Introduction
In 2008 the Medical Council of New Zealand recognised rural hospital medicine as having a distinct vocational scope of practice. Rural Hospital Medicine Fellows are suitably trained and experienced generalists, who take full clinical responsibility for a wide range of clinical presentations to rural hospitals1. Currently 26 hospitals fulfil the New Zealand Medical Council’s definition of a rural hospital2. One in four New Zealanders live in or near rural small towns, many of whom are served by this network of rural hospitals3. The New Zealand Division of Rural Hospital Medicine recognises three broad levels of rural hospitals: level one have visiting medical cover daily and on-call medical cover at other times; level two have onsite medical cover during normal working hours, and on-call cover outside this; level three have onsite 24-hour medical cover4. While all levels have acute inpatient beds, access to laboratory support varies from generally none onsite at level one, point-of-care testing at level two, to access to continuous lab support at level three. Radiology support similarly varies from offsite to periodic to continuous availability, and CT scanners are not common, even at level three. Some level three hospitals have limited specialist cover (eg in emergency or internal medicine). Staffing levels, both medical nursing and allied, are proportionately lower in levels one and two, and similarly services provided vary, although in no fixed formula. Rather, rural hospitals generally represent an appropriate response to the varied needs of rural communities based on their geography, and social and cultural composition.
This study was designed to explore the use of procedural sedation and analgesia (PSA) within New Zealand rural hospital settings. PSA can be defined as a ‘state of drug-induced tolerance of uncomfortable or painful diagnostic or interventional medical, dental or surgical procedures’5 and is commonly used as an adjunct to a variety of emergency and urgent medical and surgical procedures.
The aims of this study were to determine patterns of PSA use including indications, equipment and agents commonly used by rural hospitals, assess the logistical and medical staff support available for PSA use in rural hospitals and to determine whether current professional guidelines support rural PSA practice.
Methods
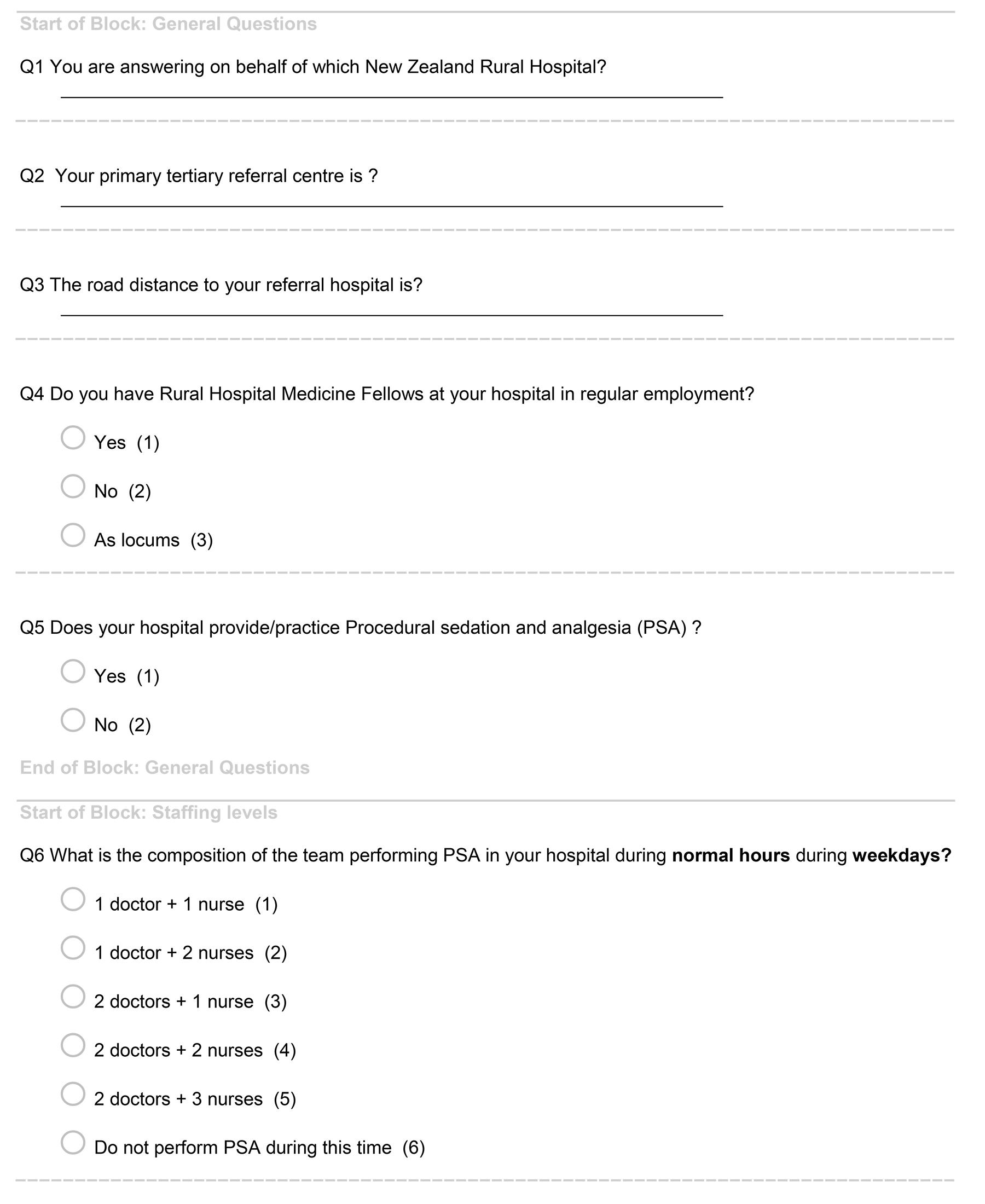
The New Zealand Rural Hospital Research Network6 is an informal network of researchers within the 26 rural hospitals in New Zealand. From this network, 17 rural hospitals out of the 26 had a research contact person available and were invited to enrol in the study. Research contacts were either clinical directors or practising clinicians at the hospital. The study was conducted electronically over 2 weeks in February 2018, utilising a University of Otago Qualtrics survey tool.
