Introduction
Many strategies have been implemented to address the shortage of medical practitioners in rural areas in Australia. One such strategy is the Rural Clinical Schools Program, which was implemented in 2000, mandating that 25% of all Commonwealth-supported students train in a rural area, coordinated by a rural clinical school (RCS) for at least 1 year of their clinical training1,2 and that 25% of students enrolled in the medical course have a rural background. There are currently 18 RCSs in Australia, representing a substantial financial investment aimed at addressing the rural workforce shortage.
It is important to determine the impact of this program in addressing the maldistribution of medical practitioners between rural and metropolitan locations. Several groups have reported that time spent at an RCS is significantly associated with an intent to practice in a rural area3-8; however, the strength of the association needs to be understood in relation to other effects on rural practice, such as rural background9. Other research groups have determined that the relationship between rural exposure and taking up a rural career is unclear and the evidence is inconclusive10,11. A recent Australian review article highlights the ‘expenditure–evidence gap’ for the myriad government initiatives designed to enhance the rural medical workforce12.
The RCSs around Australia are now funded via rural health multidisciplinary training agreements (2016–2018) with the Australian Government, which will sustain investment in rural-based training for health workers. Individual universities have reported graduate outcomes from rural training during medical school6,7,13-16. For example, a study of graduates from the University of Western Australia demonstrated that a greater number of students who participated in the Rural Clinical School of Western Australia (RCSWA) were working in a rural location (odds ratio(OR)=7.5 for rural background RCSWA students and OR=5.1 for urban background RCSWA students)17. However, no research combining data from multiple RCSs exists providing evidence about the effectiveness of the RCS Program as a whole to increase the recruitment and retention of medical practitioners in rural areas.
The aim of this study was to determine the association between rural location of practice in 2017 and (i) extended rural clinical placement and (ii) rural background for the 2011 medical graduates from multiple RCSs within Australia.
Methods
All medical schools funded under RHMTP (or similar) were contacted by email about participation in this study. Participating universities supplied de-identified data for the 2011 graduating class, which corresponded to postgraduate year 5 in 2017. At this postgraduate stage, all alumni would have either finished vocational training for colleges such as the Royal Australian College of General Practitioners or the Australian College of Rural and Remote Medicine, be accepted in a vocational college in any of the 16 other specialist colleges, or have opted for a generalist training pathway. Some but not all training could be conducted in a rural area for most colleges. For each domestic student, information about their gender, origin (rural or metropolitan) and participation in extended rural clinical placement was obtained. Rural background was defined as living in an Australian Standard Geographic Classification-Remoteness Area (ASGC-RA) 2–5 area for at least 5 years since beginning primary school1, where RA1 corresponds to a major Australian city, RA2 to inner regional, RA3 to outer regional, RA4 to remote and RA5 to very remote areas. Extended rural clinical placement was defined as having students trained in a rural area, coordinated by an RCS for at least 1 year of their clinical training. Practice location was extrapolated/assumed from their current (2017) postcode location recorded in the publicly available Australian Health Practitioner Regulation Agency register. Postcodes were classified into rural and metropolitan areas using the ASGC and the more recent Modified Monash Model (MMM), which groups RA2 and 3, then separates based on population. MMM3 includes towns with a population of 15 000–50 000; MMM4 populations of 5000–15 000, and MMM5 populations <5000, while MMM6 and 7 are remote and very remote locations respectively. For this study, rurality is defined as RA2–5 (inner regional or smaller) and MMM3–7 (towns with populations <50 000). Both classifications were considered in this study as the RCS program is still funded based on the ASGC, whereas the MMM is the current classification system used by the Commonwealth (and focusing on 3–7 allowed exploration of more rural outcomes than the standard rural ASGC). The main outcome measure was whether the students were working in a ‘rural’ or ‘metropolitan’ area.
