Introduction
In Canada, ‘Indigenous peoples’ refers to the original peoples of present-day Canada and their descendants, including First Nations, Inuit and Métis. In the North West Local Health Integration Network’s region in Northwestern Ontario, Canada, a geographical area comparable to the size of France, there are 69 First Nations communities recognized by the government of Canada, 25 are accessible by fly-in only (Fig1)1. The rural and remote locations of many First Nations communities pose numerous challenges in accessing health care services. When services are accessed, many barriers remain, such as the complexity of navigating healthcare services, fragmented care, historical trauma and lack of culturally sensitive care2,3. First Nations people were very healthy prior to colonization4,5. While many First Nations individuals continue to lead healthy lifestyles, colonial policies and Westernization have negatively impacted the health of Indigenous people at a population level2,6. It is important to frame health barriers in this colonial context2.
Recent available evidence from the Ontario Cancer Registry suggests that between 1991 and 2010 colorectal and breast cancer incidence increased 6–7% and 25%, respectively, among First Nations in Ontario4. Cervical cancer incidence among First Nations women in Ontario has declined significantly over time4.
Available data show some encouraging trends in cancer screening. For example, First Nations women now have the same rates of cervical screening as non-First Nations women, and a similar proportion of off-reserve First Nations and non-First Nations individuals are overdue for colorectal screening7. However, disparities between First Nations and non-First Nations populations remain. Furthermore, some data were collected via self-reported surveys, thereby potentially introducing social desirability bias, which may result in over-reporting cancer screening histories8.
Currently, no data are available for colorectal screening for on-reserve First Nations people. Additionally, only 70% of eligible on-reserve First Nations women aged 50–74 years report having recently had a mammogram, whereas 82% of non-First Nations women and off-reserve First Nations women of the same age report a recent mammogram in Ontario7. It is critical to note that in Ontario these statistics include urban, rural and remote First Nations people instead of categorizing them by their geographical remoteness. This additional data could provide helpful insight, but ascertaining rural/remote-specific data may be difficult for a number of reasons, including challenges with using postal code data. Research from the Australian context demonstrated that Indigenous women in Australia have lower cervical screening rates than non-Indigenous women, which is different from the previously mentioned Ontario data suggesting that First Nations women now have the same rates of cervical screening as non-First Nations women in Ontario7,9. However, this study was able to categorize First Nations women by geographic remoteness, which would build interesting context if Ontario could produce this data.
Lower rates of cancer screening among First Nations people may also impact mortality and survival rates. First Nations people have higher mortality rates of colorectal, cervical and breast cancer than other people in Ontario4. Survival is best for females with breast cancer, but First Nations people still have poorer survival than other people in Ontario, despite improvements in survival from 2001 to 20104.
In addition to barriers such as geography, reasons for lower adherence to cancer screening for First Nations populations may include less knowledge about cancer screening, unfavorable attitudes and behaviors toward the healthcare system and a lack of integrated cancer screening recruitment in existing health care3,10. Integrating better cancer screening education into existing healthcare services to increase recruitment and participation in cancer screening among First Nations people may be a helpful solution to increase cancer screening participation as a whole3. Ontario has organized cancer screening programs for breast, cervical and colorectal cancers. In Northwestern Ontario a mobile coach travels throughout the region, providing all three screening modalities, therefore minimizing travel for many clients. However, it cannot reach all First Nations communities. While access to convenient screening is not the only relevant factor affecting screening rates, it is a factor that could be modified.
The Wequedong Lodge Cancer Screening Program (WLCSP) was a pilot program to provide access to cancer screening education, screening opportunities and increase uptake of cancer screening for First Nations people in Northwestern Ontario.
