Context
Tasmania is a small island state, located 240 km from the southernmost part of mainland Australia. North West Tasmania is a rural and remote area of geographically dispersed communities, classified as Modified Monash Model 3–71. There are smaller district hospitals in rural and remote sites, and two larger hospitals: North West Regional Hospital (NWRH) in the large rural town of Burnie, providing moderate complexity inpatient (160 beds) and ambulatory care services2; and 95-bed Mersey Community Hospital (MCH), in the large rural town of Latrobe, providing low-to-moderate complexity inpatient (95 beds) and ambulatory care services2. A statewide digital medical record means patient information can be accessed at all Tasmanian Health Service hospitals. North West Private Hospital (NWPH) is a 101-bed facility co-located with NWRH. The public health service commissions NWPH for birthing services for the region2. There is a heavy dependence on locum staff. For example, in 2014–15, 39% of the full-time equivalent medical staff establishment at MCH was filled by locums and 15% were locum staff at NWRH2. In March 2020, locum staff, as essential workers, were initially exempt from the COVID-19 14-day quarantine implemented across state borders. As escalation increased, exemptions were withdrawn, and many locum staff (medical and nursing) withdrew from contracts.
This article describes the decommissioning and recommissioning process undertaken at the NWRH site. The aim is to provide a foundation for site-specific adaptation to include in pandemic escalation plans in other regional and rural settings.
Issues
Within 5 days of the first healthcare worker infection with COVID-19 at NWRH, 14 more staff and patient infections were confirmed there1. A decision to take operational control of the adjacent NWPH was made to assist with outbreak management3. Seven days after the first healthcare worker infection, there were 35 confirmed cases including 26 healthcare workers and 9 patients or close contacts3. An initial containment strategy to isolate suspected or confirmed cases and furlough close contacts of the infected healthcare worker rapidly compromised hospital operations. Ten days after the first local case, it was announced the hospital site would close to undergo a deep clean.
There are no frameworks to guide decommissioning, cleaning and recommissioning processes for hospitals in pandemic planning. Health sector response plans for preparation, activation, escalation or de-escalation and recovery response phases focus on management for predicted surge in patient demand and care4. Nevertheless, ward and whole hospital closures have previously been required to contain infection5-7. The efficacy of ward closure only in outbreak management in healthcare settings is uncertain, and there are ethical and legal considerations about providing ongoing patient care where known transmission is occurring8. Containment measures during this pandemic continue to develop9,10. In comparing containment in three hospitals in Singapore during a severe acute respiratory syndrome outbreak, Gopalakrishna and colleagues concluded that, to avoid hospital closure and quarantine of all staff, early outbreak detection with rapid identification of the infection cluster and a complete list of contacts is required within 48 hours7. It is reasonable to propose that many longstanding weaknesses in rural health services, such as a lack of specialists (including infectious diseases physicians) and health workforce shortages, make regional and rural services particularly vulnerable.
Hospitals are complex organisations that are not designed to be left uninhabited. High-risk infrastructure such as kitchen, medical gases and fire detection systems; as well as high impact assets such as pharmacies, patient information storage, mortuaries and security systems require preparation and protection. Additionally, terminal cleaning must be a robust process to both rid the infection and restore the confidence of staff and the community in the safety of the healthcare environment. Openly planning for a possible hospital closure amid a crisis may be compromised by the need to maintain confidentiality of sensitive information prior to formal announcements at the government level. Rapid development of workable plans to decommission an entire hospital site within 48 hours of the announcement due to diminishing staff numbers is not ideal, and there may be few resources left to accomplish this.
The very practical nature of this significant task overlaid the very human reality of a community and workforce deeply impacted and exhausted by the COVID-19 outbreak and its sequelae.
Decommissioning
As NWPH had also been closed due to transmission across from NWRH, the hospital was included in the closure, cleaning and recommissioning process. A small management group on the ground made an initial plan to identify required tasks and source additional personnel willing and able to assist as a work party on the prescribed day. Formal waivers to be on site during decreed staff quarantine were required.
