Context
Canada, like much of the world, is in the midst of an opioid crisis. In 2019, there were 3823 accidental deaths (10.2 per 100 000) and 4435 hospitalizations (15.2 per 100 000) related to opioids1. A rise in toxicity of the drug supply through contamination by synthetic opioids such as fentanyl, and Canada’s status as second largest consumer of prescription opioids in the world, contribute to the crisis2. Harms associated with opioids disproportionately impact young men and Indigenous peoples, and occur in urban, suburban, and rural communities across Canada3. There is some regional variability in opioid use, and in the province of Ontario the rates of hospitalization for opioid poisonings are highest in small cities with populations of 50 000–99 9993, whereas rates of methadone maintenance therapy per capita4 and hospitalizations among youth for substance abuse are highest in rural and remote areas5.
Rural communities are heterogeneous with respect to geographic, social, and economic conditions; however, rural Ontarians tend to have higher levels of unemployment and reliance on social assistance, lower incomes, and fewer years of education6. These social determinants of health, in addition to mental illness and history of trauma, frequently lie at the root of substance use7. The small population size of rural communities, fixed social identities, and beliefs among many residents that harm reduction approaches enable drug use, contribute to stigma as a barrier to both developing and seeking addiction services8. Spatial inequalities, such as large geographic distances to services, limited transportation options, and fewer qualified healthcare professionals, also create unique challenges for treatment of opioid use disorder (OUD) in rural communities9.
In rural Ontario, most clients receive opioid agonist therapy (OAT) through a publicly funded physician fee-for-service model that is separate from mental health and specialty addictions services10. While gaps in knowledge persist regarding the most efficacious forms of care for people using substances in rural areas11, it is considered best practice in OAT to integrate pharmacological therapy with counselling, social support, and mental health services10. Opioid agonist therapy alone, often facilitated via telemedicine from a physician in an urban area, does not address the full breadth of addictions supports required for patients with complex needs. Given the chronicity of OUD and lack of specialty addictions services in rural communities, treatment can most appropriately be delivered by a multidisciplinary team within primary care12. However, there is a paucity of literature describing and evaluating primary care-based addictions support in the rural Canadian context.
The setting for this program was a small town in Ontario’s cottage country with a population of less than 4000. Local residents once relied on mining and lumber industries for employment, but a shift toward a tourism economy has led to challenges finding year-round full-time employment and contributes to 25% of the population living at or below the low-income cut-off13. The only public transit available is a volunteer-run van service, there is a shortage of affordable and safe housing, and other social determinants of health such as food security are often lacking. No local data exists regarding the prevalence of substance use in the area; however, county-level data indicate that rates of opioid-related hospitalizations and self-reported illicit drug and marijuana use are higher than the provincial average14,15. Locally, service providers and community members have observed an increase in patients seeking OAT, drug seizures by police, and discarded needles in public settings, suggesting a substance-use crisis has emerged in recent years. It was in this context that the Rural Outpatient Opioid Treatment (ROOT) program emerged.
Issue
Program description
ROOT was developed to bring some of the structure of an inpatient treatment program into a rural outpatient setting. The program began as a collaboration between a registered nurse (RN) system navigator and family physician within a family health team, and expanded to include a multidisciplinary team of community-based service providers to facilitate integration of group recovery work, primary care, harm reduction, peer support, smoking cessation, OAT, screening and treatment for hepatitis C and HIV, and longitudinal follow-up. These services were coordinated within primary care, and aimed to provide barrier-free support for people who use drugs from a harm reduction approach. A small pocket of funding was secured from the local health authority, and a nurse researcher from the local university was invited to assist in program evaluation.
Participants were selected through either self-referral or from local providers. After completing an application and intake process, including an interview and baseline research and evaluation tools (WHO Quality of Life (WHOQOL16 and Addiction Severity Index17), the program ran for 12 weeks of intensive programming, followed by 9 months of aftercare. All participants who completed the intake were accepted into the program. Each participant was also offered a space in the family health team roster; if they already had a doctor, the family physician offered to support that doctor or have the patient move over to that doctor’s practice. Participants were offered OAT, although most who desired it were already on therapy. No participants’ OAT doses were meaningfully changed throughout the duration of the program. Time with the family physician was reserved every 1–2 weeks for ROOT patient visits to review primary care and other presenting social issues, which was coordinated by the RN.
