Context
Most health professions rely heavily on the clinician’s ability to perform competencies safely and effectively. Tertiary health professional education (HPE), continuing in-service education and accredited professional development, such as Advanced Life Support, all depend, at least in part, on the acquisition of discrete psychomotor skills that are underpinned by knowledge and a rationale, placing them in the context of professional practice1. Psychomotor skills are typically taught face-to-face (F2F) and mastery of these skills requires deliberate practice over time2,3.
The current novel coronavirus, COVID-19, has challenged the provision of F2F training for health professional communities across the world. Under advice to reduce physical gatherings in the hope of reducing transmission of the virus, many HPE activities and courses have either been cancelled or transferred to online media. The disruption extends to online courses that include intensive training or residential schools. In the chaos of course conversion, the risk to HPE is that skills education is too hard in this context.
Skills training for health professionals based in regional, rural and remote locations has traditionally come at a cost. Regional, rural and remote clinicians and students often travel significant distances to large regional hubs or urban centres to participate in F2F skills-based training, which has costs for both the individual and the supporting health service through lost wages, travel time, the cost of travel and accommodation, and extended periods away from work and family4. If HPE can deliver robust and reliable skills training through virtual means during COVID-19, the long-term improved access for regional, rural and remote clinicians and learners will offer significant relief and benefits for them and their communities.
The global implications of COVID-19 for HPE are significant. Professional registration renewal, tertiary course accreditation and ongoing professional development are all implicated. There is an opportunity, however, to reconsider the foundations of skills-based training, and consider new ways to enable it amidst the current restrictions, as well as beyond. This commentary explores the foundations of psychomotor skill education and development, and solutions to this complex problem.
Issues
What is involved in learning new psychomotor skills?
Various models have described the continuum of development from novice to expert5-8, and numerous teaching models have existed to guide educators in the process of teaching skills1,9,10. In the context of learning new psychomotor skills, it should be self-evident that no single teaching session will actuate the cognitive, cerebral and muscular markers of reliable, expert performance and, as such, models of teaching that claim to culminate in autonomous practice immediately following education are questionable11.
Learning psychomotor skills is complex12. First, correct chronology requires recall of the skill’s performance principles, underlying basic science and action order. Second, many skills demand specific strength and dexterity, often unparalleled in daily life. For example, controlling a needle driver while suturing, grasping a laryngoscope and opening a glass medication ampoule all feel awkward for novices as the motor outputs demand activation of specific motor cortical tissue and efferent (motor) neuron pathways13. Third, a health professional’s hands, afferent (sensory) pathways and sensory cortex must all become increasingly equipped to perceive and interpret sensations to guide the progressive development of competence14. Finally, neuroplastic and myoplastic development occurs over time with intentional, reflective and guided practice to build corporeal literacy: a bodily knowledge possessed by a health professional. This corporeal literacy informs insights such as, ‘this airway doesn’t feel right …’, ‘I saw flashback, but I’m not sure about that cannula …’, or ‘this bandage isn’t sitting properly …’. Health professionals easily relate to the struggle with these facets of skill development. Designing online skill education that acknowledges these complexities will be an unfamiliar task for many health professions educators; however, the theory and education principles already used in F2F teaching remain applicable to online education. Embracing creative licence to think differently about skill education might be all that is needed to rethink education online.
Rethinking online skill education
Videos that demonstrate how to perform a skill speak to the foundational layer of Miller’s pyramid15,16, to know. Attentively watching an action17 or listening to its description18 activate mirror neurons, which are the precursors to motor neurone activation. Thus, actively watching and listening will excite and strengthen the precursory neural pathways required to physically perform a skill. The use of videos is not, however, a silver bullet. While they are a convenient and reusable resource, their use should facilitate active learner involvement19. The use of video examples may imply that skills can only be correctly performed one way, thereby neglecting the natural in-practice variation encountered by health professionals. Supraglottic airway insertion, for example, need not be a rigid procedure in pre-hospital medicine, so long as the aim of rapidly rescuing an airway is achieved20. If video review is directly followed by a skill competency session, the motor development and sensory expertise required by competent health professionals are neglected, as learners are expected to leap from seeing a skill to performing it competently. Vygotsky’s zone of proximal development21 reflects the gradual development of mastery, whereby the learner progresses to content which uses foundational previous learning. In this zone of proximal development, content is sufficiently stimulating to prevent boredom, but not so much of a leap that it disengages learners through cognitive overload22. To employ Vygotsky’s principle, online media should guide a learner to develop step-by-step, allowing them to continually reflect, generate new meaning for themselves, incorporate adaptations, and reorganise previously held assumptions and lessons.