The decommissioning plan focused on several components/phases (Fig1).
Staff and patient communications: All staff were directed to the formal announcement of closure, after which open discussion with all patients and their families was enabled.
Patient decanting: A medical review of each patient was conducted to determine those patients for discharge, those for transfer to MCH or, for those with medical goals of care exceeding the capacity of MCH, for transfer to a higher level facility. A medical physician performed the reviews to ensure clinical handover, then was also furloughed as a healthcare worker exposed to the NWRH site.
On the day of decanting, 2-hourly briefings to track progress and issues were attended by the work party to assign tasks, identify any emerging issues or safety concerns and track resolutions.
Patients for discharge Those patients who could be safely discharged into 14 days of mandatory home isolation were sent home and Public Health Services Tasmania notified for follow-up. Patient information packs were prepared, containing:
- a surgical mask for wearing outside of quarantine (to home or to medical appointments)
- instructions for home quarantine
- Contact information for Public Health Services Tasmania.
Those patients unable to be discharged to their usual residence but able to safely reside independently were found alternative accommodation.
Patient transport was provided by family members or staff as public transport services were disinclined to transport persons at risk of infection. Surgical masks were provided for these family members. Safe hygiene practices, including wipe-down of vehicle surfaces and hand hygiene, were emphasised.
Patients for transfer Most patients were sent to MCH. The ambulance service was engaged in planning, and patient transport requests were sent the night before. Due to the number of patients requiring transfer, and the need to clean the vehicles between each transfer, private providers were engaged. All staff wore full personal protective equipment, which was changed between patients, for patient transfer.
Patient belongings were packed into plastic bags and patient notes into an envelope for transport with each patient. Every patient was required to wear a surgical mask and perform hand hygiene prior to transfer. All patients at low risk of infection were transported first; those with higher goals of care were transported when an appropriate response for acute deterioration at the receiving facility was ready. All patients with confirmed COVID-19 were transported last. Medical staff remained on site at NWRH to attend to any deterioration in condition of patients prior to transfer.
Patient privacy Given the publicity surrounding the outbreak, media were endeavouring to capture images of the closure. To protect patient privacy, tarpaulins were erected as screens at the immediate decanting point, and security ensured media maintained their distance.
Regional emergency response: Ambulance redirect to other hospitals commenced during decant and remained in place until the temporary emergency department was running. Urban hospitals were briefed to receive regional transfers. A helicopter was located at the hospital for urgent transport.
Signage and communication: Road signs advising of temporary hospital and emergency department closure were placed on highways, redirecting those who required healthcare assistance to alternative facilities. Media outlets provided public messaging about how to access services during interim closure.
Securing of the facility: As the facility’s usual contracted security service had been furloughed, another contractor was engaged to provide continuous security of the external perimeter. Security video was redirected to the new contractor. Swipe-card access was suspended for all non-essential staff. All keys were returned to the incident management team assigned to cleaning the facility.
Drug fridges, heating, cooling, and food fridges already linked to the electronic/remote monitoring system were reconfigured for remote monitoring.
Ongoing outbreak management: All staff who had worked during the period of the outbreak, and their immediate household, were sent into mandatory quarantine, defined as 14 days from the date of the last family members’ contact with the facility. Staff unable to quarantine at home were provided alternative accommodation. Public Health Services Tasmania assumed the responsibility for conducting daily checks of quarantined individuals and contacts and providing relevant advice.
Screening clinics were increased, with drive-through clinics established within 48 hours of the hospital closure.
