Introduction
Worldwide, postpartum haemorrhage (PPH) is the leading cause of largely preventable maternal mortality1-3. While the worldwide maternal mortality ratio (MMR) decreased by almost 44% between 1990 and 2015, largely due to improved access to family planning, access to skilled birth attendants and provision of basic obstetric care remain limited for some women, contributing to inequalities in women’s birthing outcomes4. The MMR in less-developed regions, for example, is estimated to be 14 times higher than in more developed regions, accounting for 99% of global maternal deaths in 20153,5. Of those maternal mortalities, rural women are most affected, attributable to inequalities in access to maternal and childcare services6-13. The highest risk to preventable maternal death is obstetric haemorrhage (27%), of which PPH, characterised by bleeding (>500 mL) after delivery is the most common2,3,14,15. The risk of dying due to PPH is increased in women with pre-existing medical conditions and, in particular, anaemia, which remains a significant burden among women in less-developed regions2,16-19. Even where women survive PPH, they may experience severe morbidity and long-term psychosocial sequelae17,20.
The most effective preventative strategy for PPH is active management of the third stage of labour2,8,21. This includes administration of a prophylactic oxytocic, either oxytocin by injection or misoprostol orally1,2,22. Oxytocin is WHO’s recommended oxytocic for prevention and treatment of PPH2. Oxytocin however, requires administration by trained healthcare providers, sterile injection equipment and storage at 2–8°C23,24. In lower–middle income countries, where many women continue to deliver at home, maintaining cold chain requirements for oxytocin is often not possible due to poor power supply and refrigeration facilities23,25. Some oxytocin injectable products are more heat stable and can be stored below 25ºC, suggesting they can be stored under some ambient conditions. These products, however, are unsuitable for use in many lower–middle income countries, where hot climates and resource limitations would result in exposure to temperatures greater than 25ºC24, making oxytocin unviable in many rural areas in lower–middle income countries11,23. In such circumstances, WHO’s and other international guidelines recommend community distribution of oral misoprostol for prevention of PPH2,8,21,23.
Lao People’s Democratic Republic (Lao PDR) is a lower–middle income country in South-East Asia26. The country is characterised by a diverse topography and a mainly rural, ethnically diverse population, amplifying the challenges in providing equitable access to skilled health care27. While the MMR has decreased, largely due to improved access to family planning and access to skilled birth attendants, at an estimated 197 deaths/100 000 live births, the MMR remains the highest in the region, with PPH the leading cause of maternal mortality and morbidity28. To reduce the MMR, the Laotian government introduced a free maternal health services policy (now integrated under a national insurance scheme), which provides pregnant women free access to maternal health services and covers treatment costs, transportation (with a co-payment), food allowance, and an incentive to attend four antenatal care appointments29,30. Coverage of services in rural and remote areas, however, remains limited. To access services from the village level to a health centre, patients usually walk or use their own transport. District hospitals have an ambulance they use for referral of patients to the provincial hospital, with the cost covered through the national health insurance scheme with a co-payment31. Sometimes patients may bypass one level of care depending on their condition or if road access to a higher level facility is easier. Access to transport and transport costs in very remote areas present a considerable barrier to referral for the poorest communities31.
The Lao Ministry of Health includes oxytocin in the essential medicine lists, and it is recommended under the standard treatment guidelines as first line for prevention and treatment of PPH in district and provincial level hospitals. At the health centre and community level, however, oxytocin is always unviable due to the requirements for maintenance of a cold chain, access to sterile injectable equipment and trained health care25. Furthermore, despite the free maternal health services policy, approximately 45% of women in rural areas continue to deliver at home without a skilled birth attendant28. Many are from ethnic minority communities, living in mountainous areas with limited access to health care and a preference for home delivery due to social and cultural practices28,29. To prevent PPH for women who do deliver at home without access to a skilled birth attendant and oxytocin, the Lao PDR National Strategy and Action Plan for Integrated Services on Reproductive, Maternal, Newborn and Child Health 2016–202532 now includes the prophylactic use of oral misoprostol for PPH as an interim measure to decrease maternal mortality from PPH.
