Introduction
Nepal is a landlocked country bordered by China to the north and India to the east, south and west. Geographically, it is divided into three regions: Mountain, Hill and Terai, each stretching from east to west across the country1,2. Nepal has a total population of 28.5 million, with an average growth rate of 1.35%3. Recently, Nepal was administratively divided into seven provinces with each province having rural municipalities (called Gaunpalika) and urban municipalities (called Nagarpalika)4,5. At present, Nepal has 263 municipalities, and 59% of its total population live in the urban areas4.
Health profile of Nepal
In recent years, Nepal has made a substantial improvement in the health outcomes of its citizens. There has been an improvement in life expectancy at birth, which increased to 70.77 years in 2017 compared with 50 years in 1981. Between 2000 and 2016, neonatal mortality fell from 39 to 21 deaths per 1000 live births, infant mortality rate declined from 64 to 32 deaths per 1000 live births and under-five mortality decreased from 91 to 39 deaths per 1000 live births. Likewise, the maternal mortality ratio decreased from 548 per 100 000 live births in 2000 to 239 in 2016 (Table 1)4. Despite these achievements, substantial inequities in health outcomes across different geographic regions and socioeconomic groups persist.
Table 1: Indicators of major health outcomes in Nepal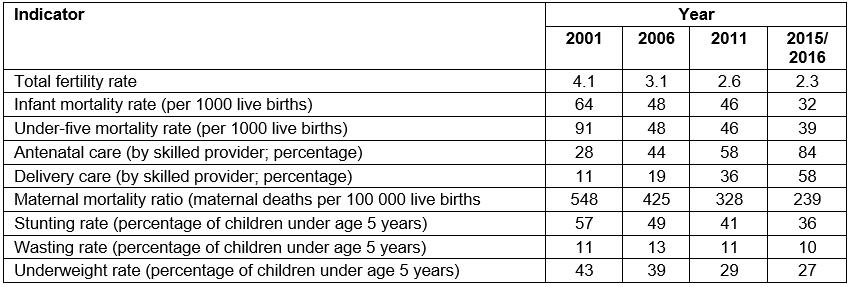
Health system structure
Under Nepal’s Ministry of Health and Population (MoHP), there are three departments: Department of Health Services (DoHS), Department of Drug Administration and Department of Ayurveda. DoHS is responsible for delivering preventive, promotive, diagnostic and curative health services all over the country. The healthcare service points are designed as health posts to the primary health care center (PHCC) to the district, zonal, sub-regional, regional and finally to central level hospitals. Female health care volunteers, primary health care outreach clinics and expanded program for immunization outreach clinics are other programs designed to provide healthcare services down to the grassroots community level (Table 2).
Table 2: Healthcare facilities under Department of Health Services6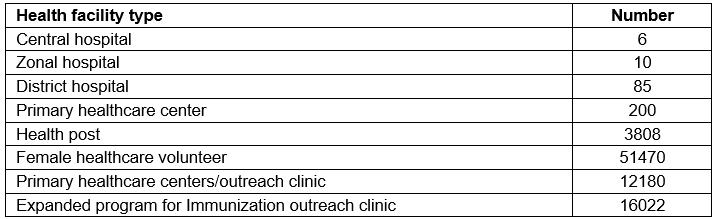
Human resources for health
According to the human resource for health (HRH) assessment conducted in 2013, there were 54 177 health workers in the country in total. Doctor-to-population ratio was 0.17 doctors per 1000 population, and health workers (including doctors, nurses and midwives)-to-population ratio was 0.67 per 1000 population7,8. The health workers-to-population ratio was significantly less than WHO’s recommended ratio of 2.3 doctors, nurses and midwives per 1000 population, which is calculated based on requirements for skilled attendance at birth and immunization9. Only 4% were doctors among the total health workers. Out of the total, 39% were working in the private sector7. Table 3 shows that 71% of the total sanctioned posts were filled in the public/government health facilities. PHCCs (78%) and health posts (72%) were more likely to have sanctioned positions filled than district (64%), zonal and higher level hospitals (69%).
