Introduction
People living in rural and remote areas have poorer health status than their urban counterparts and poorer access to health care1-3. The challenges of rural practice as well as the workforce issues for rural practitioners are well documented2-6. Boundaries between primary and secondary health care necessarily become more blurred the further the distance from urban centres where specialist and diagnostic resources are concentrated. Rural communities need access to a wide spectrum of health services including hospital and community-based care3,6.
In New Zealand (NZ) the current dominant model of care for health services is one of separated services for primary and secondary care, which dates back to NZ’s Social Security Act 19387. These services also have different funding streams: most primary care is provided through general practices working to a small business model with direct patient charges (co-payment) while free secondary care is provided via public hospital services operated by district health boards7,8. Within this health system framework, both general practice and rural hospital medicine have only relatively recently been recognised as having a vocational, as opposed to a general, scope of medical practice. (Note: Medical practitioners in NZ can practise either as vocational registrants in a recognised medical specialty or as general registrants, this latter group having undergone no vocational training program and having no affiliation with a professional college.)
In 1995, general practice was recognised as a vocational scope of practice with focus on providing community-based primary health care: there was no provision for the specific needs of rural areas9,10. The changing regulatory environment meant that hospital and emergency care was not part of general practice work11. Other vocational medical specialties (emergency medicine, 1995; urgent care, 2000) began providing emergency and acute care in NZ’s towns and cities12,13.
In rural NZ, things did not develop in the same way. Rural medical practitioners provide a wide range of services that in urban settings are provided by medical specialists and a range of other health professionals1,5,6,14. The NZ health reforms in the 1990s saw eroded health services for rural communities with the withdrawal of specialists from rural hospitals and the downgrade or closure of many facilities15. Increasing demands on rural general practitioners (GPs) to cover this care ‘gap’ contributed to a growing rural GP shortage16. Lack of rural specific medical training options and a rural-specific career pathway were seen as key obstacles to the rural medical workforce crisis17-19. The tendency to think of rural health as being limited to primary care as practised in the NZ urban context20,21 had put rural hospital and emergency care into an anomalous situation where the needs of rural communities were overlooked22.
Rural hospital medicine (RHM) was recognised by the NZ Medical Council as a new scope of practice in 200823.The new scope aimed to provide recognised training and professional development standards for medical practitioners working in rural hospitals23. It was intended that the new scope would also encourage the establishment of quality systems in rural hospitals23. The Division of Rural Hospital Medicine, now a chapter within the Royal New Zealand College of General Practitioners (RNZCGP), was established as the professional body for RHM. The RNZCGP is thus the professional home for two separate scopes: general practice and RHM24. Descriptions of the RHM pathways, the history of their development and their integration with GP training have been previously outlined25. The ‘dual pathway’ (combined GP and RHM training) has strong similarities to the ‘rural generalist’ pathways being developed in Australia25,26.
While previous studies have provided baseline information for the wider sector involved in workforce planning, little is known about the impact of the RHM scope in specific rural settings27,28. The aim of this qualitative case study was to explore how the RHM scope had affected health practitioners and the health service in one NZ rural community.
Methods
Study setting
Hokianga, an area in the far north of NZ, is regarded as a place of beginnings for Tangata Whenua (local indigenous people, NZ Māori)29,30. Hokianga has a population of 6500 people, with 70% identifying as Māori. The population is dispersed over an area of 1520 km2 with poor transport links31. Although historically and culturally rich, Hokianga is today one of the most economically poor populations in NZ32. An integrated (primary–secondary care) health service including a hospital, based on principles of equity, accessibility, affordability and cooperation, has operated in Hokianga since 194133. The model of care, funding and governance at Hokianga differs from most NZ health services. Maintaining the Hokianga health service over the years has meant adapting to policy, funding and regulatory changes31,34.
Today, Hokianga Health Enterprise Trust, or Hokianga Health, operates as an independent community-owned organisation. Health services are distinguished by the kaupapa (policy or purpose, NZ Māori) of its model of care, which is distinctively and uniquely Hokianga, Māori and community focused31,35. All services, in both primary and secondary care, are provided free at the point of care31.
The hospital, providing continuous inpatient and emergency care, has 10 acute, ten long-stay and four maternity beds. The nearest base hospital, Whangarei, is 126 km away. The nearest tertiary centre (closest cardiac, neurosurgical and vascular surgical intervention centre) is Auckland, 275 km away. There are about 750 acute admissions to Hokianga hospital each year of which around 20% are transferred. Medical staff (seven full-time equivalents) are employed by Hokianga Health and provide all medical services. Around half currently have dual vocational general practice–RHM registration35.