In cases of home delivery without a skilled birth attendant, the recognition of early signs of PPH is critical in preventing delays in seeking skilled health care33,34. Little is known, however, about how women, especially ethnic minority women in rural and remote areas, understand and manage postpartum bleeding, or how they may feel about a medication to prevent this bleeding. To inform implementation of a PPH prevention program, it is crucial to assess local beliefs and practices relating to pregnancy and labour, including attitudes to health care and the administration of oral medication to prevent PPH8,35. In other similar settings, traditional beliefs around pregnancy and bleeding have been identified as both barriers and facilitators to improving maternal health, and directly impacted upon education and training of healthcare workers and women themselves34,36-40. Taking these local beliefs and attitudes into account can help to ensure education and information is easily understood, appropriate for the target group, and addresses potential barriers in acting on public health messages.
The purpose of this study was to understand community perceptions and management of postpartum bleeding during home births, to examine strategies used to identify excessive bleeding, and to assess the potential acceptability of oral medicine to prevent PPH. This builds on previous research at the central, provincial and district levels within Lao PDR highlighting key policy and operational factors related to community-based misoprostol distribution41,42. The intent is for the findings of this study to inform public health interventions for PPH prevention that are sensitive to the needs of women and their families in remote Lao communities.
Methods
Study design
This was a qualitative study based on five focus group discussions (FGDs) in five remote communities, complemented by key informant interviews (KIIs) with village health volunteers (VHVs), village health workers (VHWs), community leaders and health centre staff (midwife/health worker).
Study setting
The study was undertaken in the north-west of the Lao PDR in three districts: La, Namo and Nga, situated within Oudomxay province. These districts are ethnically diverse and have a mountainous topography. Oudomxay has high maternal mortality and low rates of births attended by any skilled personnel28.
Within Lao PDR, tertiary hospitals are based in the national capital, Vientiane, with second-tier hospitals in each provincial centre, and first-level referral hospitals at the district level. At the subdistrict level, health centres (souksalas) serve several surrounding villages42,43. These centres usually have at least one staff member who has completed a variable level of training in primary health care or nursing. Within each village is a VHV, a community member trained as a lay health worker. Many villages also have a VHW, with the intent to have a VHW in every village. The VHWs are a relatively new cadre and, unlike VHVs, are government employees who have at least 7 years of schooling and have undergone a 6-month generalist training program in basic primary health care, but are not trained as skilled birth attendants. Typically, the VHWs also conduct antenatal and postnatal visits for birth preparedness, and health education around care of the mother and newborn. The village head (Nai Ban) provides leadership and administrative duties supported by key village personnel, such as representatives from the Lao Women’s Union.
The villages included in this study were of Khmu, Hmong-Mien and Tibeto-Burman ethnicity. All were in extremely mountainous terrain and accessed in the dry season by a four-wheel-drive vehicle. Access during the wet season is limited, with villages isolated from both the souksala and district hospital. Families live a semi-subsistence agrarian lifestyle, with simple traditional housing of mainly wooden walls, an earthen or wooden floor and thatched roof. There is limited access to potable water and sanitation.
Sampling
Criterion sampling was used by obtaining a map of known villages from each district health office to select five villages for the FGDs44. Village selection was based on (1) known cases of PPH as reported by the District Health Director, (2) travel time from the provincial capital (2–4 hours), (3) distance to the district health service (>4 km)4 and (4) population (50–150 people). Criterion sampling ensured included villages were likely to provide information-rich data and opportunities for appropriate interventions to reduce PPH44. The sampling also ensured a diversity of ethnicity between villages. This resulted in selection of the five villages farthest from the district health service (from Namo, Nga and La districts) with the following ethnic groups: Khmu (n=2), Akha (n=1), Lanten/Yao Mien (n=1) and Hmong (n=1). In total, 34 participants were included in FGDs (n=34). Additionally, VHVs/VHWs, community leaders (n=7) and health centre staff (midwife/health worker, n=2) were interviewed.
At the village level, nomination sampling was used whereby, upon arrival, available and appropriate participants likely to be relevant sources of information were nominated by the village head, VHV or VHW44. In each village, five to nine FGD participants were selected based on the inclusion criteria: women aged 18–40 years, women with children aged less than 5 years, and husbands, mothers or mothers-in-law of these women, if culturally appropriate (Table 1). In consultation with key village informants (village heads, VHVs and VHWs), the most appropriate format for the interviews was determined as women only; a combination of women, mothers or mothers-in-law; or a combination of women, mothers or mothers-in-law, and husbands. In line with cultural norms, women were invited to bring children to each FGD.