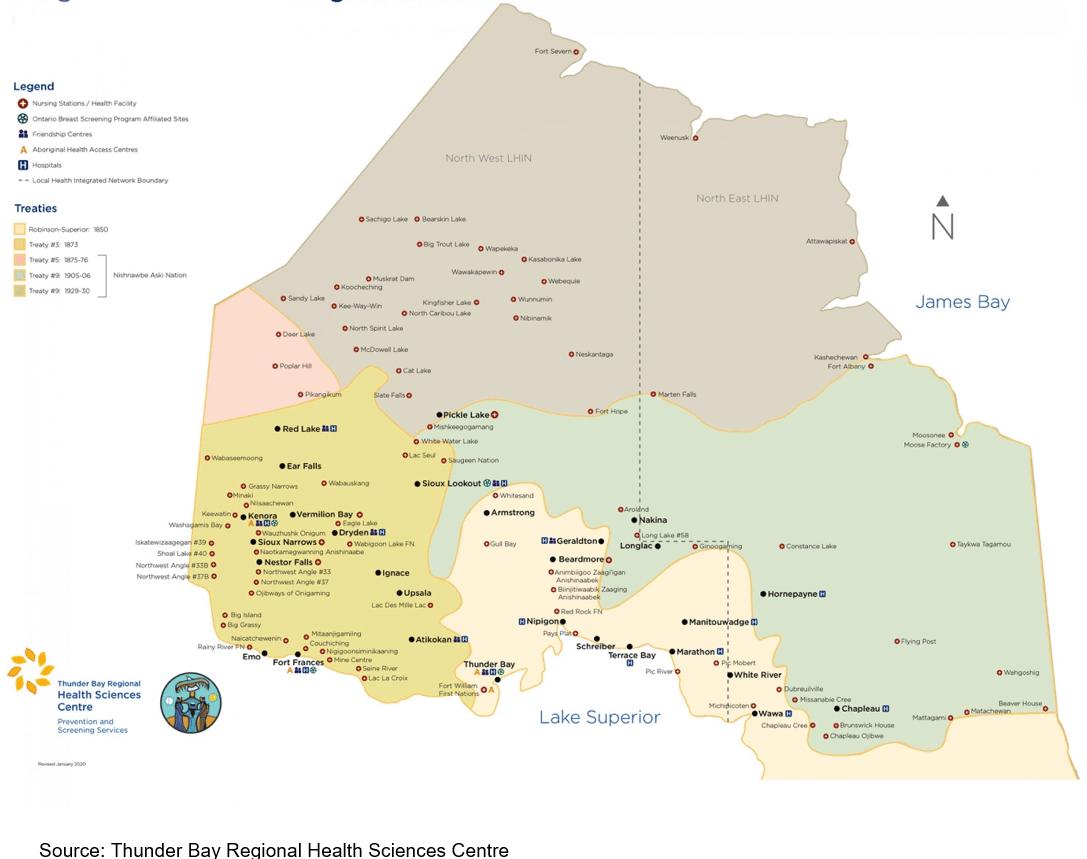 Figure 1: Map of First Nations communities in Ontario, Canada.
Figure 1: Map of First Nations communities in Ontario, Canada.
Methods
Program development
The WLCSP program was a partnership between Wequedong Lodge and Prevention and Screening Services at Thunder Bay Regional Health Sciences Centre (TBRHSC), Northwestern Ontario’s largest regional hospital, with support from the Nishnawbe Aski Nation Chiefs Assembly by way of resolution, and Cancer Care Ontario’s Indigenous Cancer Care Unit. Wequedong Lodge provides accommodations for approximately 9500 First Nations adults each year who require medical services in Thunder Bay, Ontario, Canada. The majority of the clients of Wequedong Lodge are First Nations people from rural and remote communities. Prevention and Screening Services coordinates health prevention/promotion efforts as well as cancer screening for Northwestern Ontario, and is based in TBRHSC. Nishnawbe Aski Nation is a political territorial organization representing 49 First Nation communities within Northern Ontario. In September 2013, planning the WLCSP pilot project began as a result of discussion with TBRHSC’s Indigenous Cancer Care Committee, whose representatives included Wequedong Lodge, the Regional Indigenous Cancer Lead (RICL), Prevention and Screening Services and First Nations communities and organizations. Wequedong Lodge representatives and the RICL at the time, an Indigenous family physician, discussed partnering to launch the pilot program. Community chiefs in Nishnawbe Aski Nation territory and physicians in the Sioux Lookout First Nation Health Authority, which provides health services to 33 First Nation communities in Northwestern Ontario, were notified about the program and provided with information about program logistics and patient follow-up strategies.
Cancer screening programs
The initial goal of the WLCSP was to educate eligible men and women about cancer screening and to connect women with breast screening appointments. Later, with additional funding allocation, all three organized cancer screening programs (breast, cervical, colorectal) were offered to eligible clients. In Ontario, women who are residents, have no current breast implants, have not had a mammogram in the past 11 months, and with no acute breast symptoms or personal history of breast cancer are eligible for a breast screening mammogram every 2 years at ages 50–74 years11. Women are also eligible for cervical screening every 3 years at ages 21–69 years if they have a cervix, but were ineligible for screening if they were pregnant due to limitations in the scope of practice of program nurses11. Women and men with no contraindications (ie are at average risk of colon cancer) are eligible for colorectal screening every 2 years at ages 50–74 years11.
In the early stages of the program (2013–2014), the RICL was the healthcare provider for WLCSP appointments. Later, a registered nurse filled this role, under a physician medical directive, and offered Pap tests and fecal occult blood test (FOBT) kits. A clinic room at Wequedong Lodge was renovated and used to conduct the private appointments. A project coordinator, an employee of TBRHSC, helped establish WLCSP logistics and provided administrative support.