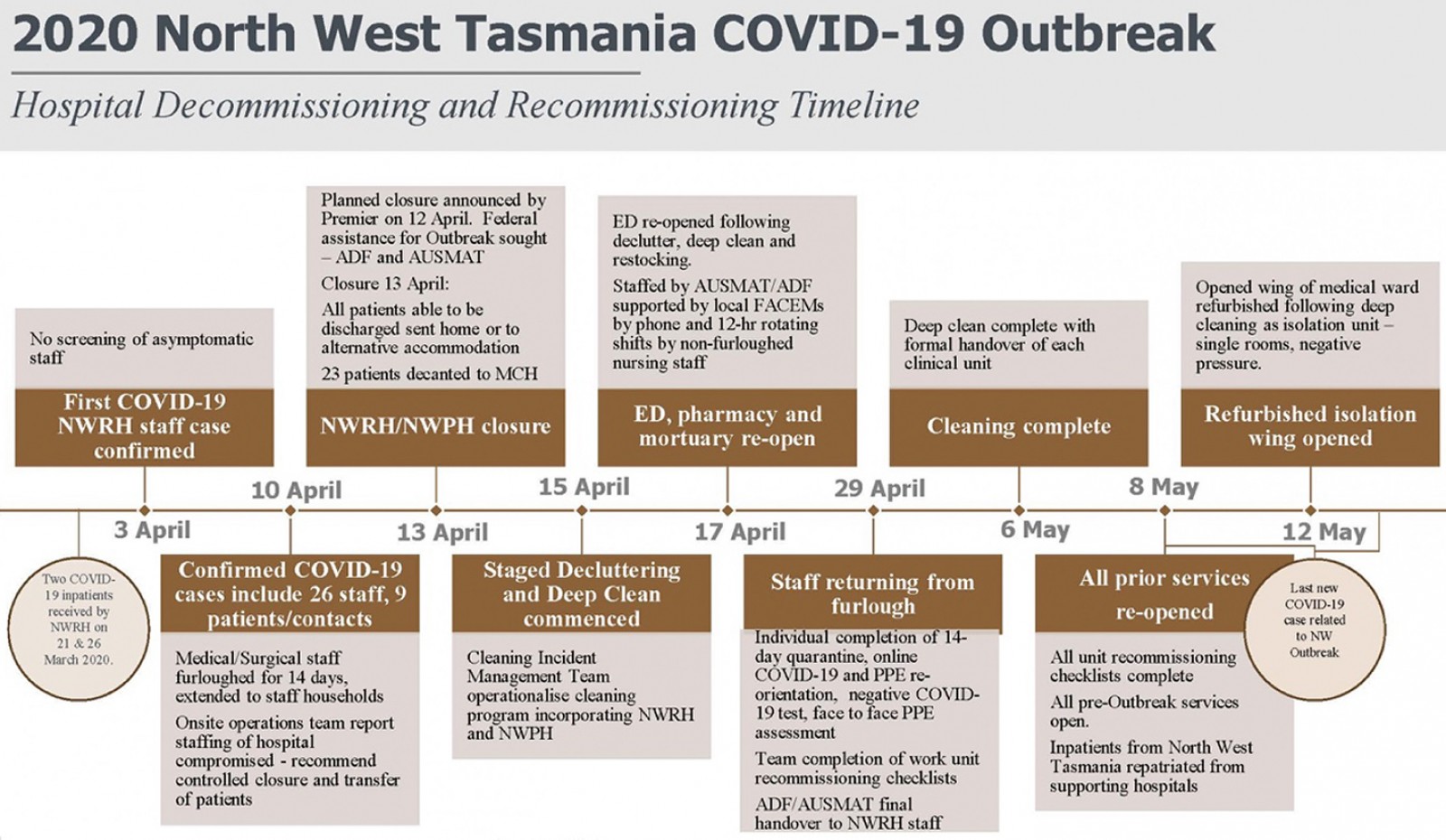 Figure 1: North West Tasmania outbreak decommissioning and recommissioning timeline.
Figure 1: North West Tasmania outbreak decommissioning and recommissioning timeline.