Table 1: Study participants in interviews and focus group discussions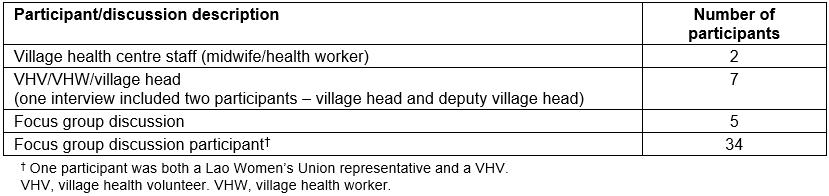
Data collection
KIIs and FGDs were conducted in each study village using semi-structured interview guides8,35. KIIs aimed to reach an in-depth understanding of each participant’s opinion and perceptions of the topic, while FGDs aimed to collect a diversity of views, actively encouraging contributions from all participants44. Semi-structured interviews enabled coverage of all relevant areas of interest but still allowed participants to raise issues of interest44-47. Interviews and FGDs were recorded with informed consent, using an audio-recorder with written summary notes. Data collection included questions on women’s beliefs about postpartum bleeding, recognition and management of PPH (including acceptability of taking an oral medication immediately after delivery to prevent PPH) and access to health care and health-seeking behaviour related to child birth.
Interviews and FGDs were conducted in Lao, English or the ethnic language most suitable for the sample group and simultaneously translated by native speakers. All transcripts were translated into English, back translated where necessary for accuracy and checked against interview recordings.
All questions were checked for cultural and linguistic appropriateness. Refreshments were provided during FGDs, and a small gift of soap, adhesive bandages and antiseptic cream was given to participants in recognition of participants’ time. Participants were not aware of the gift before the interview, and the gift was not considered large enough to be coercive.
Data analysis
Data analysis commenced during the data collection process for an initial understanding of participants’ perceptions of PPH and to inform further interviews. Subsequently, all transcribed data were reviewed several times and differences and similarities identified to capture themes and patterns related to the research questions. This process gave a sense of the entirety of the data before the entire data set was coded. Extracts from the coded data were entered into as spreadsheet as thematic patterns were identified in relation to the research objectives. Interpretation of the data themes and coding was an ongoing process, with codes and themes checked by the research team45,48.
Ethics approval
Ethics approval for this study was granted in Australia and Lao PDR by both the University of Queensland School of Public Health Ethics Review Committee (approval IH101015), and the National Ethics Committee for Health Research, Ministry of Health of Lao PDR (approval 004). All data were de-identified. It was stressed that participation was voluntary, and participants could withdraw at any time and decline to answer any question. Hard copies of informed consent and information sheets were provided to all participants who requested them. Where participants were illiterate, informed consent and information sheets were read to participants in their preferred language. Given the low levels of literacy, both ethics review committees gave approval for illiterate participants to either be assisted to sign their name or to provide witnessed verbal consent, depending on their preference. Written consent was obtained from all other participants.
Results
Traditional beliefs about postpartum bleeding
In the FGDs, participants stated that bleeding after child birth was a normal cleansing process. They stated postpartum bleeding should typically continue for several days and would stop naturally. Normal bleeding was characterised as bleeding that is intermittent, slow-flowing and decreasing over 3–5 days. Participants also associated normal bleeding in the first days after delivery with pelvic pain (afterbirth pains) and viewed this as a natural process. A few women expressed this normal bleeding as expelling ‘bad blood’ from the body. If this ‘bad blood’ was inhibited, it would be retained in the women’s womb and likely result in complications. The following quotes illustrate how some women viewed ‘normal’ or ‘good’ bleeding that if stopped would prevent mothers returning to a state of good health and cleanliness:
We’re concerned that stopping bleeding, we believe that the bleeding blood is … blood that is bad, it’s a bad blood for the body to get this out. So, if we stop the bleeding, the bad blood will stay inside the body, so the body will be dirty, unhealthy. (FGD_01)
If the bleeding is feeling good, she will not feel blurred vision or vertigo. If the blood is less, she will feel not good, she will have vertigo and blurred vision. (FGD_02)
One health centre staff member explained how typically after giving birth, the mother lies with her head higher than her feet in the belief that the ‘bad’ blood would come out and ‘take all the blood clots out of the uterus’ (KII_17_health centre).