On a typical intensive programming week, participants met twice in a clinician-led group setting: Mondays were a structured relapse prevention program18 and Wednesdays a mindfulness-based relapse prevention program19. Two clinicians led each group, with regular visits by the family physician. Throughout the three rounds of the ROOT program, clinicians included a social worker, addictions counsellor, RN, and member of the local violence against women organization. On Tuesdays, a peer-led group was offered and on the other days participants could meet with their physician and/or OAT prescriber, nurse or addictions counselor. There were often additional phone calls throughout the week to check in with participants, as well as occasional fitness sessions. Harm reduction supplies, including naloxone kits, were readily available at group sessions. Participants provided weekly urine drug screens, completed the Addiction Severity Index and monitoring questionnaires monthly, and the WHOQOL at 6 and 12 months. None of these measures were mandatory to continue with the program, in an attempt to reduce barriers to participation. Incorporating the practice of contingency management20, participants received CA$5 in gift cards each week for attending at least one group.
Including peer support workers was integral to the ROOT program. For the first round, two peers from a local peer support agency who had lived experience with substance use were recruited. Due to timing and funding constraints when the program was being developed, they were not involved in the study design. The peers participated in the twice-weekly, clinician-led groups and then led their own group once per week. In subsequent rounds of ROOT, the same two peers did not attend the clinician-led groups but continued in all other capacities. Peers were trained in harm reduction philosophy, non-judgmental communication, and active listening. They conducted intake, 6-, and 12-month interviews, and were available for one-to-one sessions to support participants when needed. The peer support workers collaborated closely with the other team members and helped reinforce skills learned within the clinician-led groups.
Interviews and focus groups were also conducted for program evaluation and to understand the influence of the rural context on participants’ recovery experience. Baseline and 3-month interviews were conducted by the peer support workers, while the RN and nurse researcher facilitated the focus groups. Focus group participants were recruited as part of regular outreach by the RN and peers. Questions for the individual interviews were semi-structured, with a focus on what a typical day looked like, successes and challenges encountered in their recovery, and their goals for the future. Three-month follow-up questions were similar to the baseline interview, with the addition of questions pertaining to what participants had learned since becoming involved in the program and how life had changed. Focus group discussions centered around the impact of the program on participants’ lives and how their experience was influenced by the rural context. Additional questions were posed during the focus group with peers around the benefits and challenges associated with their role. Results from the quantitative analysis were presented and focus group participants were offered an opportunity to reflect on these findings. Interviews and focus groups were audio-recorded and transcribed verbatim for analysis. The RN and nurse researcher analyzed the data separately and then discussed and refined themes collaboratively using an interpretive descriptive approach21.
Program evaluation
To date, three rounds of the ROOT program have been delivered. The final group is currently completing aftercare, although most data collection has ceased due to COVID-19. There were six participants in each of the first two intakes and four participants in the third intake, for a total of 16 participants enrolled in the program between October 2018 and March 2020 (Table 1). Participants ranged in age from 19 to 57 years and were predominantly female. They attended an average of 65% of the sessions, and while urine drug screening was not mandatory, most participants submitted weekly urine when they were in attendance. Findings from the urine drug screen showed that opioid use declined throughout the first 12 weeks of follow-up (Fig1) while other unprescribed substances, particularly methamphetamines and cocaine, remained high throughout the program (range: 33–64%). The reduction in opioid use appeared to be sustained during longer term follow-up; however, this data is not included due to less frequent urine drug screening and missing data. Monitoring questionnaires showed that at intake only 13% of participants had used illicit stimulants in the previous 30 days, while range of use was 17–54% throughout the subsequent 6 months. Marijuana use was also common, as self-reported by 57% to 83% of participants who completed monthly monitoring questionnaires (consistent with marijuana use among 67% of participants at intake).
These monthly questionnaire results were supported by weekly urine drug screen results. With respect to social stability, monitoring questionnaires showed that one participant was arrested and there were four overdoses within the first 6 months of the program. Due to missing data from ROOT 2 and cessation of data collection from ROOT 3 participants, a thorough analysis of the QOL and Addiction Severity Index scores is not possible.
Qualitative data were collected from 11 participants via individual interviews (11 participants at baseline and six participants again at 3 months) and two focus groups (three participants in one focus group and two peer support workers in a separate focus group). This provided important insight regarding participants’ experience with ROOT 1 and 2 and how the rural context influenced their substance use and recovery.
