|
Article
Title
|
First Author
(year),
country
|
Population and context
|
Aim of study
|
Sample size
|
Study
design/
methodology/
Intervention
|
Relevant results/findings
and recommendations
|
Limitations/bias
|
Army and
Navy ECHO Pain telementoring improves clinician opioid prescribing
for military patients: an observational cohort study
|
Katzman
(2019)[34]
USA
|
Primary
care clinicians (PCCs), including physicians, advanced practice
clinicians and care teams at remote military, army and navy,
medical treatment facilities (MTFs)
|
To
assess whether Chronic Pain and Opioid Management TeleECHO
(Extension for Community Healthcare Outcomes) clinic (ECHO Pain)
telementoring improved pain management and safe opioid prescribing
skills
|
99 ECHO
Pain clinics
1283
control clinics
52,431
ECHO patients (annualised total)
1,187,945
control patients (annualised total)
Oct 2013
- Sep 2016
|
Observational
Cohort
study
Pre-/post-test
time series
Statistical
analysis
Intervention
group and comparison group
Primary
outcome: decreased prescriptions
Secondary
outcome: evaluation of dosage and co-prescribing
Onsite
and virtual training of expert teams was provided to the hub and
spoke clinicians taking part in the ECHO model
Military
MTFs, 5 US Army and 2 US navy sites were chosen as hubs based on
geographical location and availability of integrative and
interdisciplinary pain specialists to serve as facilitators
Intervention:
2hr
weekly, videoconferencing sessions including short evidence-based
pain and addiction didactics, case-based learning and
evidence-based recommendations
|
52% of
PCCs participated in four or more training sessions
PCCs in
the intervention group had greater declines in
annual
opioid related prescriptions per patient (-23% vs -9%, p <
0.001)
days of
co-prescribed opioids and benzodiazepines per user (-28% vs -73%,
p < 0.02)
number
of opioid users (-202% vs -08%, p < 0.001)
Future
prospective clinical trials may provide information regarding
benefits of the ECHO model at the patient level
|
The
study could not randomise the assignment of PCCs and patients into
matched groups therefore the baseline demographics for the
comparison group are skewed towards male and active-duty patients
PCCs
volunteered to attend ECHO Pain clinics
Data was
provided on individual clinics and not individual providers or
patients
It was
not possible to quantify how much each individual dose changed or
address specific patient/level causes of reductions in
prescriptions
|
|
SCAN-ECHO
for pain management: implementing a regional telementoring
training for PCPs
|
Ball
(2018)[14]
USA
|
Primary
care providers (PCPs) including MD/DOs, PharmDs, and nurse
practitioner's community-based outpatient clinics (CBOCs)
Cleveland,
South Texas or Wisconsin Veterans Health Administration (VHA)
medical centres
|
To
describe and provide an effectiveness assessment of Specialty Care
Access Network (SCAN)-ECHO for pain management (PM) training
program
|
21
MD/Dos
2
PharmDs
2 nurse
practitioners
2011-2014
|
Brief
research report
Pilot
Mixed
methods
Pre- and
post-training questionnaires
Qualitative,
virtual group interviews immediately following SCAN-ECHO PM
sessions
Statistical
analysis
Multidisciplinary
team of pain management specialists at the Cleveland Veterans
Affairs Medical Center delivered the ECHO program
Intervention:
Weekly
VC sessions including pain condition didactics and real-time
discussion on patient cases
|
Statistically
significant increases in confidence ratings and knowledge scores
on questionnaires pre- to post- training
Group
interviews:
Gains in
knowledge; self-efficacy - increase in confidence in providing
treatment; program format - conducive to learning; improved
patient care; improvements in networks and communication between
PM specialists and PCPs
Future
studies should examine whether and how this program has improved
access to specialty care, changes in provider behaviour and cost
savings
A
sustainability analysis will be critical to ensure that reported
gains can be and are maintained
|
Small
sample size and non-randomised sampling
Data are
limited to the participants who were interviewed only (2 sessions
each with 7 PCP's)
Potential
site-specific cultural differences and large variations in veteran
demographics across VHA facilities
|
|
Project
ECHO telementoring intervention for managing chronic pain in
primary care: insight for a qualitative study
|
Carlin
(2018)[16]
Canada
|
PCPs
including physicians, nurses, nurse practitioners, occupational or
physical therapists, pharmacists and social workers from rural,
remote or underserved areas of Ontario, Canada
|
To
report participants' experiences and assessment of Project ECHO
|
17
physicians
20
allied health professionals
2014-2015
|
Qualitative,
descriptive
Sandelowski's
qualitative-descriptive method of analysis
Six 1 hr
focus group discussions
Interdisciplinary
team of pain management experts including practitioners of
psychiatry, neurology, nursing, pharmacy, psychology, social work,
physical therapy, occupational therapy, chiropractic, addiction
medicine and family medicine delivered Project ECHO
Intervention:
Weekly
ECHO sessions including didactic lectures and three de-identified
case discussions
|
Focus
groups findings:
Challenges
of managing chronic pain in primary care - feeling helpless
before ECHO
Gained
confidence and knowledge -chronic pain clinical encounters were
less stressful; responsible opioid prescribing; changes in patient
management of cases "ripple effect" not presented at ECHO;
valued acquisition of knowledge about treating chronic pain
Sharing
of newly acquired knowledge with patients and colleagues
Developed
a sense of community and feeling less isolated
Disadvantages
-
Time
constraints, less time spent on didactic vs case presentations,
connection issues, viewing ECHO session highlighted PCP isolation
Further
qualitative research is underway to evaluate patient outcomes
Future
research will focus on the role and experience of the ECHO "hub"
of experts
|
The use
of a relatively public, open nature of discourse might cause
hesitation in the participants to reveal information
Participation
was on a voluntary basis
Knowledge
acquisition was self-reported rather than assessed independently
Data is
cross-sectional in nature and does not reflect change over
participants' time in ECHO
|
|
Effectiveness
of NIMHANS ECHO blended tele-mentoring on integrated mental health
and addiction counsellors in rural and undeserved districts of
Chhattisgarh, India
|
Mehrotra
(2018)[39]
USA
|
Counsellors
including clinical psychologists and psychiatric social workers
from 8 rural and underserved districts of Chhattisgarh, India
|
To
evaluate the feasibility and effectiveness of National Institute
of Mental Health and Neurosciences (NIMHANS) ECHO in training
counsellors
|
12
counsellors
41
patient cases discussed
Sep 2017
- Feb 2018
|
Pilot
Pre-/post-test
(3, 6 months) online surveys
Moore's
evaluation framework (first five levels) - Level 1:
participation, Level 2: satisfaction, Level 3: learning, Level 4:
competence and Level 5: performance; based on a 5-point Likert
scale
Statistical
analysis
The
specialist hub team consisted of a clinical psychologist,
psychiatrist and a psychiatrist social worker with expertise in
mental health and substance use related issues.