Recognising and managing PPH
While not skilled birth attendants, some of the VHVs/VHWs interviewed had witnessed cases of PPH or had heard about cases through their home visits. These VHWs and VHVs explained that they recognised PPH as continued heavy bleeding after delivery, alongside signs of the mother becoming weak. In the FGDs, women characterised PPH as bleeding that is steady and continuous, associated with pallor, weakness, feeling dizzy and fainting, with the mother starting to grow weak. One woman also noted that this PPH could lead to loss of appetite:
If it [blood] comes out more … they will feel the body is very heavy. Cannot lift the body, they will feel eating food is quite allergic to them – they may be allergic to some food [loss of appetite] – if their bleeding is more than three days. (FGD_02)
If it takes longer days, it’s dangerous. It must be less and less. If it’s more and more, it makes you can’t eat, can’t stand or even you can’t hold your baby. (FGD_01)
While describing PPH as constant and potentially hazardous, neither the women nor VHWs/VHVs were able to describe ways of estimating the volume of blood loss. In labour, when women showed signs of PPH, traditional treatments were described as the first course of action. These included performing a spiritual rite, taking a warm bath, drinking plenty of water and/or traditional herbal tea, as one participant stated:
First, we call elderly people for give a pray, [then] if it’s getting worse, we look for a medicinal root [to make a tea]. (FGD_01)
Other participants mentioned using a cold compress on the abdomen and abdominal massage to stop PPH. In one village, women talked about following the practice of lying on a ‘hot bed’ under which embers and traditional herbs are placed, typically for 10–35 days postpartum, to help the uterus contract, reduce pain and allow the mother to return to health. One VHW explained how he had tried to assist a woman in the village with a PPH by taking a hot cloth and using it to massage the pelvic area.
Some people, especially the VHWs, stated when a woman experienced PPH, they should attend a health facility. In general, VHWs/VHVs were aware of the Ministry of Health policy of referring cases of PPH to hospital and recognised the value of this policy. As such, VHWs/VHVs would recommend women seek treatment at hospital; however, they acknowledged that poor road access, lack of transport and/or costs often preclude this from happening. In one FGD, participants stated the local hospital could give ‘some drug injection’ (FGD_03) to stop the bleeding.
While many participants described late symptoms of PPH, recognition of the causes was generally poor. There was some understanding, however, mainly among VHWs, that an atonic uterus or retained placenta were among the causes of PPH. The latter was recognised as a danger sign and, in the absence of a skilled birth attendant, a common way of removing the placenta was to employ the use of a piece of bamboo to wrap around the umbilical cord to apply traction:
Slashed into two parts and wrapped around the cord. (FGD_3)
Access to healthcare facilities
In every FGD, women saw themselves as the main decision makers on whether to go to a healthcare facility during labour:
Only they [women in labour] can make the decision because no one has labour pains like them, they have their own labour pains, so they decide where they can deliver for themselves. (FGD_01)
Themselves. No one can force them even their parents. They just don’t want to go to the hospital. (FGD_05)
However, women often consulted their husbands, mothers or mothers-in-law about where to deliver:
We discuss with our husbands and mothers-in law but they don’t have the condition [of being pregnant] so they have no choice. (FGD_02)
We do talk to our family, especially our husbands. (FGD_04)
However, barriers to presenting at a health facility generally included economic and logistical considerations, and dissatisfaction with healthcare staff attitudes. For example, women often felt the health staff were dismissive or impolite and that they were stigmatised for their ethnicity. Other barriers to attending a health facility included language barriers, and cultural and social preferences. Further impediments included postpartum bleeding being attributed as normal, inability to accurately recognise when postpartum bleeding was becoming excessive, and reliance on traditional spiritual beliefs and practices. Women from an Akha village explained that, traditionally, the mother and newborn baby cannot leave the house for 13 days. Although in the past this may have prevented the seeking of trained health care altogether, it was recognised by the younger women that in the case of PPH both mother and child could go to the hospital. Alternatively, the mother could travel for assistance while leaving her baby in the care of her mother-in-law. Reasons for the tradition were unclear:
We don’t know. We just follow our traditional rules. After 13 days of delivery, the baby will be able to go out. (FGD_05)
Most women did not think their decision to seek health care would be influenced by the gender of healthcare workers. Akha women however said they felt uncomfortable when male staff undertook vaginal examinations or saw them naked, which may affect health-seeking behaviours:
Yes, the women do not allow the male doctors to help them for delivery, only female doctors are permitted. (FGD_05)
Other reasons for not seeking health care, even when signs of complications were recognised, related to determinants of access. These included transport costs or the lack of available transport, poor road conditions or no roads at all in some mountainous locations, long distances to healthcare facilities, attitudes of healthcare staff, language barriers, privacy issues, and perceptions of cultural and social inappropriateness of the formal healthcare sector:
Last year because of no car, one mother died because the placenta did not come out. (KII_25_village)
There is very difficult road to reach there [hospital] so I deliver at home. (FGD_02)
We don’t go because we are shy, so we choose to deliver at home ... Mostly [the reason is] because we don’t know anybody there and we don’t understand the language. (FGD_05)
Acceptability of oral misoprostol for PPH prevention
In each village, women were generally in favour of taking oral medication immediately following delivery to prevent PPH. This was especially the case if the treatment was recommended by a healthcare worker and if medication would not prevent normal postpartum bleeding. As one woman explained:
If it can confirm that it is stopping blood and the body is clean, then OK we will take but if it stops bleeding right away then the mother will be concerned about bad blood still keep inside of her … it should be little by little stopping, if it’s immediately stopped then it’s bad. (FGD_01)
To determine the acceptability of oral medication to prevent PPH, women emphasised the need for clear instructions on its use, storage and side-effects to be provided to everyone present at the birth. This could usually include the woman’s husband, mother or mother-in-law and a trusted senior village woman. Women suggested simple verbal and pictorial instructions as:
It might be hard to remember if the direction is a bit confusing. (FGD_05)
It was perceived that accessing misoprostol in the village would alleviate the difficulties faced in accessing healthcare facilities:
It’s good because some people live far away from hospital and if there is something wrong, we can take the medicine immediately. (FGD_01)
While misoprostol could be provided to women during antenatal care, according the healthcare workers and female participants, most women in the study area only have one, instead of the recommended four, antenatal care visits – usually to confirm pregnancy.
Most participants stated they would prefer to be given the medication immediately after, or close to, the time of delivery. Most women agreed it would be acceptable to receive misoprostol prior to delivery for self-administration provided that relevant information about the drug was supplied by an educated healthcare provider:
Anyone who has the knowledge on how to use the drug … Anybody who is educated. (FGD_05)
It is good to have the drug nearer the time of pregnancy because sometimes the village health volunteers are not at home or even away from the village, so it’s good to give it the woman nearer the date of delivery. (FGD_04)
Discussion
All women giving birth should have access to skilled birth attendants and active management of the third stage of labour, including administration of a prophylactic oxytocic, controlled cord traction and uterine massage after delivery of the placenta to prevent PPH2,8,21,49. In Lao PDR, while the government is committed to equity in access to appropriate care during delivery, many women who deliver at home without adequate management of the third stage of labour, including access to a prophylactic oxytocic, are especially vulnerable to PPH12. The purpose of this study was to understand community perceptions of postpartum bleeding, how this is managed during home births, and the acceptability of taking an oral medication such as misoprostol to prevent PPH in the immediate postpartum period when birthing at home. The study suggests that local beliefs and practices about postpartum bleeding, logistical access factors, and cultural and social inappropriateness of the formal healthcare sector influence healthcare-seeking behaviours. These insights could help inform the design of culturally appropriate public health interventions addressing PPH prevention in remote Lao communities.