An Indigenous program screening liaison was available at Wequedong Lodge as a dedicated on-site support for the program. The liaison was an existing Wequedong Lodge staff member. She spoke English, Ojibwe, Oji-Cree and Swampy Cree (all Nishnawbe Aski Nation territory languages) and assisted with recruiting individuals interested in screening, booking appointments, preparing charts, inputting data and issuing follow-up letters. Her primary role was to be an on-site staff who was able to provide culturally sensitive services in clients’ first languages, as well as assist with general administration of the program.
Client recruitment
Wequedong Lodge has a client database that captures information about clients coming to stay at the lodge for medical appointments in Thunder Bay, including health issues, medical appointments and travel arrangements. The liaison was able to view this regularly. She was able to discern which clients may have been eligible for screening, and contacted them by calling their rooms or speaking with them in common areas. Interested clients, regardless of their age eligibility for screening, were given the opportunity to book an appointment. Clients who did not meet cancer screening eligibility were provided education at their appointments. Recruitment occurred three days per week, typically overlapping with WLCSP days. Since <1% of Wequedong Lodge clients are Inuit and Métis, all clients were assumed to be First Nations for the project’s purposes.
Appointments
Appointments were scheduled for 20 minutes in length, but typically ran longer. They included a short client assessment and education about cancer screening. Initially, the program ran one afternoon weekly for 2.5 hours; later, this increased to 1.5 days per week.
Education
Initially, the RICL used colon and cervix models and pictures as educational tools. These proved ineffective and time consuming. Then, in collaboration with Prevention and Screening Services at TBRHSC, Wequedong Lodge, and Cancer Care Ontario, a First Nations specific education cancer screening toolkit was developed to help improve cancer screening education using a culturally sensitive resource. The toolkit is a colorful, mostly picture-based flipbook, incorporating methods such as storytelling and pictures, that care providers can use interactively with First Nations clients to discuss cancer screening. It provides education about cancer, cancer screening methods, signs and symptoms of cancer and how often cancer screening should occur (Appendix I).
Cancer screening pathways
Pathways for breast, cervical and colorectal cancer screening were developed to ensure that processes were in place for clients who may require follow-up as a result of their cancer screening appointments. Pathways were modified and adapted over time to reflect changes in WLCSP care delivery, for example when the program began to offer cervical and colorectal screening services. Figure 2 represents a simplified final pathway.
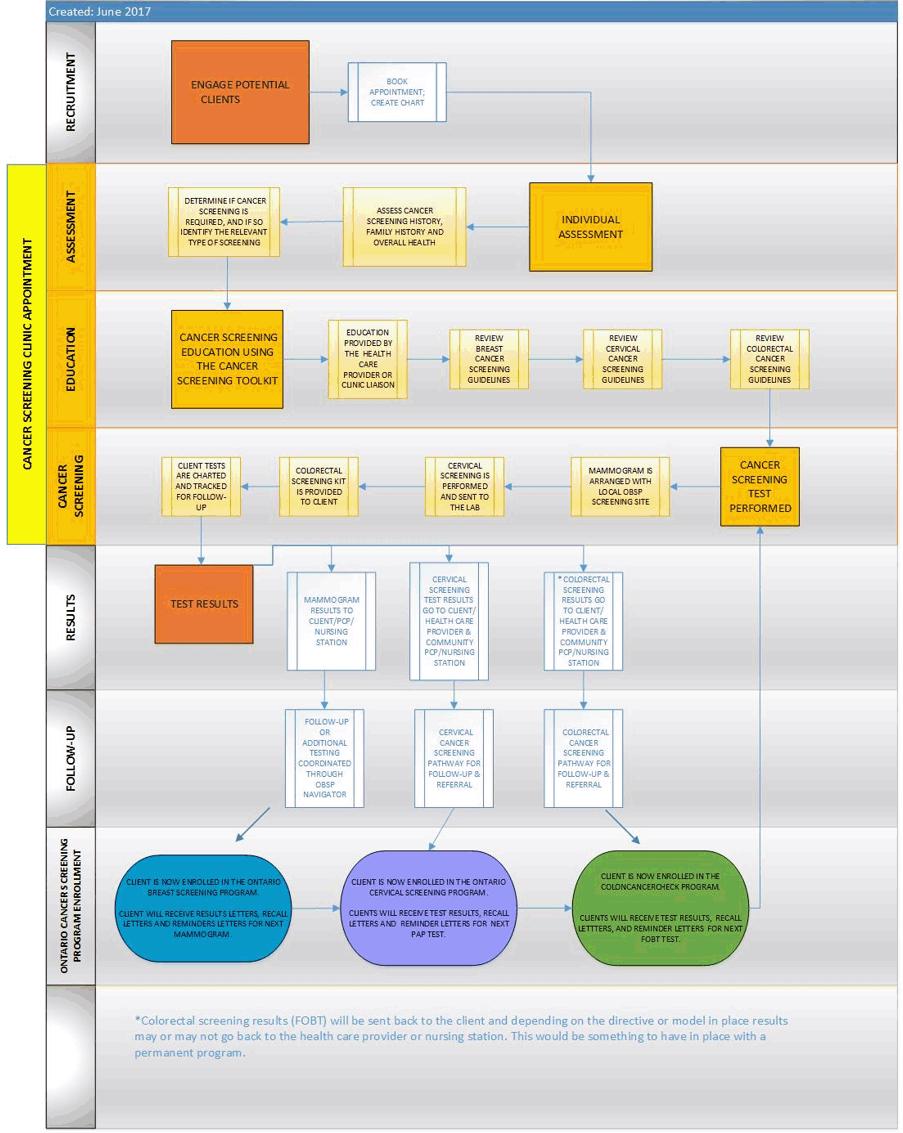 Figure 2: Overview of Wequedong Lodge Cancer Screening Program cancer screening pathway.