Videos can be engaging and immersive if each learner in a group is tasked to narrate different aspects of video skill performances. This shifts the learners into Miller’s knows how level. For example, one learner might narrate the clinical reasoning pathway, another the sensory aspects, another the patient or family communication, and so on. Furthermore, videos depicting skill application across a range of patient needs and presentations allow students to develop a repertoire of acceptable skill adaptation, and seek learners’ critique and reflection of what they witnessed. Videos requiring the learners to indicate their choice or recommendation at certain paused intervals prior to the video’s continuation may be another strategy to engage students, using questions such as ‘What would you do next?’ or ‘What provisional diagnoses would you shortlist for this case and why?’. The use of video in these ways can draw the learner into the learning and out of passivity.
Another well-established strategy to learn and practice new psychomotor skills in professional sport23 and surgical training24 is imagery. Imagery is not simply visualising a motor task, but rather recruiting all the relevant senses to mentally practice skilled performance in order to build motor and sensory fluency.
The transition to the next level, showing how, demands even more planning and creativity. The example in Box 1 presents one example of how skill training might continue during COVID-19, rather than come to a standstill, and can be adapted to tertiary, in-service and professionally accredited training. It employs a model of distributed or spaced practice25,26 by training skills remotely over an extended period rather than at a single intensive workshop, and it graduates learners methodically up Miller’s pyramid.
This solution allows learners to develop motor and sensory function over time, supporting the co-development of knowledge (to know), rationale (to know how), and practice (to show how); and provides evidence to external accreditation bodies that declarative and procedural knowledge can be applied by graduating students who are defensibly worthy of accreditation. There are many similar examples to that in Box 1. Health professional educators in all contexts have an opportunity and responsibility like never before to innovate and test new ideas in HPE for the medium- to long-term.
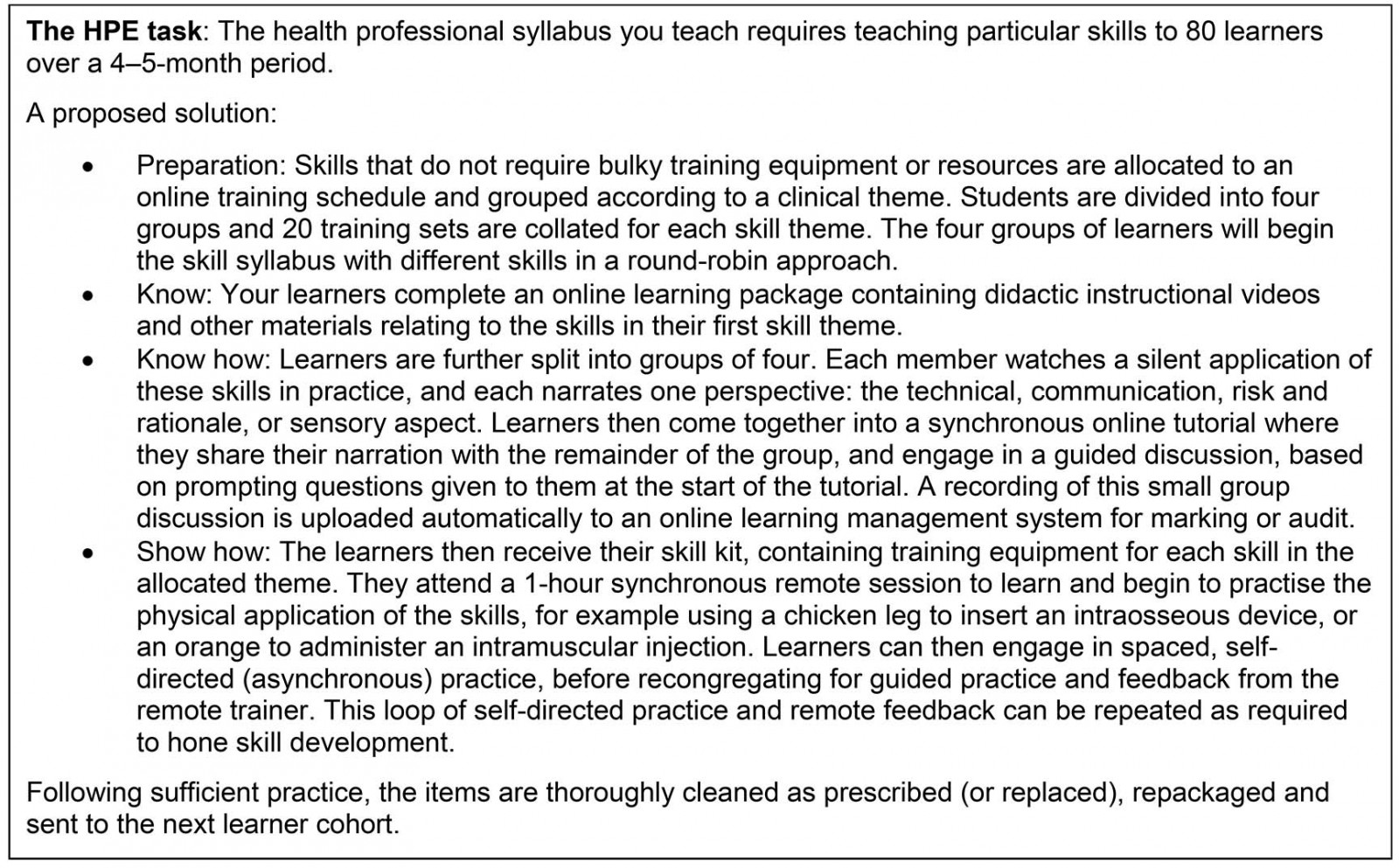 Box 1: An example of online skill training in health professions education.