Needs
assessment tele-ECHO clinic initially held to formulate the
curriculum
Intervention:
12
fortnightly tele-echo clinics - brief didactic session, patient
case presentations and peer-led discussion
|
6
participants attended over 80% and all participants attended over
60% of clinics There were no dropouts indicating acceptability of
the model
Statistically
significant increase in mean scores for perceived knowledge,
self-confidence and self-efficacy after 6 months
Participants
liked "relevance to the courses to clinical practice";
"group-based discussions" and "a reduction in professionals'
isolation"
Future
studies: explore the long-term effects of the ECHO program on both
learner and patient outcomes; interview patients to enable an
evaluation of direct patient satisfaction
|
The
small numbers limit the generalisation of the findings
The
long-term effectiveness of the training was not monitored
|
|
Building
provincial mental health capacity in primary care: an evaluation
of Project ECHO mental health program
|
Sockalingam
(2018)[53]
Canada
|
PCPs
including family physicians, nurse practitioners, nurses, social
workers, counsellors, and other allied health professionals from
rural health integration networks
|
To
evaluate a mental health and addictions-focussed ECHO Ontario
Mental Health (ECHO-ONMH) program on improving primary care
knowledge and competency, specifically provider self-efficacy
related to mental health and addictions care
|
131
participants
26 sites
Oct 2015
- June 2016
|
Pre-/post-test
knowledge and self-efficacy surveys
Weekly
satisfaction surveys
5-point
Likert scale
Moore's
evaluation framework (first 4 levels) - Level 1: participation,
Level 2: satisfaction, Level 3: learning, Level 4: competence
Bandura's
theory of self-efficacy and guidelines for self-efficacy scale
development
The
ECHO-ONHM hub consisted of a team of specialised mental health
care at the Centre for Addictions and Mental Health (CAMH) and the
University of Toronto including psychiatrists with expertise in
child and youth, psychological trauma and medical psychiatry,
family medicine, addictions medicine, pharmacist, social worker
and health librarian
Intervention:
32
weekly, 2 hr ECHO-ONMH clinics, didactic lecture and case reviews,
written summary of recommendations
|
First
reported outcomes of ECHO model for mental health
Primary
outcome: PCP knowledge and perceived self-efficacy improved
post-ECHO (knowledge change was significant, p < 0.001;
self-efficacy approached significance p = 0.056)
Attrition
was low (77%)
Average
of 26% weekly attendance
Satisfaction
ratings were high - change in patient management; increased
diligence screening; increased knowledge
Future
studies will focus on determining how knowledge acquisition
translates to PCP practice patterns and patient health outcomes
|
Data was
obtained from a single province in Canada
Only
group mean scores were used so unable to compare individual
participant changes pre- to post-
Long-term
data is unavailable to determine sustained effects of ECHO-ONMH
Did not
capture data on primary care sites' practice change related to
knowledge increases in the management of mental health and
substance use disorders
|
|
Evaluation
of a national telemedicine initiative in the Veterans Health
Administration: factors associated with successful implementation
|
Stevenson
(2018)[54]
USA
|
PCPs and
clinical leaders, specialty care providers (SCPs) in pain
management, diabetes or cardiology, other providers (nurse
practitioners, pharmacists), support staff (medical support
assistants) from remote locations
|
To
provide guidance and support for the implementation and spread of
SCAN-ECHO
|
52
initial SCAN-ECHO surveys sent to 37 sites prior to implementation
June -
July 2012
55
interviews
2nd
survey 198/450 providers
77 sites
Sept
2012 - Jan 2013
|
Convergent,
mixed methods
2
quantitative surveys
Semi-structured
telephone interviews approximately 1-year post-implementation of
the initiative
Consolidated
framework for implementing research (CFIR)
Specialist
teams deliver SCAN-ECHO
Intervention:
SCAN-ECHO
12-18 month curriculum of didactic presentation and case studies
|
22
SCAN-ECHO leaders responded to initial survey viewing 14/39 CFIR
constructs as important
86%
agreed that SCAN-ECHO increased PCPs knowledge and competencies
All
sites expressed positive attitudes to SCAN-ECHO
Design
quality and packaging, compatibility and reflecting and evaluating
were 3/14 CFIR constructs that distinguished high and low
implementation sites
Complexity
of programme was a challenge for participants
Leadership
engagement - failure of leadership to provide protected time was
a barrier to participation
Recommendations
including: more effort given to developing and distributing
educational materials; restructure primary care staffing and team
composition such as engaging more nurse practitioners; establish
an audit and feedback mechanism for monitoring and improving the
programme, developing a formal implementation blueprint to reduce
complexity; obtain local leadership support for PCPs with
dedicated time for participation
|
Use of
only 9 sites for qualitative interviews limits the
generalisability of findings
Survey
data sample although larger, was still insufficient to achieve
significance
The
project was conducted in a large, integrated health system and it
is not known whether similar findings would be obtained in
smaller, community healthcare systems
|
|
Improving
pain care with Project ECHO in community health centres
|
Anderson
(2017)[9]
USA
|
PCPs
including internists, family doctors and family nurse
practitioners in medically underserved areas of Connecticut and
Tucson, Arizona
|
To
evaluate the impact of Project ECHO Pain on knowledge and quality
of pain
|
10
intervention group/10 comparison group
12
clinic sites at Community Health Center Inc, Connecticut
4 clinic
sites at El Rio Community Health Center, Tucson, Arizona
48 ECHO
Pain sessions
107
unique patients
Jan -
Dec 2013
|
Quasi-experimental
Pre-/post-test
with comparison/control group
Mixed
methods
Surveys
KnowPain-50
(KP50) pain care knowledge assessment tool
6-point
Likert scale
Focus
groups
Statistical
analysis
A
multidisciplinary team of pain specialists in anesthesiology/pain
medicine, behavioural health, occupational medicine, addiction
medicine, Chinese medicine/acupuncture and primary care from the
Integrative Pain Center of Arizona (IPCA) delivered Project ECHO
Intervention:
48,
weekly, 2-hour Project ECHO Pain sessions included 20-30 min
didactics and 3-4 case presentations
|
Compared
with the control group, PCPs have a statistically significant
increase in pain-related knowledge and self-efficacy (p <
0.001)
PCPs
suggested that they had acquired knowledge that they were able to
apply in their practice
Increased
referrals to behavioural health and physical therapy
Significant
reduction in prescribing of opioids
