Introduction
Overview of diabetes
Diabetes is a critical health issue that impacts more than 422 million people worldwide1. Children are not exempt from the impact of this potentially debilitating disease. Around 193 000 individuals aged less than 20 years have diabetes in the USA2 and more than 500 000 worldwide1. Diabetes management during childhood impacts the development of future health complications3. Students with chronic health conditions, such as diabetes, have an increased risk for adverse effects on their education if their condition is poorly managed3. Furthermore, students with diabetes need appropriate care in the school setting to reduce the risk of short- and long-term complications. According to WHO1, people with diabetes can live long and healthy lives if their diabetes is well managed; consequently, school staff should be trained to test blood glucose, provide insulin injections, provide glucagon injections, know how to recognize and treat hypoglycemia/hyperglycemia and know the meal plans of children with diabetes3.
Diabetes care in rural areas
Due to its widespread prevalence, diabetes is an international health concern. In the USA, rural residents have a 17% higher rate of type 2 diabetes than urban residents4. Individuals living in rural and remote areas often encounter increased difficulties in managing their diabetes due to barriers to healthcare access and health education5. Amongst other system-level barriers, rural communities grapple with minimal exposure to diabetes education and limited access to specialty care and emergency services5. Additionally, despite the fact that 16% of the US population live in rural areas, only 10% of physicians practice there5. Furthermore, 62% of rural counties within the USA do not have access to diabetes self-management education and support4. During the past couple of decades, several strategies have emerged as ways to improve diabetes management in rural areas to include the utilization of telemedicine programs, web-based efforts, telephone help lines, and support delivered via trained lay individuals4. In rural and remote areas, the provision of care to students with diabetes in the school setting is particularly important. Beyond education, rural schools play an important role in the health of students and the community.
Law addressing diabetes care in schools
All levels of policies regarding student health services strive to guide schools’ provision of diabetes care. The primary federal laws within the USA providing protection for children with diabetes include Section 504 of the Rehabilitation Act, Individuals with Disabilities Education Act, the American with Disabilities Act (ADA) and the Family Medical Leave Act6. According to these laws, schools are not allowed to discriminate against children with diabetes and those schools receiving federal funding must reasonably accommodate the needs of students with diabetes6.
Although federal laws provide equivalent protection to students with diabetes across the USA, state and local legislature such as the Nurse Practice Act and the United States Department of Health and Education regulations designate who is allowed to provide diabetes care to students. Laws in many states restrict who can provide diabetes care in schools, which can include restrictions that prohibit students from managing their own condition; elsewhere, the ambiguity of laws designating who can provide care results in inconsistent diabetes care in schools3. Although both federal and state legislation exists, schools are often unaware that diabetes is included under the ADA; as a result of limited knowledge surrounding legislature and diabetes care protocol, students with diabetes often receive inadequate care management support from lay individuals such as non-medical school personnel3.
Diabetes care in schools
Several studies have been conducted to examine the provision and quality of diabetes care management in schools; there is sufficient evidence throughout the literature to assume that students with diabetes do not always receive appropriate or adequate care in the school setting6-9. These studies primarily analyzed the experiences of students with diabetes through surveying the students themselves and/or their parents or guardians. A common finding throughout these studies was that parents and students felt dissatisfied with the level and quality of care received during the school day. A study conducted by Hellems and Clarke assessed the capacity of identified school staff members to provide adequate care7; of the 185 Virginian parents surveyed, 75% were dissatisfied with the care provided to their child. Another study found that parents of students with diabetes possessed very little to no confidence in the ability of the school to care for their child; only 55% of parents reported that their child had a written care plan, indicating a lack of preparation by school staff in the case of emergency episodes6. Schwartz et al evaluated type 1 diabetic students’ experiences with management of care in schools and found that a majority of students felt as though they were treated differently because of their diabetes and up to 53.2% reported being prevented from self-management of their diabetes8; in addition, only about 28% of students felt that school staff were knowledgeable enough to provide adequate care.