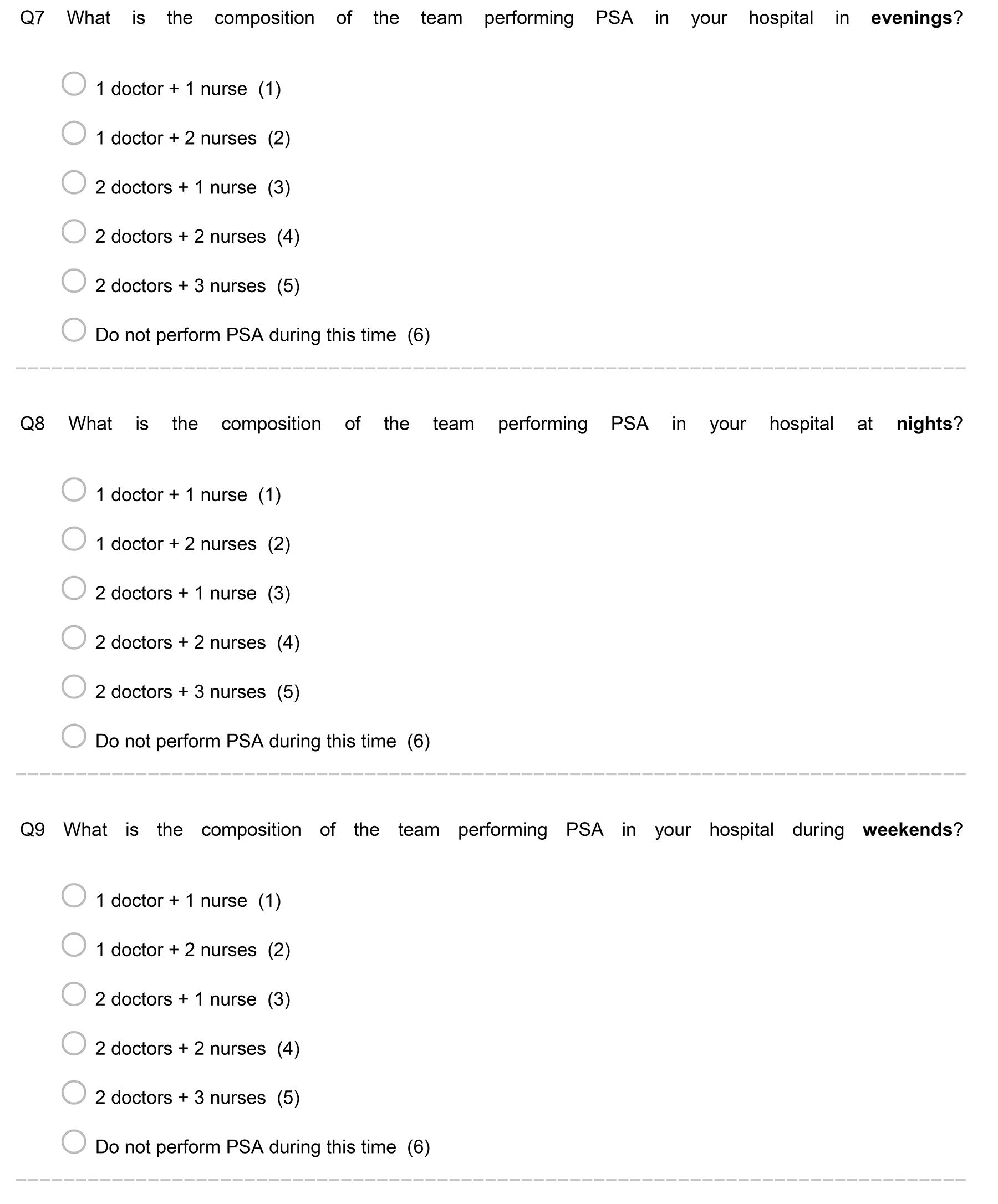
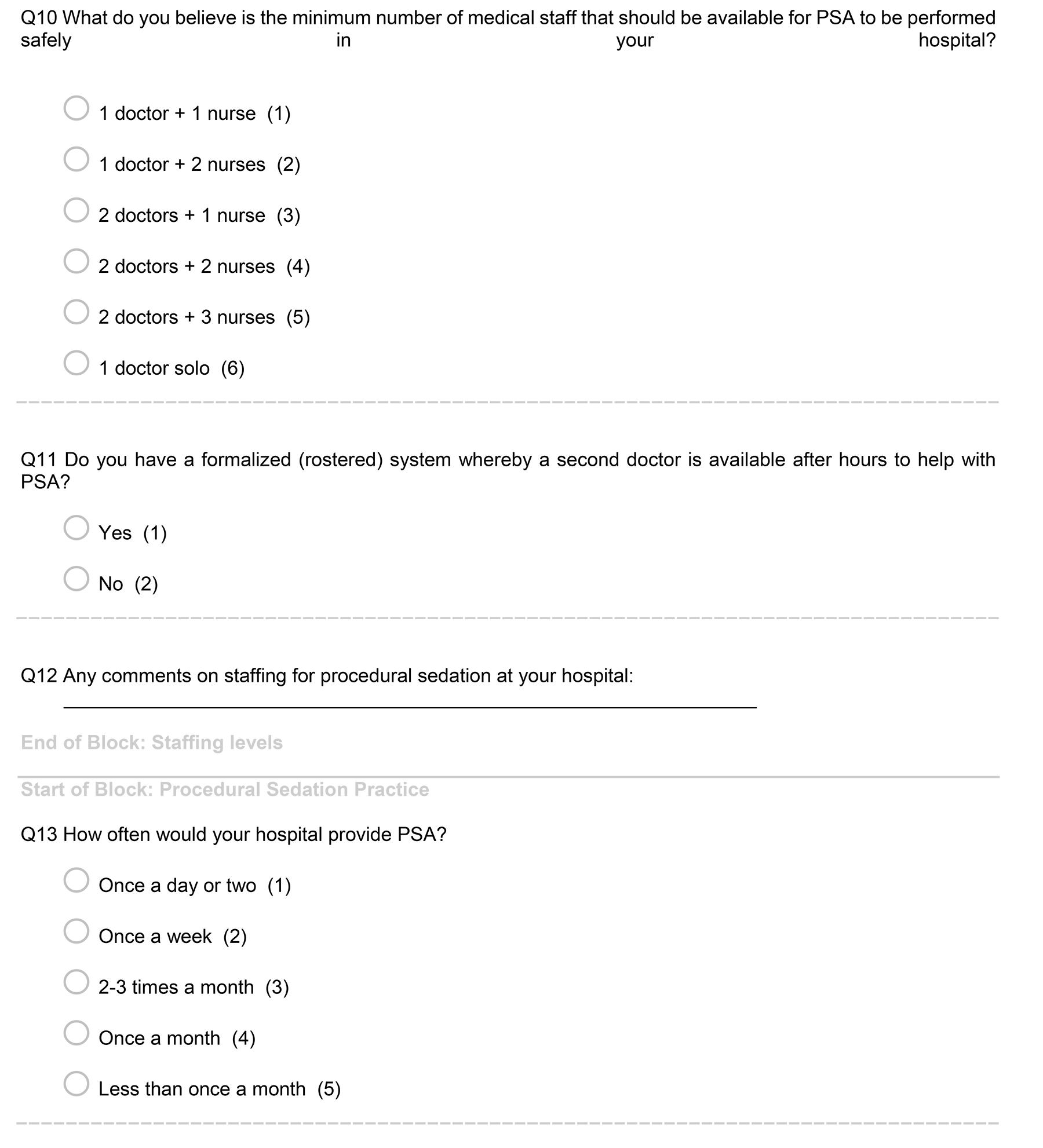
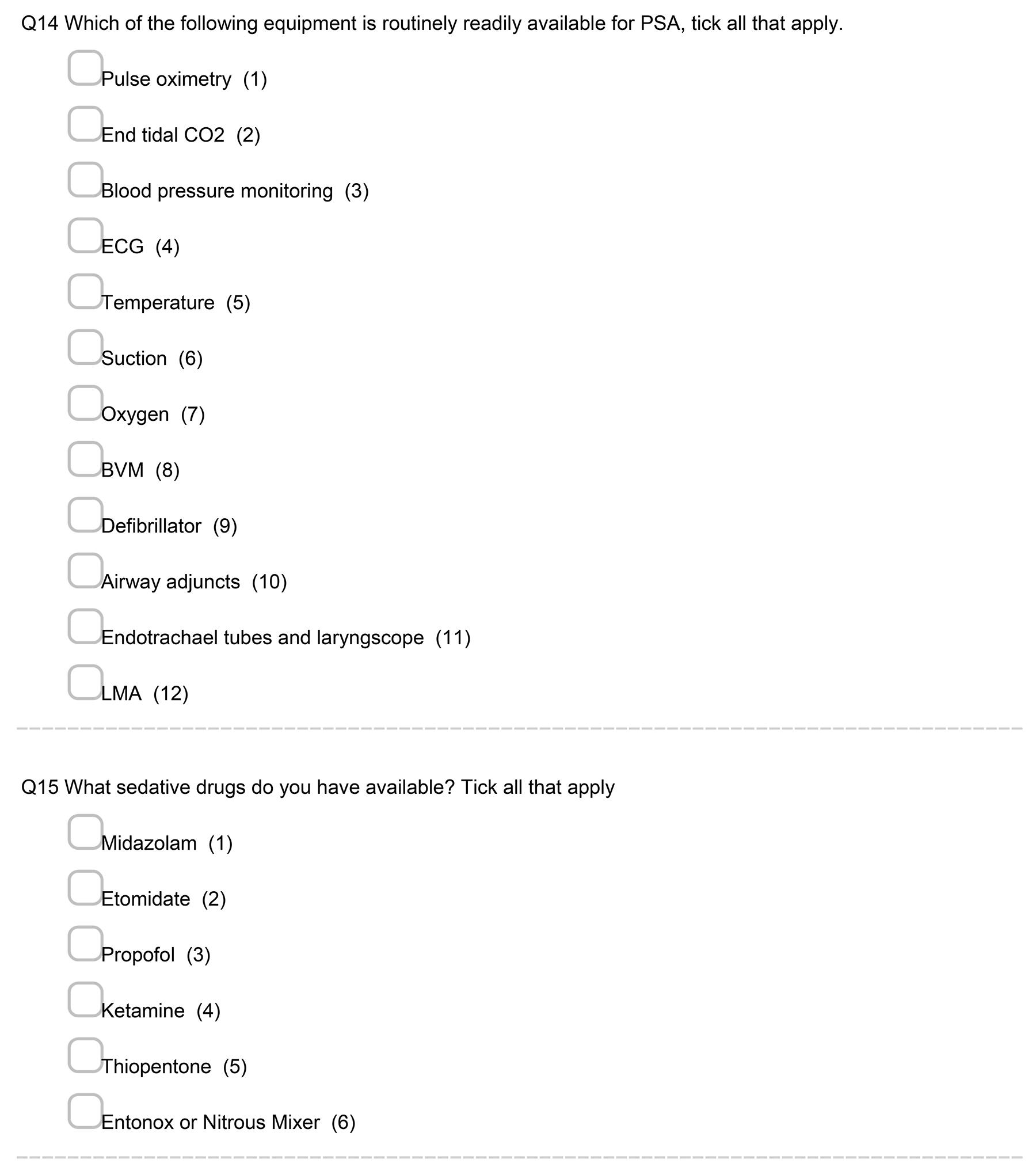
The quantitative descriptive survey consisted of 31 questions. Five concerned general information, six addressed sedation staffing level, and 12 questions explored procedural sedation practice. A further three questions sought information on clinical documentation and five questions on training guidelines. Question format was closed in 23 and open in 8 questions (Appendix I). Data were downloaded to the Statistical Package for the Social Sciences v25 (IBM; https://www.ibm.com/support/pages/downloading-ibm-spss-statistics-25).
Ethics approval
Ethics approval from New Zealand Health Disability Ethics Committee (HDEC) was not required after initial application (HDEC ref. 15/NTB/48) and Māori consultation sought through Eru Waiti from Te Komiti Whakarite.
Results
A total of 17 surveys were electronically distributed to the study rural hospital contacts. A total of 14 surveys were started, with 12 surveys fully completed. One hospital contact responded only to the general questions and another hospital contact did not answer questions regarding staffing levels or questions on training, but otherwise responded to the survey. Thus, number of results varied from 12 to 14 in each section of the survey.
