Context
Acute rheumatic fever (ARF) and its sequela, rheumatic heart disease (RHD), are prevalent among Australian Aboriginal people, with the most common ages of ARF acquisition being between 5 years and 14 years1. The mainstay of medical management in Australia for a confirmed or probable case of ARF is a regimen of long-acting benzathine benzylpenicillin G (BPG) injections. Oral penicillin has been shown to be inadequate as secondary prophylaxis in this instance2. The Australian guideline currently recommends that the regimen is continued for 5–10 years after the last known episode of ARF, depending on cardiac involvement, or until the person reaches the age of 21 years, whichever is longer3. The long-term nature of this management is due to the high risk of reinfection with group A Streptococcus in northern Australia. BPG injections are given at no later than 28-day intervals to maximise protective serum levels of benzathine penicillin. ‘Days at risk’ of recurrence are calculated as the number of days after day 28 that an injection is not received and the person is therefore susceptible to ARF4. Some children are prescribed a 21-day regimen if an ARF recurrence occurs on the 28-day regimen.
Physiological pain of the injections is assumed to be caused by high viscosity and the large volume of medication injected. Children who are prescribed the regimen face a long-term ‘repeated painful procedure’. Online guidelines from the Royal Children’s Hospital in Melbourne state that for procedural pain ‘it is often difficult to distinguish between pain, fear and anxiety’, therefore ‘the combination is often referred to globally as pain related distress’5. ARF is most often diagnosed in children, therefore managing pain related distress of the injections is a central component for care. Thoughtful attention to care plans with reference to strategies in the Australian guideline mean that individual patient management can be of high quality6. As most patients on the regimen in northern Australia are Aboriginal, with many having English as a second language, non-Aboriginal clinicians’ cultural understanding and health communication is a further requisite for good care.
Background
Laynhapuy Health Service is part of an Aboriginal Corporation initiated in 1985 with a vision to support Aboriginal clans living on their custodial lands, called homelands. The service provides health care for 20 very remote small homelands in Arnhem Land covering an area of 6500 km2. The health team includes an offsite general practitioner (GP) with additional qualification as a physician, one onsite, part-time GP, a long-term nurse-manager, two GP trainees, six nurses and 11 Yolngu (local Aboriginal) community health workers who reside onsite in homelands. Continuous and rotating health outreach by clinicians to the homelands is organised at weekly team meetings. Priority is given for homeland outreach where patients are due BPG injections to facilitate the 28-day penicillin schedule, along with other time-critical medical needs. At the end of 2019, Laynhapuy Health Service was managing 43 cases of ARF with regular penicillin injections.
Issues
Children experiencing severe needle phobia
The first case is an Aboriginal boy aged 7 years living in a homeland 114 km from the health service office, a 2-hour drive on an unsealed road. He had an unremarkable general medical history with normal growth data and full immunisation. He was diagnosed with probable ARF in August 2017 after presenting to the local health clinic with polyarthralgia involving both ankles, limp and diarrhoea. There was no history of fevers, sore throat or chorea but a history of recent skin sores. Examination of the heart, joints, skin and subcutaneous tissues was normal including no audible murmur. Vital signs were normal including temperature. Weight was 38.5 kg. ECG was normal but 2 weeks later revealed a prolonged PR interval that subsequently resolved. An echocardiogram was normal. The anti-streptolysin O titre was 420 U/mL and anti-DNase B titre 600 U/mL (upper limits of normal for his age 276 U/mL and 499 U/mL respectively)3and C-reactive protein 15 mg/L (level required to fulfil Jones criteria in high risk settings is ≥30 mg/L)7.
The boy was hospitalised as per the Australian guideline for suspected ARF to facilitate diagnosis. His symptoms met the revised Jones criteria for a diagnosis of probable ARF in a high-risk population3,7: one major criterion (polyarthritis) and one minor (first degree heart block) plus evidence of streptococcal infection. He was commenced on BPG (1 200 000 units (900 mg) for >20 kg child) by intramuscular injection once every 28 days, which will be required until age 21 years (for a total of 14 years) according to the guideline3 to prevent ARF recurrence and development of RHD.
The boy experienced severe distress with the injection regimen such as crying out for help. His distressed responses continued despite use of recommended strategies: pressure to injection site, ice to the site, use of a vibrating icepack (Buzzy®) rewards-based therapy, talking calmly, including other family members in his care, and at times use of concurrent local anaesthetic. Additionally, he experienced buttock pain the day following the injection, which was not relieved by oral paracetamol. His continued needle phobia and high distress in turn distressed his parents, the community health workers and nurses.
The Laynhapuy clinical team discussed the boy’s case to determine availability of further options. Although all recommended strategies were being used to alleviate the boy’s severe distress, they were concerned as a group that it was not adequate in this instance. In a collegial approach, the team discussed analgesia commonly used to manage strong pain and/or severe distress in hospitalised children (such as ketamine, nasal midazolam or fentanyl and nitrous oxide) and considered how the remoteness of their practice impacted potential use of such pharmacological interventions. The boy’s family were also keen to try something new to address the severe trauma.