Table 1: Characteristics of Rural Outpatient Opioid Treatment participants (n=16)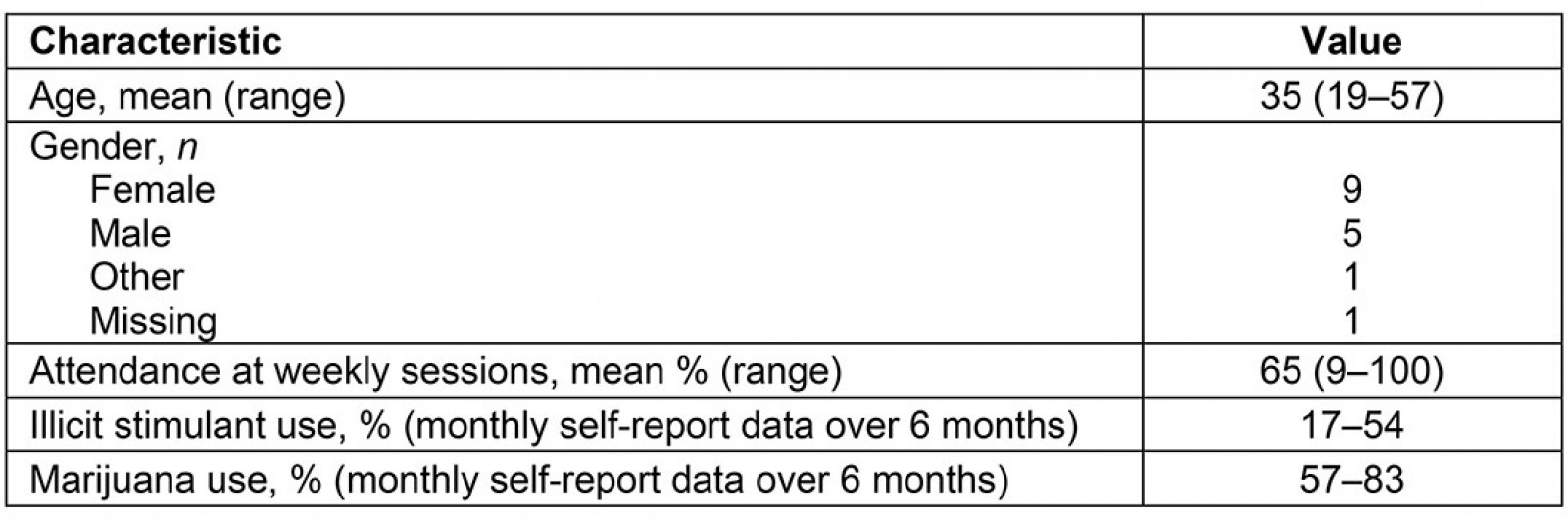
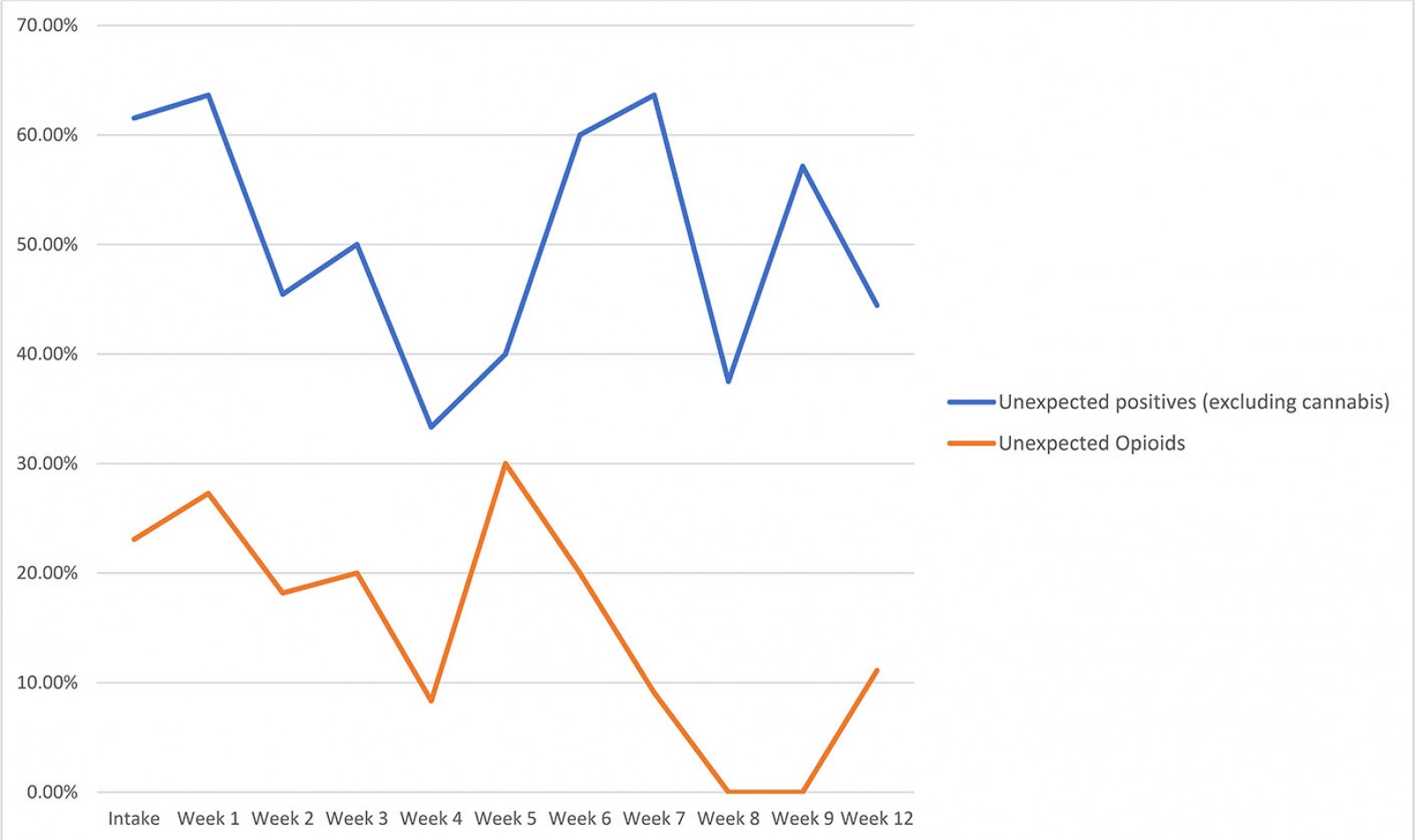 Figure 1: Combined urine drug screen results for three consecutive Rural Outpatient Opioid Treatment program groups.
Figure 1: Combined urine drug screen results for three consecutive Rural Outpatient Opioid Treatment program groups.
Access to social support: Participants spoke about the opportunity to be around people who understood their experiences, didn’t judge or label them a ‘junkie’, and became social supports to them outside of group. One participant who was new to the area met another parent at the weekly group and stated their ‘kids have been able to support each other as well’, illustrating the benefits of an expanded social network that extended beyond group. Another participant felt attending group was ‘like a group getting together to talk … it was just like … like everyone was just kind of friends’. For some participants, it was the first time they opened up about their substance use: ‘Other than [group], I would not talk to anyone about drugs at all. This is the first time I have done that’. Having something to be a part of, and feeling able to help others in a similar situation while they received help in return, was identified as ‘fulfilling’. These factors contributed to some participants’ sense of accountability to the group that encouraged them to keep coming back.
Access to service providers and peer workers: The multidisciplinary nature of the ROOT program gave participants access to a range of providers, including being added to the roster of the family health team. The integration of mental health counselor, physician, nurse, and peer workers was labelled ‘seamless’, and the follow-up and outreach