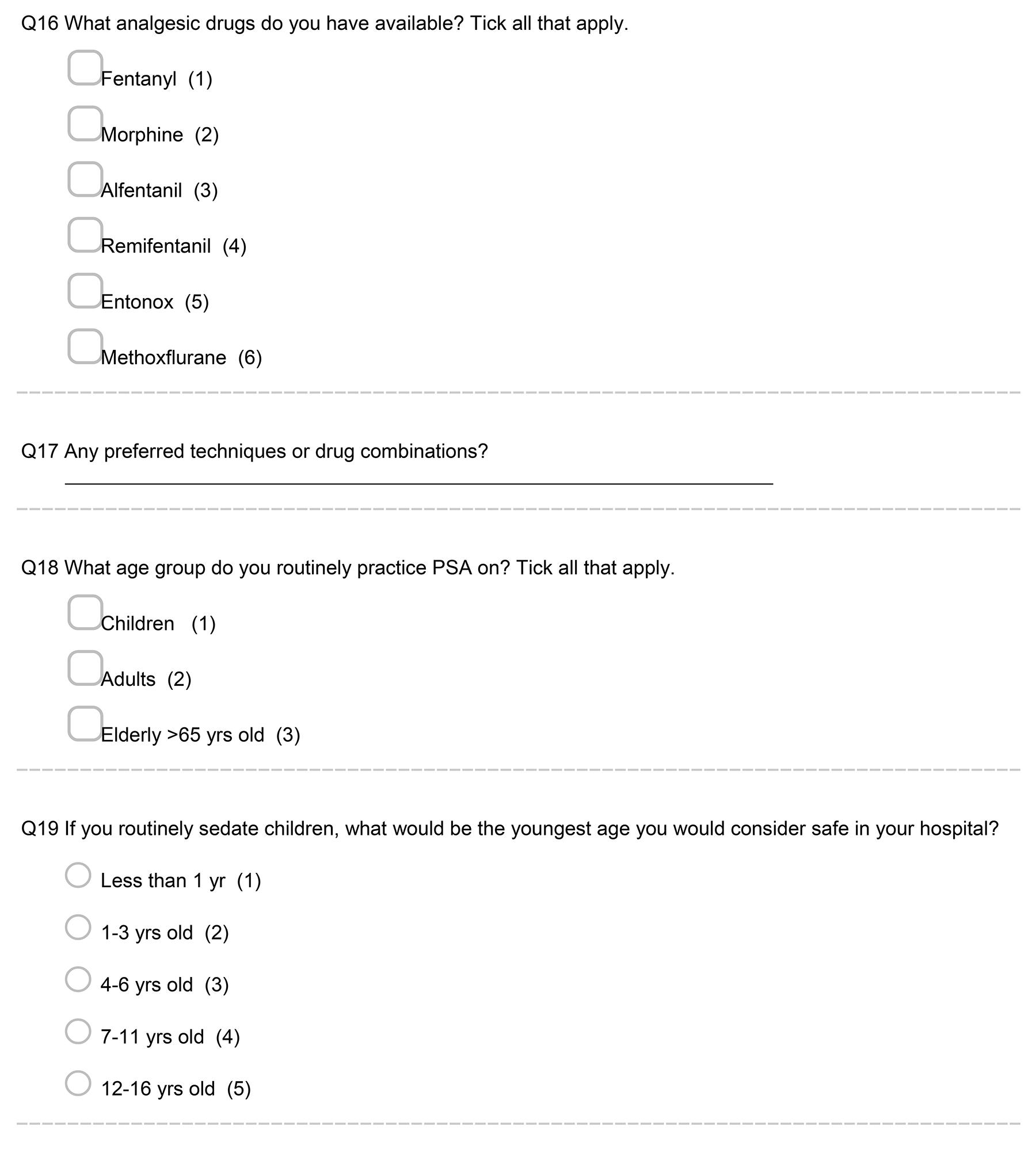
Ten rural hospitals were larger level three hospitals (71%) and four were level two (29%). None of the smaller level one hospitals were represented in the survey. The study hospitals were distributed throughout New Zealand, with six (43%) in North Island and eight (57%) in South Island. Waikato was the main tertiary referral centre for North Island hospitals, and Dunedin and Christchurch were the tertiary referral centres for rural hospitals in the South Island (Fig1).
The distance of rural hospitals to their referral hospitals varied, with the closest being 65 km and the furthest at 326 km away. Range was 261 with a mean of 147 km and median of 105 km. Three rural hospitals identified their base hospital as the main referral centre, rather than the regional tertiary hospital. Those base hospitals identified were: Southland, Taranaki Base and Whangarei hospitals. All study hospitals performed procedural sedation and twelve hospitals (85%) had Rural Hospital Medicine (RHM) Fellows in regular employment.