Table 3: Percentages of government sanctioned posts filled, by background characteristics10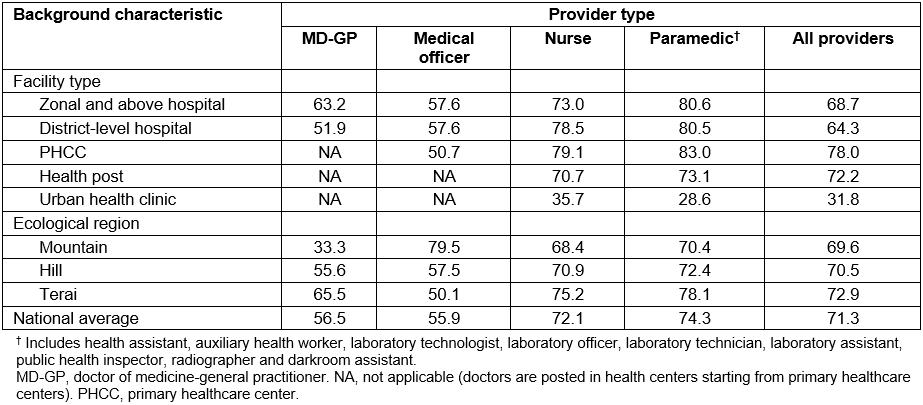
Policies and programs on human resources for health in Nepal
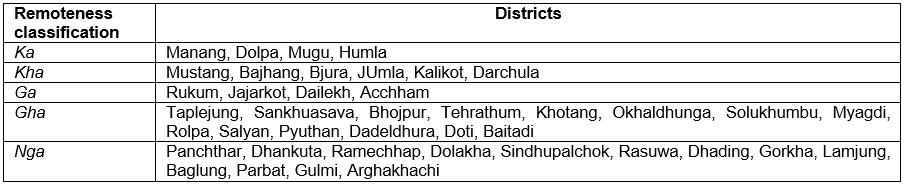
The government of Nepal promulgated the Health Service Act 1997 to manage human resources for health, which states that in order to be eligible for promotion health workers must have worked in a remote area for at least 2 years, and such health workers are prioritized in nomination for scholarship and training opportunities. The districts of Nepal are categorized into levels of remoteness (in the Devanagari alphabet they are named as ka, kha, ga, gha, nga, respectively, in the order of classification (Appendix I). For villages in remote districts, health workers also receive a remote allowance as a financial incentive for taking up a job in a remote area.
A comprehensive framework of policies, strategies and plans such as Nepal Health Policy 1991, Second Long Term Health Plan (1997–2017), Nepal Human Resource for Health Strategy (2003–2017) and Nepal Health Service Act was formulated to address the issues pertaining to human resources for health11-14. In 2010, MoHP established the country coordination and facilitation mechanism and developed the HRH Strategic Plan 2011–2015 to acknowledge the HRH-related problems15. Similarly, the Nepal Health Sector Strategy (NHSS) 2015–2020 and Nepal Health Sector Strategy Implementation Plan (NHSS-IP) 2016–2021 have also been issued16,17.
In a bid to improve access of the Nepali citizens coming from historically disadvantaged socioeconomic, gender, regional and ethnic groups to medical education/profession, and thereby also to diversify the HRH workforce of the country, reservation quotas have been put in place by the government. The reservation quotas thus allocated are 33% for women, 25% for economically or socially disadvantaged groups, 2% for individuals with a disability, 27% for indigenous groups (janajati), 9% for the relatively disadvantaged groups (dalit) and 4% for those from the remote areas18. These reservation quotas are implemented to ensure that eligible Nepali citizens from the said groups get the allocated percentage of total places at the medical schools in order to pursue medical or dental education. The remaining places are then allocated to all other Nepali citizens who do not meet any of those reservation criteria. The selections of successful candidates are made based on their academic merits and performance in medical entrance examinations.
In addition to setting up the reservation quotas for pursuing medical education, the government started a 2-year bonding service program in 2004, especially targeting the rural areas, as an additional effort to manage HRH workforce distribution in the country. Under the current provisions, private medical schools owned by a Nepali citizen must reserve 10% of seats whereas medical schools in Nepal owned by non-citizens must reserve 20% of seats of each session for the free education of students19,20. The expenses of educating the students selected for scholarships from the Ministry of Education are a part of the medical schools’ general operating budgets. In return for scholarships (such as free medical or dental education), medical/dental doctors have to serve in the assigned rural places for 2 years following their graduation. The Ministry of Education provides the graduation certificate and DoHS under MoHP assigns the place for such rural postings. The certificate is not issued by Nepal Medical Council unless the 2 years bonding service program is completed13,18.
Issues surrounding Nepalese human resources for health
Inadequate numbers of qualified skilled HRH workforce is one of the most critical constraints for achieving the Sustainable Development Goals for health and other health-related indicators. Inadequate numbers of skilled health workers in remote and rural regions is a serious and worldwide problem but it affects low- and middle-income countries such as Nepal even more severely21. According to WHO, the Sustainable Development Goals index threshold of 4.45 skilled health workers (physicians and nurses/midwives) per 1000 population is needed to meet health needs, which was previously 2.3 skilled health workers per 1000 population calculated based on requirements for skilled attendance at birth and immunization9,22. However, availability of health workers in Nepal is significantly lower than that threshold with 0.67 health workers (doctors, nurses and midwives) per 1000 population. Furthermore, only 0.17 doctors are available per 1000 population. Doctors in Nepal are unevenly distributed with 60% of doctors living in urban areas, resulting in critical shortages in rural and remote areas of the country7,20.