Facility preparation for cleaning and recommissioning
In parallel with decanting, preparations were made for decluttering and cleaning (Fig1), including:
- preparation and use of a checklist to guide disposal of consumables (open packaged items, disposable curtains), items that could be preserved but stored, items for removal (signage), and clearance of horizontal environmental surfaces
- storage and security of medications
- security of patient ward files and removal of patient information from whiteboards
- powering down of electronic devices
- removal of perishable items from kitchens
- diversion of meal delivery services to a supporting hospital
- collection and storage of unopened personal protective equipment
- transfer of switchboard services to a local receiving hospital
- use of an authorised script for switchboard operators to provide consistent messaging to callers
- confirmation all medical gases were off and secure
- confirmation that fire panel notifications would be automatically received by the local fire station
- planned collection of management laptops, web cams, mobile internet dongles and headsets to enable quarantined staff to work from home (not achieved)
- provision of a substantial and ongoing supply of personal protective equipment, cleaning equipment (trolleys, mop heads and handles, cleaning cloths), clinical waste bags, alginate bags for declutter and decanting scrubs and cleaning chemicals to prevent delays in cleaning. This required:
– consideration of additional workplace health and safety requirements
– liaison with waste contractors to establish new processes, resources and collections to manage the additional clinical waste (All COVID-19 waste was treated as clinical by the contractors.)
– notification to laundry services of the increase in cleaning items (mops, rags scrubs) and agreement of a 24-hour turnaround
– communication with linen contractors to ensure their needs were meet for returning contaminated linen to protect their site, staff and other community customers (All linen was treated as contaminated and placed in alginate/dissolvable bags.) The 5-day service was increased to a 7-day service for this period
- shutdown of non-essential services and equipment and preparation of risk assessment of shutdown for recommissioning engineering services.
Establishment of a cleaning incident management team: An incident management team was established to operationalise a cleaning program supported by the infection prevention and control (IPC) team, comprising IPC clinical nurse consultants and an infectious disease physician. Because the staff hospital cleaners were furloughed, personnel were contracted from elsewhere, many of whom were not familiar with cleaning a healthcare facility. Phone support was provided to guide them to on-site resources such as trolleys and vacuum cleaners. Donning and doffing stations were set up in various areas of the hospital based on the staged plan. The IPC team, boosted by non-furloughed IPC resources, led the cleaning and disinfection that was required for the facility. This included:
- education and training for all personnel undertaking the environmental cleaning on transmission of infection, hand hygiene, respiratory hygiene, appropriate use of personal protective equipment and principles of cleaning (using Chlor-Clean – a 1000 ppm chlorine-based, hospital-grade disinfectant11) and assessment of cleaning
- supervision of environmental cleaning protocol and program, with worksheets to track:
– the ‘terminal’ clean of all clinical and high-risk areas
– cleaning of non-clinical ‘low-risk’ areas focusing on horizontal surfaces, floors and high-contact areas
– steam-cleaning of all soft furnishings and carpets
- assessment by visual inspection and application of the fluorescein-gel assessment framework12.
A cleaning staging plan detailed the order and estimated timeframes for decluttering, cleaning and recommissioning to inform the staged reopening of services.
Recommissioning services
Recommissioning included all physical, human and process-related elements required to safely reopen a service.
Regional emergency service: Paramount in consideration of closure was the need to establish an emergency medical facility for the rural and regional community as soon as possible13. A combined Australian Defence Force and Australian Medical Assistance Team staffed the hospital’s emergency department as soon as it was cleaned. (A field hospital may be a preferable option.) Collaboration with these teams commenced alongside decommissioning, initially by virtual communication means such as Zoom. Thereafter, two non-furloughed nursing staff members undertook alternating 12-hour shifts to work with the visiting team for the duration of their duty, and local emergency medicine specialists alternated telephone on-call duties to provide continuous support. All patients requiring further clinical management were transported to higher level facilities by helicopter or road. The Australian Defence Force and Australian Medical Assistance Team remained on site until the usual emergency department staff returned from furlough to resume work.