The director of anaesthesia in the tertiary referral hospital (Darwin) was contacted for advice. The recommendation of oral clonidine was made as a safe and effective option for children experiencing procedural trauma. Oral clonidine is an alpha-2 adrenergic receptor agonist with broad cardiovascular and central nervous system effects in children and adults, including analgesia and sedation. Clonidine produces sedation by decreasing sympathetic nervous system activity and the level of arousal due to activation of central nervous system alpha-2 receptors. The result is ‘a calm patient who can be easily aroused to full consciousness’8. Use of clonidine has not been reported in primary healthcare settings locally or internationally for children prescribed the BPG regimen; however, it is increasingly used as an adjunct in anaesthesia and to reduce postoperative pain in children9,10 as well as with good effect for a range of other conditions such as sleep and behavioural disorders11 and secondary dystonia12.
Under guidance of the director of anaesthesia, a starting dose of 3 µg/kg given 45 minutes prior to the penicillin injection and a 2-hour observation time was planned. A dose of ibuprofen 10 mg/kg was recommended to be given concurrently to assist with muscular pain post-procedure. If the child was stable and rousable after 2 hours and awake enough to protect the airway, then they could be discharged home. The health team decided to commence the first dose of clonidine with the boy as an inpatient in the regional hospital in January 2018. The starting does was just under 3 µg/kg (100 µg for child weighing 38.5 kg) along with oral ibuprofen and paracetamol. These were given 45 minutes prior to the penicillin injection. The episode was assessed as successful: the boy declined to have the injection in the buttock but accepted the thigh. He watched the needle throughout the procedure. Blood pressure, respiratory rate, level of consciousness and emotional state were monitored for 3 hours with no adverse events being recorded.
The next phase was to deliver the new strategy in the remote homeland setting with no doctor present and the clonidine being administered by experienced nurses. The nursing team created a procedural counselling protocol specifically for use with the clonidine strategy (Box 1). This comprises six elements as sourced from the Royal Children’s Hospital, Melbourne clinical nursing guideline for procedural pain management5.
The homeland dose of clonidine was reported to cause mild sedation with relief of the boy’s anticipatory anxiety; he was calm prior to and during the injection. Sedation was no longer evident with repeated dosing. Anxiety was greatly reduced in the boy although he continued to show overt signs of emotional relief post-injection. Six months into the new clonidine strategy, the boy had just one ‘day at risk’ compared with 4 days at risk prior to the strategy. ‘Days at risk’ of recurrent streptococcal infection/ARF are counted as every day after day 28 that a BPG dose is not administered4. After 18 months on the strategy, clonidine was ceased due to the boy’s decreased fear and anxiety around injections. He continues to cope well with the regular injections with good adherence: in the 12-month period after ceasing clonidine, 4 days at risk were recorded, attributed to patient movements over the school holiday period rather than to fear of needles.
Two other children aged 9 years and 8 years on the BPG injection regimen were subsequently diagnosed with pain related distress and were commenced on the clonidine strategy. The second child commenced the clonidine strategy in the local clinic rather than in hospital and at the time of writing had been receiving clonidine for 6 months with effective reduction in anxiety, no adverse effects and complete adherence to the penicillin regimen. The third case to commence the strategy was unsuccessful. This failure was attributed to starting clonidine in the emergency department of the regional hospital in rushed circumstances without procedural counselling. This third child has temporarily stopped the penicillin regimen (with oral penicillin substitution in the interim) and will recommence as soon as feasible with a new injection care plan.