The unequal distribution of doctors in the rural parts of Nepal has been a challenging and longstanding problem for the government. Therefore, the government has been prioritizing the deployment of doctors as well as all other health workers in remote and rural parts simultaneously through the National Health Sector Strategies I (2004–2010), II (2010–2015) and III (2015–2020)7,12,15-17. Consequently, the number of doctors has been successively improving, from 12 194 registered doctors in 2010 to 20 192 in 2018, but there is still a shortage of doctors and specialists in rural areas7,23,24. One of the major problems for Nepal is the ‘brain drain’ of qualified medical doctors, with more than 500 doctors emigrating each year, making it difficult for the country to maintain that growth8.
A variety of interventions have been applied to different categories of the HRH workforce to address the geographical imbalance in their distribution in Nepal, such as financial incentives, better opportunity for postgraduate studies and a bonding service program7,16,25,26. One of the main interventional steps taken by the Nepal government to address the shortage of doctors and to improve the services provided by the public health centers in remote parts of Nepal is the 2-year rural bonding service program, aimed at doctors who have completed their undergraduate medical degree with a government scholarship15. Further, a 5-year bonding service program has been started for those doctors who have completed their medical/dental specialist degree with a government scholarship27.
The areas to which doctors are sent are generally rural, underdeveloped and deficient in infrastructure, professional development opportunities and personal/family amenities. These are settings that do not attract doctors under the current circumstances23,28,29. Lack of well-equipped health centers, weak support supervision and guidance to enhance skills and limited opportunities for career development prevent recent graduates doctors from taking up rural positions, and those who do face many problems due to insufficient equipment, personal and professional development options and geographical constraints23,28,29.
Studying the bonding service program
The government is using the bonding service program as a way to deploy doctors to prevent them from emigrating and to address the lack of doctors in many geographically challenging rural areas, but the challenges, outcomes and impacts of this exposure on the deployed doctors has hardly been researched8. Therefore, understanding the experience and perception of the doctors who have been deployed in rural parts is a notable issue that the government needs to address since they are the lynchpin of the program. The effects of the program are dependent on the deployed doctors’ attitude, performance and his/her reaction towards the program. Further, if the problems in the rural service are not addressed, the doctors who are forced to work in the rural areas for some period might end up migrating to urban areas, or to foreign countries out of frustration in the longer run, which further adds to the loss in the numbers of qualified health workers.
Effective human resource management strategies, plans and policies are needed for appropriate distribution and deployment of HRH workforce to ensure community access to health services and better health outcomes. Therefore, continuous periodic assessments and revision of health policies and interventions are required to maintain relevance to the changing context and to acknowledge the new challenges21. It is very important for policymakers to have an understanding and knowledge of the effectiveness and impact of a policy intervention.
It is therefore essential to closely examine the challenges, outcomes and impacts surrounding BSP to analyze the current situation and discuss the program in the light of experiences of those who are directly influenced by the program. Since no contextual and evidence-based study has been conducted yet on the bonding service program in Nepal following its implementation, and the government is preparing to implement a 5-year bonding service program for doctors after the completion of post-graduation, the findings of this study could provide some insights to the policymakers into the experiences of the deployed doctors, and take their needs and expectations into account for a successful implementation of the program.
Objectives
The current study had the following objectives:
- Explore the overall experience of recent medical graduates deployed in Nepal’s rural areas under the bonding service program.
- Assess the medical graduates’ perception of the bonding service program under which they were deployed.
- Understand the challenges faced by the medical graduates working under the bonding service program and identify ways to address those challenges.