Traditional beliefs about postpartum bleeding
This study indicates that, amongst labouring women, decreasing levels of blood loss in the postpartum period are considered a normal and necessary cleansing process, a finding observed elsewhere33,50,51. Women in Morocco, on the other hand, fear excessive bleeding, which they think drains the energy from the new mother52. Women in the present study felt that, while excessive bleeding may lead to feeling drained, they preferred to rid the body of ‘bad blood’ and may delay care-seeking as a result. In other settings where women also described the need to rid the body of ‘bad blood’, it was associated with delayed access to health care33,50,52,53.
Recognising and managing PPH
Women and VHVs were unable to explain a point at which normal bleeding becomes excessive, nor could they describe measurement of blood loss volume. Ambiguity around what constitutes PPH is common in rural communities in lower-income countries33,34,50,51. Some communities determine PPH based on the number of pieces of cloth soaked51. In Uganda, women and some traditional birth attendants felt PPH was equal to the size of two clenched fists33. In the same study, another woman used a plastic mug to measure the blood after delivery of the baby and placenta, with blood loss more than the plastic mug a sign of PPH33. The lack of clarity around the definition of PPH at the community level, alongside the fact that some bleeding is normal after delivery, may delay recognition that bleeding is at a dangerous level4,51. While unable to explain when normal bleeding becomes excessive, participants were able to describe some late symptoms of PPH related to hypovolaemia. In the Lao PDR context, and similar settings where rates of anaemia are high, this is of particular concern as even moderate levels of bleeding can place women at risk14.
In this study, and in other parts of South-East Asia, the practice of lying on a ‘hot bed’ or ‘hot bed roasting’ was reported to help stop postpartum bleeding54,55. This involves boiling a variety of herbs and having the mother sitting on a wooden bed over a fire for 30 days to flush out retained blood and placenta, increase involution of her uterus, flatten her stomach, remove stretch marks and heal perineal tears54. Lying on a ‘hot bed’ postpartum is also thought to help sweat out ‘poisonous’ water so that the mother can absorb ‘good’ water. This practice is commonly considered in these places to be an essential part of recovery, promoting physical recovery and perineal healing, protecting against puerperal fever, relieving symptoms of postpartum anaemia, stopping postpartum bleeding, stimulating expulsion of lochia and inducing lactation56. This practice is also thought to protect women in later life from a range of symptoms54. While lying on a hot bed may help to ensure adequate rest for rural women, there is no evidence linking these postpartum practices to stopping postpartum bleeding or illnesses in later life54.
Spiritual rites were reported by some women, particularly those from the Hmong village, as the first response to PPH. Other participants reported the use of a traditional medicinal tea to stop PPH; however, many women recognised this was often ineffective. Furthermore, taking oral fluids does not replace the lost blood volume33. The belief and reliance on the powers of spiritual healers or herbal teas to prevent PPH can act, however, as a delay to seeking care.
Despite breastfeeding immediately after delivery being promoted by the government, immediate post-delivery breastfeeding to assist prevention of PPH was not mentioned in interviews. Nipple stimulation is thought to help reduce postpartum bleeding by increasing the secretion of oxytocin, causing uterine contractions57. A Cochrane review, however, found inconclusive evidence that breastfeeding/nipple stimulation on its own reduces bleeding during the third stage of labour57.
Access to healthcare facilities
In this study, most respondents said the decision to access a health facility during labour was made primarily by women, following consultation with key family members. While participants were generally able to access souksalas, access was often restricted to the dry season only, with roads becoming impassable during the wet season. Even when health centres were accessible, participants reported barriers to access related to financial and logistical factors as well as sociocultural concerns. These related to real or perceived negative attitudes held by healthcare staff, language differences, concerns about privacy, and cultural and social inappropriateness of formal healthcare settings. As in other studies, the onset of labour at night and precipitate labour also prevented women from accessing health facilities, especially where road access was poor49,58. Other studies have also documented these challenges experienced by women in accessing health care in the case of complications during child birth, including PPH11,14,17,51,59.
Feasibility of implementing misoprostol for PPH prevention
While participants provided examples of how they managed PPH at the community level, they were also aware that these methods were often ineffective. To reduce morbidity and mortality secondary to PPH, this study suggests women need more knowledge on markers of excessive bleeding and when to seek care. Delivery with a skilled birth attendant and early initiation of breastfeeding should continue to be emphasised in promotional messages, usually delivered through printed materials and village leaders, to women and also to husbands, village elders and trusted opinion leaders. Reliance on traditional practices, combined with challenges in accessing healthcare facilities, may help to explain, at least in part, why self-treatment was reported as the first line of action in managing PPH.