Another common finding amongst the literature was that many schools lacked the daily presence of a nurse on campus6,10-12. According to the study conducted by Jacquez et al, 45% of parents reported that a nurse was not present at their child’s school6. Unfortunately, that is not an isolated finding and even if a nurse was present in the school system, they were caring for 1350 students or more11. The American Academy of Pediatrics calls for a minimum of one full-time registered nurse in every school to care for 750 well students and 225 students requiring regular nursing assistance10; according to the National Education Association11, only 13 states currently meet the 1:750 ratio objective. This circumstance causes the delivery of proper medical care, specifically diabetes management, to be left in the hands of unlicensed and untrained school personnel. In a recent School Nurse Workforce Study, 25% of America’s schools do not employ a school nurse and only 39% have a school nurse available at all times during the school week12. The situation is particularly dire in rural America, as many communities lack any healthcare providers, so the school nurse, if there is one, becomes the frontline expert and conduit for healthcare information13.
Knowledgeable and trained school personnel are fundamental in the appropriate management of diabetes; however, studies have found that personnel feel incompetent when it comes to administering diabetes care. Fisher found that the confidence of school nurses to provide diabetes care was positively correlated to years of experience and to the frequency of administering care to children with diabetes14; however, the study also revealed that very few school nurses have access to a diabetes training curriculum. In a study with school nurses, Nabors et al found that only 54% reported adequate knowledge when working with diabetic students and 97% felt that teachers and coaches needed more diabetes care education15. Providing training and education to school personnel, and not just the nurse, can enhance the support and care that students with diabetes receive in their learning environment. The ADA suggests that educated school personnel collaborate with healthcare providers and parents to create appropriate diabetes care plans and establish locations for students to monitor their blood glucose and administer insulin16. Given the lack of nurses and lack of diabetes care training, particularly in rural areas, it is absolutely imperative that rural school systems intensify their efforts to improve provision of proper and adequate diabetes care to students.
Online diabetes education training
An increasingly popular approach to addressing diabetes care in rural, remote and underserved communities is involving trained lay individuals who understand their communities and are familiar with the day-to-day management of diabetes. Consequently, one of the most fitting ways to improve provision of care to students with diabetes in rural and remote communities is through the education and training of school personnel on how to administer diabetes care and respond to diabetic emergencies. Technology-based diabetes education has been suggested as an effective approach to reach rural populations17-19 and studies have demonstrated these types of programs can effectively improve diabetes knowledge and diabetes self-management20,21. A recent study evaluating the effectiveness of using technology to provide diabetes education for rural communities found that diabetes knowledge scores showed a statistically significant increase from pre- to post-educational intervention22. Bachman and Hsueh piloted an online diabetes care education program for school nurses23. They found that 91% of the participants thought the program increased their ability to appropriately manage students with diabetes while noting a preference for online education because it fit into their personal schedule, did not require them to travel, did not require them to miss work, and built on their previous knowledge at their own convenience and speed. Online continuing education programs can enhance the school nurses’ and lay individuals’ ability to care for students with diabetes by providing a more manageable and accessible, time- and money-saving learning format than in-person courses. Providing accessible training for school personnel could significantly improve the care that students with diabetes receive and improve their overall long-term health outcomes.
Theoretical framework
Bandura’s theory of self-efficacy has been used frequently in health literature to analyze and document outcomes of education programs; self-efficacy can be described as an individual’s belief about their capabilities to exhibit a certain level of performance on a given activity24. Although studies have demonstrated that online diabetes education programs can increase the knowledge and self-efficacy of participants and clinicians25,26, few studies have addressed the self-efficacy of school employees for providing diabetes care. As the number of students with diabetes continues to rise, more research needs to be conducted and more education regarding diabetes care needs to be provided in order to assist school personnel with developing the required skills and confidence to provide optimum care to students. The purpose of the present study was to analyze the impact of the online diabetes education program Diabetes Care at School: Bridging the Gap on the diabetes knowledge and self-efficacy of school personnel in rural areas to administer care to students with diabetes.