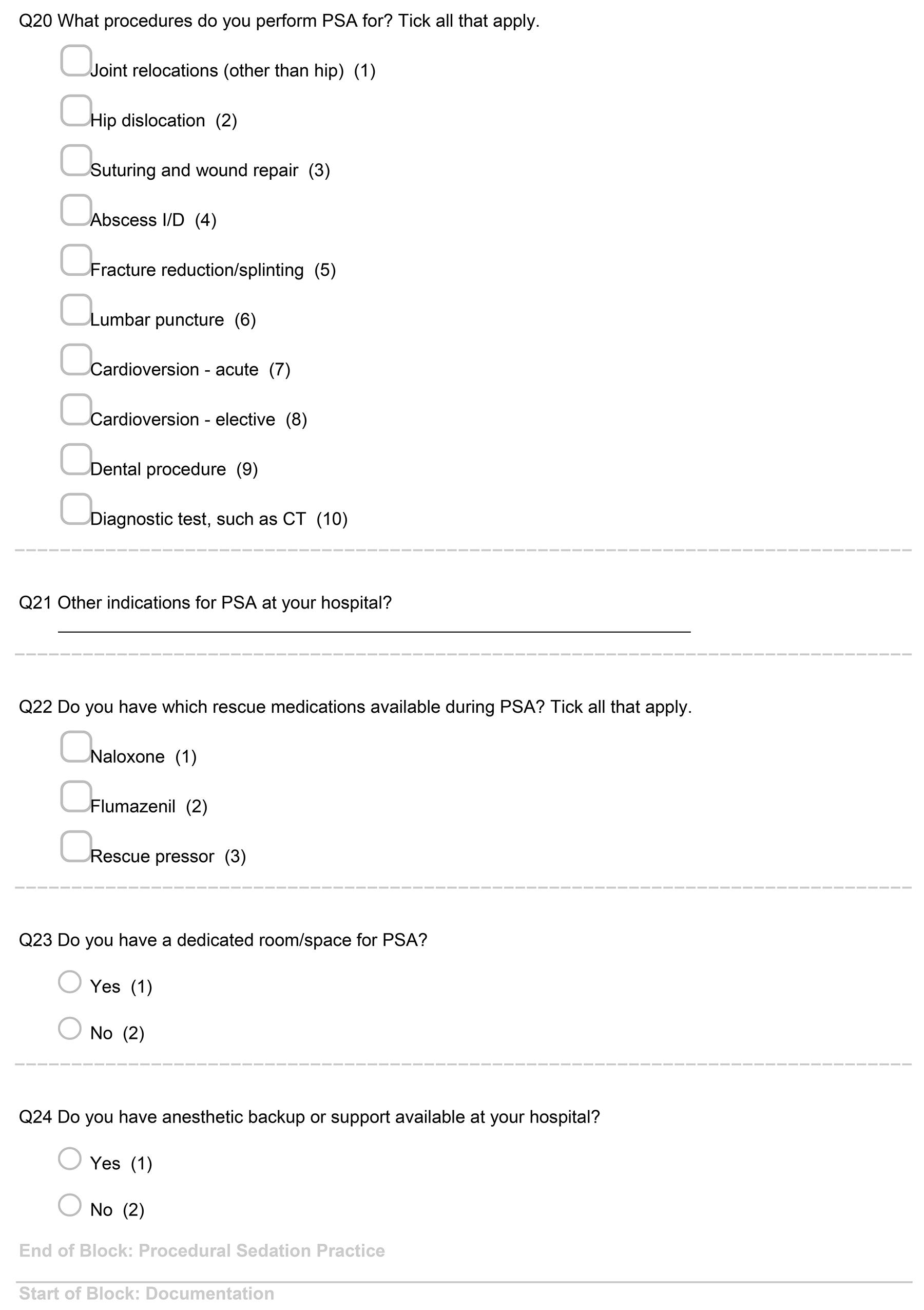
Twelve hospital contacts responded to the staffing level questions. Staffing levels available for sedation in the surveyed hospitals varied. During normal weekdays, six hospitals (6/12, 50%) had two doctors available for sedation. However, the majority of hospitals had only a single doctor available for sedation during evenings (8/12, 67%), and over the weekends there were seven (7/12, 58%). One hospital (1/12, 8%) did not provide sedation services during evenings and weekends. At night, four hospitals (4/12, 33%) stopped sedating patients and seven hospitals (7/12, 58%) had only a single doctor available for sedation during nights. Nursing support varied from one to two nurses available for help, and no hospital had three nurses available for sedation. Three hospitals (3/12, 25%) had a formal system for a second on-call doctor in case of the need for staffing support for sedation. Eight respondents (8/12, 67%) felt that a minimum safe level for procedural sedation in their rural hospital required only a single doctor. Changes to sedation team composition over the working week and surveyed safe sedation staffing personnel are shown in Figure 2.
There were thirteen responses regarding the practice of PSA. Six of the rural hospitals (6/13, 46%) performed procedural sedation more than once a week, with another two hospitals (2/13, 15%) sedating once a week. Three hospitals (3/13, 23%) sedated patients a few times a month, and two hospitals (2/13, 15%) less than once a month. All 13 hospitals routinely used pulse oximetry, blood pressure and heart rate monitoring when sedating patients and all had resuscitative equipment available. In addition, eight hospitals (8/13, 62%) used end tidal CO2 monitoring in their sedation practice.
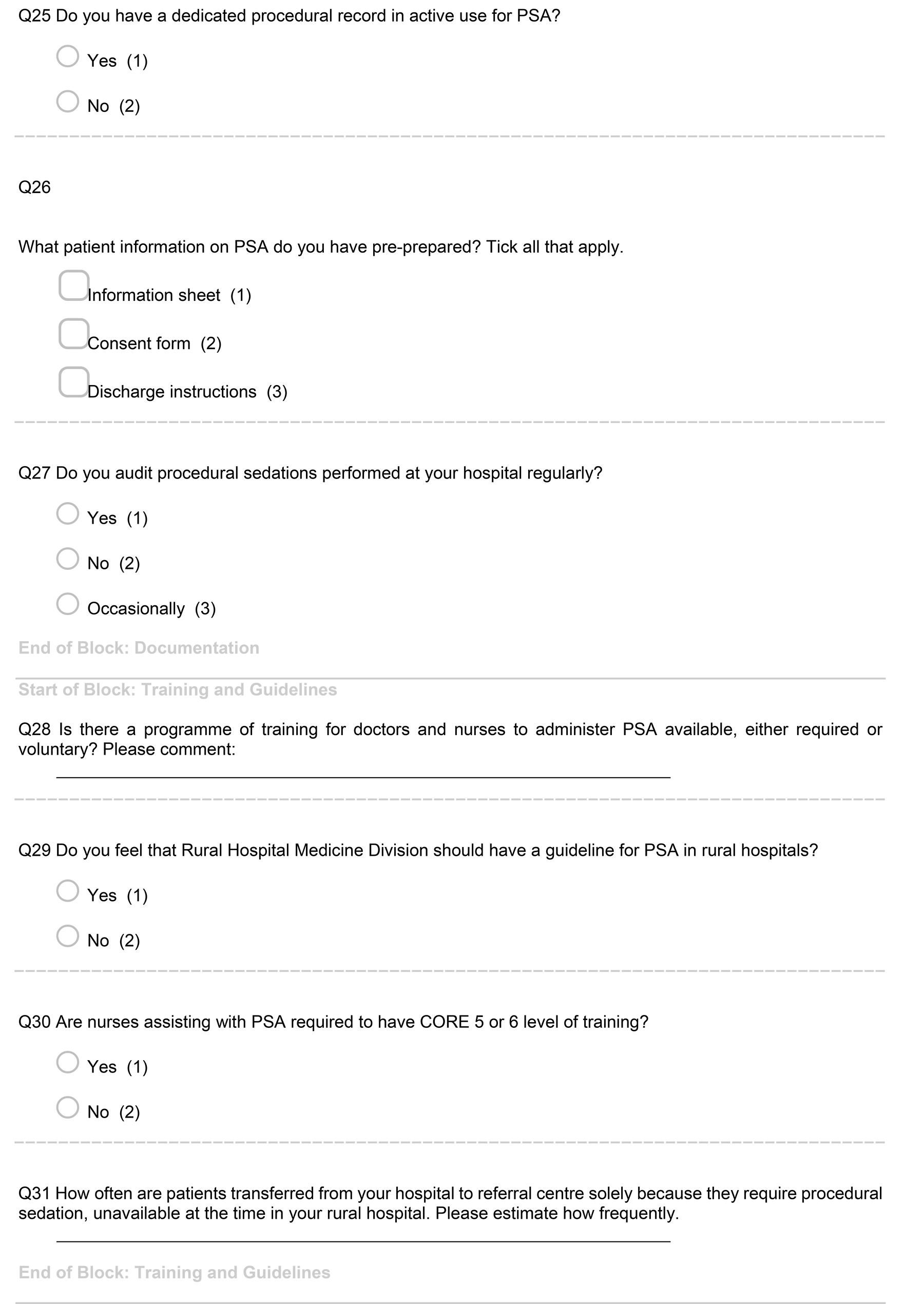
All of the 13 surveyed hospitals had fentanyl, morphine and nitrous oxide available for analgesia as well as sedative agents midazolam and ketamine available. Analgesic and sedative medications available in rural hospitals are shown in Figure 3. Ketamine was the preferred sedative medication according to many respondent comments (6/9, 66%), with replies such as ‘use a lot of ketamine’. Most hospitals also had access to propofol (11/13, 85%) and etomidate (7/13, 54%). All sites had naloxone available, 12 hospitals (12/13, 92%) had rescue flumazenil and nine (9/13, 69%) had a rescue pressor available. All hospitals sedated adults and 10 (10/13, 77%) sedated children. No hospital used procedural sedation in children aged less than 1 year.