Methods
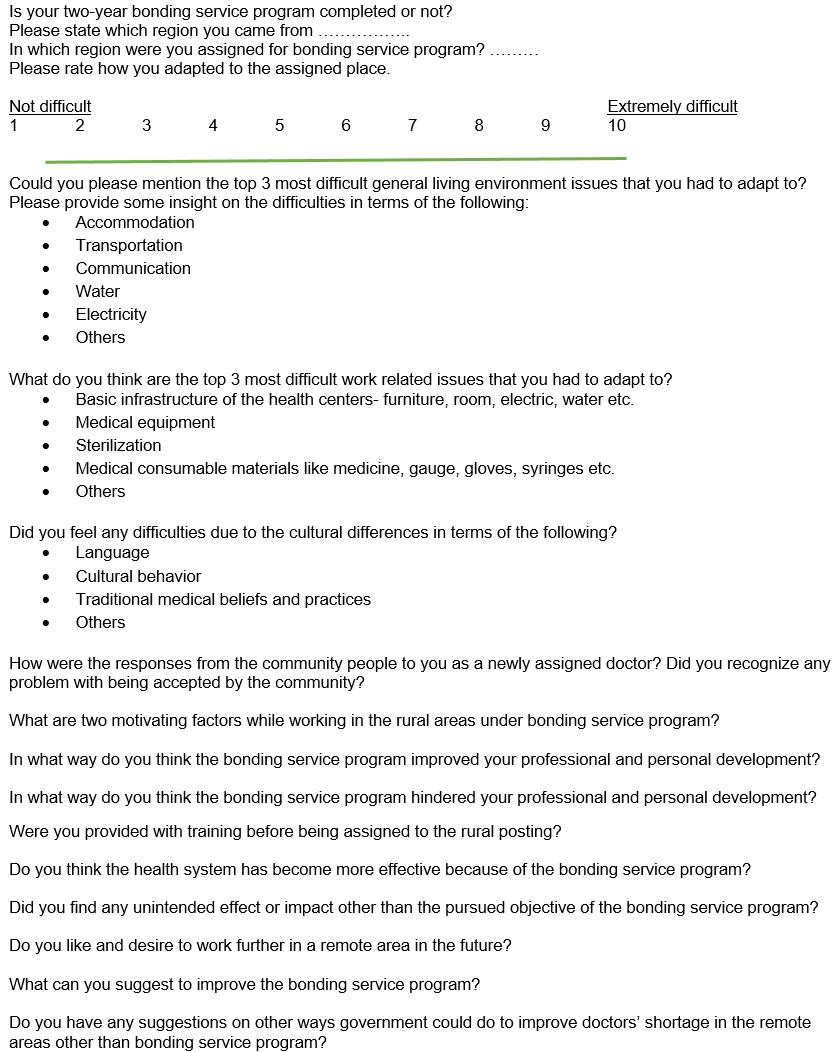
For this exploratory qualitative research, a semi-structured questionnaire (Appendix II) was prepared and circulated using the online survey platform Survey Monkey between June and July 2018. The survey link was circulated in the professional networks of the first author (BT) using his Facebook timeline as well as two Facebook groups of Nepali medical doctors and Nepali dentists. Four posts each were made about the survey to the Facebook group Doctors Society of Nepal and Dentists of Nepal. These two groups are among the biggest Facebook groups of Nepali medical doctors and dentists. Likewise, two posts were made from the Facebook timeline of the first author (BT). That Facebook post was further shared by four Facebook friends of the author to their own timelines.
The survey information sheet as well as the social media post clearly explained the purpose of the survey, its target population and the voluntary nature of participation. The survey was conducted among the doctors who had completed their medical/dental education (MBBS or BDS) with a Nepal Government Scholarship Program and were obligated to work in the bonding service program for 2 years. Doctors who studied in private funding were excluded because they are not obligated to take part in the bonding service program following graduation.
The survey link was placed online on 30 June 2018 and the last survey entry was received on 17 July 2018. Thereafter, the collected data was downloaded from the online survey platform and transferred to a Word document where the responses were categorized under the pre-established analysis domains. Even though the responses were quantitatively analysed to some extent, more focus was given to qualitative synthesis, documenting the experience of the respondents rather than numbers. It was done both because of a small sample size as well as the overall purpose of the study.
The language used in the survey form was English and the responses were also received in English. The medical education in Nepal is primarily taught using English textbooks, and all the exams are also conducted in English. Almost all of the formal written medical communications among Nepali medical and dental professionals take place in English. Therefore, language was not considered to be an issue among the medical graduates who had completed their medical education in English.
Ethics approval
Ethics approval for this study was obtained from the Research Ethics Committee of the Royal Tropical Institute, Amsterdam, The Netherlands. Participation in the survey was entirely voluntary and the potential respondents were informed that they were free to leave the survey at any time if they wished to do so. Respondents accessed the survey link through social media and anonymously completed the survey. Anonymity was maintained throughout the survey process – the researcher knew only how many people accessed the link and how many completed the survey and had no access to the name or social media handle/username of the person who accessed the link.
Results
Between 30 June 2018 (when the survey went online) and 17 July 2018 (when the last entry was received), 69 unique entries were received, all of which were completed entries. Even though the survey was kept open, no further entry was received after 17 July 2018 despite several reminding social media posts made by the primary author for participation. Out of the 69 doctors who completed the survey, 72% had already completed their 2-year bonding service program while 28% were still working under their agreement.
