Introduction
The role of point-of-care ultrasound (POCUS) in assessing patients with suspected abdominal aortic aneurysm (AAA) and blunt abdominal trauma (focused assessment with sonography in trauma (FAST)) is well established in emergency medicine. These are often the first POCUS examinations that urban emergency physicians learn1. The potential benefits of POCUS may be even greater in rural settings2, where access to imaging modalities, including ultrasound, is generally limited. There are, however, few published studies to support the use of POCUS in the rural context.
New Zealand’s dispersed rural communities are served by 26 rural hospitals staffed by rural general practitioners and rural hospital generalists. Only two of these hospitals have onsite surgical services, few have onsite ultrasound and at the time of this study only three had onsite CT3. Nineteen percent of New Zealand’s population is reliant on rural health services4. When compared to non-Māori New Zealanders, Māori are more likely to live in rural areas and are twice as likely to die as a consequence of AAA5,6.
Ruptured AAA can be a particularly problematic presentation in rural medicine. Survival falls rapidly with delay to definitive treatment, which can only be provided in a major surgical centre. The symptoms and signs are non-specific and unreliable, resulting in a misdiagnosis rate of 30%7. CT and formal ultrasound are frequently unavailable in rural areas, particularly outside normal working hours3,8. Rupturing AAA is most often mistaken for renal colic and diverticulitis, both of which are more common than AAA and can often be managed on an outpatient basis or in small rural hospitals9. Therefore a reliable ‘rule out test’ for AAA in the rural context has the potential to reduce the number of patients being transferred to exclude what is an important, but infrequent, diagnosis.
There are close parallels with the use of FAST to assess blunt abdominal trauma, another common rural presentation. As with AAA, the physical signs are unreliable but the consequences of missing solid organ injury can be potentially serious. Despite its limitations, the assessment of blunt abdominal trauma in rural areas is still frequently reliant on careful clinical assessment and serial observation.
The aim of this article is to evaluate two common POCUS examinations, AAA and FAST, in the rural New Zealand context, in particular the ability of the rural generalist doctors to obtain and correctly interpret images, and the impact of these POCUS examinations on diagnostic decision-making and patient management.
Methods
This study is the subgroup analysis of a larger study that examined the use of POCUS in six geographically dispersed rural hospitals in New Zealand10,11. None of the study hospitals have onsite surgical services. A more detailed description of the methods, study limitations, the characteristics of the participating doctors (including POCUS training), the hospitals and patients scanned is published elsewhere10,11.
Twenty-eight POCUS active rural generalist doctors were enrolled for a 9-month period during 2012. Each time they undertook POCUS as part of their routine clinical duties they completed a questionnaire both before (pre-test) and after the POCUS (post-test). This recorded the estimated likelihood of the major diagnoses being considered (diagnostic probability) and the planned patient disposition (discharge, admission to the local rural hospital or transfer to a specialist base hospital by road or air). The differences between pre-test and post-test recordings were used to measure the impact of POCUS on diagnostic decision-making and patient disposition. The participating doctors also recorded on the questionnaire their impression of the image quality (self-reported scan quality) and their interpretation of the images (POCUS findings).
The clinical records were reviewed by the investigators and if there was any doubt about the impact the POCUS had on patient management, the case was referred to a specialist panel (comprising an emergency physician with interest in POCUS, a radiologist and a sonographer). Where possible, definitive findings were determined based on the results of formal diagnostic imaging (CT or ultrasound), the final diagnosis or a review of the saved POCUS images. The impact of POCUS on the patient management was assessed by the investigators and specialist panel as either nil, some, significant, major or negative. ‘Some’ impact on patient management included confirming a diagnosis that was likely to have been made without the scan or ruling out an important but very unlikely diagnosis. Examples of ‘significant’ impacts on management included changing the intended patient disposition (eg deciding to discharge a patient that might have otherwise been admitted for observation) or leading to a diagnosis that was unclear prior to the scan. To meet the threshold for ‘major’ impact there had to be evidence that the POCUS avoided major disability or death. ‘Negative’ impact was any situation in which it appeared the patient would have been better not to have had the POCUS scan (ie it delayed the correct diagnosis or resulted in inappropriate clinical management).