Funding for primary healthcare services is provided in association with the regional primary health organisation, while funding for the hospital is provided through the regional district health board.
Design, sampling and data collection
Document analysis was undertaken, providing background and context and as means of tracking change over time at Hokianga Health. Semi-structured interviews were conducted, providing in-depth individual perspectives. The two data sets were analysed sequentially and separately. The research subject was embedded in the real-life experience of the lead researcher. Measures taken for ensuring rigor in this context included explicitly acknowledging the insider status of the lead researcher in participant information and consent forms, using a reflective diary, team member reviewing of data collection and regular team discussion during the analysis phase36,37.
Document analysis: Documents were selected electronically (University of Otago search engines: search terms included 'Hokianga Health', 'rural hospital', 'RHM') and manually (Hokianga Health archives). The focus was on documents from 2000 to 2016.
Interviews: Semi-structured interviews were conducted between October 2016 and February 2017. Participants were either medical or non-medical and had been employees of Hokianga Health for a minimum of 6 months in 2006–2016. The interview topic guide explored the participant’s view of how the RHM scope of practice had affected their work and the health service. The topic guide varied slightly for non-medical participants. Average interview duration was 50 minutes and interviews were recorded and then transcribed for analysis. All transcripts were sent to participants to check accuracy and invite further edits.
Data analysis
Documentary analysis: This analysis was conducted (KB, SD, TS) using Bowen’s systematic document review method38. Documents underwent attribute coding to establish the meaning of each document, its original purpose and thus its contribution to the research question. Initial codes (key words and phrases derived from the literature review) were applied to each document in a first-pass analysis. Four documents with no codes identified were not further considered. Excerpts were then coded and collated using descriptive coding39. A comprehensive iterative analytical process (KB, TS, SD) led to the identification of overarching themes. NVivo v10 (QSR International; https://www.qsrinternational.com/nvivo) was used to manage the analysis.
Interviews: These were analysed thematically, using the framework method40. Analysis utilised an iterative process in which a framework of categories and themes (KB, TS) was developed from the initial open coding of transcripts (KB). After initial coding (KB) an analytical framework was developed (KB, TS) leading to the development of categories and themes. NVivo was used to manage the analysis. The consolidated criteria for reporting qualitative research (COREQ)41 were used to structure reporting of study methods and findings.
Ethics approval
Ethics approval for the research was obtained from the University of Otago Human Ethics Committee (16/085).
Results
Document analysis
Thirty documents were identified for analysis and 26 were included in the final analysis. Ten were internal to Hokianga Health, and included annual reports and meeting minutes. Sixteen were external to Hokianga Health and included district health board commissioned reviews and academic publications. Themes were embedded within a wider chronological narrative in three timeframes.
2002–2007, defining what Hokianga Health ‘does’: In a changing regulatory environment, part of Hokianga medical practice – the hospital aspect – was no longer regarded as general practice. At an organisational level, while Hokianga Health saw itself clearly aligned with the new national primary health strategy, hospital services were not considered in this strategy. These developments posed a threat to the Hokianga Health model of care.
An external review of Hokianga Health in 2007 assessed the clinical and financial viability of the inpatient service. Reviewers recognised the importance of a broad practice scope in enabling access to services for the population and described the hospital service as ‘acute inpatient GP care’. The review saw Hokianga Health retain its hospital service. Hokianga Health was becoming more aware of the importance of aligning with changing practice and nomenclature.
2007–2009, a new scope of medical practice and a new definition of a rural hospital: With the establishment of the RHM scope providing a match for the missing component of Hokianga medical practice, and the inclusion of Hokianga Hospital in a 2008 list of rural hospitals came a sense of national connection and belonging. External connections were strengthened, particularly with rural health networks and medical training institutions, Hokianga Health increased its teaching commitments and collaborated with NZ universities on a number of hospital-focused research projects.