Further
research is needed to assess whether the knowledge leads to
lasting improvements in adherence to guidelines and improvement in
patient outcomes
Studies
are underway to assess the impact of Project ECHO Pain with a more
limited time commitment
|
Absence
of data on dosage of opioids prescribed limits conclusions that
can be drawn
Changes
in knowledge following the intervention were relatively small to
account for the change in behaviours of the intervention group
|
|
Telemedicine
specialty support promotes Hepatitis C treatment by primary care
providers in the department of veterans' affairs
|
Beste
(2017)[15]
USA
|
PCPs in
21 regions of USA nationwide (including rural)
|
To
assess whether primary care provider participation in Veterans
Affairs Extension for Community Health Outcomes (VA-ECHO) was
associated with hepatitis C treatment and sustained virological
response
|
152
sites, nationally
376
VA-ECHO PCPs
6431
VA-ECHO patients
559 case
reviews
3797
non-VA-ECHO PCPs
32,322
control patients
April
2011 - June 2015
|
Quantitative
Statistical
analysis
VA-ECHO
program was run by hepatitis C specialists from a regional hub at
1 of 7 tertiary facilities
Intervention:
1-2
weekly, 60-90 min sessions, brief didactics and case presentations
|
VA-ECHO
exposed patients were more likely to be rural (25%) vs unexposed
patients (20%)
The rate
of PCP-initiated antiviral medication was 214% among referred
patients for case review on VA-ECHO compared with 25% for control
patients
VA-ECHO
patients without individualised case review had similar treatment
rates compared to unexposed patients
No
difference in sustained virological response for patients with
exposed primary care providers
Cost-effectiveness
and sustainability remain to be demonstrated
Future
randomised controlled trials to clarify effects of the ECHO model
|
Participation
in VA-ECHO was voluntary
Each VA
region had the authority to tailor its didactic curriculum
therefore the curriculum was heterogeneous
|
|
Telementoring
primary care clinicians to improve geriatric mental health care
|
Fisher
(2017)[25]
USA
|
PCCs
including physicians, nurse practitioners, physician assistants,
care managers, social workers, pharmacy/medical students and
program managers in rural and underserved communities in
10 New
York counties
|
To
evaluate whether Project ECHO GEMH (geriatric mental health) is an
effective strategy to address geriatric mental health challenges
in rural and underserved communities
|
154
participants
54 sites
33 ECHO
sessions
Sep 2014
- Feb 2016
|
Mixed-methods
Claims
data analysis
Semi-structured
interviews
Specialists
in geriatric psychiatry, medicine, nursing, social work,
psychology and pharmacy from the University of Rochester Medical
Center (URMC) deliver Project ECHO GEMH
Intervention:
Didactic
sessions and case presentations on best practices related to
geriatric mental health care
|
26
participants were interviewed
Participants
reported improvements in clinician GEMH knowledge, confidence and
treatment practices, improved health outcomes for patients, and
increase in sense of professional support
Some
participants reported sharing information with colleagues had
changed treatment practices while other colleagues were not open
to new information
Health
insurance claims data suggest that emergency room costs decreased
for patients with mental health diagnoses
Additional
research is needed to understand the potential impact of program
on patient health outcomes, as well as long term impacts on health
care costs
Future
research should focus on opportunities to optimise and sustain
clinical engagement, effects of program dosage and long-term
impacts
|
The
study team was only able to interview a small portion of program
participants and interviews were voluntary
The team
only had access to utilisation and cost data from a single heath
plan
The
study focussed on select mental health disorders; other conditions
may influence outcomes of interest
|
|
Project
extension for community healthcare outcomes (ECHO) in multiple
sclerosis - in increasing clinician capacity
|
Johnson
(2017)[30]
USA
|
PCPs
including neurologists, psychiatrists, internists, family medicine
specialists, physician assistants, naturopathic physician in the
Pacific Northwest, including rural areas of Alaska, Idaho, Montana
and Washington State
|
To
determine the feasibility of using the Project ECHO telehealth
model to increase capacity and capability of clinicians in rural
areas to treat people with multiple sclerosis (MS)
|
24
clinicians
12
neurologists
3
psychiatrists
3
internists
2 family
medicine specialists
3
physician assistants
1
naturopathic physician
13 sites
38
unique case presentations
12-week
series
|
Pilot
Interviews
The MS
Project ECHO program included 3 neurologists, 2 psychiatrists, a
rehabilitation psychologist and a rehabilitation counsellor from
the University of Washington (UW) Medicine Multiple Sclerosis
Center and staff from the National MS Society
Intervention:
Weekly,
20-30 min didactic education sessions and 30-40 min case
presentations
|
The
primary barrier to participation was the time of day or time
constraints (9/15; 60%); participants were spread across 3 time
zones
67% of
participants (10/15) involved in follow-up interviews indicated an
increase in confidence in treating MS
60%
indicated that the program met their expectations and showed
interest in future participation
87%
appreciated having a mix of specialities represented
The
Pilot warrants further investigation regarding its potential
effects on access to MS delivery for underserved populations
|
It was a
challenge to get participants to come forward with cases due to
the small numbers of patients with MS
|
|
Telehealth
to
expand
community health nurse education in rural Guatemala: A pilot
feasibility and acceptability evaluation
|
McConnell
(2017)[38]
USA
|
Community
health nurses (CHNs) who conduct home and group visits for
pregnant women and children up to 3 years of age
in
rural Guatemala (population - 30,000 people)
|
To
evaluate the interactive education via telehealth to CHNs in rural
Guatemala via telehealth
|
Average
of 55 learners
2
instructors
10
lectures
|
Pilot
Pre-/post
test
Surveys
Likert
scale (1-4) to rate statements regarding lecture content,
technology & personal connection
Statistical
analysis
Instructors
were a lead paediatrician, 2 other Paediatricians, a Paediatric
nurse practitioner and a recent medical school graduate from
Center for Global Health at University of Colorado
Child
health lectures organised into two blocks of 5 topics - selected
based on CHNs preferences and instructor availability
Intervention:
30
min of didactic lectures and 15 min for questions, case
presentations and discussions of current cases and experiences in
the community
|
Pilot
results from survey responses from instructors and learners were