Support services: A skeleton staff of radiology and pathology service providers supported the emergency response through modified off-site services until onsite services could resume. IT personnel organised access to all required IT systems, and training was provided through a combination of ‘cheat sheets’, online training modules, and remote one-to-one training. Supply of personal protective equipment was confirmed, aligned with the IPC framework. Clear channels of communication were maintained with the ambulance service to ensure safe patient transport and care. Food delivery (sandwiches and cold items) was arranged by MCH, and hot food was ordered in for prolonged patient stays.
Pharmacy: The hospital pharmacy was re-established for medication supply.
Mortuary: As the only mortuary for the region, this area was a high priority for re-establishment. To enable cleaning, coronial release forms were expedited and commitment to early collection arrangements with funeral services confirmed.
Maternity services: Women from the region who were within 4 weeks of their birthing date had to relocate to the nearest birthing hospital, so resumption of this local service was prioritised.
Other emergency clinical support: The intensive care unit and operating theatre were the next order of priority to support emergency care.
Cancer services: Patients requiring cancer care had to travel to alternative facilities, so these services were next order of priority.
Recommissioning staff
Communications and wellbeing checks: Public Health Services Tasmania was responsible for checking and communications with all furloughed staff. Challenges existed in providing consistent and relevant information due to the rapidly changing situation. Question and answer fact sheets provided ongoing updated information to staff, such as:
- details regarding self-quarantine
- who in the family and/or household was required to quarantine and for what period
- alternative quarantine accommodation
- pay during quarantine
- arrangements for planned leave
- Workers Compensation pathway and requirements
- access to psychosocial support
- work-from-home arrangements.
Another challenge was the inability to support staff confirmed to be infected with COVID-19, given that this is confidential health information. Hospital managers were encouraged to maintain contact with all staff during the quarantine period to check on their wellbeing more generally and refer staff members to the employee assistance telephone service. A psychosocial plan implemented prior to the outbreak provided access to local mental health specialists for individual and group support.
A series of online staff forums was conducted with frontline workers to discuss preliminary understanding of the outbreak and actions being undertaken to improve the hospital response in preparation for return to work. Staff were encouraged to check facts, ask questions and air concerns.
Alternative accommodation: Staff in alternative accommodation were provided food or meal payments.
Staff training: Pandemic planning and preparedness requires staff to train and retrain in IPC. It was determined that all staff should complete a mandatory education package prior to returning to work to re-orientate to personal protective equipment. This online education package comprised e-learning modules on COVID-19, hand hygiene, videos demonstrating appropriate donning and doffing of personal protective equipment, and specific healthcare facility IPC COVID-19 protocols. The education was hosted internally and on an external server accessible to contractors. Computers were made available onsite on reopening for those staff without private access.
Staff were required to demonstrate appropriate donning and doffing of personal protective equipment for contact and droplet precautions prior to their first shift and to answer IPC questions. Ongoing compliance audits were introduced to provide timely feedback to staff about personal protective equipment use. Senior clinical staff volunteered as personal protective equipment guardians in each area to maintain the integrity of IPC frameworks and escalate emerging issues for IPC consultation.
