Introduction
Internal migration is a type of migration that occurs within the same country (mobilization of people between urban and rural areas), being more frequent than international migration. Internal migration is linked to the search for economic and educational opportunities in areas of higher development, usually an urban setting1-3. Indeed, it has been estimated that more than 740 million people worldwide have migrated within their own country of birth, according to the Human development report 20094.
In 2017, depression ranked third as a cause of years of life with disabilities worldwide5, being more frequent in women (5.1%) than men (3.6%)6. The migratory phenomenon has an impact on the health status of populations7. It has been described that the risk of developing mental health problems, including depression, is higher in migrant populations, with a prevalence of 16%8. Although the migration rates according to sex are usually similar, women are more vulnerable to developing physical and mental health problems during migration and are affected differently9. This has been associated with sociocultural factors, gender and child care, unfavorable working conditions and difficulty in accessing health services10,11.
In Peru, there has been a considerable internal migration phenomenon motivated by finding new employment or educational opportunities and avoiding violence and internal armed conflicts12. The phenomenon of internal migration in Peru has been variable in recent decades, with internal migrants representing 8.4% of the population in 1993 and 6.2% in 200712. By 2015, approximately seven million Peruvians (22.6%) were internal migrants12.
Neuropsychiatric diseases are in first place concerning disease burden in Peru, with unipolar depression being the more frequent mental health problem (224 535 disability-adjusted life years lost annually, constituting 3.9% of the total), with an equivalent of 7.5 years lost per thousand inhabitants13. Nonetheless, despite many reports in the medical literature about migratory processes and the effects on mental health in the migrant population, the evidence is scarce in the Peruvian context14,15.
In many countries, demographic health surveys are carried out to study health problems, including mental health problems. Since 1986, the National Institute of Statistics and Informatics of Peru has performed the Demographic and Family Health Survey (ENDES), which is widely used to study various health problems in women of childbearing age and children aged less than 5 years16,17. Taking into account that the phenomenon of internal migration in Peru may be associated with mental health disorders such as depression, and since women are vulnerable to depressive symptoms, the aim of the present study was to estimate the prevalence and factors associated with depressive symptoms in Peruvian women of childbearing age and the probability of presenting these symptoms according to internal migration conditions.
Methods
Study design, sample and sampling
A secondary analysis of the ENDES data obtained over the 5 years from 2014 to 2018 was performed and the results of the five surveys combined to increase statistical power. Since 2014, ENDES has been used annually to collect data to assess the mental health status of the Peruvian population. ENDES uses balanced two-stage, probabilistic, stratified and independent sampling, with representativeness at the departmental level and by urban and rural area. More methodological details can be found in the ENDES technical report18.
Data available for women between 15 and 49 years were included in the study. Women who reported being home visitors or international migrants were excluded from the study. Thus, in 2014–2018, the numbers of women included in the study, respectively, were 9024, 13 100, 12 806, 13 086 and 1842.
Variables
The dependent variable was the presence of depressive symptoms (yes/no) during the 14 days before the survey, measured by the Patient Health Questionnaire (PHQ-9). The PHQ-9 is a screening test to detect and measure the severity of depressive symptoms19, and it has been validated through expert judgment in several countries, including Peru20. The PHQ-9 test has also been validated for reliable comparisons according to the sociodemographic characteristics in the Peruvian population in a recent publication21.
The PHQ-9 contains nine questions. The answers are measured on a four-point Likert scale, ranging from 0 (not at all) to 3 (nearly every day) with a total score ranging from 0 to 27 points19. In accordance with another national study22, a cut-off point of ≥10 points was considered to define the presence of depressive symptoms.
Migration condition was considered as an independent variable for the analysis. Following the methodology of other studies23,24, the variable was constructed using the answers about age, current place of residence and previous place of residence reported by the women. The following questions were used to construct the migration condition (codes of the variables within the database appear in square brackets): Type of residence where you live [V102], How long have you been living continuously in (name of current place of residence)? [V104], Before you came here, did you live in a city, a town, or in the country? [V105] and age of the woman in years [HA1]. This information was used to construct six categories of the variable condition of migration: non-rural migrant (woman residing in a rural area throughout her life), non-urban migrant (woman residing in an urban area throughout her life), intra-rural migrant (migrant woman within a rural residence area), intra-urban migrant (migrant woman within a urban residence area), rural–urban migrant (migrant woman from rural to urban area) and urban–rural migrant (migrant woman from urban to rural area). These categories are mutually exclusive for the condition of migration. The same categories were used in a previous study about migration and obesity in Peru24 and related to modern contraceptive use among migrant and non-migrant women in Kenya23.