Common clinical indications for procedural sedation included relocating dislocated joints in all hospitals, and wound repair, hip reduction and fracture manipulations in most hospitals (11/13, 85%). A majority of the hospitals also provided acute sedation service for cardioversions (10/13, 77%) and abscess incision and drainage (8/13, 62%). Some hospitals also utilised sedation for elective cardioversions (4/13, 31%), diagnostic tests such as CT (3/13, 23%), and dental procedures/lumbar puncture (2/13, 15%). Indications for sedation requirements are shown in Figure 4.
Nine of the thirteen rural hospitals (9/13, 69%) did not have a dedicated room or space to perform procedural sedation. Only four hospitals (4/13, 31%) had a dedicated procedural sedation area, and only two hospitals (2/13, 15%) had anaesthetic backup available at their hospital. Regarding procedural sedation documentation, seven hospitals (7/13, 54%) did not have a dedicated sedation clinical record in use, nor were regular audits performed on sedation records. Only one hospital (1/13, 8%) audited regularly. None of the hospitals surveyed had training available for either doctors or nurses on procedural sedation. However, three of the respondents noted that such a program would be useful to have. Nine of the respondents (9/12, 75%) thought that the Division of Rural Hospital Medicine should have a sedation guideline available for New Zealand rural hospitals.
The final question asked hospital contacts to estimate how frequently they would have to transfer a patient from their rural location to a referral centre, solely for procedural sedation purposes. Out of 12 responses to this question, six hospitals (6/12, 50%) transferred a few patients each year and the remaining respondents estimated transfer of a few patients each month to tertiary hospitals.
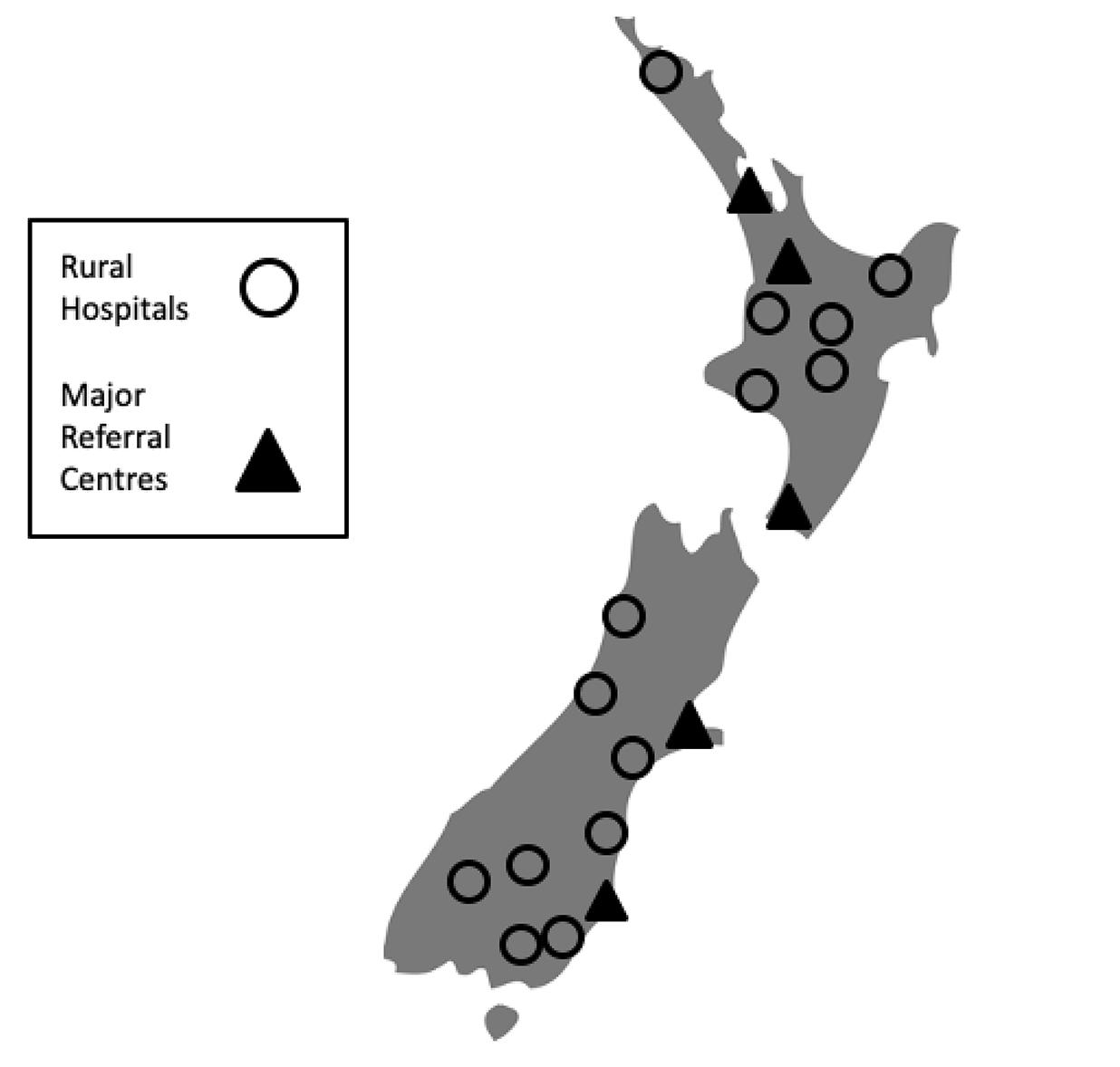 Figure 1: Locations of surveyed rural hospitals with tertiary referral centres.
Figure 1: Locations of surveyed rural hospitals with tertiary referral centres.