by providers were contrasted with a hospital-based program one participant had been enrolled in, where ‘it was just more like they were just feeding information than actually, you know, caring’. Another participant felt that ‘somebody hauling you in, things like that I think, makes you…just makes you feel like somebody cares’. Participants felt the providers were non-judgmental and facilitated new knowledge and skill development that included meditation, how to get out of ‘autopilot’, and strategies for educating participants’ loved ones about their substance use. The benefits of having peers who had ‘been through it all’ were appreciated by participants who reported feeling understood. One participant described the supportive role of the peer worker, in which ‘I’d have shitty days, just like text [peer] and she’d come meet me at the park and we’d take the dog for a walk’.
From the perspective of the peer support workers, the structure of the program in which they attended the sessions as part of the group within the first round of ROOT was important for building trust with participants. They stated this helped them feel connected to participants as though ‘we’re all in this together’. It was more challenging to build relationships during the second and third round of the program, as the peers were concerned they were considered outsiders or ‘part of the professional group now’. Although the nature of the work was rewarding, as peers felt they were a ‘beacon of hope’ for others and that ‘all of the shit was worth it’, the role could also be triggering with respect to their own substance use and recovery, and was taxing on them due to exposure to the chaos of others’ lives and feeling attached to their role ‘24 hours a day’, which meant boundaries and time away were important.