Box 1: An example of online skill training in health professions education.
Clinging to face-to-face skill teaching
During F2F skill training, the four facets of psychomotor skill development merge organically, through demonstration and explanation (chronology), guided practice (motor) and prompts to reflect on how the skill feels to the learner (sensory), all of which scaffold a trajectory of cognitive, associative and autonomous learning, towards an embodied, corporeal literacy. The shift from F2F to online skill education creates obvious barriers for teaching and learning psychomotor skills. For example, even if learners are able to access training equipment remotely and participate in online learning, educators may not easily be able to view the learners’ skill performance from the best perspective in order to guide development and correct errors, thus mistakes may be inadvertently reinforced through omission of correction when required.
Early solutions to the risk of continuing with F2F teaching centred around health screening27 and deferral of weekly practical sessions to periods of intensive teaching and learning. All are problematic in their own way and signal the reluctance to enable skill development by means other than in person, F2F.
Student and tutor health screening standards typically consist of documenting a mandatory temperature check and self-reporting other symptoms (sore throat, cough or myalgia). Only students who are afebrile and declare no symptoms can then participate in the session, while screening documents are filed for future reference. Aside from legislative requirements for education (ie non-clinical) organisations to securely store these confidential health records, this approach has several other flaws, including:
- disadvantaging students who become ill by excluding them
- incentivising deception through antipyretic medication administration to mask symptoms, or withholding symptom declaration in order to complete coursework
- failure to identify asymptomatic carriers through temperature checks and symptom questionnaires28,29
- failure to address the risk of fomite transmission via equipment in contact with people outside the learner cohort
- continuation of group gatherings (of learners) in opposition to the principles of social distancing.
Deferring skills-based education to intensive blocks or residential schools is another educational response. Such an approach may convert eight 3-hour practical classes over the course of a semester to an intensive period of three 8-hour days, for example, following the resolution of the current pandemic30. Currently across the world, however, there are unclear and highly variable characteristics of the virus’ first wave, so education institutions planning for future intensives are unable to reliably anticipate the potential timing and impact of a second or subsequent waves, as has been seen in other pandemics31. Furthermore, the construction of muscular and neuronal pathways to support organised recall, perception, stamina and fine motor control require time to develop, a luxury often denied by intensive instruction. Experiential learning cycles32 require spaced or distributed learning, which is known to better support recall and practice25,26.
Learning psychomotor skills cannot be considered akin to a Lamborghini’s feat of 0 to 100 km/h in 2.9 seconds. Rather, skills acquisition requires a steady, measured pace of development. To teach, practice, assess and document the competency in rapid succession over an intensive one- or two-day period neglects what we know about skill retention and attrition, and motor learning.
The current pandemic has prevented much F2F skills training, but it does not remove the need for practitioners to update their skills, reduce the need to access accredited training, nor waive the principles underpinning accreditation.
Lessons learned
Educators are urged to review relevant pedagogical theories and principles, and to consider creative ways to apply these to online learning to ensure the continuation of skills education. The experiential learning cycle29 can be engaged through means other than F2F practice, including watching, listening and guided visualisation. Whether a learner can enter the experiential learning cycle vicariously (without physically attained ‘concrete experience’) may be debated. As neurobiology has established that neuronal responses can be achieved without physical interaction, however, HPE may question whether traditional F2F teaching is the only way to effectively teach psychomotor skills.
Proficiencies in discrete skills are building blocks for skilled practice5, which is the focus of the next article in this series. There are many more ways that creative HPE activities can effectively teach psychomotor skills remotely, and resolution of COVID-19 need not signal the end of creativity in this realm. If educators establish defensible online teaching practices, regional, rural and remote learners and urban-based learners will experience a new era of equitable access to education and professional development.