2009–2016, a time of settling in and realignment with a new scope of practice and new definitions: Defining the hospital aspect of medical practice gave Hokianga Health validity and encouraged benchmarking, leading to quality hospital improvements including provision of diagnostics and credentialing. There was increasing recognition of RHM, perceived by the district health board as a new area of practice: ‘… increasing integration of rural hospital medicine specialist … and GP led models of care that blur traditional boundaries between primary and secondary care’. For Hokianga Health ‘traditional’ was blurred boundaries between primary and secondary care. A 2013 external review of the service acknowledged the relevance and value of Hokianga Health’s model of care. Challenges of the RHM scope were those associated with sustaining a workforce able to work across and meet the regulatory requirements of both general practice and RHM. The 2016 Hokianga Health annual report affirmed the positive impact of RHM: ‘The [RHM] … programme is invaluable to the future rural workforce and to Hokianga Health’.
Changing nomenclature used to describe Hokianga’s hospital service over time is shown in Table 1.
Table 1: Document analysis – changing descriptions of Hokianga Health service over time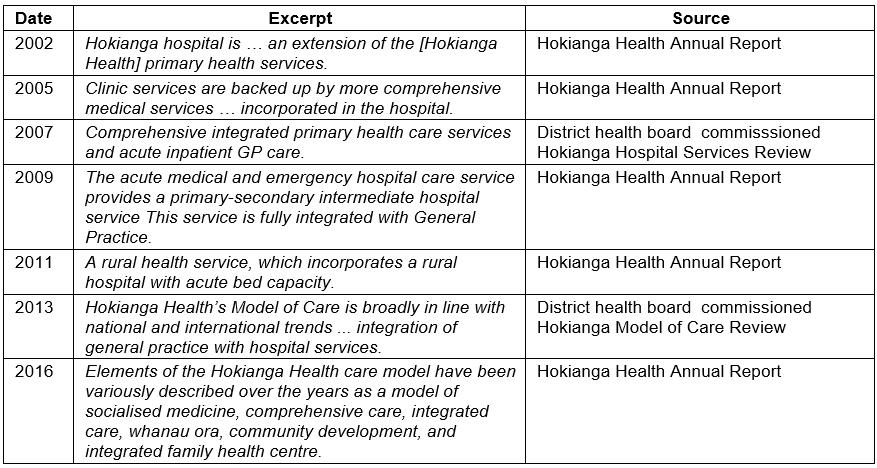
Interviews
Eleven interviews were conducted; no one declined to participate. Eight participants were medical practitioners and three were non-medical professionals. The non-medical participants (all at Hokianga Health for over a decade) were one senior manager, one senior nurse and one Māori cultural advisor. Medical participant characteristics are presented in Table 2. Two medical participants were retired at the time of the interviews but had continued to work at Hokianga Health until 2015.
All participants were designated a number (1–11) and were referred to throughout the study by this coding (eg P5).
Four main themes were identified. Illustrative participant quotes are presented.
Table 2: Key characteristics of medical participants (n=8) 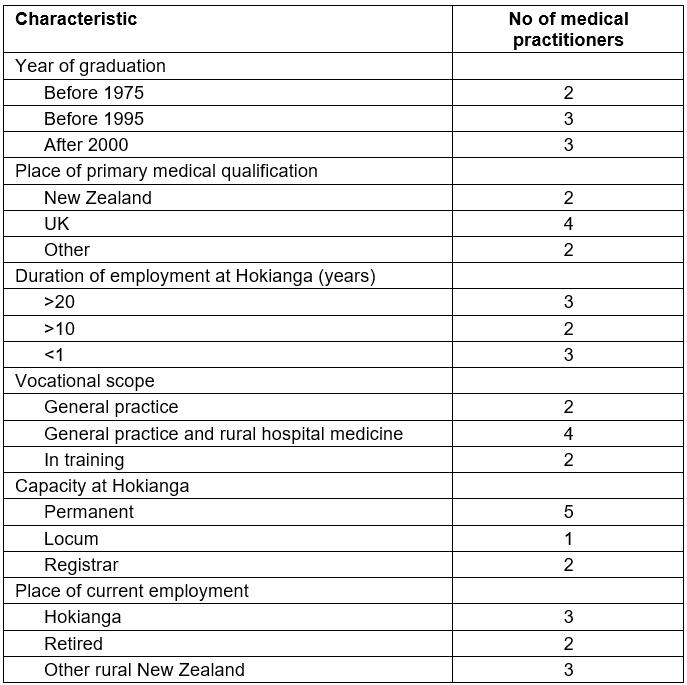
1. ‘What I do’, articulating the scope of medical practice at Hokianga Health: Participants’ accounts of the scope of medical practice at Hokianga Health fell into two subthemes: the clinical aspects of the day-to-day work and perspectives on the ‘right training’ for this work.