Figure 2: Overview of Wequedong Lodge Cancer Screening Program cancer screening pathway.
Evaluation survey
When the nurse model was implemented, a client evaluation survey was created to collect feedback about client experiences with the pilot program (Appendix II). The survey was distributed to attendees by the program nurse or liaison.
Program evolution
The program was conducted between October 2013 and November 2016 and underwent various adjustments due to its improvised nature, such as clinical appointments initially being conducted by a physician and then by a nurse. Initially (2013), appointments consisted only of education and breast screening bookings and occurred 1 day per week. Later, the program ran 1.5 days per week, and appointments included cervical screening and dispensing of colorectal screening kits (2015). Beginning in 2015, the nurse began collecting information on reasons for missed appointments and declined screening and the liaison began distributing the evaluation surveys. The program ended in 2016 due to a lack of sustainable funding. Appendix III provides a timeline for the WLCSP.
Data recording and analysis
Data were managed using Microsoft Excel. Screening uptake was presented as percentages and proportions and client attendance was discerned from client charts. Evaluation survey responses were input into SurveyMonkey. Nursing notes reported on an Excel spreadsheet provided client-reported information about why clients declined cancer screening; however, it was inconsistently reported.
Ethics approval
Requirement for ethics approval from Thunder Bay Regional Health Sciences Centre Research Ethics Board was formally waived on 5 September 2018, as this project aimed to evaluate a pilot initiative to improve existing cancer screening services, and was therefore considered a quality improvement initiative.
Results
Overall program uptake
Overall, of all the program bookings 81% of appointments were attended. There was a 96% increase in the bookings in the period between 2014 and 2015, and 84% between 2015 and 2016 (Table 1). Participation in the screening program increased 62% in the period between 2014 and 2015, and 68% between 2015 and 2016 (Table 1). More age-eligible females than males attended the program, accounting for approximately 81% (685/841) of attended appointments over 3 years, and 49% (410/841) of all clients were women aged less than 50 years (Table 2). Given that approximately 9500 adults stay at Wequedong Lodge each year, it is estimated that 2% (157/9500) of Wequedong Lodge clients attended the program in 2014, 3% (255/9500) in 2015 and 5% (429/9500) in 2016.
Table 1: Screening education program appointment summary 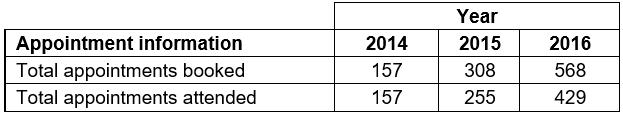
Table 2: Proportion of participants attending appointments, by year† (n=841)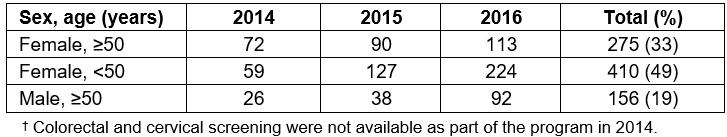
Breast screening
Over the duration of the program, 24% (66/275) of age-eligible female clients had a mammogram booked (Table 3). Of these booked women, 91% (60/66) completed an Ontario Breast Screening Program screening (53/60) or diagnostic (7/60) mammogram. One reason for not receiving a mammogram included self-reporting being up to date with screening. Other reasons for refusal were not recorded in client notes.