As mentioned, the findings have been categorized into pre-established domains for an organized and systematic presentation of the study findings.
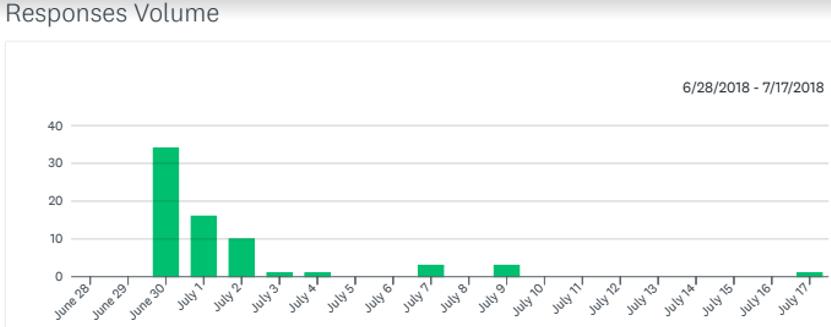 Figure 1: Volume and trend of completed survey entries from the day the survey went online
Figure 1: Volume and trend of completed survey entries from the day the survey went online
Domain 1: Preparation for rural service and realities of assigned locations
Respondents exclaimed that they were not provided any training prior to being assigned to the rural areas through the bonding service program. When a doctor is assigned to a PHCC, he or she is supposed to manage the administrative issues of the institution along with treating the patients. Government-employed permanent doctors are provided training, before being deployed to the workplace, on administrative issues and working conditions in the rural place. However, no such training was found to have been provided to the temporary doctors deployed under the program.
In addition to the training on handling of administrative duties, the respondents were also asked about orientation to the local conditions of the place to which they were deployed as a part of preparation for the rural service. Ninety five percent of the respondents were assigned to locations other than their own home districts, which meant they were not familiar with the local conditions. Furthermore, no orientation was provided to help them prepare for the living conditions and other practical realities of working in these rural areas.
Subsequently, once they were deployed, 53% of the respondents reported that they had found it very difficult adjusting to the appointed place because of the general living environment pertaining to housing, food, transportation, communication, electricity and water. Housing was ranked highest with regards to the adaptation problem by 80% of respondents, followed by food, transportation, communication, electricity and access to clean water.
In addition to the personal challenges faced due to lack of basic amenities in the rural locations, the respondents realized that poor infrastructure and inadequate to absent medical equipment created further professional challenges.
The major problems mentioned about work-related issues were the lack of infrastructure and consumables such as medicines, local anesthesia, injections, and gloves, which were supplied very late, contributing to their shortage most of the time. Likewise, dental surgeons were posted in hospitals but there were very limited instruments they needed to provide service. Most medical/dental equipment was lacking.
Proper sterilization was not available in many health centers and, because of that, the young doctors argued that they had to work in a risky environment. Along with the inadequacy or absence of medical equipment and consumable medical goods, problems related to basic infrastructure of the health centers were also mentioned by the doctors. For example, the number of rooms for service provision were not enough and doctors had to work in congested working areas with no space whatsoever for protecting patient privacy.
Difficulties related to administrative working environment were also mentioned. In some health centers, the junior doctors felt that other permanent government health workers including senior doctors treated them poorly. This kind of treatment and lack of cooperation towards the young doctors who had just set foot into the medical profession had reportedly affected their working environment adversely.
About one-third of the respondents (32%) argued that the mere presence of doctors without proper infrastructure and essential facilities would not achieve the purpose of bonding service.
One respondent summed up their perception of the realities in the assigned locations:
Politicians only wanted to show to their electorates that they are concerned about the health of the people. Therefore, this program was started, but without enough preparation. As a result, the infrastructure is not up to the mark in the majority of the health centers. This bonding service program must not just be implemented to serve the vested political interests of politicians but to actually benefit the rural Nepali people.
Adapting to the culture
Nepal is a multicultural and multilingual country with a lot of traditional beliefs and practices continuing to persist in the rural areas where these young medical graduates are deployed. About one in three respondents (34%) found it difficult adapting to the local culture and about a quarter (26%) of the respondents noted some difficulty understanding the language. Conversely, almost 31% of the respondents reported that they did not feel any difficulty regarding cultural practices, traditional beliefs and/or languages.
On the other hand, gender-related issues such as female doctors being treated with low respect by the staff members, and patients preferring male doctors to female doctors for treatment regardless of the levels of expertise, were reported by eight doctors.