Clinical aspects Participants discussed their clinical work at Hokianga Health in relation to recognised scopes. The long-serving doctors had always aligned with general practice and had previously had no reason to explicitly define their scope of practice; it was simply ‘what we do’ (P2). Now they tended to see RHM as part of their-long established Hokianga or rural general practice scope, which had now been named:
… it’s helped us as clinicians think that through … and clarify that there is an extended scope, whereas before – this is what was expected of GPs – whereas I think now, no-one would think that, and people come into it knowing that this is a rural hospital doctor plus GP. (P11)
Younger doctors had come into their training with the two scopes and training pathways clearly differentiated. They identified as rural doctors or rural generalists but not rural GPs. RHM brought a specific focus to inpatient aspects of clinical work. Participants described their hospital work as varied and complex with a different daily rhythm, skill set and case mix from their general practice. Participants described how the scopes came together at Hokianga Health:
Here it is very integrated, we look after everyone no matter what they come with really and yeah … I did 6 months rural hospital and 6 months rural GP [training] here but I did them all mixed up together and that worked really well … you just see everyone and don’t think about the separation which is quite nice. (P1)
Some doctors challenged what they saw as the ‘GP approach’ for hospital care:
I wonder if everyone understands the whole scope. … some are more general practice oriented and probably less … inpatient focused, some may have got a bit out of date with some of the inpatient management, with the technical side. (P7)
Some participants perceived as a loss a tendency to separation of the workload, with individual doctors having more focus on either general practice or RHM.
The right training Participants discussed the importance of appropriate training and skills for a doctor in the rural context:
Rural disadvantage can lie in distance to secondary and tertiary care so that well educated rural hospital generalists have a critical role in minimising inequity of care and opportunity. (P9)
Participants saw combined general practice and RHM training as the best fit for Hokianga Health. Younger doctors in particular were confident that ‘dual training’ was fit for rural purpose nationally:
Now there is a pathway that you can work out yourself to acquire the skills that you need for something like the work [here] … and you do need the formal training to be able to do [the inpatient care] confidently and efficiently. That’s the benefit of the rural hospital training. I think the dual training is beneficial. (P6)
In discussing rural training, participants commented on the importance of exposure to high clinical workloads for trainees planning to practise rurally:
Essential to those wanting to work in a place like this – exposure to lots of cases before going rural – ideal would be a small base hospital for a few years – several years more than what some docs are getting prior to going into GP, need to have seen lots of patients across acuities and with responsibility – not just watching … they’ve got to spend more time in the places where the action is. (P8)
2. ‘What we do’, the importance of the Hospital at Hokianga: Participants discussed the importance of the hospital’s role in the wider context of health care: geographical isolation, limited resources, cultural aspects and socioeconomic deprivation:
… you have to have that ability to treat people for 24–48 hours when you’re this far away, because it just makes so little sense to send many people away. (P11)
Participants argued the importance of access, the need for appropriate resources, including workforce and equipment, to offer quality hospital care for people in ‘their own place’:
… not the really sick people that you transfer off, but the ones that stay in the hospital which is probably in the outside world, the part that’s least understood. … in terms of having a service that’s high quality, that’s in Hokianga, people can stay in their own place for things that don’t need to go out. (P2)
Participants discussed the role of RHM training in equipping doctors to manage emergencies and transfers:
… when to transfer and what mode you will transfer, and all that is, part of the RHM training, pretty important. I mean, this hospital can’t exist without [base hospital and tertiary] services, but the clinicians here need to be aware what those services are, and when we need to access them. (P7)
Participants also emphasised the hospital’s wider scope beyond acute emergency care:
The understanding of context, yeah and the ability to be flexible and to cope with that set of context. The medical intervention is quite a small part of treatment, isn’t it, often? It’s about being able to observe, have a place of safety, and have a place of recovery as well. (P11)
3. ‘On the fringes’: Participants reported a sense of vulnerability (both as individuals and as an organisation), a sense of not completely belonging to recognised scopes of practice. With the integrated model and the clinical work straddling two scopes, participants felt there was a tendency for misunderstandings, misperceptions and external scrutiny of practice:
They look at the Hokianga and it feels to them like it’s the wild west and it’s kind of, ‘there be dragons’ … Because we step outside the standard model it’s then – people look at it and think, well are there gaps in that then – are they not doing the right thing? (P11)
For the health service and individual practitioners, working in an integrated way on the ground meant meeting multiple central regulatory requirements. Participants reported frustration and at times resignation:
Because that’s a bit of a norm for us … as an integrated provider, we have to double up everywhere – triple, quadruple up in so many areas … Nothing gets designed around our model. Everything gets designed in discrete lumps of what we do and yet we have to comply with everything. (P5)
Lack of clarity in nomenclature (eg defining the health service as primary or secondary care, ‘GP-beds’ or a rural hospital) was mentioned by all participants as contributing to misunderstandings:
I’ve rattled on in the past about GP hospitals, and primary care hospitals, and people say, well you can’t call it a primary care hospital because by definition it’s secondary care. Yeah, okay let’s never mind the semantics. (P4)
Having gained a sense of belonging with the wider national connections made through the introduction of the RHM scope, Hokianga Health, at the small end of the rural hospital spectrum, faced the reality of keeping up with ‘dual scopes–dual systems’ (RHM practitioner and GP; rural hospital and general practice) regulatory processes for their practitioners and their service as a whole. Participants worried that if the larger rural hospital model (rural hospitals serving larger populations tended to have a RHM-only workforce) came to dominate direction and process within the RNZCGP, they might not be able to ‘keep up’, to meet all the requirements:
You need to encompass that [bigger rural hospital with a CT scanner], but you also need to encompass the one doctor and two nurses at night … in Hokianga – with you and a stethoscope and an ultrasound machine. (P11),
and they worried about the potential consequences of this for their community:
… in which case, that would mean, that this kind of service in this kind of place would be fundamentally different from what it is, and in my opinion, would be to the massive detriment to the health care for people in some of the most vulnerable areas. The community very clearly want there to be a hospital service here, but they want it to be high standard, and want it to be well supported. (P11)
4. Survival: Participants discussed how the new RHM scope had influenced the sustainability of the hospital service. For participants involved in the 2007 and 2013 external reviews of the service, RHM providing targeted training and support was identified as having been essential to ensure clinical safety and consequently the hospital’s survival:
I could see a future where … when clinical safety, the skills of our medical workforce was going to become an issue … we’ve got to do a whole bunch of things, but one of them is a trained for purpose medical workforce … if it had been shown [in the external review] that our clinical services were not up to standard, that staff have not being trained for the purpose of the acute hospital, we couldn’t have defended that. It would have been the end of our hospital service. (P5)
Relevant diagnostics attained as part of benchmarking, such as point-of-care laboratory testing, were seen as crucial for clinical decision making:
You have to look at what this hospital is doing in the context, and then looking at, well does it have to do this? Yes it does. Does it have to do that? Well, yes it does. If it does have to do these things, is it actually able to do them safely? Are they supported? Have they got the kit? Have they got the expertise? That’s what that’s about. (P4)
Participants were committed to raising and maintaining standards but they were also aware of the costs of this benchmarking and the challenge of meeting these costs posed for a small community trust:
The challenges lie in being able to stay up to date, of being able to meet all the standards … in a timely way and for the Trust to be able to fund doctors in order for them to meet these standards. (P9)
Discussion
The study findings facilitate the understanding of the effect of the RHM scope of practice at a rural health service level.
Before the RHM scope’s development there was a mismatch between the scope of medicine practised at Hokianga Health and recognised scopes and training pathways: the hospital and emergency aspects of practice were outside the general practice scope. This created a vulnerability for individual practitioners and the health service. The RHM scope brought validation to inpatient and emergency care at Hokianga Health. Together RHM and general practice provided the right fit for practice across the integrated service. The defining of their hospital practice (as RHM) and their hospital (as a rural hospital) meant alignment for Hokianga Health with RHM regulatory policy, systems and processes. The consequent strengthening of clinical practice and improved scope of services ensured the clinical safety and thus the viability of the hospital service. Challenges resulting from the RHM scope at the individual practitioner level mirrored those at the health service level: practitioners and the service trying to fit regulatory systems and processes that had not been set up with their scope of practice or service model in mind.
The study findings highlight the critical role of well and appropriately trained medical practitioners in minimising inequity of care and opportunity for rural communities. The findings concur with the literature, that medical practice in a rural context differs from that in metropolitan areas3,4,14,42,43, and add to growing international consensus on the need for targeted rural postgraduate training and professional development pathways. The findings suggest that a rural workforce not trained for purpose can put clinical safety at risk. The Delhi Declaration calls for generalist health practitioners to be appropriately trained to meet the specific challenges faced in providing rural health services43.