Rural context: A unique feature of this program was its integration into a rural primary care setting. The rural context impacted participants’ experience within the program as well as with their substance use and recovery. Participants discussed the challenges with small town stigma regarding substance use, boredom, and lack of privacy where ‘if you’re seen walking in, or in the methadone clinic parking lot … everybody in the whole town looks at you differently’. Once a person was known in the area as a drug user, participants felt the police ‘will mark you’, which deterred some residents from seeking OAT and even harm reduction supplies such as a naloxone kit. A reputation, either one’s own or their family’s, can stick because ‘people have been growing up here their whole lives, so the people in community have watched them … from when they were a child to now in their 20s, 30s, and 40s, knew their parents, knew their grandparents …’ Even among those using substances, judgment toward other users was prevalent when they discussed methamphetamine use and its increase locally among young people. Two members of the focus group were clear that they did not associate with anyone who used methamphetamine and found it ‘disgusting’. Another described being shocked when she saw a 15-year-old buying methamphetamine during a high school lunch break. Overall, the small population increased visibility in the community and branded people as users, while a shortage of housing and lack of transportation options also meant it was hard to get away from one’s social network when trying to stop using or avoid certain people and places.
These challenges with using substances in a small town existed in parallel to the benefits. Some participants who lived outside of town felt the rural geography and isolation were helpful. ‘It’s easier for me to stay clean here because I’m in the middle of nowhere. And especially before I ended up with a car, I couldn’t go anywhere unless my parents were with me … you can’t exactly go to your drug dealer’s house with your mom’. One of the peer workers felt the location of her home in the countryside allowed her to maintain boundaries with participants. The small population and connectedness of people within the area also made it easier to access people who use substances and for peers to do outreach.
This study was approved by the Health Sciences Research Ethics Board at Queen's University, reference # 34995.
Lessons learned
The ROOT program offered a variety of lessons. The first was in relation to methamphetamine use and the need for polysubstance support. It was found that while the unexpected opioid positives decreased throughout the program, there was an increase in crystal methamphetamine use over the same period of time. This coincided with increasing methamphetamine use in the broader area, which participants accounted for by its low cost and ease of access. The local methadone clinic also reported increases in methamphetamine positives locally and across the province, consistent with findings about increasing rates of methamphetamine use in Canada22 and in the USA among chronic opioid users23. This finding calls for support to be polysubstance in nature and highlights the importance of creating relationships that are free of stigma. With fentanyl in the drug supply2, it is especially important to support people using all substances and to help reduce the associated harms.
The second lesson learned was regarding the importance of providing a safe space, non-judgmental approach, and meeting people where they are at. One of the common themes in feedback received from participants was that the caring and non-judgmental support from providers who had the ‘right attitude’ made participants feel comfortable. This stands in contrast to the literature regarding the pervasive lack of trust between people who use substances and their healthcare providers24,25. From the outset, providers committed to developing a harm reduction, rather than abstinence-based, program. Voices of people with lived experience were incorporated by way of peers with substance use history, which was identified by participants as a strength of the program. It was recognized that when participants simply showed up for a session, regardless of level of engagement or urine drug screen result, this was a victory.
Finally, given the challenges encountered with lack of access to addiction services, infrastructure, transportation, and qualified staff in many rural areas9, this pilot project demonstrates that outpatient substance use treatment can be successfully integrated into a rural primary care setting. Requiring people who use substances to leave their communities for treatment is a significant barrier to quality care. The integration of multiple service providers from existing agencies, outreach by the nurse and peer workers, and addition of participants to the family physician’s roster led participants to feel cared for and that it was ‘not hard to find help’. This ease of access to holistic health and social care could be considered an anomaly in a rural setting. Access to care and removing barriers to participation were the highest priorities for the team. This required the RN to spend a lot of time on logistics, such as transportation, occasionally relying on in-kind contributions by members of the team, including the primary care physician, who could not bill for practices such as attendance at support groups. Data collection and maintaining control over the study conditions were of lower priority, a limitation of the evaluation but consistent with the project’s approach to prioritizing care.
Those who had negative feedback about the program were undoubtedly less likely to attend a focus group or share their feelings with the peer support workers involved in delivering the program. However, the combination of quantitative data and participant experiences highlight that even with a slight improvement above baseline, when providers took a harm reduction approach and saw these patients as people first, it was received with gratitude by patients. This demonstrates the sad reality that patients with addictions have very low expectations of support. Yet with collaboration among existing service providers and a small amount of funding, it is possible to develop and implement a patient-centered rural outpatient program that helps move participants along in their recovery journey. Given the success of the pilot program, ROOT has now been integrated into the family health team’s core primary care programming.
References
You might also be interested in:
2015 - Developing a culturally competent, sustainable rural model for diabetes prevention
2010 - Meeting the needs of Nunavut families: a community-based midwifery education program