combined across 10 lectures
Survey
questions assessed knowledge gain as measured by percent
improvement per subject & overall pre to poste scores overall
was 109%
Learners
evaluation was overall positive especially regarding lecture
content, strongly positive for technology questions regarding ease
of use and convenience Learners were better able to hear the
instructor at 94.5% than see them at 87.3% 94.5% agreed that
lecture via telehealth was as good as in person
3
lectures rescheduled due to lack of internet connection at the
site in Guatemala - Internet connection most frequently took 5-10
min Instructors evaluation - audio quality was better than video
quality 100% agreed upon ease and convenience
Strengths
were low start-up costs and minimal resources needed to develop
and implement the program
Major
advantage using telehealth technology over web-based e-learning is
the ability to have real time interaction and active participation
that facilitates question, receiving clarification and discussing
case presentations
|
Specific
cost effectiveness analysis was not performed as the set-up of
equipment, bandwidth, licensing of software Faculty & CHN
salaries were all including free of charge
Paucity
of data overall - especially in the educational (non-direct
patient care) usage of telehealth - likely due to equipment,
time & software used are shared among projects in an academic
setting therefore no tracking of costs spent or saved with
specific telehealth program
Instructor
& learner time commitments were not calculated in the
evaluation
CHNs
completed surveys anonymously, preventing pairing of pre and post
test scores or the ability to adjust for lecture attendance -
this was done to encourage full participation and remove concerns
the CHNs may have to relation to job performance
Small
data set
Unable
to define if the knowledge gain was translated to better work
performance
|
|
Mixed-method
study of uptake of the extension for community health outcomes
(ECHO) telemedicine model of rural veterans with HIV
|
Moeckli
(2017)[40]
USA
|
Human
immunodeficiency virus (HIV) specialists, PCPs and administrators
in West Coast and Midwest metropolitan and rural areas
|
To
evaluate 3 HIV ECHO programs in the VHA, focussing on uptake of
primary care clinics and veterans
|
31
participants
21
primary care clinics
|
Mixed
methods
Data
analysis
Semi-structured
interviews
HIV ECHO
was run by physicians, pharmacists, psychologist and /or nurse
case managers with expertise in HIV from the University of Iowa
Intervention:
Didactics
and discussion of cases presented
|
43% of
primary care clinics adopted HIV ECHO
HIV ECHO
had limited uptake due to sense that HIV care should not be
integrated into the wider primary care system, a reluctance to
share ownership of care between specialty and primary care clinics
and a perception that HIV care is too infrequent to drive the
program.
Incentives
to adopt HIV ECHO included a perception of improving access to
care for patients, professional development and trust in the HIV
ECHO team
|
Did not
interview PCPs who refused to participate in HIV ECHO, who may
have had unique perspectives
Did not
examine process or outcome measures of HIV care quality
|
|
Using an
innovative telehealth model to support community providers who
deliver perinatal HIV care
|
Ness
(2017)[41]
USA
|
PCPs in
low resource and rural settings in Washington, Alaska, Montana,
Idaho, Oregon and Colorado
|
Evaluate
the impact of an ECHO telementoring program on the management of
perinatal HIV
|
53
community clinicians
13
patient cases
|
Longitudinal
Embedded
mixed methods
Surveys
Mountain
West (MW) AETC (AIDS Education and Training Centre) and University
of Washington
Intervention:
15
min didactic update on clinically relevant topics, followed by
brief question and answer period; and 1 hour of case consultations
and discussion using de-identified cases; written final
recommendations
|
77.4%
response rate for survey completion
100% of
providers reported that ECHO had "very much" impacted
management of the case
All
cases had the successful outcome of prevention of mother-to-child
transmission of HIV
88% of
providers reported increased knowledge
93% of
providers reported that ECHO had increased awareness of perinatal
guidelines
30% had
acted as a resource to colleagues and 42% used knowledge gained to
help colleagues manage patients
Future
studies should evaluate the cost-effectiveness, assess the
community level impact and impact on provider turnover
|
Survey
responder bias may exist
Surveyed
only active ECHO participants (selection bias)
Patient
case sample size is small
Limited
information provided to the ECHO network
|
|
Development
of a sleep telementorship program for rural Department of Veterans
Affairs PCPs: sleep veterans' affairs extension for community
healthcare outcomes
|
Parsons
(2017)[44]
USA
|
PCPs
including licensed independent practitioners (medical doctors and
advanced registered nurse practitioners), registered nurses,
pharmacists and occupational and respiratory therapists in
Northwest
VA Health Network of Alaska, Washington, Idaho, Oregon, Montana
and California
|
To
describe the feasibility of the VA-ECHO program for sleep medicine
- Sleep VA-ECHO
|
39
participants
26
primary care
7 mental
health
6 other
specialties
25
unique sites
14
states
August
2014 - initial needs assessment sent to 63 participants
July 15,
2015 - October 1, 2015
|
Pilot
Descriptive
Survey -
individual session evaluation
Survey -
summative program evaluation (participants who attended at least
one session)
Survey -
quality improvement evaluation (participants who attended 2 or
less sessions)
5-point
Likert scale
Curriculum
development based on a need's assessment survey
Sleep,
pharmacy and mental health specialists from regional VA and
Department of Defence facilities and affiliated academic
institutions delivered Sleep VA-ECHO
Intervention:
10
stand-alone, 1-hr sessions combining didactics with integrated
case reviews
|
38% of
participants worked in rural healthcare
44%
completed the summative program evaluation
93% of
respondents anticipated practice change
80%
reported increased comfort managing common sleep complaints
especially sleep-disordered breathing, insomnia and post-traumatic
stress disorder
Follow-up
survey of invitees who attended 2 or less sessions reporting
scheduling conflicts (62%) and lack of protected time for
attendance (52%)
Future
work is needed to identify objective measures of practice change
and address participation barriers
|
Program
was conducted within an integrated, single-payer healthcare
network
Project
focussed on a small group of voluntary participants who may be
highly motivated
Project
focussed on participant perception of value and not objective
measures of practice change
|
|
Internet
or DVD for distance learning to isolated rural health
professionals, what is the best approach?