Methods
This quantitative study analyzed data from participants who completed the Diabetes Care at School: Bridging the Gap online training program. The online program was specifically designed by a certified diabetes educator to help schools (with or without a school nurse) to meet state and federal requirements and to help school personnel to create a safe and supportive learning environment for students with diabetes. Participating districts received a 1-year subscription for each campus, which included constant access to the online training program for all school personnel. Thirty-six school districts within South Central Texas received free access to the program, allowing each employee to receive a username and password to access the online training program.
Participants
Purposive sampling was used to focus on the employees from those 36 rural school districts that completed the education program. This study focused on those that completed the level 2 (non-medical personnel) and level 3 (continuing nursing education (CNE)) training. Participation was optional and included school district employees who chose to complete the program, such as nurses, teachers, principals, bus drivers and food service staff. Overall, those who completed the program at each campus were typically the school nurse and diabetes care assistant assigned by the principal.
Program description
Diabetes Care at School: Bridging the Gap is a comprehensive, online, e-learning program designed to address the training needs of school staff members who may be called upon to assist a student with diabetes27. The program has three levels of diabetes training: (1) diabetes awareness training for general staff, about 25 minutes; (2) non-medical personnel training, which consists of eight modules, about 4.5 hours; (3) CNE training, which is an advanced training for school nurses to receive CNE hours and contains an additional module on laws and legal issues27. The fully narrated and interactive e-learning programs contain diabetes skills training videos; links to diabetes-related web resources; and samples of a diabetes medical management plan, individual health plan and emergency information sheet. Table 1 provides an overview of the primary topics within each module.
Table 1: Diabetes Care at School: Bridging the Gap program overview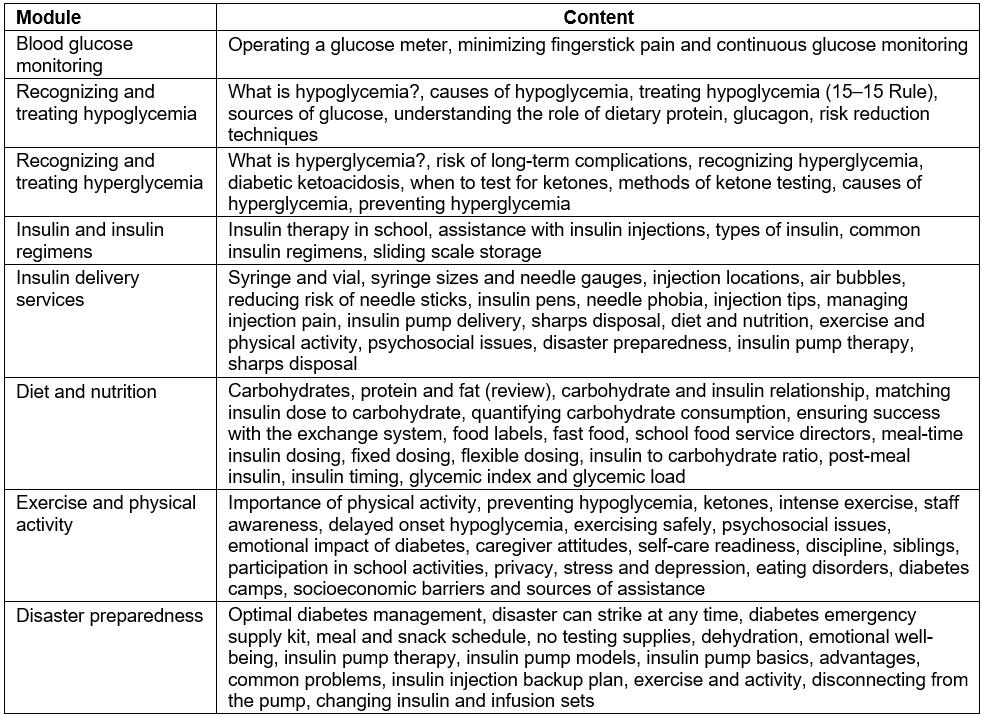
Instruments
The introductory survey required by each participant included questions addressing the participant’s current occupation (superintendent, principal, vice principal, classroom teacher, physical education teacher, school nurse, office staff, food service worker, bus driver, other), status of diabetes training in the past 12 months, and communication preferences. The 30-question knowledge pretest and post-test was developed for this study by the Texas Diabetes Council and was reviewed by a committee of certified diabetes educators to evaluate the tool for content and ease of completion. In addition, the survey was reviewed by the Texas Nurses’ Association for content validity. The instrument designed to measure the change in self-efficacy of the participants consisted of a self-assessment by participants addressing confidence for assisting students with diabetes prior to and after completing the training program. Utilizing a seven-point semantic scale ranging from ‘not at all confident’ to ‘extremely confident’, participants were asked to rate their confidence in their ability to assist students with diabetes prior to completing the online program. The instrument was reviewed by certified diabetes educators