The following covariates were considered in the analysis according to previous literature that reports these variables as being associated with the presence of depression or depressive symptoms6,8,25,26: years lived in place of residence, female head of household (yes/no), marital status (single, married or stable relationship, widow or divorced), level of education (no education, primary education, secondary education, higher education), wealth quintile (I (poorest), II, III, IV, V (less poor)), smoker (yes/no), alcohol consumer (yes/no) , presence of diabetes (yes / no), presence of obesity (yes/no), presence of physical disability (yes/no), altitude in meters above sea level of the residence area (0–499 m, 500–1499 m, 1500–2999 m, 3000 m or more). The cut-off points for the altitude of the residence area were defined based on a previous study conducted in Peru27. The variable age of the woman in years was not included in the analysis due to the correlation with the variable years lived in the place of residence. Estimating a logistic model in which two or more covariates correlate would violate the multicollinearity assumption, and inaccurate estimates of the parameters are obtained28.
Statistical analysis
The integration, processing and statistical analysis of the databases were performed using Stata v14.2 statistical software (StataCorp; http://www.stata.com). The svy command was used to specify the sample design characteristics and the weighting factors of ENDES.
To describe the quantitative variables, the mean and standard deviation were estimated. To describe the qualitative variables, absolute frequencies and weighted proportions with their 95% confidence intervals (95%CI) were reported. To assess the factors associated with depressive symptoms, crude odds ratios (OR) were estimated using bivariate logistic regression. Then, adjusted OR (aOR) were estimated using multivariate logistic regression, including those variables showing a p-value less than 0.20 in the bivariate analysis. A p-value of less than 0.05 was considered statistically significant. Multicollinearity was assessed using the variance inflation factor, which measures the inflation in the variances of the parameter estimates due to multicollinearity potentially caused by the correlated predictors.
Finally, the marginal effects were calculated and plotted together with their 95%CI from the multivariate logistic model to obtain the probability of having depressive symptoms concerning the years lived according to the status of internal migration. Rural non-migrant women were considered the reference group.
Ethics approval
This study did not require the approval of an ethics committee because it is an analysis of secondary data that are in the public domain and that do not allow identification of participants.
Results
A total of 61 852 women with a mean age of 31 years were included in the analysis. On average, women had lived continuously in their current place of residence for 19 ± 13 years. Women in an urban area who never migrated (36.8%) and women who migrated within the urban area (25.1%) during the study period were the most prevalent. The general prevalence of depressive symptoms in women decreased from 2014 (7.1%, 95%CI: 6.6–7.7) to 2018 (5.9%, 95%CI: 5.5–6.3). No variations were observed in the rest of the variables described during the study period (Table 1).
Table 2 describes the prevalence of depressive symptoms according to the migration condition. In the general population of women of childbearing age, the findings suggest a reduction in the prevalence of depressive symptoms during the study period (p<0.01). According to migrant status, only the intra-urban migrants subgroup presented a significant reduction in the prevalence of depressive symptoms (a percentage reduction of 2.5, p<0.01). The prevalence of depressive symptoms was similar across all migrant groups. Women whose migration was rural to urban, intra-rural and intra-urban showed a slightly higher burden of depressive symptoms in the study period, but these results were not statistically significant.
Regarding the factors associated with depressive symptoms, all the covariates in the bivariate model presented a significant p-value in at least one category. The multivariate analysis showed no association between depressive symptoms and obesity (aOR: 1.06, 95%CI: 0.98–1.14). Compared to women in rural areas who never migrated, all the other migration conditions showed a higher probability of presenting depressive symptoms (p<0.001 for all categories). Specifically, the probability of women with a rural–urban migration pattern developing depressive symptoms was two-fold higher (aOR: 2.11, 95%CI: 1.77–2.53) compared to women residing in urban areas who did not migrate. Also, a directly proportional relationship was found between depressive symptoms and the years lived in the place of residence (aOR: 1.02, 95%CI: 1.01–1.02). Factors such as being the head of the household (aOR: 1.30, 95%CI: 1.19–1.42), marital status (married/cohabiting (p<0.001) and separated/divorced/widowed (p<0.001)), risk behaviors such as smoking (aOR: 1.97, 95%CI: 1.71–2.28) or alcohol consumption (aOR: 1.50, 95%CI: 1.31–1.73) and the presence of other diseases such as diabetes (aOR: 2.26, 95%CI: 1.82–2.80) or an impairment (aOR: 2.09, 95%CI: 1.58–2.75) were associated with a higher probability of depressive symptoms. In addition, living at higher levels of altitude was associated with a higher probability of having depressive symptoms (p<0.001 for all categories compared to living at 0–499 m above sea level) (Table 3).