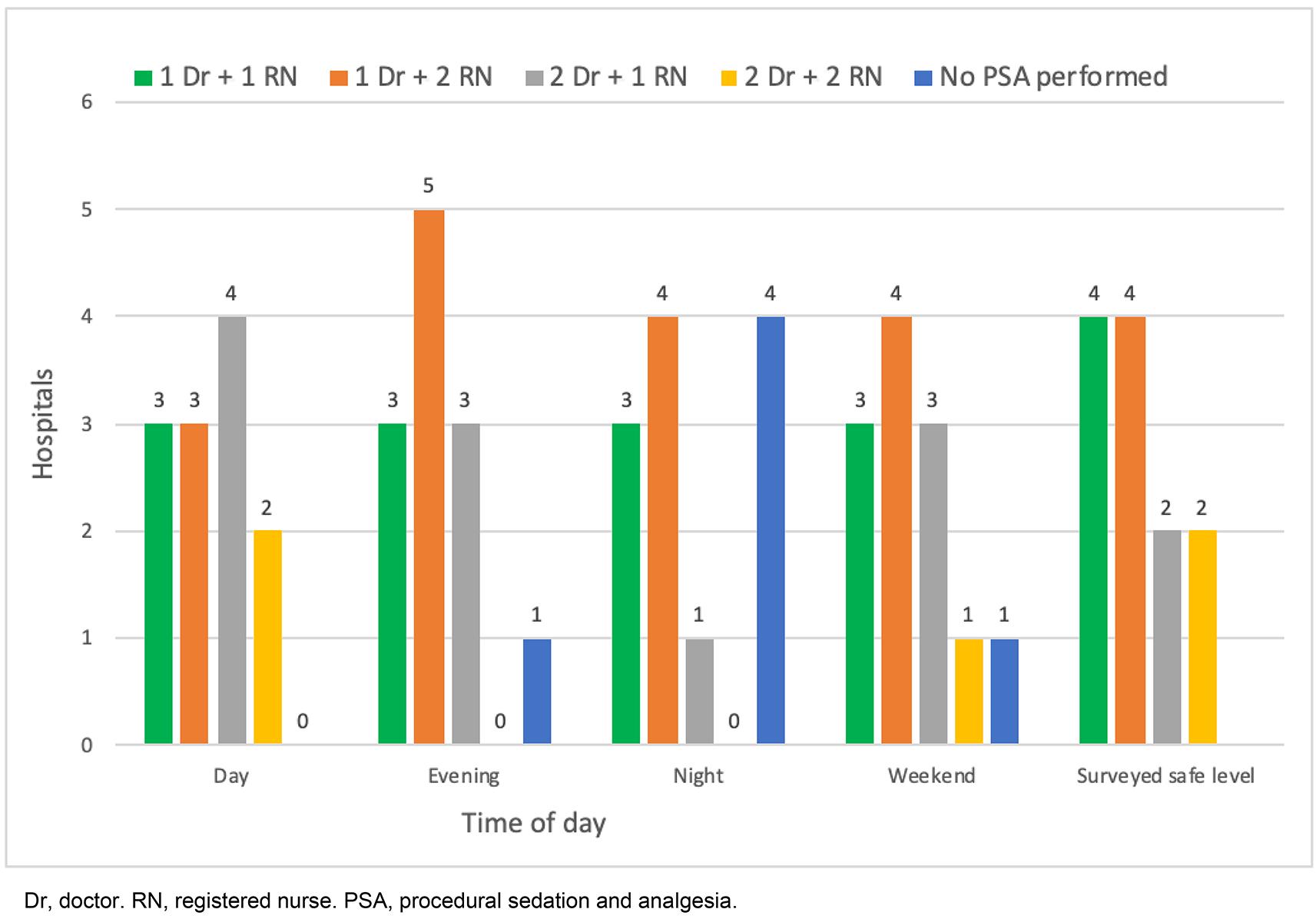 Figure 2: Rural hospital sedation team composition at different times and surveyed safe sedation staffing levels as per survey contacts.
Figure 2: Rural hospital sedation team composition at different times and surveyed safe sedation staffing levels as per survey contacts.
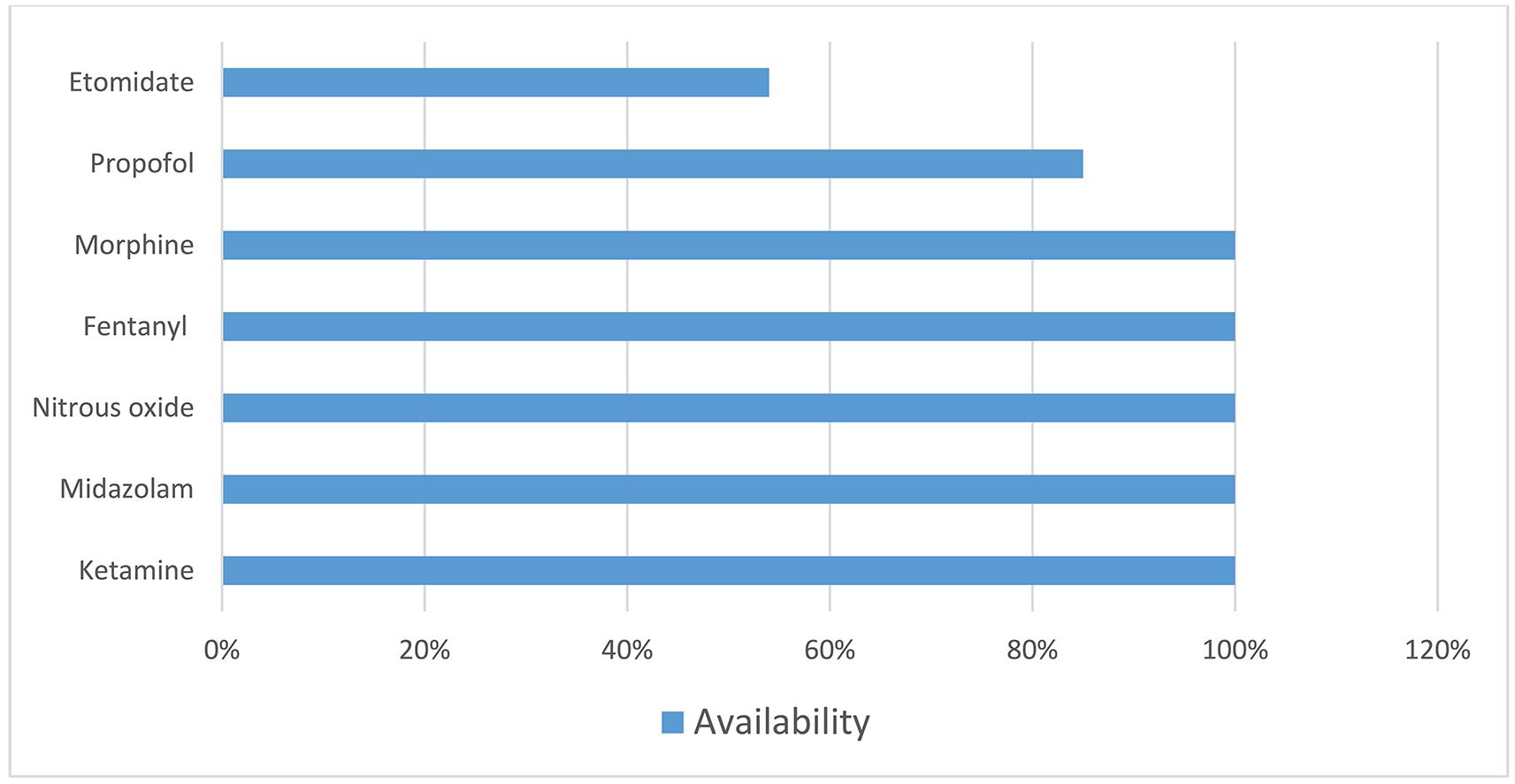 Figure 3: Analgesic and sedative medication availability in surveyed rural hospitals.