When they were available, the recorded POCUS images were reviewed by the sonographer on the specialist panel. The quality of the images was assessed (assessed scan quality) and the sonographers interpretation of the images compared with the participant’s interpretation (scan interpretation).
Statistical analysis was undertaken using the Statistical Package for the Social Sciences v23 (IBM; http://www.spss.com). Descriptive statistics were used to describe outcomes. True and false positive rates were derived by comparing participants’ POCUS findings and the definitive findings (gold standard). Sensitivities, specificities and positive and negative likelihood ratios were calculated using MedCalc (MedCalc Software; https://www.medcalc.org/calc/diagnostic_test.php). Spearman correlation coefficient was used to establish the correlation between the patients’ pre and post-scan disposition and between the post-scan and actual disposition.
Ethics approval
Ethics approval was obtained from the New Zealand Multi Region Ethics Committee (MEC/10/09/091).
Results
Sixty-four POCUS AAA scans and 87 FAST scans were undertaken during the study. Study outcomes are presented in Table 1.
Three false positive AAA scans were identified. All three were due to participants bisecting the aorta obliquely in the transverse view and in doing so obtaining a falsely elevated measurement of the diameter.
Three false negative FAST scans were identified. Two were likely due to participant error. In one case, review of the POCUS images demonstrated free fluid, which was overlooked. Although this did not result in an adverse outcome, it did delay the transfer to a city hospital. Because of this delay, this scan was judged by the specialist panel to have had a ‘negative’ impact on the patient’s care (Table 1). In another case, while POCUS images were not available for review, the patient had a formal ultrasound very soon afterwards that clearly demonstrated free fluid. In the third case, a small amount of free fluid was seen on CT but it is possible this would not have been visible with POCUS. The participant also failed to save images for this case.
Figures 1 and 2 illustrate the impact of POCUS on diagnostic probability. Having undertaken POCUS, the participating doctors were more confident that the diagnosis being considered was present or absent (high or low probability). The diagnoses being considered by the participants were rupturing AAA and solid organ injury from blunt abdominal trauma. POCUS AAA was more likely to provide certainty (probability of 0% or 100%) than FAST.
For AAA, for 15% (9/59) of patients the test altered planned patient disposition, as illustrated in Figure 3. There was a strong correlation between pre-test and post-test disposition (Spearman correlation=0.67, n=59, p<0.01) and a stronger correlation between post-test and actual disposition (Spearman=0.75, n=57, p<0.01). Correlation between pre-test and actual disposition was the poorest (moderate) (Spearman=0.57, n=57, p<0.01).
For FAST, for 20% (17/85) of patients the test altered planned patient disposition, as illustrated in Figure 4. There was strong correlation between pre-test and post-test disposition (Spearman correlation=0.67, n=85, p<0.01) and between pre-test and actual disposition (Spearman=0.68, n=85, p<0.01) as well as a very strong correlation between post-test and actual disposition (Spearman=0.93, n=85, p<0.01).