Slightly less than 1 in 10 doctors (9%) reported having faced difficulties continually during their 2-year posting. Some of the reasons reported behind such difficulties were discrimination by the community based on the doctor’s ethnicity, and lack of security. If complications arose in some cases, doctors were blamed for the complications by the patient’s relatives, which posed security risks to the doctors. As a result of such threats and lack of security, some doctors reported feeling vulnerable in their working areas.
Response from the community
In terms of response from the community to the newly- assigned doctors, 48% of respondents felt that the local communities were kind and welcoming right from the beginning of their posting and the doctors did not feel any kind of difficulty related to the community in their work.
A total of 44% of the respondents initially felt that there were problems of recognition and the response from the community was not very positive but, with time, the response became excellent. The respondents felt that local people initially believed the newly assigned doctors were mere learners with poor knowledge and skills on treatment. As a result, the local people doubted the treatment of the new doctors:
People were a bit skeptical towards a new doctor in the beginning. However, after continuous interactions, counseling and treatment, they were found to be comfortable with the doctor, and satisfied with the service.
However, this experience was not shared by all young doctors and it varied with the locations they were posted to. For example, many communities in the semi-urban areas preferred experienced doctors and expected medical treatments that were on par with the service quality of specialized tertiary centers. Continual unfavorable treatment by the community throughout their service period was reported by about 1 in 10 doctors (9%):
People doubt young and newly appointed doctors. There have been several instances when patients came and asked who the senior-most doctor in the center was, and when they saw a young doctor, they showed hesitation in consulting the doctor.
Motivating factors in rural service
One of the primary motivating factors stated by most doctors while working in the rural areas under the bonding service program was they felt they were really serving the needy and underserved people, who were deprived of modern medical facilities, services and had poor levels of awareness.
One of the respondents exclaimed:
I realized that I had the ability to treat the patients suffering from health problems who were otherwise not able to seek solutions to their woes. It motivated me to be aware of the most needy people, about their life conditions, and make them disease free. This power to help them survive and bring smile on their faces after they got their treatment after 1 or 2 days of journey to the health centre completely on foot gave me a feeling of satisfaction and happiness.
About 43% of the respondents (29/67) reported that the rural exposure gave them an opportunity to experience the real Nepal. They also reported feeling they had done some service to the nation with this rural placement. Other motivating factors were that they got extensive exposure to several disease conditions. Likewise, they also reported having received love and respect/recognition from the community people, which further enriched their motivation. Some additional motivation factors were rural allowances, opportunities for training and preparation time for the postgraduate exam.
Personal and professional benefits, and drawbacks
The respondent doctors said they had experienced both benefits and drawbacks of the bonding service program in their personal and professional lives. On perception regarding personal and professional development, doctors found that the bonding service program had provided them an opportunity to get the first-hand experience of living in rural areas of Nepal, which are very different from cities where most of these doctors grew up and pursued their education. Some doctors found that BSP had enhanced their communication skills, broadened their exposure and knowledge, taught them to work under the conditions of limited resources, and helped them understand the government health system of Nepal. It had also reportedly helped them become capable in handling various critical circumstances that were encountered during the service, where they were sometimes all on their own.
Despite some personal and professional benefits, 80% of the doctors expressed that the bonding service program had hindered them from joining the postgraduate studies for 2 years. Some places where they were deployed offered exposure to only a few specific diseases and they had to work with very limited resources, infrastructure and equipment in most places. These aspects of working had resulted in less exposure to different disease scenarios along with less exposure to advanced equipment and procedures. Similarly, 20% of the respondents reported that they were deprived of continual medical/dental education, which they felt inhibited their continuous professional development. Likewise, most doctors posted to primary healthcare centers mentioned not having had any opportunity of guidance from senior doctors. As a result, they felt stuck with the knowledge they already possessed, with no room to emulate their seniors and grow technically and professionally. On the contrary, the doctors posted in district or zonal hospitals did not report having faced such problems.
Perceptions of program usefulness to health system and serving doctors
Mixed responses were received concerning the perception of usefulness of the bonding service program for the health system as well as the serving doctors. Thirty four percent of respondents felt that the health system had not improved even with the implementation of the bonding service. They felt it had instead ruined their practice because of the lack of proper equipment and proper guidance.
One respondent commented:
I do not think BSP [bonding service program] has helped the system get any better than it was before. Thanks to the lack of instruments, we cannot even offer 10% of our total services. To make the situation better, infrastructure and minimum equipment must be made available in the health care centers.
The remaining 66% of the respondents believed that the health system had improved due to the bonding service program even though they have had to face many challenges. Although most of the respondents were not satisfied with their situation under the bonding service program, they expressed that at least the doctors’ presence had been made possible in rural areas where doctors would otherwise hardly want to go. They felt that, despite the shortages of equipment and medical facilities, many rural communities were getting better treatment in their local health centers and were referred with better diagnosis to higher levels if the local centers could not offer appropriate treatment locally.