Figure 1 shows the marginal effects at the means of the relationship between the condition of internal migration and the probability of depressive symptoms, taking into account the number of years of living in the place of residence adjusted by the covariates included in the multivariate model. Two overall results are shown. First, the effect of the number of years lived in the place of residence on depressive symptoms was lower in the group of women who had never emigrated. Second, the effect of living approximately 25 years in the place of residence on depressive symptoms was magnified in all migrant groups. Thus, the difference between the probability of depressive symptoms of the migrant and non-migrant groups gradually widened over time.
Table 1: Sociodemographic characteristics of Peruvian women (2014–2018 ENDES) 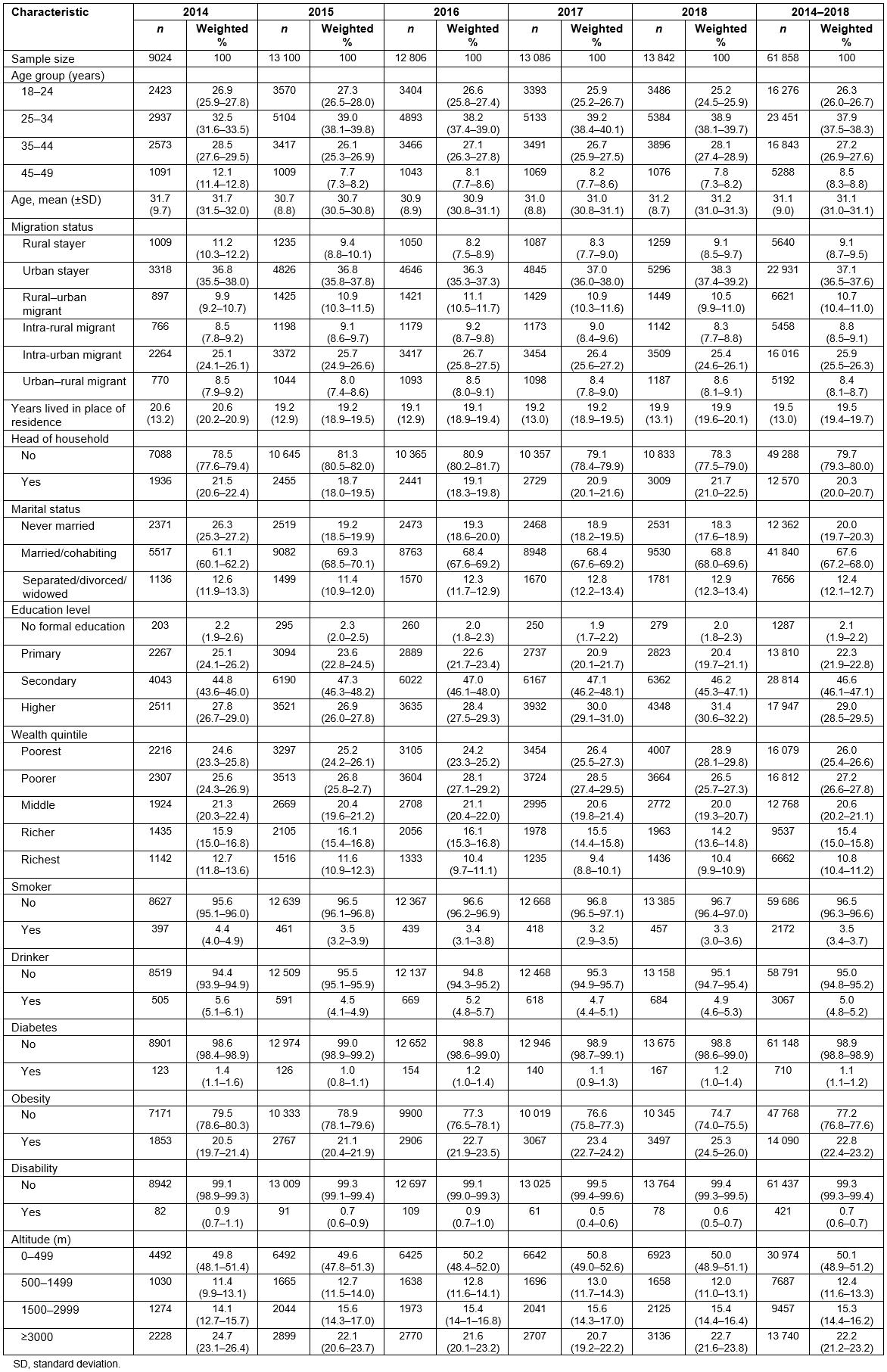
Table 2: Prevalence of depressive symptoms according to migration status in Peruvian women (2014–2018 ENDES)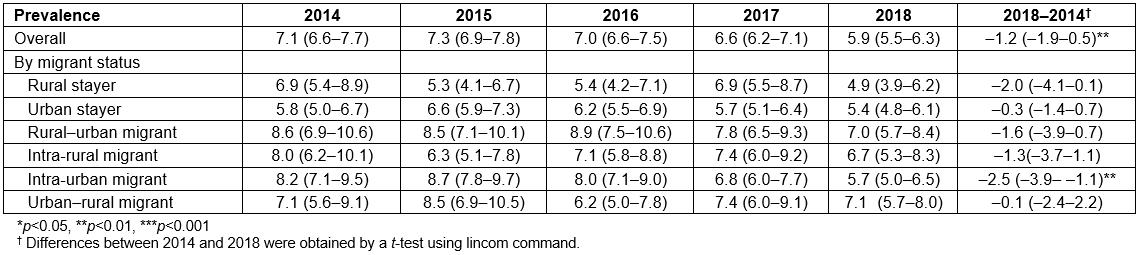
Table 3: Factors associated with depressive symptoms in Peruvian women (2014–2018 ENDES)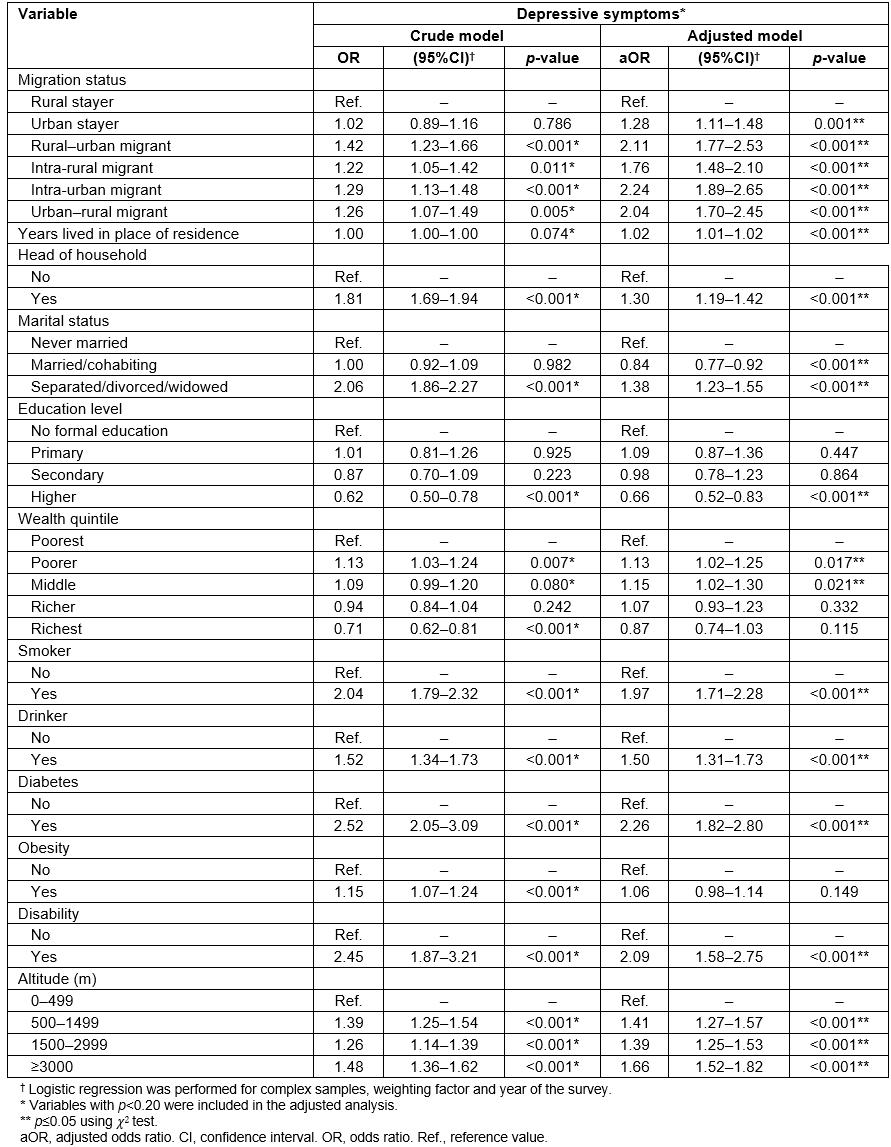