Table 1: Study outcomes for rural point-of-care ultrasound for abdominal aortic aneurysm and focused assessment with sonography in trauma undertaken by 28 New Zealand rural physicians for 9 months in 2012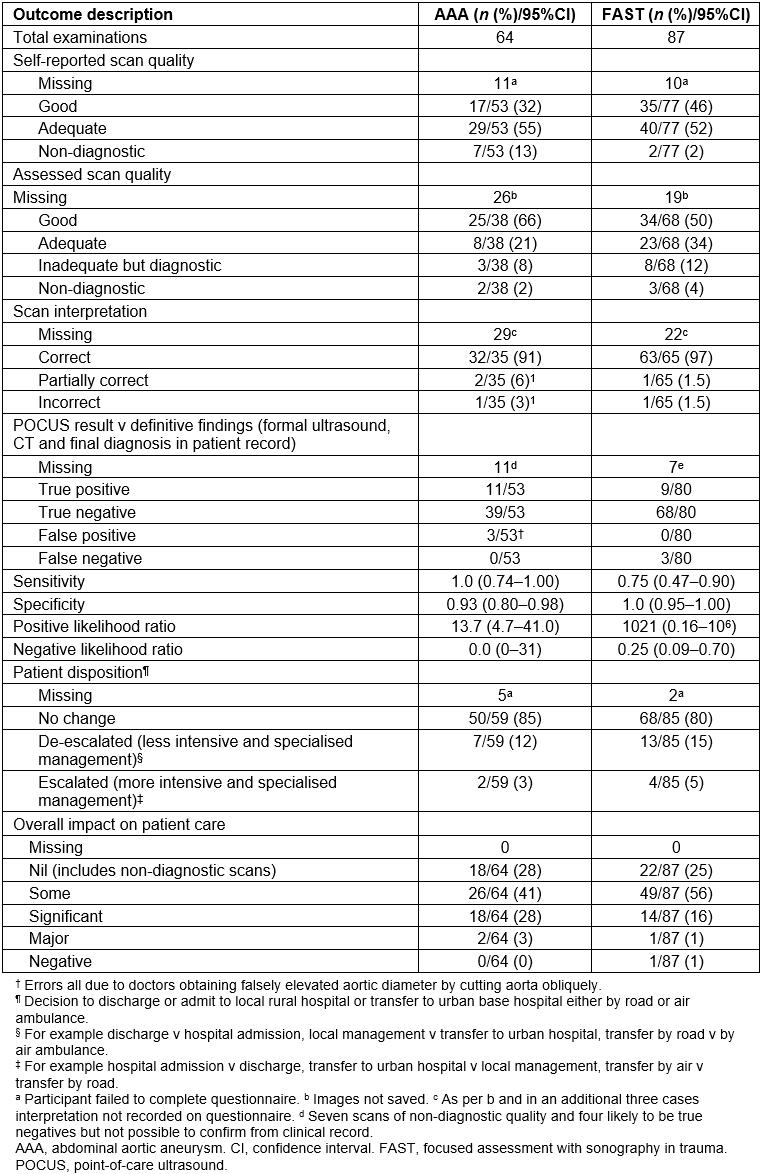
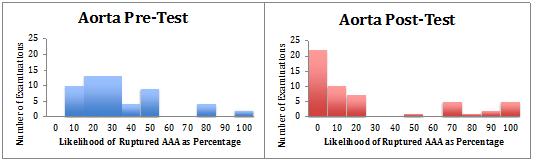 Figure 1: Physician-reported likelihood, before and after point-of-care ultrasound, of presence of ruptured abdominal aortic aneurysm.
Figure 1: Physician-reported likelihood, before and after point-of-care ultrasound, of presence of ruptured abdominal aortic aneurysm.
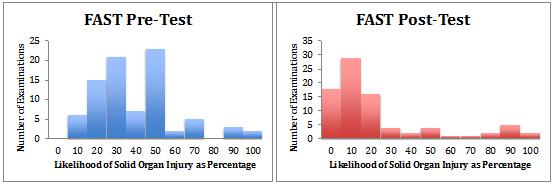 Figure 2: Participant-reported likelihood, before and after focused assessment with sonography in trauma, of presence of solid organ injury.
Figure 2: Participant-reported likelihood, before and after focused assessment with sonography in trauma, of presence of solid organ injury.