Cervical screening
Throughout the duration of the program when cervical screening was offered (2015–2016), 81% (554/684) of clients were within age guidelines for cervical screening. Of age-eligible women, 8% (45/554) completed a Pap test. Nursing notes recorded some reasons for Pap refusal, including self-reporting being up to date, ineligibility due to hysterectomy, ineligibility due to sexual inactivity, ineligibility due to pregnancy (outside nurse’s scope of practice) or did not have a provincial health card (required for cancer screening in Canada).
Table 3: Breast, cervical and colorectal screening summary†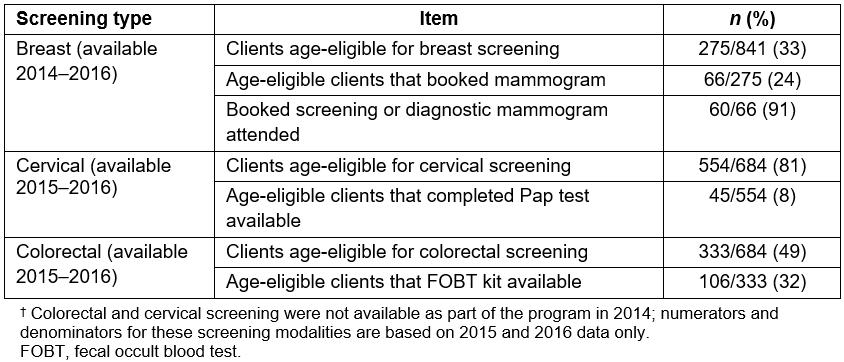
Colorectal screening
Out of the 333 age-eligible clients that attended appointments when colorectal screening was offered (2015–2016), 32% (106/333) were provided with an FOBT kit. Reasons for refusal for the remaining age-eligible clients, when reasons were recorded in nursing notes for refusal, included having had a colonoscopy (making them ineligible) or self-reporting being up to date with screening.
Client evaluations
A satisfaction survey was implemented in 2015 and was completed by 58% (396/684) of 2015 and 2016 program attendees. Similar to the attendance trends, 79% (312/396) of evaluation surveys were completed by females and 21% (84/396) by males (Table 4). When asked if the nurse/liaison explained information in a way that was easy to understand, 99% (393/396) answered ‘yes’. Most respondents, 97% (383/396), felt comfortable with the nurse/liaison. Additionally, 99% (391/396) of clients said they felt that they understood the cancer screening information that was explained at the appointment, and 98% (386/396) of clients felt that they were provided with enough information about cancer screening. Finally, 99% (392/396) of attendees were happy with their experience.
Table 4: Client evaluation results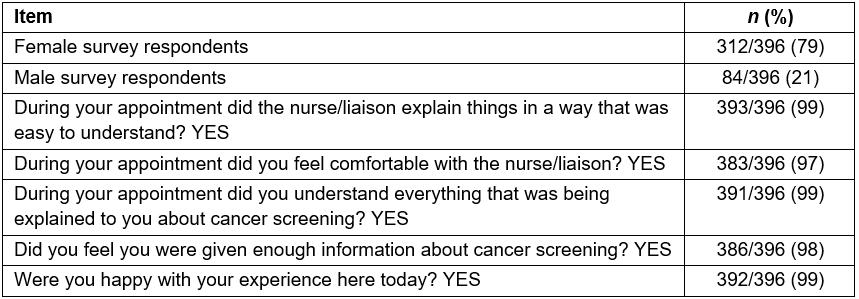
Process evaluation
Program changes posed some difficulties in assessing outcomes. In 2015, the program began utilizing a nurse rather than a physician, and began providing Pap tests and FOBT kit distribution. Additionally, reasons for declining screening were not recorded until 2015. Even then, reasons were not recorded in a standardized consistent manner in the nursing notes.
Discussion
This project report describes the design, implementation process and uptake of a cancer screening education and opportunistic cancer screening program for clients from rural and remote First Nations communities. Organized population-based screening programs are generally accepted as superior to opportunistic screening, the latter of which is generally defined as receiving screening at the advice of and from a primary care provider12-15. However, opportunistic programs present a possible avenue to screen under- or never-screened individuals, who may not otherwise attend an organized program, by integrating cancer screening into existing healthcare programs3. However, it is difficult to ascertain what might be considered acceptable screening rates for an opportunistic screening program such as the WLCSP.