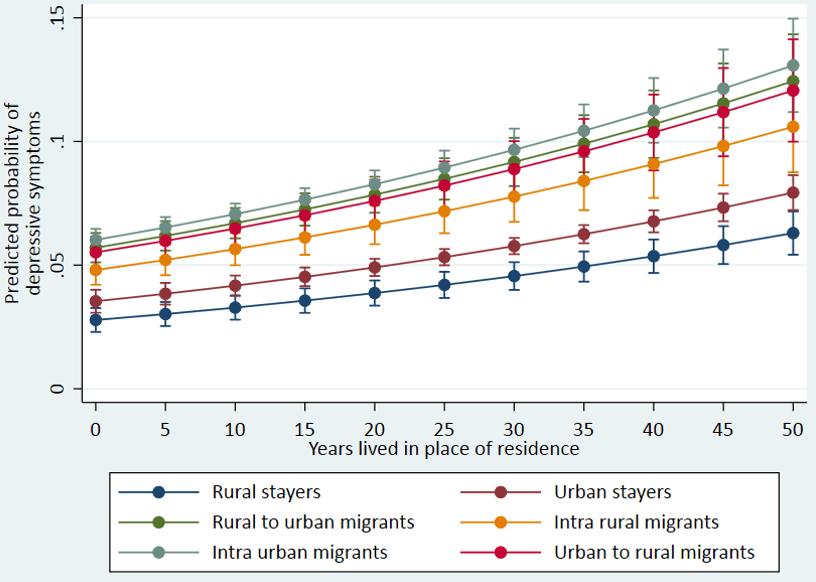 Figure 1: Adjusted prediction of having depressive symptoms among migrant Peruvian women in relation to the years lived according to the status of internal migration.
Figure 1: Adjusted prediction of having depressive symptoms among migrant Peruvian women in relation to the years lived according to the status of internal migration.
Discussion
This study determined the prevalence of depressive symptoms in Peruvian women of childbearing age and the probability of depressive symptoms according to the condition of internal migration. In the general population of women of childbearing age, the prevalence of depressive symptoms decreased in women during the period from 2014 to 2018, similar to the subgroup of intra-urban migrants. Compared to women in rural areas who never migrated, all other migrant statuses were associated with an increased probability of depressive symptoms. Furthermore, years lived in the place of residence, being the head of the household, being married/cohabiting or separated/divorced/widowed, smoking, alcohol consumption, diabetes, having an impairment, and living at levels of altitude greater than 500 m were associated with a higher probability of having depressive symptoms.
The prevalence of depressive symptoms decreased in women of childbearing age between 2014 and 2018. However, worldwide there has been an increase in the prevalence of depression in the general population, with women having an increased risk compared to men to have depression6 and increase in the global burden of disease worldwide due to this disease5. Although depressive symptoms seem to be higher in the group migrating from rural to urban areas and, in general, in migrant groups compared to non-migrant groups, these differences were not statistically significant. In Peru, the most frequent migratory pattern is towards urban areas in search of work or educational opportunities12, similar to that reported worldwide1-3. A higher burden of depressive symptoms in migrants from rural to urban areas has been reported in other countries in Latin America and worldwide8. This excess in the burden of disease can be explained by the acculturation phenomenon, including changes in eating patterns, city stress and lifestyle8,25,26, which makes it necessary to study the relationship between these factors and the development of depression in the Peruvian internal migrant population.