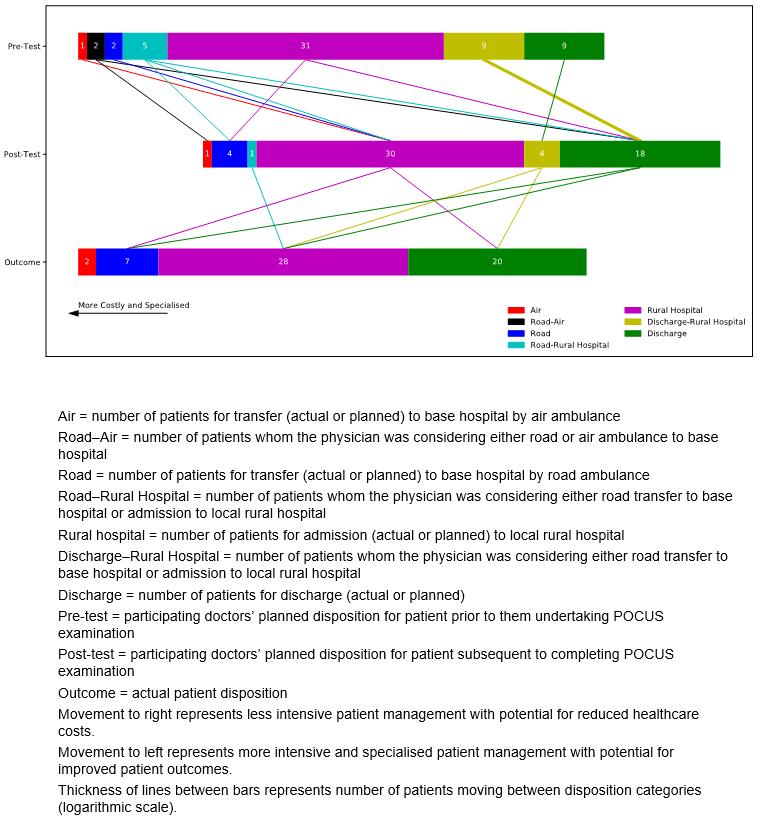 Figure 3: Impact of point-of-care ultrasound on the planned disposition of patients and the actual patient disposition for abdominal aortic aneurysm scans.
Figure 3: Impact of point-of-care ultrasound on the planned disposition of patients and the actual patient disposition for abdominal aortic aneurysm scans.
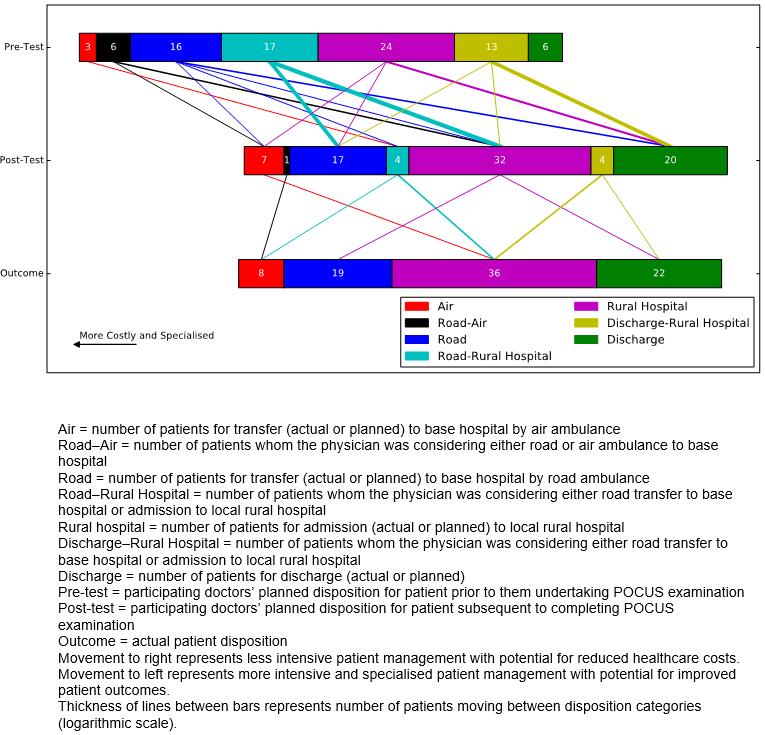 Figure 4: Impact of point-of-care ultrasound on the planned disposition of patients and the actual patient disposition for focused assessment with sonography in trauma scans.