|
Rakototiana
(2017)[46]
Madagascar
|
Heads of
Health Based Centers (HBC) including doctors and paramedics (nurse
or midwife) in three rural regions of Miarinarivo, Moramanga and
Manjakandriana
|
To
compare the knowledge acquisition of the heads of HBC for the
management of hypertension using 2 training modalities-via
internet - videoconferencing (VS) and videoconferencing (VD)
(interactive), and via DVD (non-interactive)
|
56
doctors and paramedics via VS or VD
36
doctors and paramedics via DVD
|
Empirical
quasi-experimental study
Mixed
methods
Pre-/post-test
Questionnaires
Focus
groups
Statistical
analysis
VS was
delivered by Medical Institute of Madagascar, VC and DVD was
delivered by Faculty of Medicine Antananarivo
Intervention:
2-hours
videoconferencing (VS) and videoconferencing (VD) (interactive),
and via DVD (non-interactive)
|
By
modality
Retention
of knowledge using both methods of delivery demonstrated no
difference in the mean score of knowledge obtained (p = 0.076)
By
profession
In the
internet group the average score after training for both the
doctors and paramedics was the same (not significant)
Doctors
using internet vs DVD was significant (p = 0.008) DVD group showed
greater retention
The
paramedic group showed an identical gain in knowledge in both the
internet and the DVD group
Acceptance:
All
participants had issues with both methods, but DVD was able to be
re-watched which meant that could do so if did not understand
anything-with internet could not do this. Could not ask
questions in either modality
DVD
cheaper to implement, and better accessibility as internet
coverage not equal across whole of country
Recommendations:
If
internet access available choice should be made between internet
delivery or DVD
If
internet access patchy then DVD would be best choice
|
No
randomisation used to group participants
Limited
bias as overall score for basic knowledge was same for both groups
prior to training
|
|
Videoconferencing
and telementoring about dementia care: evaluation of a pilot model
for sharing scarce old age psychiatry resources
|
Doyle
(2016)[24]
Australia
|
Healthcare
professionals in regional, rural and remote areas of Victoria and
Northern Territory (NT) managing clients with dementia
|
To
evaluate a pilot expansion of mentoring and consultation services
to test a model for improving medical supervision and clinical
governance for staff within regional and remote areas using remote
information technology
|
18
dementia service staff, including staff from linked services and
psychiatrists in regional Victoria and NT
58
interviews were conducted
18
education sessions were conducted remotely
352
staff attended the sessions
186
evaluation forms returned
|
Pilot
Mixed
methods
Using
before, mid-point and post-implementation semi-structured
interviews and questionnaires to examine orientation, acceptance &
impact underpinned by theoretical approaches to evaluation
Likert
scale from strongly agree to strongly disagree - 3 open ended
questions
Old age
psychiatrists located at Victorian and NT Dementia Behaviour
Management Advisory Services (DBMAS) sites delivered the model
Intervention:
Weekly
(reduced to monthly), 1-hour teleconference and web-based team
case presentations and education sessions
|
Education
sessions
Participants
strongly agreed or agreed to the five-statement indicating
acceptance and satisfaction with the program
High
satisfaction received for relevant topics to learning needs
Training
techniques rated the lowest - this was mainly related to
dissatisfaction with the quality of audio and VC facilities
Case
conference outcomes
Closed
questions form case conference interviews - 59% clinicians felt
the process was acceptable and improved impacts for clients
through their increased confidence in managing clients with BPSD
Overall,
clinicians reported that case conference process contributed to
improved outcomes for clients, family and staff
Almost
all staff considered the pilot increased their access to
professional development opportunities
Particularly
beneficial for sole clinicians in the NT who are professionally
isolated as they could access professional development,
multidisciplinary team, peer support, debrief opportunities
Future
education topics were identified
Reduction
in travel time across large geographical area utilising VC for
education and case conferences
Use of
technology proved to be a big challenge
IT
difficulties were audio feedback and sound quality issues -
problems stemming from overloaded hospital-based servers resulting
in intermittent outages and delays
Time and
frequency of session was found to be a critical factor in
attendance
|
Lack of
direct input from family carers or people living with dementia
Inability
to analyse full recording of interviews - leading to crucial
pieces of information being missed
|
|
Expanding
health care access through education: dissemination and
implementation of the ECHO model
|
Katzman
(2016)[33]
USA
|
PCPs and
specialists in rural (and urban) underserved areas
|
To
create a replication and training tool of the ECHO model for the
Army's Pain Management ECHO Pain collaboration - ECHO Hub
Readiness Replication Model to ensure fidelity, create consistency
in the replication process and be adaptable for use by all ECHO
programs
|
150
participants
25%
physicians
18%
mid-level providers (nurse practitioners, physician assistants,
pharmacists or psychologists)
10%
licensed rehabilitators
12%
nurses or nursing assistants
35%
other specialists (integrative medicine providers, health
technicians etc)
|
Mixed
methods
Surveys
of ECHO Pain boot camp
Focus
groups for hub clinicians
Hub
readiness ECHO (4-phase) replication model to create consistency
Specialty
care teams delivers the program from 4 hubs of Northern Regional
USA, Southern Regional USA, Pacific Regional and Europe Regional
Medical Command sites
Intervention:
cased
based learning and evidence-based didactics
|
Four
phases of the model are deliberate and add fidelity to the
original four-point model
Surveys
demonstrated that both on-site and virtual participants had an
increase in knowledge of pain management
During
the roll-out participants were eligible to receive over 9,689
hours
The tool
can be easily adopted for all chronic and complex diseases and
conditions across a large enterprise
Provides
flexibility to account for personnel and geographical variation
ECHO
Pain has helped to replicate the ECHO programs for many other
healthcare-related entities and has the potential to improve the
fidelity of the ECHO replication efforts around the world
|
Limitation
of dedicated time and multiple competing priorities are
constraints for hub clinicians
|
|
Evaluation
of American Indian Health Service training in pain management and
opioid substance use disorder
|
Katzman
(2016)[32]
USA
|
Indian
health service (IHS) clinicians from large rural areas in the
West, Southwest and Midwest regions including Arizona, New Mexico,
Minnesota and Oklahoma
|
To
examine the benefits of IHS training in pain management and opioid
substance use disorder to address the high rates of unintentional
drug overdose in American Indians/Alaskan Natives
|
1079
clinicians
92% from
IHS, tribal or urban AI/AN programs
28
states
January
2015
|
Descriptive
Pre-/post-test
Surveys
Statistical
analysis
Facilitators
at the IHS Pain and Addiction TeleECHO clinic and University of
New Mexico Pain Center and ECHO Pain
Intervention:
7,
5-hour training courses in pain and opioid substance use disorder
didactics
|
Significant
improvement (p < 0.001) in pre-/post- course knowledge,
self-efficacy and attitudes
Thematic
responses showed the trainings to be comprehensive, interactive
and convenient
Participants
suggested that training sessions be shorter, more frequent and
adaptable, include more details on pain medications and resolve
some technical issues
|
|
|
Project
ECHO (Extension for Community Healthcare Outcomes): a new model
for educating PCPs about treatment of substance use disorders
|
Komaromy
(2016)[36]
USA
|
PCPs in
underserved areas
|
To
describe a teleECHO clinic that is focussed on treatment of
substance use disorders (SUDs) and behavioural health disorders
(BHDs)
|
654
unique participants
900
unique patient cases
|
Brief
Report
Descriptive
Recruitment
for buprenorphine training (DATA-2000 waiver)
Specialists
in treatment of SUDs and BHDs at University of New Mexico Health
Sciences Center (UNMHSC) delivered the program
Intervention:
30
min didactic session followed by de-identified case presentations,
recommendations are summarised and sent to participants
|
An
average of 147 participants joined each year since 2008.