SPSS v24 (SPSS; http://www.spss.com) was used for statistical analysis. Descriptive statistics were used to present basic characteristics. A p-value <0.05 was considered significant. Pearson’s χ2 test was used to detect differences in gender, rural background and extended placement at an RCS between graduates working in ‘rural and ‘metropolitan’ locations. Univariate and multivariate binary logistic regression was used to determine odds of rural practice and 95% confidence intervals (CI) for gender, rural origin and participation in extended rural clinical placement.
Ethics approval
The University of Notre Dame Australia’s Human Research Ethics Committee approved the overall collation and analysis of the data from individual universities (approval 016190S). Each university gained approval from their institution’s HREC to provide the de-identified data.
Results
Fifteen universities agreed to participate in the study. Data were received from 14 of the 16 universities who had a 2011 graduating class. However, two universities had not started collecting origin data at this point so were excluded from the analysis. Data on 1695 graduates were included in the analysis. Each university had different numbers and proportions of Commonwealth-supported places, which is identifying information. To preserve confidentiality, the data reported here are given as percentages only. Also, the relative proportion of domestic and international students varied. This impacted the proportion of rural medical students per university, because international graduate numbers are not subjected to the same Commonwealth 25% rural place requirement that domestic quotas require.
The proportion of students with a rural background had a range of 12–76.6% and participation in extended rural clinical placement had a range of 13.7–75% (Table 1). Overall, 22.3% of students had a rural background and 29.3% participated in extended rural clinical placement. Valid Australian postcodes were identified for 1598 students (94.3%), with the remainder not found on the AHPRA register (n=82, 4.8%) or were practising overseas (n=15, 0.9%). Overall, 10% of the students had both a rural background and had participated in extended rural clinical placement, ranging between 4% and 27% for individual universities.
In 2017, 16.6% of the 2011 graduating class were working in rural areas on the AHPRA register (according to ASGC), ranging from 5.8% to 55.6% of individual university cohorts (χ2(11)=133.653, p<0.001). According to the MMM, 8.3% of the 2011 graduating class were listed as practising in rural areas in 2017 (MMM3–7), ranging from 4.5% to 29.9% of individual university cohorts (χ2(11)=51.207, p<0.001). Almost 80% of students were registered in the same state as the university where they had completed medical training.
Of those practising rurally according to the ASGC, 183 (68.8%) were located in inner regional areas (RA2) whilst 68 (25.6%) were practising in outer regional areas (RA3) and 15 (5.5%) were practising in remote or very remote locations (RA4,5) (Fig1a). Of those practising rurally according to the MMM, more than 70% were in towns with a population less than 15 000 people (MMM4–7), with 10% practising in areas classified as remote or very remote (MMM6,7) (Fig1b).
Almost one quarter (23.3%) of students who participated in extended RCS placements were practising in a rural area according to ASGC compared to 13.8% of students who did not participate in extended RCS placements (χ2=21.887, p<0.001) (Fig2). While 34.0% of students with a rural background were practising in a rural area, only 11.2% of students with a metropolitan background were practising in a rural area (χ2=101.204, p<0.001). There was no difference in gender for rural versus metropolitan practice. According to the MMM, 16.2% of students with a rural background were practising in a rural area, which was significantly higher than the 5.9% of students with a metropolitan background who were in rural practice (χ2=37.230, p<0.001). Significantly more students who participated in extended RCS placement were practising in a rural area (MMM3–7) (15.0% v 5.4%, χ2=40.955, p<0.001) (Fig2).
Overall, gender was not associated with rural practice in this study (Table 2). However, students with a rural background were 4.1 times more likely to be practising in a rural location according to ASGC (p<0.001) and students who participated in extended RCS placement were 1.9 times as likely to be practising in a rural location (p<0.001). After rural background was controlled for, students who attended an RCS were 1.6 times more likely to be in rural practice (p=0.004). After extended RCS placement was controlled for, students with a rural background were 3.8 times more likely to be practising in a rural location (p<0.001). According to the MMM (3–7), students with a rural background were 3.1 times more likely to be in rural practice than students with a metropolitan background (p<0.001). Students who participated in extended RCS placement were 3.1 times as likely to be practising in a rural location (p<0.001). After rural background was controlled for, students who participated in extended RCS placement were 2.6 times as likely to be practising in a rural location (p<0.001). After extended RCS placement was controlled for, students with a rural background were 2.6 times more likely to be practising in a rural location (p<0.001).