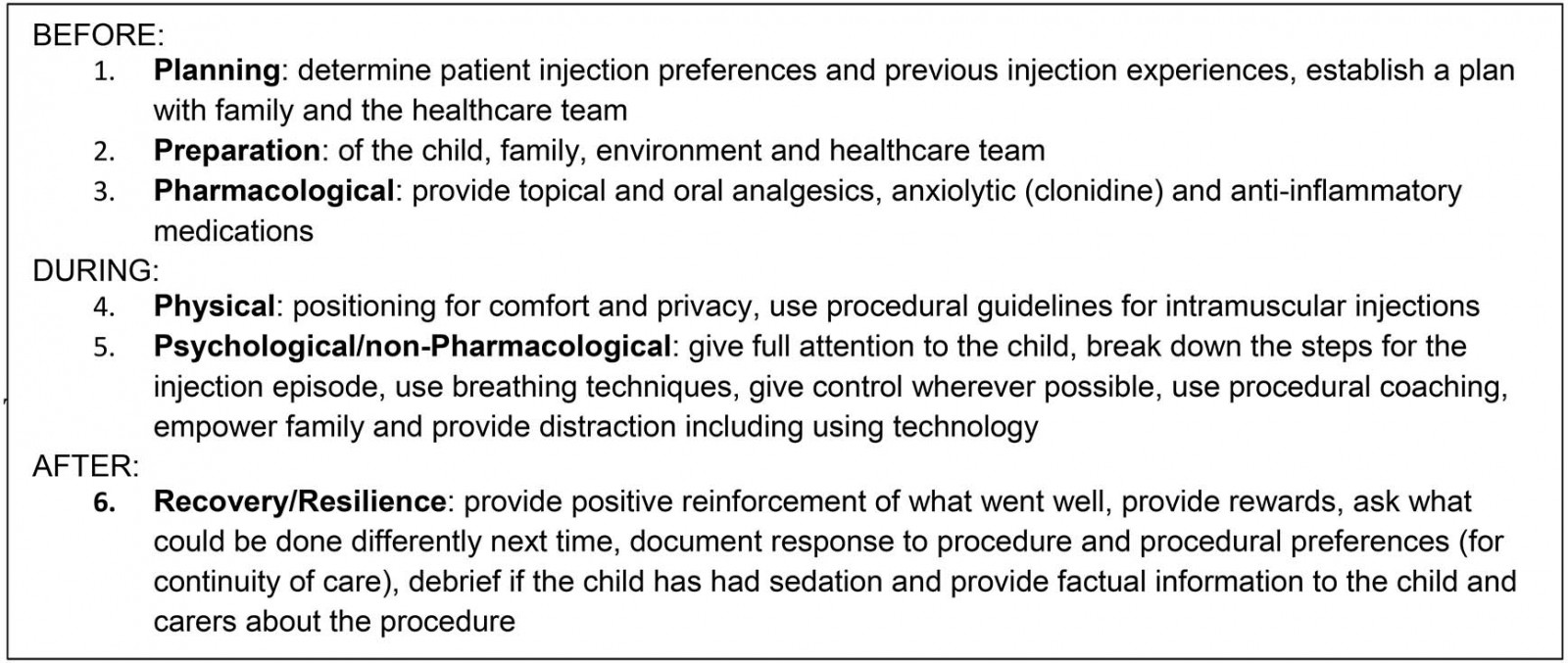 Box 1: Procedural counselling protocol specifically for use with clonidine strategy for long-acting benzathine benzylpenicillin G administration.
Box 1: Procedural counselling protocol specifically for use with clonidine strategy for long-acting benzathine benzylpenicillin G administration.
Health service protocol and new Australian guideline
In consultation with the director of anaesthesia, the health service completed an in-house protocol for prescription and administration of clonidine in cases of pain related distress in children on the penicillin regimen. Administration of clonidine in this health service is typically carried out by two nurses, or one nurse and one Aboriginal health practitioner, who are trained in paediatric basic life support, in the absence of a doctor. Monitoring was consistent with the Australian safe practice for administration of sedation13. The children in this case study had probable and definite ARF with no cardiac damage.
Due to insights gained from this case study, authors were invited to contribute to the third edition of the Australian guideline for prevention, diagnosis and management of acute rheumatic fever and rheumatic heart disease published online in February 20203. We refer readers to chapter 10 of the guideline and pages 179 and 180 specifically on clonidine use for BPG injections. The new guideline alerts practitioners to possible adverse effects of clonidine, which include hypotension and atrioventricular block, necessitating discussion with the child’s specialist in cases of RHD prior to prescribing clonidine.
Lessons learned
In determining what enabled improved and effective care for the children experiencing procedural trauma associated with regular painful injections in a very remote setting, several factors are apparent:
- Being an Aboriginal Community Controlled Health Organisation with internal continuous quality improvement initiatives provides freedom to explore and initiate new clinical strategies for better care.
- Stable clinical staffing due to supportive health service design and work environment enables staff to function at optimum levels, which increases work satisfaction, thus contributing to staffing stability.
- A collaborative approach to solving medical/social/nursing problems as they arise is important: weekly healthcare team meetings to plan and organise priorities, keep up to date with current knowledge/strategies and together determine best care.
- Individualised child-focused care is important as what works for one may not work for another.
- Sharing lessons learned and a patient’s individualised care plan with other regional health practitioners in primary healthcare and hospital settings is important given the likelihood that a patient may receive their BPG from other healthcare providers at times.
- Good planning for initial injections at ARF diagnosis needs to include procedural coaching, ideally with staff that children and adolescents already know. This may prevent or reduce pain related distress.
- Clonidine is a feasible option for reducing aversion to BPG injections in children and adolescents experiencing pain related distress, which may facilitate adherence to the long-term regimen and prevent ARF recurrences. However, for children with RHD, discussion with their specialist is required before prescribing clonidine.
Approaching repeated painful procedures in children proactively, informed by current best practices, means it is feasible for children and adolescents on the penicillin regimen and their families, as well as healthcare staff, to provide and receive optimum care within remote locations. Good adherence to the injection regimen reduces the overall risk of heart damage, which in turn reduces morbidity and mortality from RHD. Ultimately, eradication of ARF in Australia should be possible.
References
You might also be interested in:
2005 - Rabies surveillance in the rural population of Cluj County, Romania