and utilized in the pilot study. In addition, the instrument addressed the program’s effectiveness with preparing users to perform specific diabetes-related tasks. This was measured on a seven-point semantic scale ranging from ‘not at all effective’ to ‘very effective’ based upon the skills identified by the Texas Diabetes Council. For the purpose of the present study, only the confidence data from the first two questions assessing confidence prior to and after completing the program were utilized. Learner satisfaction with the online training format was measured on a seven-point semantic scale that addressed the user’s perception of the integrity of the program.
Procedure
The data were collected utilizing a quasi-experimental design. Specifically, participants completed a designated track based upon their status of school nurse or non-medical personnel. A pretest–post-test design was used to measure knowledge before and after completion of all of the modules. The pretest–post-test design was utilized to assess the participants’ self-assessment of confidence with diabetes skills before and after completing the program, and post-test only design assessed satisfaction with the online training program. The pretest, post-test and evaluation surveys were administered electronically through a learning management system (LMS). The investigator was provided with the demographic information, results of the pre- and post-tests, self-assessment rating of confidence to perform diabetes tasks, and self-assessment of the helpfulness of the tools for each participant, as captured in the LMS.
Data analysis
The quantitative data were analyzed using the Statistical Package for the Social Sciences v17.0 (IBM; http://www.spss.com). Descriptive statistics represented demographic data, knowledge change scores and confidence change scores for each participant. Paired-samples t-tests were conducted to compare the means of the pre- and post-test knowledge and confidence scores for non-medical personnel and school nurses. Independent samples t-tests were conducted to compare the change in knowledge and change in confidence scores of the non-medical personnel and school nurses. Independent t-tests were also performed to determine if prior diabetes training impacted the change in knowledge scores and confidence scores of the participants. Finally, a bivariate correlation, using Pearson’s correlation coefficient, was run to look at the relationship between knowledge change scores and usefulness of program, confidence change scores and usefulness of program, and the knowledge change scores and confidence change scores.
Ethics approval
This study was approved by the Institutional Review Board at Texas Woman’s University (protocol 16663).
Results
The sample of the study included 132 participants. As shown in Table 2, almost two-thirds of the participants completed the non-medical personnel training (63.6%) and one-third completed the school nurse CNE training (36.4%). It is important to note that three of the school nurses completed the non-medical personnel track instead of the school nurse CNE, which is why the training type and status frequency and percentages for school nurses and non-medical personnel vary. Overall, a majority of the participants were school nurses (38.6%) followed by other (28.0%), classroom teachers (9.8%), physical education teachers (9.1%), office staff (7.6%), vice principals (3.8%), principals (1.5%), bus drivers (0.8%) and food service workers (0.8%). A majority of the participants had no prior diabetes training within the previous 12 months (68.9%).