Other opportunistic cancer screening programs targeting Indigenous populations have not occurred in the same context as the WLCSP. In the USA, some Indigenous-specific cancer screening programs established on reserves or managed by tribal councils have shown increases in cancer screening by directly addressing barriers experienced by Indigenous populations. However, unlike the WLCSP, these programs have been offered on their reserves, were federally funded and did not report on opportunistic cancer screening rates based on their programs16,17. One Alaskan study by Redwood et al had a more opportunistic approach in contacting first-degree family members of Indigenous colorectal cancer patients18. This project, similarly to the WLCSP, experienced data collection issues. The study also reports an increase in colorectal cancer screening, but it could not generate program screening rates because statistics were not recorded for the first 7 years of the program’s existence18. In Northwestern Ontario, there has been specific cervical cancer screening research with First Nations women; however, it is based on HPV self-sampling testing6. That research has shown that First Nations women may prefer this type of screening modality, but currently it is not offered as part of Ontario’s provincial cancer screening programs. Based on the research, screening rates from the WLCSP may serve as a useful baseline comparison for opportunistic cancer screening rates for other initiatives globally.
After the WLCSP, a collaborative research project was conducted to explore barriers to and facilitators of participation in cancer screening among First Nations people in Northwestern Ontario (p. 130)4. Some barriers identified included limited awareness of screening, lack of culturally relevant education resources, and multiple negative experiences with healthcare providers and the healthcare system including discrimination and poor communication, resulting in lack of trust4. While the FOBT kit for colorectal screening is a take-home test, breast and cervical screening are particularly intimate. This intimate nature was identified as intensifying these trust challenges4. The present study also found that considerable healthcare provider turnover in communities and fragmented care in the region created logistical challenges with screening tracking4.These findings are supported by similar findings from several research studies6,16-19.
The WLCSP can perhaps be seen as contributing to the mitigation of some of these barriers. The primary goals of the program were to provide cancer screening education and access to cancer screening using existing healthcare services, thereby contributing to increased cancer screening health literacy and access to cancer screening services. The cancer screening toolkit aimed to provide a culturally sensitive resource to increase cancer screening knowledge, specifically by using storytelling and pictures, which are a more engaging way of learning in Indigenous cultures20. The presence of Indigenous care providers is a well-supported factor in facilitating positive healthcare experiences for Indigenous patients15. The nurses delivering the program in 2015–2016, and to the extent of the authors’ knowledge, most medical radiation technologists completing mammograms were non-Indigenous. The program nurse, from the mobile cancer screening program, had training in serving Indigenous patients. However, having a First Nations liaison was essential to the success of this program because she addressed language and cultural barriers that can prevent First Nations people from being screened18,19. In addition to her cultural and language assets, she was a familiar face at Wequedong Lodge, which helped to build trust with the clients.
Furthermore, the program directly addressed structural barriers such as a shortage of appropriate healthcare providers, and geographic and transportation barriers19. All healthcare providers were trained in cancer screening, and the opportunistic nature of the program was that cancer screening was offered after geographic and transportation barriers had already been removed, since clients were already in Thunder Bay for other medical reasons.
The authors acknowledge several limitations of this project. While survey results seemed to indicate positive patient experiences in their appointments, comfort may not equate to the level of trust patients would like to feel when engaging in cancer screening. Studies show that Indigenous women require a trusting relationship to undergo a Pap test6,19,21,22. Unfortunately, an opportunistic screening program such as the WLCSP does not typically accommodate the sort of time required for relationship building. Previously mentioned Indigenous screening programs from the USA utilized models where relationship-building barriers are better addressed16,17. Furthermore, while clients reported satisfaction with their experience, a limitation of the data collection was the use of dichotomous rather than Likert satisfaction scales. If others were to build on this program, it may be worthwhile to consider collecting more detailed satisfaction data.
Reasons for missed appointment were not determined in this project. It is possible that factors beyond the aforementioned contributed to client ‘no shows’ (eg changes in travel plans). Finally, reasons for declining appointments were inconsistently recorded in this project and therefore not included statistically in this article. In future work, systematic collection of reasons for decline may be helpful to project improvement.
Finally, WLCSP was developed rapidly in an effort to address identified gaps in cancer screening. Unfortunately, this rapid effort was not accompanied by a long-term sustainability plan or standardized data collection and evaluative procedures. Helpful data may be ascertained in future initiatives with such plans and procedures.
Conclusion
The WLCSP was developed to mitigate cancer screening inequalities facing rural and remote First Nations communities in Northwestern Ontario, Canada. It is difficult to assess the value of the screening rates obtained, with no existing opportunistic programs targeting similar populations generating screening rates for comparison. This work may provide a helpful comparison for similar future initiatives internationally. The WLCSP was helpful in mitigating some identified barriers to screening, such as provision of education and integration of cancer screening in existing services. However, the opportunistic nature may not have been effective in addressing some important factors, such as the time required to develop trusting provider–patient relationships required for cancer screening.