285
participants have attended more than one session since 2010.
Opioids
are the most commonly discussed substances (31%), followed by
alcohol (21%) and cannabis (12%)
ECHO
model provides an opportunity to promote rapid expansion of
information on new research and epidemiological trends
|
|
|
Service
providers' experiences of using a telehealth network 12 months
after digitisation of a large Australian rural mental health
service
|
Newman
(2016)[43]
Australia
|
Telepsychiatry
service providers including rural mental health teams, directors
of nursing at rural hospitals, metropolitan-based psychiatrists
and registrars, the metropolitan-based mental health team
dedicated to rural provider support, rural GPs, administrative
staff, and the executive group of the state rural health
department in rural and remote South Australia
|
To study
service providers experience of an existing regional telehealth
network for mental health care practice 12 months after
digitisation in order to identify the benefits of digital
telehealth over an analog system for mental health care purposes
in rural Australia
|
Over 40
service providers in South Australia ranging from metro central
operations to health providers up to 600km away in same state
70 sites
June -
September 2013
|
Mixed
methods
Qualitative
interviews
Focus
groups
Fieldwork
was conducted 12 months after digitisation was introduced
Thematic
analyses, focusing on 3 key areas on innovation diffusion theory:
relative advantage, technical complexity and technical
compatibility
Intervention:
Enhanced
telehealth network (Digital Telehealth Network - DTN)
|
Staff
support
Remote
clinical supervision of social workers and mental health staff
Education/training
Therapy
training
Peer
support
Clinical
case review meetings - clinical learning opportunity and
building team rapport
Improved
clinical practice
Analysis
identified 5 themes and 11 sub-themes
Digitised
telehealth network results in a range of relative advantages in
access and quality of mental healthcare patients in rural and
remote areas
Service
providers need support to overcome challenges of achieving
compatibility of telehealth with clinical practice
The
development of staff training and sharing of innovative uses could
help overcome challenges
Greater
uptake could be encouraged by service providers being given time,
cost and staff support for use (especially GPs)
|
Paper
provided the experiences of providers who had prior experience
with an analog system and who were reflecting in the interviews
Study
did not include the views of the patients or their families
|
|
Improved
glycemic control on veterans with poorly controlled diabetes
mellitus using a specialty care access network-extension for
community healthcare outcomes model at primary care clinics
|
Watts
(2016)[56]
USA
|
PCPs at
2 remote rural sites within the Cleveland VA hospital network
|
To
determine the efficacy of the Cleveland Veteran Affairs SCAN-ECHO
program for diabetes mellitus
|
2 PCPs
2
mini-clinics/outpatient sites
39
patients
19 Dec
2012 - 28 Mar 2014
|
Retrospective
chart review
Intervention
group: 2 "SCAN-ECHO clinics"/Control group: 2 "usual care
clinic"
Statistical
analysis
An
endocrinologist, health psychologist, nurse practitioner a
registered dietician (who are certified diabetes educators)
deliver the ECHO program from Cleveland VA Medical Center
Intervention:
24
sessions per year, 20 min didactic discussion, 2-3 case studies
and management recommendations
|
Mean
glycolated haemoglobin (HbAIc) improved over the follow-up period,
which was statistically significant (p < 0001)
Statistically
significant chance that the HbAlc percentages increased over time
in the comparison clinics
Future
research: randomised-controlled study of usual care vs
mini-clinics
|
Retrospective
analysis of patients who agreed to partake
Non-randomised
study
Aggregate
clinical data was used due to lack of individualised patient data
limits the analysis of variance
|
|
Impact
of telehealth program that delivers remote consultation and
longitudinal mentorship to community HIV providers
|
Wood
(2016)[57]
USA
|
HIV
practitioners in rural and underserved areas
|
To
describe key components of the program, report types of clinical
problems requested, and evaluate changes in participants'
self-assessed HIV care confidence and knowledge
|
45
clinicians
172 ECHO
sessions
553 case
presentations
1051
clinical questions
Feb 2012
- Aug 2015
|
Prospective
Pre-test/post-test
Surveys
Provider
self-efficacy assessments
Statistical
analysis
A
multidisciplinary team of academic specialists experienced in
infectious disease, psychiatry, addiction medicine, pharmacy and
social work at MW AETC and University of Washington
Intervention:
Weekly,
interactive video session, 15 min didactic update on clinically
relevant topics, followed by brief question and answer period; and
1 hour
of case consultations and discussion using de-identified cases;
written
summaries of the panel's recommendations and key points from the
discussion
|
Providers
most frequently sought consultation for changing antiretroviral
therapy, evaluating acute symptomatology and managing mental
health issues
Significant
increase (p < 0.05) in participants' self-reported confidence
to provide essential HIV care
Significant
increase in feeling part of an HIV community of practice
Significant
increase in feeling professionally connected to academic faculty,
correlating with level of program engagement
|
Varying
length of time between first and last self-assessment
Variations
in level of engagement of those surveyed
Reliance
on provider self-reported outcomes
|
|
Evaluation
of a telementoring intervention for pain management in the
Veterans Health Administration
|
Frank
(2015)[26]
USA
|
PCPs
from regional VHA networks - VA medical centres, urban
community-based outpatient clinics (CBOCs) and rural CBOCs
|
To
evaluate the impact of the pilot, VHA's SCAN-ECHO pain
management program (SCAN-ECHO-PM) on primary care delivery of
multidisciplinary pain care
|
322,435
patients with chronic, noncancer pain (CNCP)
159 PCPs
with 22,454 exposed patients; 257 patient cases were presented at
SCAN-ECHO-PM
8643
non-participating PCPs with 299,981 patients
7 VHA
regional networks
July
2011 - December 2013
|
Longitudinal,
observational
Pre/post
comparison
Pain
care specialists in physical medicine, mental health, substance
use disorder and specialty pain services, nonopioid
pharmacological management delivered the program
Intervention:
60
to 90 min sessions, 1-2 weekly, didactic and case presentations on
images submitted for consultation
|
12.9%
(exposed and 9.1% of unexposed patients were from rural CBOC
SCAN-ECHO-PM
was associated with an increase in use of physical medicine
services and initiation of nonopioid medications among patients
with chronic non-cancer pain, but not mental health, substance use
disorder or specialty pain clinics
Further
studies are needed to address facility-level barriers to uptake of
SCAN-ECHO-PM program
|
Provider
participation was voluntary
Exposure
measure did not indicate the quality or intensity of the training
delivered to participating providers
Delivery
of curricula may vary across sites or over time
Utilisation
of outpatient care or medications has not been captured outside