Definitive prevention and management of PPH requires administration of an oxytocic2. Oral misoprostol provides a safe, effective prophylaxis for PPH during home births where oxytocin is unavailable2,8,21,23,24,34-38,49,59-61. Oral misoprostol can be provided through community-based healthcare workers for dispensation to women immediately after delivery, or by advanced distribution of misoprostol to women during late pregnancy2,34,61. Women in this study felt both methods were acceptable providing that the flow of ‘bad’ blood was not interrupted. Women also felt the person dispensing misoprostol should be trained in its use, and explain the correct administration and possible side-effects, a finding also reported in many developing countries34,36,37,39. In the case of self-administration, women emphasised the need for education for both for themselves and other family members likely to be present at the birth. This approach has been effective in other lower–middle income settings, especially where trusted educators have been used34,38,53,59,62.
A previous stakeholder analysis in Lao PDR found generally positive attitudes towards the prophylactic use of misoprostol for PPH as an interim strategy, while also continuing to increase access to facility-based birthing and oxytocin42. In the present study, key informants recognised the benefits of and promoted facility-based birthing. They were, however, also supportive of the Ministry of Health’s policy of community distribution of misoprostol to prevent PPH in the absence of a skilled birth attendant32, providing that VHVs/VHWs and women and their families were given adequate training and education. Other studies have demonstrated that, with training, community health workers can effectively and safely distribute misoprostol to women, increasing access to vital health care in areas with few alternatives11,34,63,64.
Limitations
This study has some methodological limitations that may have influenced the study findings. The use of interpreters may have influenced data collection, especially in non-Lao speaking villages where a second interpreter was utilised. All efforts were made to ensure accuracy of translation, including cross-checking and back-translation of audio-recordings with the interpreter(s). Despite the limitations, such as possible translation errors and loss of original meaning, it was important the voices of ethnic minorities were included in the study, particularly given the well-documented disparities in maternal health outcomes for women from ethnic minority backgrounds28. Power imbalances between researchers, interpreters and participants may also have affected data collection, with the researchers and interpreters fulfilling changing roles as ‘insiders’ and ‘outsiders’ in varying contexts65-67. The purposive sampling of villages and small sample size mean the data is not representative of Lao PDR as a whole, or of all remote areas in Lao PDR where the application of misoprostol may be beneficial.
Conclusion
Many women in this study considered bleeding after childbirth as a normal, cleansing process. They felt that ridding the body of ‘bad blood’ is essential to return a postpartum woman to full health. Respondents’ capacity to identify early signs of PPH was limited, and women generally only seek care when late-stage signs occur. Despite the national reproductive, maternal, newborn and child health policy emphasising facility birthing and increasing skilled attendance at birth, many rural women are likely to continue to deliver at home without a skilled birth attendant for various economic, logistical and cultural reasons. Traditional practices to manage PPH such as herbal teas and spiritual rites were commonly mentioned in this study. These practices may lead to delays in seeking care, ultimately contributing to maternal mortality and morbidity. These factors must be considered when developing preventative interventions.
Respondents agreed that implementing community distribution of misoprostol was feasible if supported by adequate healthcare worker training with clear, culturally and linguistically appropriate information on the correct use of misoprostol for women and their families. Well-developed interventions require an understanding of local perceptions for the intervention to be acceptable and sustainable for the target population. This study gained a deeper understanding of women’s experiences and perceptions of PPH. It can be used to inform strategies developed under the National Strategy and Action Plan for Integrated Services on Reproductive, Maternal, Newborn and Child Health, which also includes the introduction of community distribution of misoprostol. This should not detract, however, from the recognition of the benefits of facility-based birthing and the ongoing work of increasing equality and access to essential obstetric care throughout Lao PDR.
Acknowledgements
The authors would like to acknowledge the time and effort given by all interview and focus group participants for this study.
References
You might also be interested in:
2013 - Description of healthcare needs at an episodic clinic in rural southwest Virginia