Acknowledgements
The authors wish to thank Alison McMullen, former director of Prevention and Screening Services, for her contributions to initial program design; Charles Morris, former Executive Director of Wequedong Lodge, for management approvals; and Colleen McKay, Research Project Coordinator at Wequedong Lodge, for assisting in patient care, recruitment and data collection.
References
appendix I:
Appendix I: Images from the cancer screening toolkit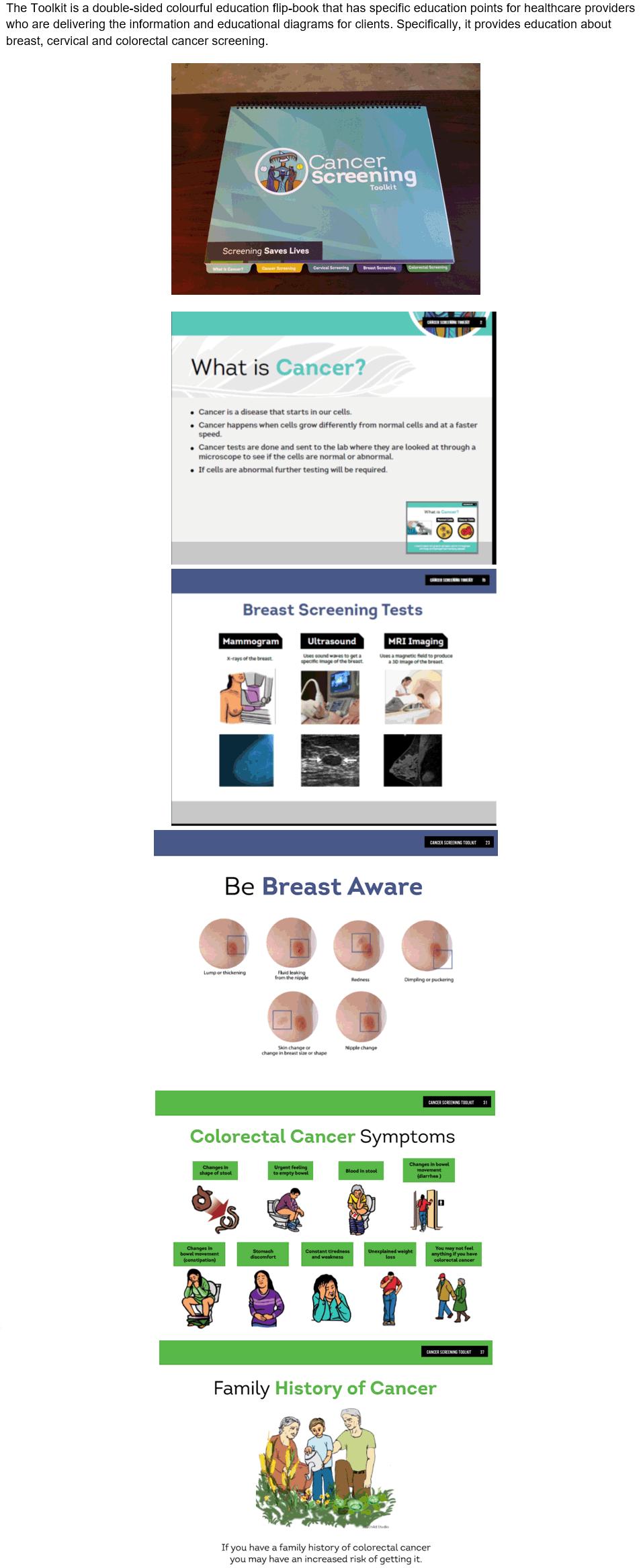