Migrant women are usually young and without family bonds, thereby facilitating their mobilization to other territories in search of economic wellbeing29. The Peruvian migrant population is also characterized by being young, as well as being female with a low education level and dedicated to the care of the home or work in the field30. A study performed in Hong Kong found that, in the general population, single people present a higher prevalence of depressive symptoms than those with a partner31. Bearing in mind that migration processes also affect the internal migrant population, the findings of this study are in the same line to the present study’s results, which showed that, compared to married women, being an unmarried Peruvian internal migrant woman was associated with the presence of depressive symptoms. Given the predominant type of migration of the Peruvian population (towards urban areas) and the sociodemographic characteristics of this population, the presentation of mental health problems among internal Peruvian migrants is to be expected, making the need for mental health strategies a priority in Peru.
A positive relationship was found between post-migration residence time and the probability of having depressive symptoms. Acculturation processes may explain this relationship for international and internal migrants, and have been associated with the development of stress and post-migration mental health problems8,25,26. In the literature, the ‘effect of the healthy migrant’ indicates that the migrant from a less developed area has a better state of health compared to the residents32,33. This ‘better state of health’ should be similar in migrant and non-migrant groups. Therefore, a higher prevalence of illness among migrant groups is considered to be due to difficulties in social adaptation and problems with access to health services32,33. Moreover, migrants have to face stressors such as unfavorable working conditions in the areas to which they immigrate, the need to be away from their families, in addition to experiencing economic and non-economic barriers to achieve access to health care34,35. In Peru, the development of strategies to tackle depression must consider migrants as a disadvantaged group.
Migrants who undergo a non-planned migration have a higher risk of developing depressive symptoms31, in addition to having a higher consumption of illicit drugs compared to local migrants36. In Peru, the consumption of alcohol in women has increased in relation to changes in cultural conceptions37, with the consumption of these substances being associated with a higher prevalence of depressive symptoms in the population studied. Therefore, it has been described that the availability of social support to migrant women reduces the likelihood of depressive symptoms38. In this regard, in Peru, Law No. 29889 (2012) is aimed at guaranteeing the rights of people with mental health problems and the continuity of care for their health demands within the Peruvian health system39. In 2018, the Ministry of Health of Peru published policy guidelines in mental health that establish the integral care of mental health for individuals, family and community, including the protection of rights, guaranteed access to mental health services and a reduction of risks, damages, disability and premature mortality due to mental health problems13. This guideline established a strategy for comprehensive care of mental health in the migrant population and recognized the impact of the migratory process on the mental health of the migrant population13. The Peruvian State has taken this position towards mental health, considering the global awareness of the high burden of disease due to mental health problems. Preserving the health of the migrant population is in line with the global panorama of the Sustainable Development Goals, ensuring a healthy life and promoting wellbeing for all people40.
Limitations
The use of secondary data can induce challenges for the analysis of health problems, since some characteristics of the population may not be available due to the nature of this source of information. The ENDES data do not specify the reason for the migration of women (forced or voluntary) or the characteristics of the social support during migration (family migration, friends, others). This information would have allowed a more detailed analysis of depressive symptoms in the migrant population. Additionally, with the tool used to measure depressive symptoms in the respondents (PHQ-9), it is not possible to establish temporality of the relationship between depressive symptoms and migration, and therefore the results could only find an association between a previous phenomenon of migration and the presence of depressive symptoms in the 2 weeks before the survey. Nonetheless, the authors consider that these findings provide an overview of an issue that requires further study in Peru.
Conclusion
There has been a decrease in the prevalence of depressive symptoms in Peruvian women of childbearing age during the period from 2014 to 2018. The number of years lived in the place of residence, being the head of the household, a marital status other than single, being of a wealth quintile 2 and 3, smoking, drinking alcohol, having diabetes, having a disability, and living 500 m or more above sea level were associated with a higher probability of presenting depressive symptoms. Regarding the migratory pattern, the group of women migrating from rural to urban areas presented the highest prevalence of depressive symptoms, although, in general, a decrease in the prevalence of depressive symptoms was found for all the internal migration conditions studied. Preventive strategies are needed to address the factors associated with depressive symptoms in female Peruvian migrants given their vulnerability to the development of this mental health problem.
References
You might also be interested in:
2018 - Oral Health Disparities among Adolescents from Urban and Rural Communities of Central Chile
2016 - Doctors as street-level bureaucrats in a rural hospital in South Africa