As shown in Figure 1, the pretest knowledge scores for nurses were significantly higher than for non-medical personnel; however, there was not a significant difference in the post-test knowledge scores between the two groups. Although non-medical personnel had a larger change in knowledge scores, there was a significant increase from pre- to post-intervention for both groups. A paired-samples t-test was performed to compare the pretest and post-test knowledge scores for non-medical personnel and school nurses. There was a significant difference in the average pretest (mean (M)=49.75, standard deviation (SD)=16.25) and post-test (M=90.04, SD=6.66) knowledge scores for non-medical personnel; t(80)= –23.12, p=0.000. School nurses also had a significant increase in knowledge scores from the pretest (M=69.58, SD=14.90) to the post-test (M=94.25, SD=5.89); t(50)= –13.92, p=0.000. There was a positive correlation for both groups; non-medical personnel and school nurses who did well on the pretest also did well on the post-test.
As shown in Figure 2, the pretest confidence scores for non-medical personnel were significantly lower than for school nurses; however, the non-medical personnel had a much larger change in confidence scores, resulting in similar post-test confidence scores between both groups. A paired-samples t-test was conducted to compare the means between the pretest and post-test confidence scores for non-medical personnel and school nurses. There was a significant difference in pretest confidence scores (M=3.46, SD=1.87) and post-test confidence scores (M=6.30, SD=1.17) for non-medical personnel; t(80)= –15.45, p=0.000. Although not as much, there was also a significant difference in the pretest confidence (M=5.80, SD=1.34) and post-test confidence scores (M=6.94, SD=0.24) for school nurses; t(50)= –6.50, p=0.000. These results suggest that the training program was effective with improving both the non-medical personnel’s and school nurses’ confidence for performing diabetes care. An independent samples t-test was performed to compare the confidence change scores between non-medical personnel and nurses. There was a significant difference in the scores for non-medical personnel (M=2.84, SD=1.65) and nurses (M=1.14, SD=1.25); t(130)=6.30, p=0.000. Non-medical personnel had a much larger change in confidence as a result of the program than nurses.
An independent t-test was conducted to determine if prior diabetes training impacted the change in knowledge scores of the participants. Participants with no prior diabetes training within the previous 12 months experienced a greater change in knowledge (M=36.28, SD=16.78) than those with training (M=29.76, SD=14.80); the difference was significant t(130)=2.14, p=0.03. However, there was no significant difference between the post-test knowledge score of those with prior diabetes training (M=91.76, SD=6.86) than those without (M=91.46, SD=6.33); t(130)=0.234, p=0.815. These results demonstrate that although those with prior diabetes training had initially higher pretest knowledge scores, after completing the modules there was no significant difference in knowledge scores between those with and without prior diabetes training.
An independent samples t-test was also conducted to assess whether prior diabetes training impacted the confidence of the participants to administer diabetes care. Participants with no prior diabetes training had lower pretest confidence scores (M=4.09, SD=2.08) than those with prior training (M=4.98, SD=1.81); t(130)= –2.359, p=0.020; however, those without prior training (M=2.38, SD=1.74) had a greater increase in change in confidence than those with prior training (M=1.73, SD=1.60) and the difference was significant; t(130)=2.042, p=0.04. For the post-test confidence scores, Levene’s test was significant at p<0.05, supporting the hypothesis that the variances between the two conditions were significantly different, which violates the assumption of homogeneity of variance. Those with no prior training (M=6.47, SD=1.08) had lower post-test confidence than those with prior training (M=6.71, SD=0.68); however, the difference was not significant; t(115.91)= –1.51, p=0.13. These results demonstrate that although those with prior diabetes training had lower pretest confidence scores, the program was effective with increasing their confidence, as there was no significant difference in the post-test confidence scores between those with and without prior diabetes training.