Willingness to work in rural areas in future
Despite the disappointing experiences of the bonding service program, 70% of the respondents commented that they would like to work in rural areas in future but with improved working conditions. The remaining 30% of the respondents said that they would never want to work again in rural areas in future.
Discussion
The bonding service program for recruiting doctors in the remote and rural parts of Nepal started in 2004 but the program has never been studied in relation to its effectiveness. Therefore there is a paucity of information on how well the program has been implemented in Nepal. The government presumes that scholarships have helped the graduates attain medical/dental education free of cost, and thus the graduate doctors who have completed their education under the government scholarship are indebted to the country. The deployment of those graduates under the bonding service program, according to the government, is a way of paying back some of that debt through service in mostly rural areas. However, there is almost no evidence available on how the graduate doctors themselves deployed in that manner perceive the program. As major program stakeholders, the young graduate doctors’ perception of the program is important to gain understanding on how this program is being run, to identify the strengths and weaknesses of its implementation and to make the required adjustments. This study aimed to fulfil that purpose of gaining understanding of the young graduate doctors’ perception of the bonding service program.
The study found that the majority of doctors deployed under BSP were dissatisfied with the program because of poor infrastructure, lack of proper accommodation, poor transportation system, and lack of basic facilities such as electricity and water in the rural areas where they were deployed. Gender issues such as discriminating cultural practices between male and female doctors were also reported by some young doctors.
Another constraint reported by the doctors working in rural areas was isolation, both personally and professionally. In professional terms, the doctors under the bonding service program are generally posted in the primary health centers. The senior doctors are essential for guiding new doctors, and also for managing some complicated procedures or cases. The absence of senior doctors or colleagues who can advise the young doctors and can provide mentorship was reported to be hampering their crucial period of learning. Likewise, the young doctors were posted to areas that were geographically, culturally, ethnically and linguistically very different from the places where these doctors grew up and received their medical education. On top of that, they were not provided any kind of professional or cultural training before being deployed to the rural locations, which meant they could not prepare themselves for the situations that were to come as a part of their daily working lives. As a result, this sometimes led to a shock and caused difficulties in personal and professional adjustment.
Challenges faced by the doctors
Literature shows that dissatisfaction is expressed by doctors to bonding service programs everywhere. The main reasons for dissatisfaction are lack of infrastructure, equipment and medicines followed by lack of proper accommodation, lack of transportation, lack of electricity and water30-35. Studies of compulsory service program in South Africa, show that 64% of doctors found themselves to have developed professionally in terms of gaining confidence during their service but they did not improve their clinical skills as there were no supervisors36. In Ecuador and Turkey, similar conditions were faced by the doctors after the implementation of the bonding service program33,37. In Kerala, India, dissatisfaction with the 3-year bonding service culminated into a strike as a result of which it was later reduced to 1 year30. A similar situation is brewing in the Nepalese medical fraternity against the 5-year bonding service program following the postgraduate medical/dental degree. Several studies concluded that there should be an additional support system and incentive mechanism in place along with the compulsory service program to support the doctors who are deployed under such bonding service schemes31,34,38-40.
Response from the community
Both positive and negative responses from the community were reported by doctors worldwide. In South Africa for example, the services from doctors were valued as a compulsory service program and it was found to have brought positive changes in community health status40. Similarly, in India, people in the communities were happy to see a doctor nearby, in the absence of whom they had to travel a long distance41,42. In Ecuador and South Africa, the community responses were not as enthusiastic as expected. Problems of not accepting the newly assigned doctors by the community for the treatment were observed because people in the communities thought that the new doctors are learners and perform experimental treatments on them. Similar problems were noted by the doctors in Nepal in the present study. However, in the long run, the problem was found to have been solved after interactions between doctors and communities40-42. Similar was the finding in the present study where most doctors reported that people in the communities started appreciating their work in the long run and in most cases their relationships with the community became much better.
Human rights and bonded service programs
In Thailand, controversy arose about whether it is ethically acceptable to force recently graduated young doctors to go to remote places, which could demoralize them35. There is also an ongoing discussion worldwide on the human rights of doctors to migrate wherever they wish to43. Although the government clearly states the provision of the obligatory service and also that they have the right to deploy the doctors after investing in their education, it still does not supersede the basic human rights of the doctors to migrate44.