Regardless of geographic classification system (ASGC, MMM) used for location of practice and of student background (metropolitan or rural), those students with an extended RCS placement had increased chances of working rurally (Table 3). Rural background and RCS placement were associated with the highest likelihood of rural work according to both ASCG and MMM classification of work location.
Table 1: Characteristics of students from participating universities 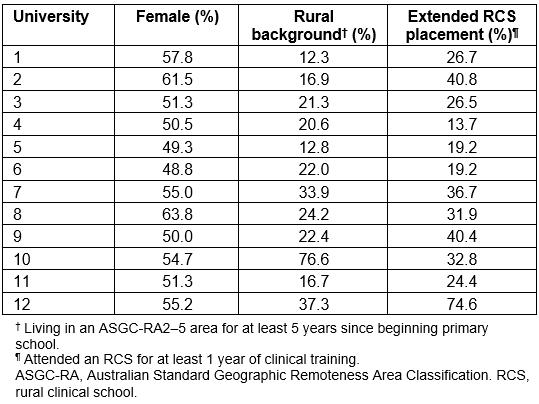
Table 2: Odds ratios for rural practice location as defined by the Australian Standard Geographic Classification and the Modified Monash Model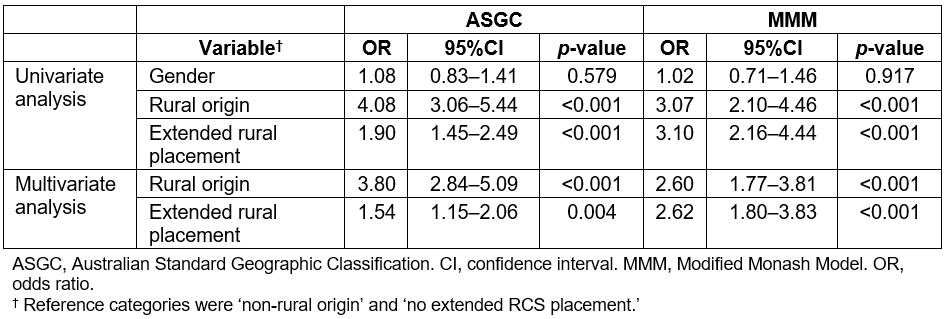
Table 3: Odds ratio for being in rural practice according to the Australian Standard Geographic Remote Areas Classification (RA2–5) and the Modified Monash Model (MMM3–7) according to background and extended rural clinical placement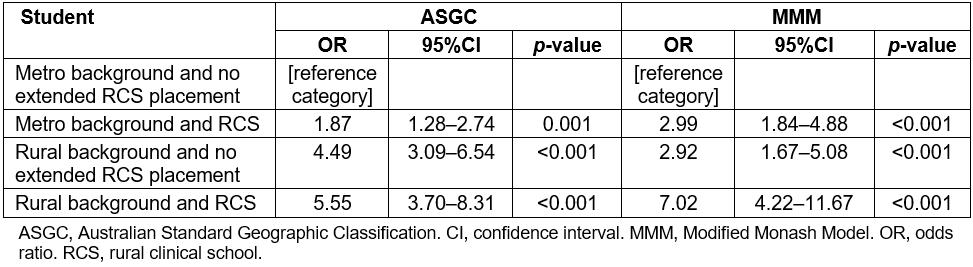
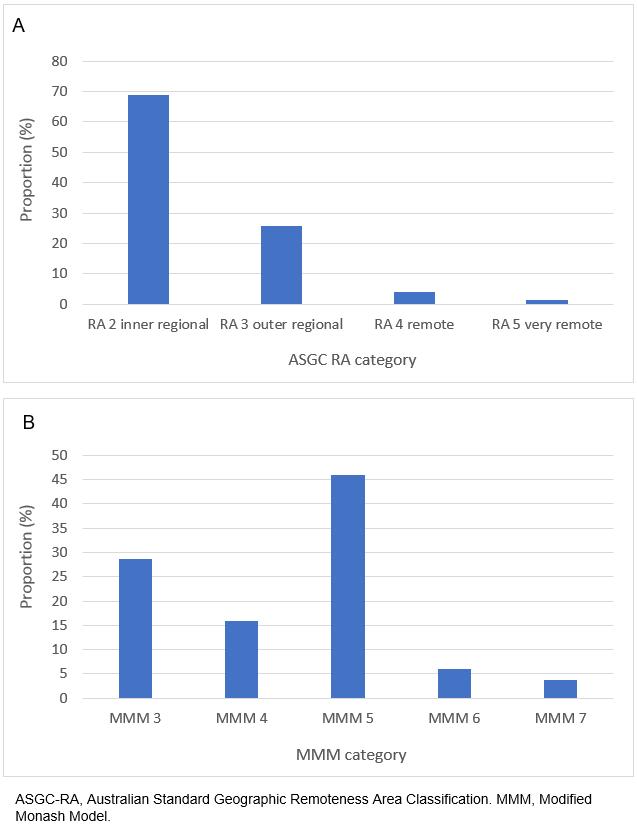 Figure 1: Distribution of rural practice locations in 2017 for students from the 2011 graduating class per remoteness category as defined by (A) Australian Standard Geographic Remoteness Area Classification (ASGC-RA2–5) and (B) the Modified Monash Model (MMM3–7).
Figure 1: Distribution of rural practice locations in 2017 for students from the 2011 graduating class per remoteness category as defined by (A) Australian Standard Geographic Remoteness Area Classification (ASGC-RA2–5) and (B) the Modified Monash Model (MMM3–7).