A bivariate correlation, using Pearson’s correlation coefficient, was run to look at the relationship between knowledge change scores and usefulness of program, confidence change scores and usefulness of program, and the knowledge change scores and confidence change scores. Although there was a negative relationship between knowledge change scores and usefulness of program, it was very weak, r= –0.092. The relationship between confidence change scores and usefulness was positive and also very weak, r=0.017. The weak relationships demonstrate that knowledge and confidence change scores were not significantly correlated with the participants’ rating of the usefulness of the program. However, there was a significant, positive relationship between the change in knowledge scores and change in confidence scores, r=0.442, p (one-tailed)<0.01. The change in confidence to perform diabetes care increased as the participants’ knowledge of diabetes increased as a result of completing the online program.
Table 2: Frequencies and percentages for categorical demographic variables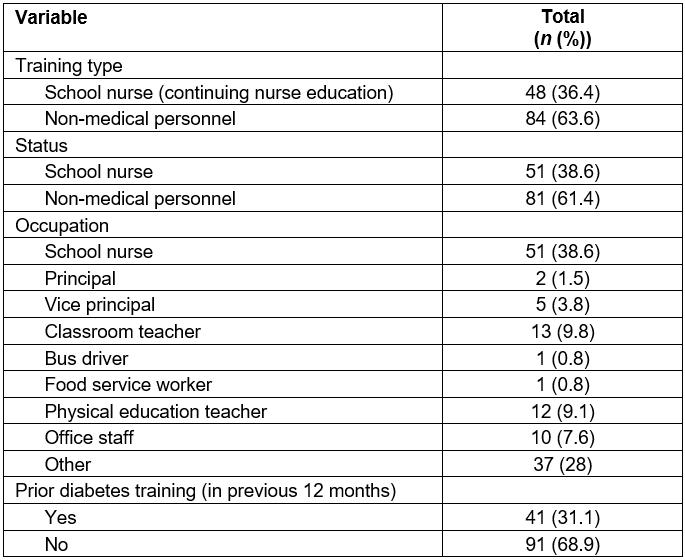
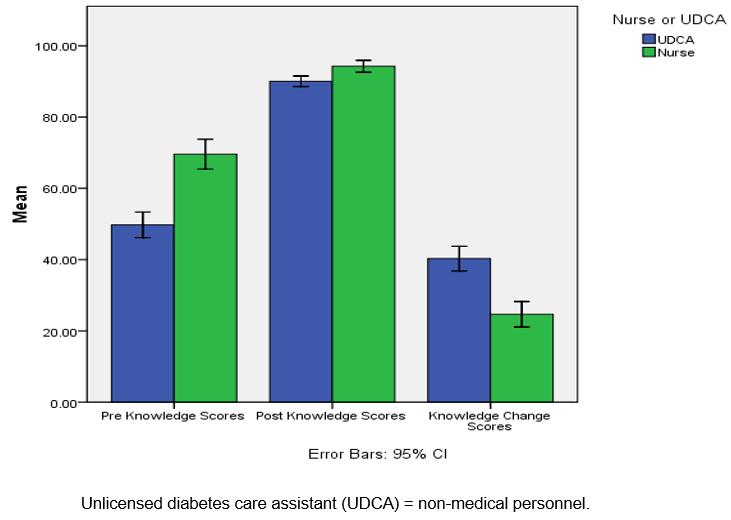 Figure 1: Overall subscale pretest, post-test and change in knowledge scores.
Figure 1: Overall subscale pretest, post-test and change in knowledge scores.