Figure 3: Analgesic and sedative medication availability in surveyed rural hospitals.
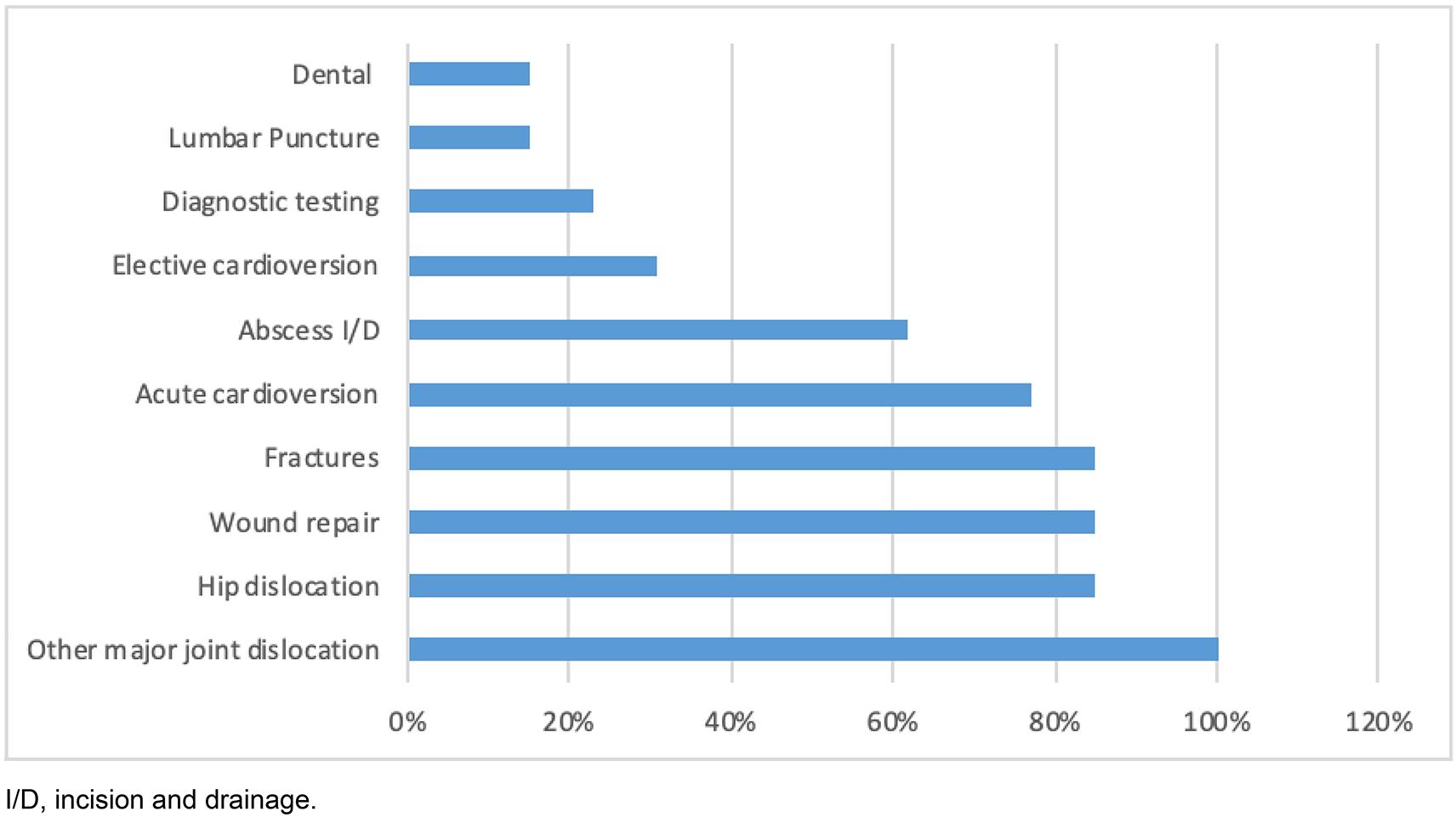 Figure 4: Common rural hospital procedures requiring sedation.
Figure 4: Common rural hospital procedures requiring sedation.
Discussion
1. Procedural sedation and analgesia is frequent
This study demonstrated that PSA is frequently performed in rural hospitals in New Zealand, with the majority of respondents performing PSA at least once a week or more. A wide variety of procedures are facilitated by rural PSA including orthopaedic and injury treatments, abscess incision and drainage, and cardioversions. In contrast, patient transfer to another centre for the purpose of PSA is infrequent, occurring a few times a month or less for all hospitals. Distances for transfer vary according to hospital, with a median distance of 105 km.
Rural PSA facilitates definitive treatment at the point of care within rural hospitals. Although this was not investigated by the present study, the authors expect that this represents significant time and cost savings to the patient, whānau (Māori-language word for extended family) and health service, and avoiding unnecessary patient transfer between hospitals is a desirable outcome.
2. Ketamine is preferred
Ketamine was the most preferred PSA agent in this rural hospital survey. Ketamine is a unique medication for procedural sedation, as it produces a state of cortical dissociation in which core protective reflexes are maintained7. Furthermore, ketamine dissociation occurs at a reliable dosing, and sedation can be reliably reached with a single intravenous dose8. Thus, ketamine's unique properties allow ketamine sedation a significant clinical safety margin. A large review of ketamine sedation with adults found ketamine to be very safe9: out of the 70 000 participants in their review, only one significant cardiorespiratory adverse event was found.
Ketamine use in staff- or resource-limited settings is supported by evidence outside New Zealand. The American College of Emergency Physicians’ 2011 clinical practice guideline supports single doctor ketamine sedation with nurse assistance as safe clinical care for an interruptible procedure10. In a more rural and remote setting, a project in rural Uganda trained nursing staff to provide ketamine sedations. In this consecutive observational cohort study in 2010, two trained nurses performed procedural sedation 191 times without any major adverse events11. A follow-up study with a second cohort of nurses in 2013–2014 showed again that ketamine sedation in 162 patients was performed safely without major adverse events12. In a survey of doctors administering ketamine in low- to middle-income countries, over half performed both the procedure and sedation without a second practitioner13.
The authors of the present study suggest that procedural sedation, especially with ketamine, can be safely performed by a single doctor and another trained practitioner for an interruptible procedure in rural New Zealand hospital context.
3. Staffing levels and professional guidelines vary
This study found that staffing and equipment available for rural PSA varies according to institution, with the majority of rural hospitals having access to only one doctor out of hours, and only half having access to two doctors within usual office hours. A minority of rural hospitals had access to more than three members of medical or nursing staff for PSA at any time. Most rural hospitals used standard non-invasive monitoring for PSA, with two-thirds having access to capnography. PSA was mostly performed without the use of a dedicated area.
There are no definitive rural guidelines in New Zealand to support these patterns of PSA practice. A 2014 professional guideline available from the Australian and New Zealand College of Anaesthetists recommends competencies and personnel for PSA. This guideline recommends the use of two-practitioner sedation technique when using intravenous sedation medications. A practitioner was defined as a medical person with skills in airway management and cardiopulmonary resuscitation5. In contrast, and in recognition that ‘generous evidence exists to imply safety of these agents when used appropriately by single PSA providers’, a New Zealand rural hospital network position statement on procedural sedation in New Zealand rural hospitals supported a single-doctor model for PSA delivery14.
The present study shows that rural PSA does not adhere to a staffing level of two medical practitioners, particularly out of hours, nor do many of the rural practitioners think it necessary to do so – only a third of rural respondents agreed with the necessity of a two-doctor standard for PSA. Availability of two medical staff at different times, with opinions of two-staff safe sedation, are shown in Figure 5.