Effectiveness of bonded service programs
Arguably, it can be said that the bonded service program has been successful in addressing the problem of unavailability of doctors at the primary healthcare levels in rural areas of Nepal. At the same time, the children of those Nepalis who are otherwise unable to pay the expensive medical tuition fees are getting an opportunity to become medical doctors and dentists. However, it is difficult to prove the program’s effectiveness and impact on population health. This is because the population health outcomes do not necessarily depend only on doctors’ availability but also on the availability and services of many other categories of health workers.
Absolute indicators were not methodically determined before and after the implementation of the bonded service program. Therefore, assessing the program effectiveness remains a technically difficult task. Similarly, it is difficult to judge the cause and effect relationship because out of the numerous factors that influence HRH, the bonded service program epitomizes only one factor. Different types of compulsory service programs have been practiced in different parts of the world. Nonetheless, in most cases, those compulsory service programs are not formally evaluated due to lack of funds, shortage of expertise to evaluate and a lack of mandate to do so. From what is understood, it is clear that although explicit information is not gathered, the compulsory service programs can be implemented and sustained over a long period, even without enthusiastic support.
Recommendations for improving the bonding service program
On the basis of this study, the authors make the following recommendations:
- Manage the workplaces with better provision of infrastructure and medical equipment followed by proper laboratory facility for diagnosis.
- Increase the number of allocated doctor seats for the government health centers and use permanent doctors to provide service rather than using temporary intervention mechanisms to solve the perennial problem of the health system.
- Increase salary structure for the doctors sent through the bonded service program because doctors working in the private sectors are paid far better than the doctors working in rural areas.
- Create career security for doctors so that the doctors won’t have to stay idle after the completion of bonding service program.
- Implement the plan of first posting doctors to semi-rural areas where they can receive guidance from the existing senior doctors. They could then gradually be posted to more rural areas after a certain period so that they do not get overwhelmed right from the beginning, culminating into a negative perception towards the whole program.
Limitations
This study was based on the perception of a limited number of doctors who voluntarily participated in an online survey. Likewise, the study was based on a short, self-administered questionnaire. As a result, the responses could not be explored to the same extent as for in-depth interviews. As there were no cross-questions, the depth in the responses might have been limited.
Conclusion
The bonded service program was believed to be an appropriate intervention strategy in 2004 by the Nepal government to address the uneven distribution of doctors between rural and urban areas. This program was envisaged under the pretext that there were few medical schools in the country, tuition fees of medical education were too high as a result of which only children of wealthy families could become medical doctors. Therefore, the government decided to offer medical education to the children of Nepali citizens from low- and middle-income families by providing scholarships. Despite the good intentions behind the program, some inherent programmatic and logistic problems exist in the program that need to be addressed for its effective implementation.
Some of the programmatic problems revealed in this study are:
- assigning doctors to locations that are not only very far away from home but are also very different culturally and linguistically
- undue political influence in posting doctors who are related to the politically powerful people in relatively easier locations
- systematic disparities in pay and/or other government facilities between permanent health workers and the temporary doctors deployed under the program
- poor health infrastructure and inadequate medical equipment in rural areas
- lack of mentors in health centers where these doctors are deployed
- lack of personal security in case something goes wrong unintentionally while providing a health service.
Similarly, there are some logistic problems such as provision of appropriate housing facilities, transportation, clean water, electricity and communication at the health facilities where the doctors are deployed.
In the current context of Nepal, deploying around 400 doctors in the rural areas every year seems to partly solve the problem of shortage of doctors in rural parts of the country. Nevertheless, there is a massive production of doctors, at the rate of 2000 doctors per year in the country. If the production of doctors increases at a similar rate and the government does not think of absorbing these doctors into the government health system as permanent staff members, it might give rise to a situation where on one hand there are more doctors than positions available in the government and private health sector combined and, on the other hand, the disappointed doctors are continuously deployed unevenly as temporary government health service providers in places that they do not like, with hampered chances of further education and no job security after the end of the bonding service program. Therefore, the government has to identify other possible interventions that are contextually relevant rather than continue using the services of the temporary doctors who are bound by the conditions of the bonded service program.
The success or failure of the bonded service program depends on how all of these influencing factors are addressed according to the changed context from the time when the program was first envisaged. It can also be said that a single approach to address HRH inadequacy carries the risk of being ineffective because, as also found by this study, multiple factors influence the doctors’ willingness to be involved in rural health service. Therefore, the bonded service program should aim to serve the purpose of convincing the doctors to not only work wherever they are required to for a bound period of time in the rural areas but instead to become the real champions of rural health service – even in future ,when they are not forced by any government rural service bonds. That depends on the willingness of the government to tackle the constraints that are making not only BSP but also the overall rural health service unattractive to a considerable proportion of young doctors.