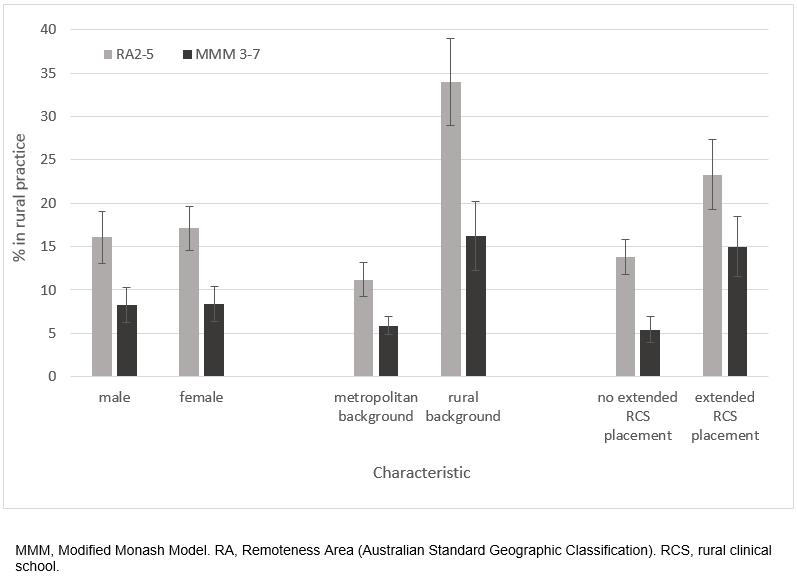 Figure 2: Proportion of 2011 graduating classes practising in a rural location.
Figure 2: Proportion of 2011 graduating classes practising in a rural location.
Discussion
Although individual Australian universities have reported graduate tracking outcomes, this study is the first to present collated data from multiple RCSs about the influence of the RCS Program as a whole on the recruitment of medical practitioners in rural areas. This study demonstrated that, independent of rural background, students who have participated in extended RCS placement were 1.5 times as likely to be in regional and rural practice (ASGC) 5 years after graduating from medical school and 2.6 times as likely using the MMM. Based on the combined data from three-quarters (12/16) of the Australian medical schools at the time, this provides evidence that the RCS initiative as a whole is having a significant positive effect on the regional medical workforce at 5 years postgraduation, and continued funding of this policy is warranted. This result concurs with that of a recent study which accounted for all known confounders, identifying that at least 12 months immersion was associated with 1.8 times the odds of rural work outcomes compared with wholly metropolitan-trained students and rural background, with 3.118. Stronger associations with rural work outcomes were found as immersion duration increased to 2–3 years (OR 4.4), although the study presented here did not delineate those having longer than 12 months immersion.