Figure 4: Impact of point-of-care ultrasound on the planned disposition of patients and the actual patient disposition for focused assessment with sonography in trauma scans.
Discussion
AAA
In this study, POCUS AAA by rural generalist doctors was both sensitive (100%) and specific (93%). The participants appeared capable of both obtaining images of diagnostic quality and interpreting them correctly. This is consistent with a systematic review of comparable studies in the emergency medicine literature that quotes a sensitivity of 99% and specificity of 98%12.
The authors can conclude that POCUS AAA is a reliable ‘rule out’ test for AAA in the rural context. It is therefore not surprising to find that it improved diagnostic certainty and often altered patient disposition, often having a significant (28%) and occasionally a major (3%) benefit on patient care without evidence of patient harm. It is a particularly useful tool in the assessment of older patients with unexplained abdominal pain at a distance from other imaging and surgical care.
It can at times be difficult to find a good sonographic window in the upper abdomen in unfasted patients who are in pain, which could account for the 13% of scans that were non-diagnostic. The false positive rate (6%) could be reduced by an increased emphasis on the importance of measuring the aorta in a true transverse plane by those who teach POCUS to rural doctors.
FAST
By contrast, from the cases examined, FAST was a highly specific (100%) but less sensitive (75%) examination than POCUS AAA. This is consistent with previous larger studies in the emergency medicine literature, which quote sensitivities as low as 42% but specificities of 95%13,14. The loss of sensitivity was due to operator error (failure to identify free fluid) and limitations of the technique (inability to detect small amounts of free fluid). These factors have the potential to negatively impact patient care if doctors lack the necessary technical skills or are unaware of the examination’s limitations.
Although it did not perform as well as POCUS AAA, FAST frequently improved diagnostic certainty and had a positive impact on patient care. This study reinforces the importance of not using POCUS FAST as a ‘rule out’ test14, something that reduces its utility in the rural setting and needs to be emphasised by those teaching this technique to rural doctors. However, as a ‘rule in’ test it can on occasions appropriately escalate the level of care or urgency of transfer with the potential for improved outcomes.
Patient disposition
The decision to transfer a patient to a distant urban hospital by road or air ambulance is a routine part of rural medical practice that has major implications both for the level of care the patient will receive and resources (costs to both patients and to the healthcare system). In this study, POCUS AAA and FAST altered planned disposition for 13% and 18% of patients respectively. The strong and very strong correlation, respectively, between post-test and actual disposition suggests POCUS is prompting decision-making in the direction of appropriate patient management. Overall, POCUS reduces the need for hospital admission and inter-hospital transfer, suggesting potential savings for the healthcare system.
The size of the study and incomplete data are significant limitations of this study. The participants collected the data while undertaking their routine clinical duties in a group of dispersed rural health facilities. This generated useful information on the role of POCUS in the rural context but created the potential for bias, which could have occurred if participants failed to include particular cases, omitted some information, or provided incorrect information, on the study questionnaires. Also, the data were collected in 2012, and POCUS is a rapidly developing field.
Conclusions
This is the first study, that the authors are aware of, to examine the impact of FAST and POCUS AAA on acute patient management in the Australasian rural context, and one of the first in any rural context. The results are consistent with those of larger emergency medicine studies undertaken overseas, namely that POCUS AAA is a good ‘rule out’ test for AAA and POCUS FAST a good ‘rule in’ test for solid organ injury.
This study has demonstrated that POCUS AAA and FAST increase diagnostic certainty and have a direct impact on patient management including decisions to discharge or transfer patients, in ways that improve clinical care, increase the number of patients that can be safely discharged and reduce healthcare costs.
The authors recommend that POCUS for AAA and FAST should form part of the POCUS scope of practice for rural generalist doctors.
Acknowledgements
The authors thank Dr Rosylne McKechnie and Ms Bron Hunt for administering the data collection and analysis, and for liaising with the participants.




