first food and in 32.1% of those who were not. This difference was found to be significant.
While the number of defecations in infants who took in breast milk was found to be 2.3 per week on average in the studies, that decreased to 0.1–1 in those who did not18,19. Tunç et al observed in their study that there was a decrease in the number of defecations in infants who took in food as well as being breastfed at one, two and four months after birth compared to those who were breastfed only during the same time periods20. Fontana et al determined in their study conducted on children under 3 years that the number of defecations was 3.2 per week in those who were breastfed and 2.0 in those who took in food as well as being breastfed in the same period21. In some studies, it was determined that breast milk intake and duration did not affect the number of defecations21,22. In the present study, constipation was determined in 30.2% of children who started to take in supplementary food before the sixth month and in 13.2% of those who started to take in supplementary food after the sixth month. While the amount of breast milk intake and breastfeeding frequency was higher in the first months, they decreased after 16 weeks. It was thought that the difference might be due to differences in the age groups in the studies. There are some hypotheses about the frequency of defecation in infants taking in breast milk. These hypotheses mention that there is likely a factor accelerating transport, that the lipids in breast milk could be digested more easily, and that there are prebiotics in breast milk23.
In order to avoid the pain that occurred during defecation, a child exhibits continence behaviour. The stool gets harder as it accumulates in the rectum. Because the stool has hardened, its excretion becomes more difficult and painful, which sets up a vicious circle18. Continence behaviour was observed in 80.6% of the children who participated in the present study. A total of 69.3% of children aged 1–17 years in a study by Kirsaçlioglu et al and 35% of those aged 4–9 years in a study by Kim et al were observed to exhibit continence behaviour24,25.
Abdominal pain was determined in 86.1% of infants with constipation in the present study. Abdominal pain was determined in 9.3% of constipated children aged 1–17 years in the study by Kirsaçlioglu et al24, in 66% of constipated children aged 1–16 years in the study by Sahin et al10, in 61.6% of 120 children aged 1–6 years in the study by Çataklu et al22, in 5% of children aged 4–9 years in a study by Kim et al25, and in 47.9% of constipated children in a study by Kocaay et al18. According to Gedik and Kocoglu, patients living in rural areas have both poor disease management and more complex healthcare requirements26.
The problem of defecation arouses feelings of restlessness in child. While the feelings of restlessness during defecation was determined in 91.7% of infants who participated in the study, this rate was found to be 33% in the study by Kocaay et al conducted on children aged 0–6 years18. The reason for this difference may be low health literacy in rural areas
In the present study, the rate of incidence of constipation in infants whose mothers had a constipation problem was found to be 36.7% while in those whose mothers did not have a constipation problem it was found to be 11.7%. According to the results of logistic regression analysis, it was determined that the probability of having constipation in infants whose mothers had a constipation problem was 4.7 times higher than in the infants whose mothers did not have a constipation problem. This suggested that there was very significant statistical difference (Table 1).
In the present study, the rate of incidence of constipation in infants whose fathers had a constipation problem was found to be 26.7% while in those whose fathers did not have a constipation problem it was found to be 17%. It was determined that the frequency of constipation was higher in infants whose fathers had a constipation problem, but the difference was not significant. In various studies, a relationship of 8.2–86.6% has been found between family history of the infants and their rate of incidence of constipation22,24,27-29. In general, a relationship has been seen between the family’s constipation history and the incidence of constipation in the child, which suggests that heredity may have an effect on intestinal motility. A gene associated with functional constipation has not so far been found. However, the presence of a constipation history in more than 40% of the constipated children’s family, and the presence of six times more constipation in identical twins compared to dizygotic twins suggests the existence of a genetic susceptibility30. It is also thought that the reason for the very significant difference between infants whose mothers had a constipation problem and those whose mothers did not might be the mother’s feeding behaviours and the fact that an iron preparation was used.
In the present study, according to the BMI percentile values, the rate of incidence of constipation in mildly obese and obese infants was found to be significantly higher than that in underweight and normal weight infants (p=0.035). The logistic regression analysis indicated that there was a significant (p<0.05) relationship between the infant’s BMI (whether or not he/she is obese) and incidence of constipation (p<0.05). The rate of incidence of constipation in infants who were mildly obese or obese was found to be 2.8 times higher than that in normal weight and underweight infants (Table 1). Obesity is among well-recognised risk factors in children, and, in many studies, prevalence of constipation in obese children was found to be higher27,29,31. People with constipation more commonly have a sedentary lifestyle, low calorie diet intakes and low education levels. This situation indicates the characteristics of the people of the rural area.
Limitations of the research
In this study, no specific Bristol stool neonatal scale was used.
Conclusion
It was determined that about one-fifth of the infants living in rural areas in Turkey have constipation. More epidemiological studies in Turkey are warranted.
References
You might also be interested in:
2019 - Social and community networks influence dietary attitudes in regional New South Wales, Australia
2017 - Building a community of practice in rural medical education: growing our own together
2013 - Advanced rural skills training: are recently qualified GPs using their procedural skills?