appendix II:
Appendix II: Wequedong Lodge Cancer Screening Program client evaluation survey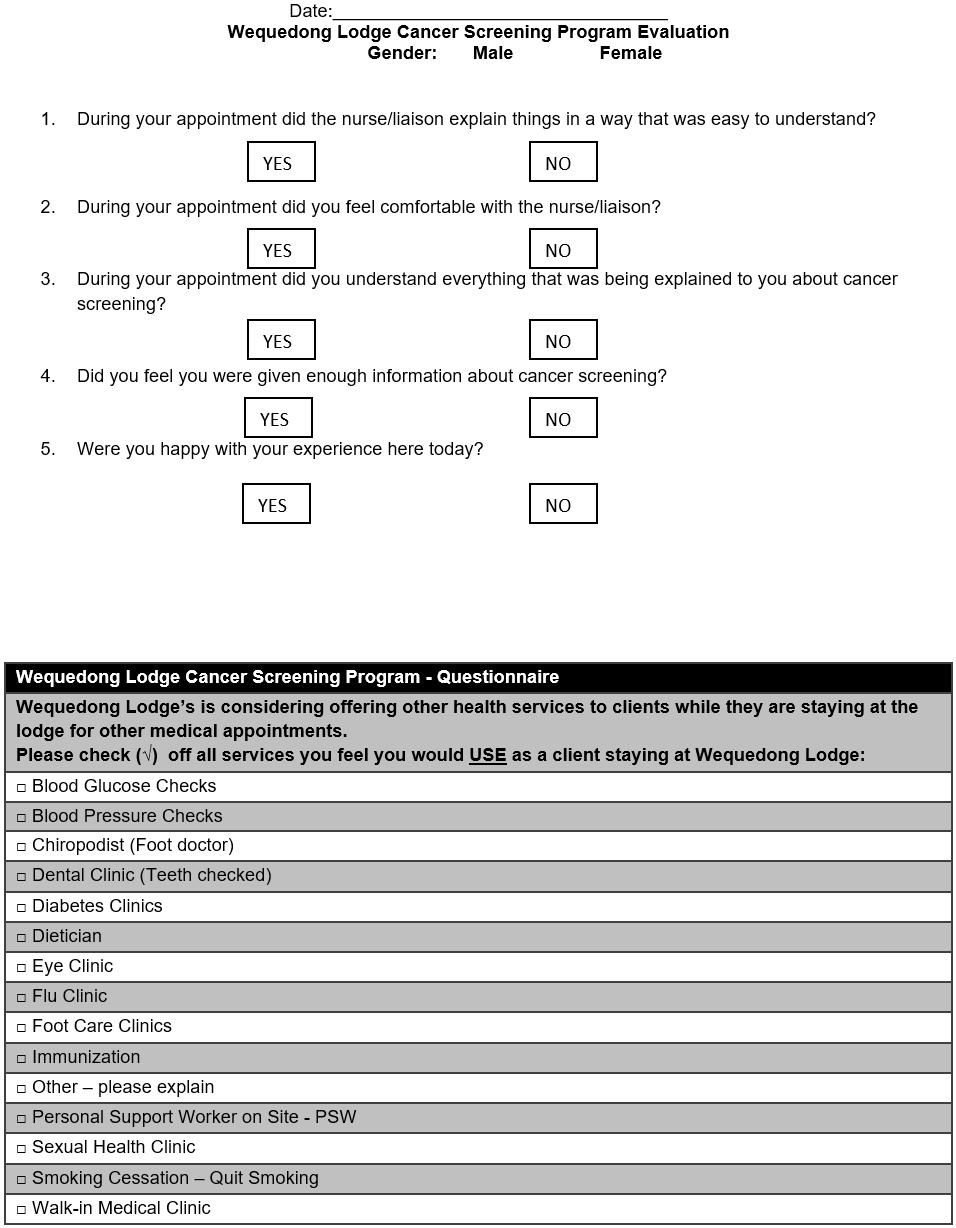
appendix III:
Appendix III: Wequedong Lodge Cancer screening program timeline, 2013–2016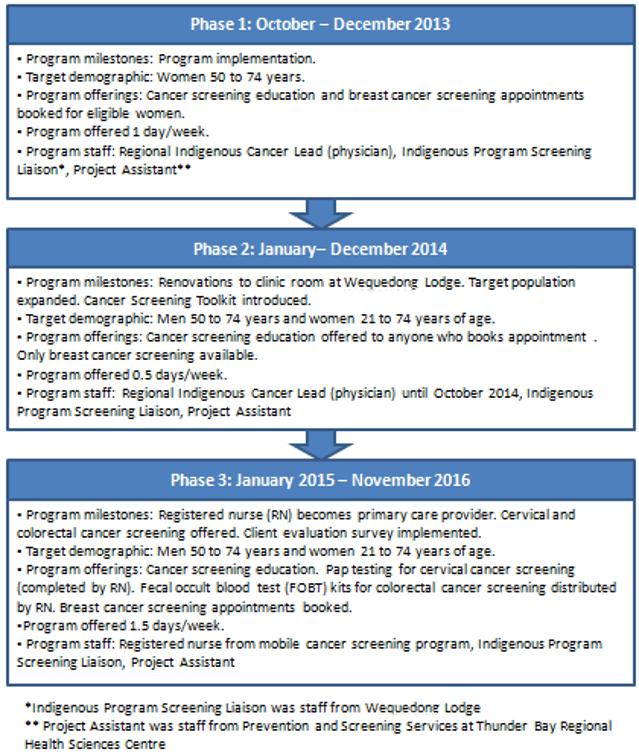
You might also be interested in:
2018 - Health Disparities in Rural Communities: Challenges and Opportunities
2012 - Psychogeriatric care: building rural community capacity