In addition to the ketamine studies previously cited, several studies support the safety of single-doctor and non-specialist delivery of PSA. In a large North American multicentre community hospital retrospective chart review, 435 procedural sedations were performed safely and effectively using a one doctor–one nurse model for orthopaedic fractures and dislocations15. In another prospective study, procedural sedation in a rural Canadian emergency department16 was provided by general practitioners who lacked formal anaesthesiology training. Data were collected from a standardised procedural sedation record. A total of 160 consecutive charts were reviewed for analysis. Overall, sedations were performed safely and successfully in this study. No intubations or procedures were cancelled due to an adverse event, with apnoea (10%) being the most common adverse event noted. This is likely due to the use of propofol and fentanyl in the majority of the sedations, ketamine only accounting for 5% of sedations. However, the present study supports that procedural sedation can be safely performed by non-specialists in rural hospitals. In this study, for a procedural sedation to be performed, the additional member of staff could be either an additional nurse or a second doctor.
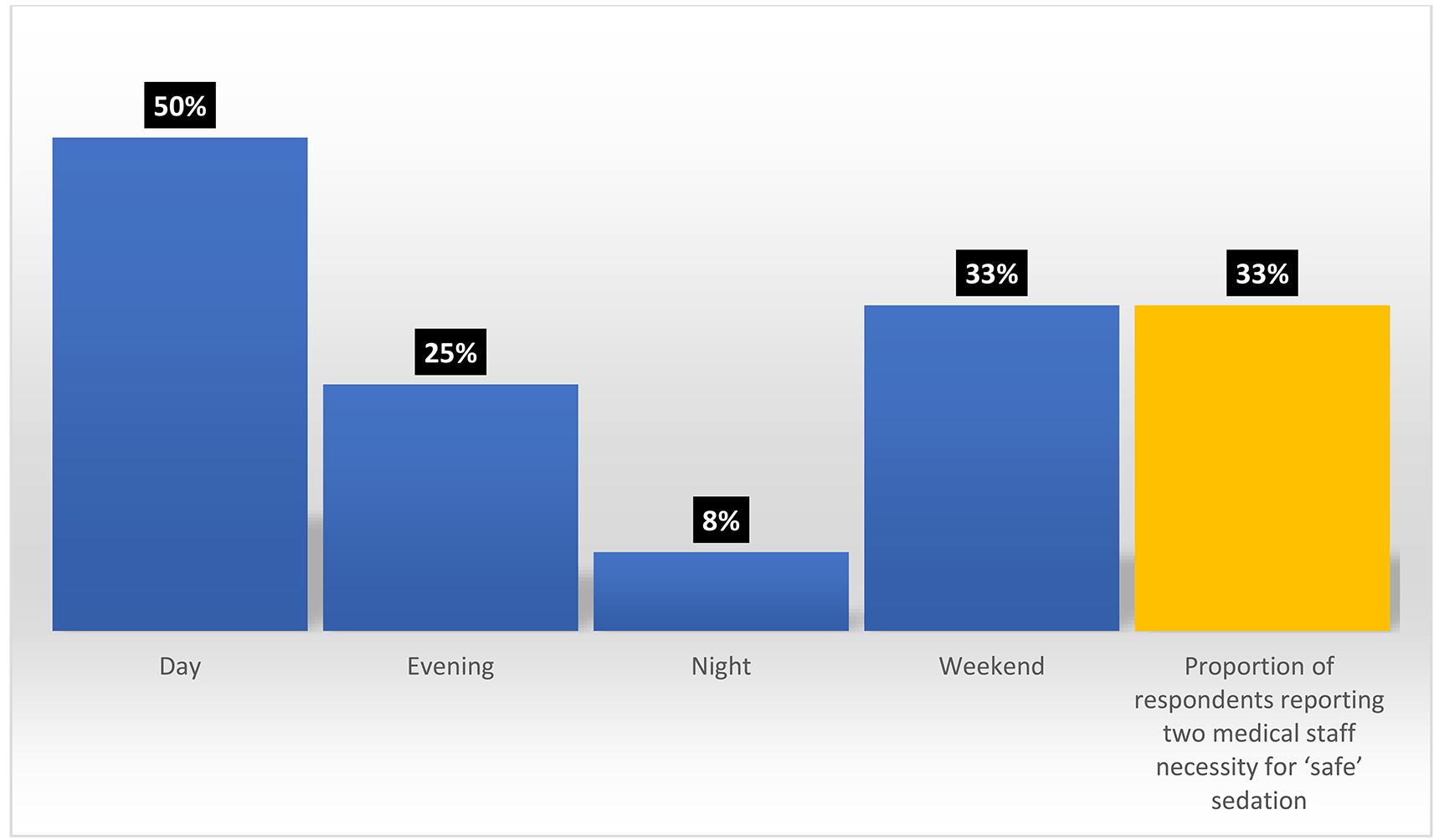 Figure 5: Proportion of hospitals with two medical staff available for procedural sedation and analgesia at different times (blue), and proportion of respondents reporting two medical staff necessity for ‘safe’ sedation (yellow).
Figure 5: Proportion of hospitals with two medical staff available for procedural sedation and analgesia at different times (blue), and proportion of respondents reporting two medical staff necessity for ‘safe’ sedation (yellow).
4. A rural approach is supported
A specifically rural approach to PSA was supported by the majority of contacts in this survey. The authors recommend that future versions of sedation guidelines engage the rural workforce to provide guidelines that are safe, achievable and patient centred. Recommendations should reflect the complexities of real risk and opportunity costs for rural patients, communities and health services, where utilisation of limited resources for interhospital transfer, loss of income and distance from whānau are just a few examples of the wider outcomes relevant to the rural context. In the rural context, the competencies of interprofessional practitioners may be more important than specific prescriptions around team composition, and solutions such as altering timing of procedures to match resources can be considered.
In addition to staffing levels, this survey identified several components of PSA practice that varied considerably between settings and would also benefit from establishing minimum standards. Other examples were identifying and establishing dedicated procedural sedation areas with equipment including capnography and implementing a dedicated sedation clinical record for use at all times. This would lay the foundations for regular audit capability and a rural sedation registry in the future.
Finally, this survey identified a need for rural PSA training, as well as establishment of national-level guidelines. At the time of this survey, none of the hospitals had training available on procedural sedation for nurses or doctors, nor were there rural-specific guidelines.
Limitations
A major methodological limitation of the survey was the insufficient data from 12–14 individual responses to answer the research aims. The survey was limited by response rate, and most responses came from active larger centres with a greater baseline staffing level. The authors cannot draw conclusions about the prevalence of PSA within the smaller rural centres, nor draw conclusions about the influences upon those hospitals not performing PSA. This study was a survey, not a review of individual practice, and therefore is susceptible to reporting bias.
Implications for future research
Other than the findings of this initial survey, little is known about procedural sedation in the New Zealand rural hospital context. Further definitive research is warranted to determine answers to the study aims, for example using a structured national rural hospital sedation audit, followed by prospective rural hospital data collection. Future outcomes could include developing rural guidelines, standards and practices for procedural sedation, professional training opportunities for rural medical and nursing staff in rural hospitals and advocating for safe clinical sedation practices.
Conclusion
A survey of rural hospital PSA practice demonstrated that PSA is a commonly performed procedure for a variety of indications. Ketamine was the most preferred PSA agent. Staffing and equipment available for rural PSA vary according to institution, with most rural hospitals performing PSA with one or two doctors. There is no current professional framework that suitably defines minimum standards for rural PSA practice, and specific training resources are limited.
Providing procedural sedation and analgesia is an essential rural hospital service that is patient and whānau centred, saves patient transfers, and should be supported by a safe, pragmatic and realistic framework of tools, recommendations and training for rural practitioners.
Acknowledgements
This research was made possible through grants from Advance Ashburton Trust.
References
You might also be interested in:
2017 - Demographic and rural-urban variations in dental service utilization in Taiwan
2007 - Medical services for rural Ethiopean Jews in Addis Ababa, 1990-1991