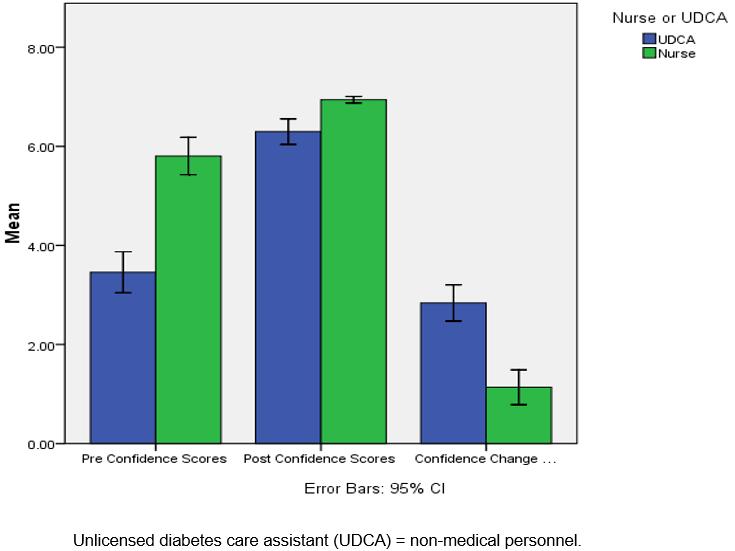 Figure 2: Overall subscale pretest, post-test and change in confidence scores.
Figure 2: Overall subscale pretest, post-test and change in confidence scores.
Discussion
This study examined the impact of an online diabetes education program on the diabetes knowledge and self-efficacy of school personnel in rural areas to administer care to students with diabetes. It specifically looked at lay individuals and nurses working in school settings in rural areas across South Central Texas. It was found that although the pretest knowledge and confidence of the non-medical personnel was significantly lower than for the nurses, both groups made significant gains in knowledge and confidence to administer care as a result of the online diabetes education program.
Limitations
Although the results of this study are encouraging, several limitations need to be mentioned. The data were limited to those school district employees in South Central Texas, specifically the school nurses and lay individuals that decided to complete the online training program. The circumstances and knowledge of the non-medical personnel varied. Some voluntarily chose to be trained; others were appointed by the principal. Some may have had existing knowledge and understanding of diabetes. The demographic information gathered in the LMS was limited and did not include information such as education level, primary language and computer literacy. The data in the study provided a good indication of differences in change in knowledge and self-efficacy scores among school personnel specifically in South Central Texas. However, given the data and sampling limitations, it should not be taken as completely accurate or generalizable to the entire population. Additional studies should be performed.
Recommendations for future research
Although significant changes in the knowledge and confidence of participants to administer diabetes care in schools were demonstrated within the study, additional follow-up is necessary to assess the implications to school health practice and care of students with diabetes in rural and remote communities. Future research should be devoted to surveying the parents of students with diabetes from the campuses that participated in the online training program to assess their satisfaction with the diabetes care at school; questions should specifically assess whether or not care improved after the program was administered. Follow-up studies should also be conducted to assess the outcomes for the students with diabetes. Surveys with students and parents can further assess their perspective of blood glucose monitoring, insulin administration, and other aspects of diabetes care at school. Finally, further work is needed to identify practice outcomes related to online diabetes education programs and to assess the sustainability of knowledge gains and practice changes with this educational platform. With the exponential growth of the internet and distance education, further studies are necessary to maximize the efficacy of this educational format, particularly in rural areas.
Conclusion
As the prevalence of school-aged children with diabetes continues to increase, an important finding of this study is that online programs with up-to-date information on diabetes care may enhance the ability of school personnel to include both lay individuals and school nurses to effectively manage the care of students with diabetes. The online method allows for continuing education opportunities for school nurses, teachers and non-medical personnel who don’t have access to face-to-face training opportunities. The online program allows flexibility with completing the modules, allowing participants to access and complete at their own pace. In addition, they can access in the future if they want to review materials, videos or links to resources. The online format saves travel time and substitute teacher expenses. However, it is important to note that access to a computer and computer skills are needed to complete the program. Another important finding is that online programs are not preferred by everyone; this study found a weak relationship between change in confidence and knowledge and the participants’ rating of the usefulness of the program. With up-to-date diabetes information delivered in a user-friendly and accessible format, more school personnel in rural and remote areas can be trained. Hopefully, this will result in better daily diabetes management and fewer diabetic emergencies of students while at school. Ultimately, the goal is to create an environment that is safe and conducive for learning for all students.
References
You might also be interested in:
2006 - Medical students' assessments of skill development in rural primary care clinics