Results from the 2011 Medical Students Outcome Database Survey of students at 19 medical schools within Australia showed that 15.7% of 2011 graduates had non-urban (regional city, large town, small town or small community) future practice intentions as their first preference19. In the present study, a similar proportion (16.6%) of the 2011 graduating class were listed on the AHPRA register as practising in rural areas at 5 years postgraduation.
In a survey of students who had completed a Bachelor of Medicine, Bachelor of Surgery (MBBS) at Monash University, Hogenbirk et al20 found that 40% of respondents who reported having rural practice intentions during their MBBS training were actually in rural practice following completion of their vocational training. They suggested that ‘the rural-background effect diminished over time and may need continued support during training and full practice’. Shires et al14 illustrate this urban drift of graduates after postgraduate year 3 from a regional medical school. In a study of Australian general practitioners based on data from the MABEL study, McGrail et al21 found that there was a strong significant association between ‘rural training pathways and subsequent rural practice that was sustained for 5 years after vocational registration’. Other researchers have expressed a need for additional rural posts for internships and vocational training in rural areas22,23. A survey of 1645 members of the RACGP found that a quarter of respondents reported practising in a rural location at the time of the survey with strong associations between having a rural childhood (at least 1 year in RA2–5 before age 18 years) and rural exposure (during medical training as an intern, resident or registrar)23. It is often argued that rural background is a confounding factor when looking at rural exposure; however, when Runge et al23 analysed only those respondents with a metropolitan background, respondents who had done their internship in rural area were 5.3 times more likely to be in rural practice than those without rural exposure (OR 5.33, 95%CI 1.6–17.60, p<0.01). The recently announced Regional Training Hubs and National Rural Generalist Pathway development will be important in facilitating increased opportunities to continue to train and work in rural areas.
By 2012, only five RCSs had developed a system to track the practice location of their graduates22. The present pilot study provides systematic research on outcomes because it was based on all domestic medical students graduating from multiple RCSs in 2011. Fourteen of 15 RCSs that agreed to participate in this study provided de-identified data for their students, although two RCSs had not begun collecting rural origin information in 2011 and were excluded from this analysis. However, the methodology developed for the pilot is simple and straightforward and can be repeated easily for additional studies. For example, the pilot was a cross-sectional study that only looked at practice location at 5 years postgraduation, when the majority of graduates would not yet have completed vocational training. Furthermore, the study did not include other factors known to be related to rural work such as bond status, nor did it examine the effect of rural clinical placements longer than 12 months. It is possible that some graduates may be training in metropolitan areas, yet have rural practice intentions post-training. It would be useful to do another cross-section at 10 years postgraduation after the majority of graduates would have completed vocational training. Additional future research could include factors known to be associated with rural work, such as socioeconomic background17, rural intent on entry to medical school24, time spent in rural training as a postgraduate21, and entry to a general practice rather than specialist college25.
Conclusion
There is now solid national evidence to indicate that RCSs are associated with a statistically significant improvement in rural workforce relative to urban trained peers. These results are additional to the known positive effect of rural background in recruiting a rural workforce, which this article also demonstrates. These results confirm previous data reported by individual RCSs. Furthermore, these data most likely represent the earliest stages of a rural workforce, since postgraduate year 5 represents a relatively junior medical cohort. The rurality of cohort may continue to accrue as graduates attain vocational college membership and enter stable long-term practice. The development of a vocationally qualified rural workforce is expected to take a further 5–10 years. Ongoing funding is therefore important to fulfil the Commonwealth mandate to produce a locally trained graduate workforce.