the VHA networks
Not able
to assess the impact on patient-centred outcomes eg functional
status and quality of life or appropriateness of pain management
decisions on individual patients
|
|
Treating
hepatitis C in American Indians/Alaskan natives: a survey of
Project ECHO (extension for community healthcare outcomes)
utilisation by Indian health service providers
|
Pindyck
(2015)[45]
USA
|
Navajo
Area Indian health service (NAIHS) providers including physicians,
pharmacists, physician assistants and nurse practitioners for
American Indians/Alaskan natives (AI/ANs) in Arizona, New Mexico
and Utah
|
To
delineate IHS-specific barriers to utilising the University of New
Mexico (UNM) HCV TeleECHO clinic by surveying NAIHS providers
interested in treating HCV
|
13 NAIHS
providers mentored to treat at least one patient with HCV ECHO
25 NAIHS
providers with an interest in HCV ECHO
15
facilities
March
2013 - 2014
|
Surveys
Statistical
analysis
Active
participant survey (APS) IHS providers mentored to treat at least
one patient with HCV ECHO
Non-participant
survey (NPS) sent to IHS providers with an interest in HCV ECHO
UNM
academic medical centre specialists provide ECHO services
Intervention:
Monthly
IHS exclusive HCV TeleECHO clinics with VC technology
|
100% of
respondents rated being well-informed, self-efficacy, access to
expertise, collegiality and decreased professional isolation as
moderate to major benefits
50% of
APS respondents stated they would not treat HCV without regular
participation in the clinic
67% of
NPS respondents reported lack of administrative time as the major
barrier to utilising this resource
|
Due to
the limited scope of the study a power analysis was not conducted
Survey
results are limited by the inherent biases associated with
self-reporting and the limited number of respondents
|
|
Innovative
telementoring for pain management: Project ECHO Pain
|
Katzman
(2014)[31]
USA
|
PCPs
including physicians, physician assistants, dentists and nurse
practitioners in rural and underserved communities
|
Assess
over a 3-year period how the Chronic Pain and Headache Tele-ECHO
Clinic (ECHO Pain) met the objectives, and quantify attendance and
case presentation data
|
763
participants
42%
physicians/dentists
19%
mid-level clinicians
9% other
clinicians
30%
nurses/other
3835
instances of participation
191
sites
29
states
Jan 2010
- Dec 2012
|
Mixed
methods:
Surveys
5-point
Likert scale
Focus
groups
Statistical
analysis
Annual
clinical data
ECHO
pain specialists at UNM facilitate the clinics
Intervention:
Weekly,
30 min didactics, 2 or 3 de-identified case-based presentations,
demonstrations and written summaries
|
Statistically
significant improvements in participant self-reported knowledge,
skills and practice were demonstrated
Focus
group (14 participants) analyses of 5 topics detailed specific
practice improvements through learning and applying concepts and
new knowledge from case presentations and didactics to their
patients
Future
studies will investigate this model within certain replicating
sites and health care systems
|
|
|
Palliative
care professional education via video conference builds confidence
to deliver palliative care in rural and remote locations
|
Ray
(2014)[47]
Australia
|
Rural
health practitioners including medical students, doctors, nurses
and allied health professionals (occupational therapists,
physiotherapists, speech pathologists and social workers) across
North QLD
|
To
evaluate the educational impact of video conferencing to increase
confidence among doctors and other health professionals to provide
quality palliative care in rural and remote areas
|
174
rural health practitioners
101
health professionals completed the study
10
Medical doctors/students
71
Nurses
5
Occupational therapists
4
physiotherapists
2 speech
pathologists
5 social
workers
4 Other
34
worked in outer regional areas
35
worked in inner regional areas
28
worked in remote location
4 worked
in very remote location
|
Mixed
methods approach with a qualitative component that utilised the
RATS guidelines on qualitative research
Quantitative/qualitative
Surveys
Educational
needs - pre-intervention assessment
4
monthly, evaluation surveys - post intervention
Statistical
analysis
Accessibility/Remoteness
Index of Australia (ARIA) scores were used to categorise locations
Members
of the tertiary level multidisciplinary palliative care team and a
palliative care researcher delivered the video conferences
Intervention:
Monthly,
education lecture-style sessions on palliative care followed by
case-based discussion and sharing of resources
|
Participants
rated the content of the video education useful
No
significant effect on profession was found (p = 0.088) but there
were significant differences in rating of effect between allied
Health professionals and both medical doctors (p = 0.033) and
nurses (p= 0.018) suggesting that allied health professionals
found it less useful that nurses and doctors
No
significant difference in content usefulness based on location of
work
Medical
students/doctors had the highest confidence in palliative care
topics pre-intervention, followed by nurses, then allied health
professionals
Allied
health professionals had significant lower confidence than nurses
(p = 0.018) and medical doctors/students (p = 0.013)
Participants
in inner and regional rural areas had lower confidence in
palliative care that those in rural areas
There
was an increase in confidence in the VC palliative care education
across all participants with no difference between location
Doctors
reported the highest level of confidence but there was no
significant difference between the professions
The
number of patients with palliative care issues affected had a
significant impact on the confidence change with education-those
caring for less than 5 pts had a greater confidence change
Results
indicate that locally generated content and the ability to deliver
education repeatedly enhanced confidence across all participant
groups
The VC
education was found to be valuable with staff with greater than 20
years finding it beneficial
The
discussion that occurred between rural and remote practitioners
with tertiary sites assisted to enhance professional networks
The VC
education sessions that were provided demonstrated that they met a
significant need for rural practitioners by providing regular
opportunities for education, professional support and maintaining
confidence in their ability to provide palliative care in their
context
Further
research required to explore other aspects of palliative care in
rural and remote areas
|
Finding
of study cannot be generalised as participants self-selected to be
involved were limited to those with work email addresses, access
to computers and those who were willing to take time to complete
surveys
|
|
The
educational impact of the Specialty Care Access Network-Extension
of Community Healthcare Outcomes program
|
Salgia
(2014)[49]
USA
|
PCPs
including physicians, physician assistants, and nurse
practitioners in rural and underserved areas of the VHA network in
Michigan, Indiana, North-western Ohio and east-central Illinois
|
To
determine factors that led to participation in the SCAN-ECHO liver
program and the educational impact of the program