The establishment of the RHM scope aligns with recent international developments in postgraduate rural medicine pathways44-46. The findings concur with the literature in emphasising that rural training pathways be flexible, facilitating movement within the broad scope and remaining responsive to clinical and structural requirements of the spectrum of rural practice46,47.
With requirements for postgraduate medical training programs to function within the context of national regulations, country-specific solutions have emerged. In Australia, the Australian College of Rural and Remote Medicine was established as a separate rural college providing training across the rural generalist spectrum47. The Royal Australian College of General Practitioners has developed rural specific options within its general practice training program48. In Canada and the USA, family medicine colleges have established rural streams or ‘rural training tracks’ (USA) and rural residency options within their family medicine training programs49,50
In NZ, the establishment of a separate scope of practice (RHM) is providing a solution at the secondary and advanced-skills-competency end of the rural generalist spectrum. The decision to position the Division of Rural Hospital Medicine within the RNZCGP has proved an important one – in this way the whole rural generalist spectrum sits within a single college25,26. With shared professional structures and systems this allows minimising of barriers and costs for those doctors training in (or working across) GP and RHM25. While there is continued discussion around developing targeted rural streams within the general practice training program, these are yet to be established.
The RHM scope represents just one change facing Hokianga Health within the wider regulatory environment. The study findings portray a rural health service adept at adapting to regulatory changes, in order to retain a service that delivers for its community. It is well known that the more remote the care of a health service, the more fragmented the related centrally based systems, processes and funding models on which the service is dependent51,52.This rural–urban mismatch creates not only frustrations but also vulnerability for individual practitioners and has the potential to threaten the sustainability of small rural health services such as Hokianga Health. Findings also caution against the poorly considered application of urban-centric definitions to the rural context as this may risk accentuating divisions that do not benefit rural communities.
By remaining cognisant of the potential effects of regulatory changes on the diverse range of rural health services and the practitioners working in them, professional colleges can help to ensure that rural communities are not further disadvantaged.
Strengths and limitations
This study used two data sets (document analysis and interviews) with converging lines of inquiry, and generated an in-depth and multi-faceted exploration of the issues. The study focused on a single rural health service with a particular model of care, geography and population, and participant numbers were small. This needs to be taken into account when transferring findings to other settings.
Further research
Comparative studies should be undertaken in other rural areas with different models of care and should consider community perspectives as stakeholders of interest. The national outcomes of the first decade of the RHM training program will further understanding of the influence of the RHM program on NZ wide rural practice and workforce.
Implications for policy and practice
To ensure that the implications of policies take the needs of rural communities and rural health services into account, thus mitigating against possible negative effects, national and global bodies are increasingly calling for rural-proofing of health policy43,53-56. The findings from this study support the notion that NZ implements a process of rural health impact assessment. As already identified, requirements for this would include that ‘rural’ has a seat at the policy-making table of national bodies (including the Ministry of Health, professional bodies and universities), and that comprehensive rural health-relevant national research data are available and fit for purpose47,53,57,58. Neither of these requirements is yet in place in NZ58-60.
Conclusion
This qualitative case study found that the introduction of the RHM scope enabled the strengthening of both clinical practice and wider quality systems and standards at Hokianga Health, thus meeting the scope’s intentions. The study also identified challenges resulting from the new scope’s introduction, both for individual practitioners and the health service as a whole. The RHM pathway provides a necessary partial solution for NZ rural medical practitioners maintaining a broad skill set. In order to meet a range of different practitioner and rural health service needs, continued flexibility is required in training programs. With the RHM scope situated within the RNZCGP, opportunities for progressing targeted postgraduate rural training across the whole rural generalist spectrum are well within reach in NZ. The study findings support the proposal that NZ should implement a process of rural health impact assessment. The study findings may be relevant to other rural health institutions and services both in NZ and internationally.
Acknowledgements
We acknowledge Professor Susan Dovey (formerly University of Otago) for her guidance and contribution to this study. We thank all the study participants for their assistance with this project and acknowledge the staff of Hokianga Health for their continual support.
References
You might also be interested in:
2012 - Rural older adults' mental health: status and challenges in care delivery
2009 - Incidence of needlestick injuries among Ugandan student nurses in a rural hospital