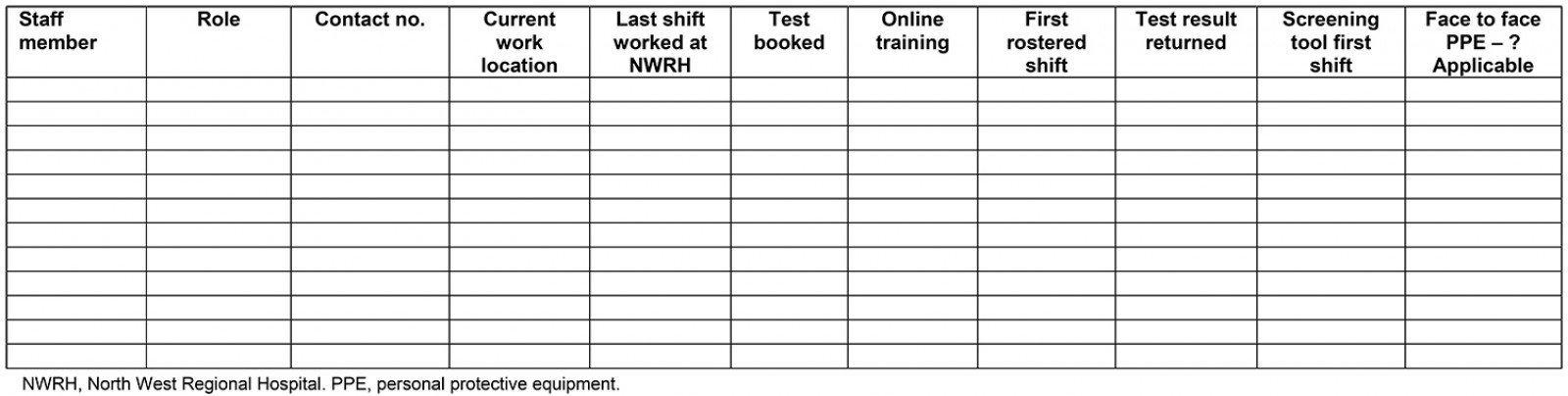
Staff clearance for return to work: A formal process of return-to-work signoff required evidence of completion of online education, personal protective equipment assessment and a negative COVID-19 swab taken at least 14 days after an individual’s last shift at the hospital. If the staff member had contracted the infection, they must have met PHS criteria for ‘release from isolation’ of two negative swabs within a 24-hour period following recovery before returning to work (Appendix I).
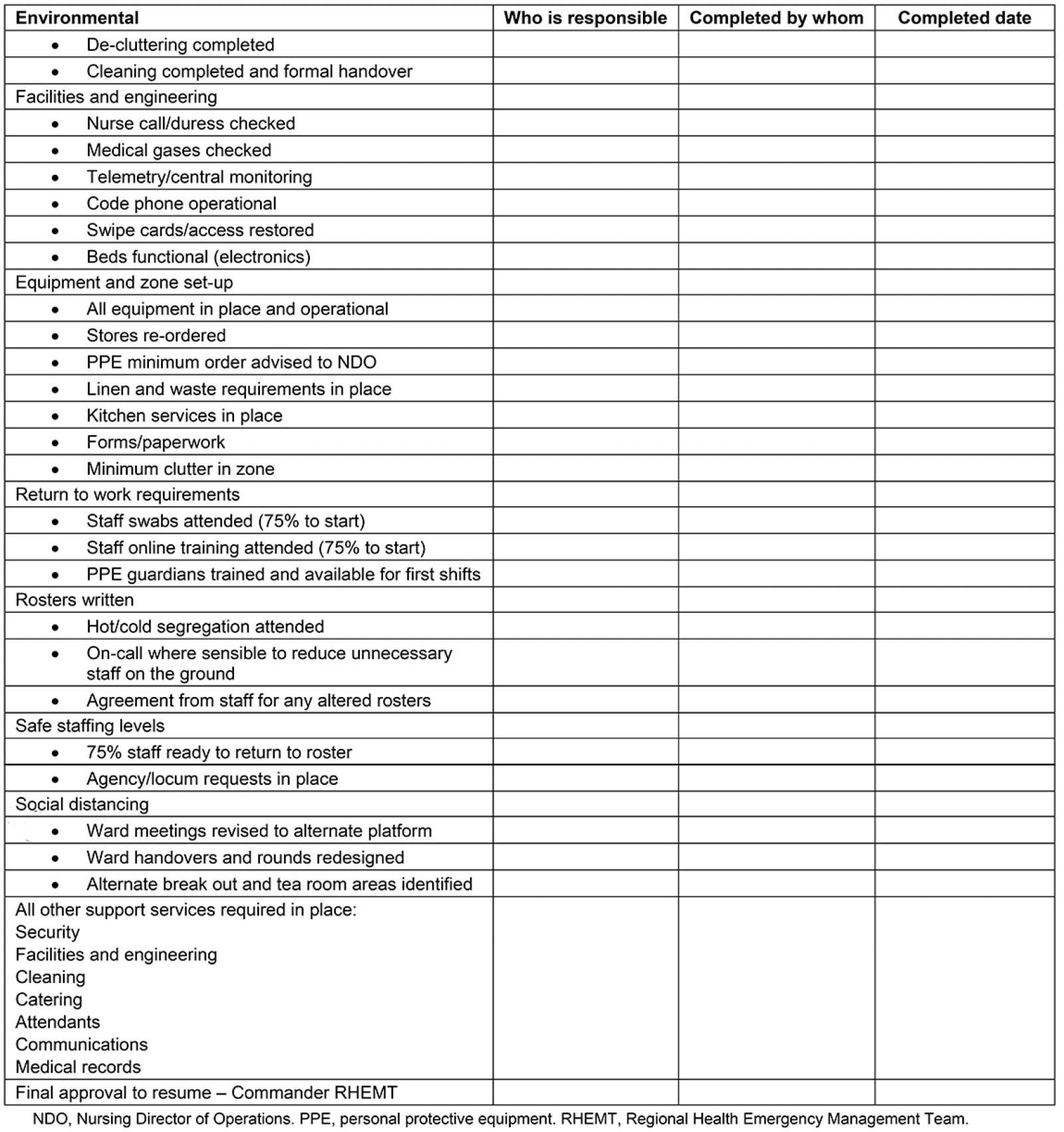
Recommissioning checklists
Staff returning to work re-established functional workspaces and completed a recommissioning checklist (Appendix II).
Repatriation planning (from supporting hospitals)
As soon as a clinical unit was deemed ready, local patients admitted to hospitals elsewhere were repatriated to NWRH.
Updating protocols
During the closure, information and procedure for COVID-19 related care changed, requiring review of local protocols with stakeholder engagement.
Lessons learned
The decommissioning and recommissioning processes undertaken in one rural hospital outbreak setting in Australia are described to assist other rural sites to identify, secure commitment from and prepare in advance the individuals and services needed. An early, planned response may preserve health service function or fortify a seamless closure and recommissioning, should that be necessary.
Early contract tracing and isolation is imperative in preserving healthcare services. Identification of trigger points for early ward containment and hospital closure should be part of health service pandemic response plans. In a rural setting, there are limited resources to implement such measures. Able external sources may be reluctant to become involved without prior preparation. Negative commercial and social media and stigma may further wither reserves. Regional healthcare services will need to be ready to support more rural or low-resourced facilities and accept additional patient load from diverted services.
A robust, connected, high-level command was essential in quickly securing the required authority to implement plans and action these with staff. During closure, staff coordinated the recommissioning from home, where internet service through the National Broadband Network is predominantly through wi-fi connection. Bandwidth was variable; audio-only communications were adopted at times to maintain connectivity. For rural and remote regions with satellite communications, maintaining clear communication links may be challenging.
The opportunities for further research are many. As the epicentre of an outbreak where the challenges experienced by staff are ongoing, it is hoped a focus of any research will be its contribution to rebuilding community and healthcare worker trust and confidence in managing essential health services for the region, as well as furthering knowledge about pandemic response in rural areas. The independent review3 has a broader description of the whole-of-service response.
Acknowledgements
The coordinated and cooperative response described was a collective effort of key individuals and teams at government and local level and the community of North West Tasmania. We acknowledge the staff who continued to work to provide patient care and reinstate essential services at the most trying of times, those staff who unwittingly contracted the disease, Ambulance Tasmania and the Australian Defence Force and Australian Medical Assistance Team who came to our aid unreservedly and were exceptional, and those staff at the receiving hospital required to stand up an unplanned response, provide ongoing care for patients caught in an unfolding tragedy, and contain the outbreak. We pay tribute to the patients and family members who bravely navigated the outbreak and closure beside us, some of whom have since died. We offer our learning in memory of these individuals.
References
You might also be interested in:
2014 - Dental practitioner rural work movements: a systematic review