|
55
participants
203
cases
183
unique patients
24
survey participants
13 (54%)
physicians
4 (17%)
physician assistants
7 (29%)
nurse practitioners
14 sites
June
2011 - Sep 2012
|
Descriptive
Pilot
Surveys
Specialists
in liver disease deliver the SCAN-ECHO program from the VA Ann
Arbor (tertiary care) Medical Center
Intervention:
Twice
monthly, pre-recorded didactic session and "live" case
presentations
|
More
than 75% participated in more than one SCAN-ECHO clinic
76%
indicated that the motivation for participation was to learn more
about liver disease
75%
applied the knowledge they gained to future patients
75%
desired to increase collaboration with specialists
71%
reported that the didactic component and case-based discussion
were equally important
75% had
personally discussed information that they had learned from the
case presentations with colleagues
42% had
helped a colleague care for their patient with their learned
knowledge
42%
indicated that preventing professional isolation was important
77%
indicated the main barrier to participation was their time
schedule
|
Survey
design - the potential for recall bias depending on the time
between provider participation in SCAN-ECHO and survey completion
Majority
of questions were choice questions - to overcome contextual
interpretation of answers providers were given the option of
free-text responses
Survey
studies are limited by response rates
Potential
for social desirability bias, as providers who like the SCAN-ECHO
program are more likely to respond favourably
|
|
Continuing
Distance Education: A capacity-building tool for the de-isolation
of care professionals and researchers
|
Bagayoko
(2013)[13]
Switzerland
|
Healthcare
professionals (HCPs) including general practitioners, nurses,
medical assistants, midwives and others, using RAFT (Telemedicine
network in French Speaking Africa) in isolated care facilities in
African countries
|
To
evaluate the impact of distance continuing education to build
capacity, increase satisfaction and enhance the performance of
care professionals in isolated health care facilities
|
39 HCPs
completed surveys
33%
general practitioners
28%
nurses
13%
medical assistants
8%
midwives
18%
other professionals
17
African countries with more than 100 connected sites
|
Descriptive
Survey
62
questions
Likert
scale 1-5 designed to probe 11 domains
Statistical
analysis
An
educational committee consisting of 6 RAFT local leaders
(including a recognised medical authority and a medical
co-ordinator who is a junior physician) coordinates the
educational program
Intervention:
weekly
webcast followed by 30 min discussion
|
87%
completed surveys
Results
suggest that the availability of eHealth access for continuous
education, improves retention and facilitates the recruitment of
young health care professionals to remote locations
Access
to continuing medical education is consistently considered the
most important with a preference for live, interactive courses
The
possibility to interact with other HCPs is particularly important
Intermittent
connectively and mobility are important key drivers of accessing
information - the system has been upgraded to allow courses to
be downloaded when the user has connectivity and played on mobile
devices later
|
Focusses
on reporting education platform
No
context or focus on clinicians
|
|
Pilot
project and evaluation of delivering diabetes work-based education
using video conferencing
|
Maltinsky
(2013)[37]
UK
|
Health
care professionals in peripheral settings within National Health
Service (NHS) in the Scottish Highlands regions of Fort William,
Golspie, South East Community Health Partnership, Lorne and
Islands
|
To
deliver teleconferenced diabetes training to healthcare and allied
healthcare professionals who provide base level care and
management of people with diabetes, and to evaluate this training
|
12
participants
face to
face group
2 sites
15
participants
videoconference
group
3 sites
|
Pilot
Short
communication
Descriptive
Semi
structured questionnaires
A
control group was established at two sites and content was
delivered in the traditional face to face method with the other
cohort using video conference in three sites
A
trainer from the Highland Diabetes Managed Clinical Network
delivered the educational package
Intervention:
Didactics,
practical demonstrations, discussion and question-and-answer
session
|
Pass
rates in both cohorts were similar 9/11 in face to face and 8/10
in video conference
Participants
attended training to upgrade their skills and gain confidence in
treating diabetes
Concerns
raised focused on moderate sound and picture quality, and the lack
of interactivity in VC compared to traditional face to face
education
Some
respondents noted that the decrease in travel/commute time
increased their willingness to enrol in training
Recommendations
include trainers require development sessions to enable them to
transfer their skills to a videoconference environment
Training
through videoconference should include regular breaks in order to
avoid eye strain and fatigue
|
Some
technical issues highlighted with video conferencing dropping out
Small
pilot
No
feedback sought from practitioners that chose not to undertake the
course and their reasons for not participating
Methodology
and what have been evaluated are unclear
Outcomes
are unclear
|
|
The use
of telemedicine to train perioperative nurses in rural settings
|
Seibert
(2013)[51]
USA
|
Perioperative,
registered (RN) nurses in rural areas of Idaho and Oregon
|
To
investigate whether a preceptor programme delivered by
telemedicine could be as effective as one delivered in person for
nurses working in the OR
|
35 RN
working within a perioperative area
22 RN
(telemedicine group) at 6 rural hospitals in Idaho and Oregon
13 RN
(person group) at 1 regional medical centre in Idaho
2007 -
2013
|
Comparative
study between a rural RN group and an urban RN group undertaking
an OR training program over a 6-year period
Rural
group - telemedicine preceptorship model
Urban
group - in situ preceptorship model
Both
groups undertook the AORN examination at the end of the course
Post
course completion satisfaction survey
10 RN
preceptors at an urban hospital delivered the programme
Intervention:
Self-paced
preceptor 26-module curriculum and weekly sessions of questions
and answers and setting weekly goals
|
No
significant difference between both groups in final exam
scores-all participants passed
No
significant difference in the time taken to complete the course
between both groups
No
significant difference in the clinical skills assessment scores
between both groups
Both the
telemedicine and urban RN groups thought the program was
successful (92% urban vs 91% telemedicine)
The
preceptors considered the program to be successful
86%
telemedicine group believed the course increased their knowledge
and would strongly recommend it to others
Both
telemedicine group and urban group education delivery models were
equally effective in training perioperative nurses
Variables
(sex, age, computer knowledge, prior hospital exp) did not affect
performance in the training
Research
suggests that telemedicine should be considered for training of
perioperative nursing and that it may be able to be generalised
across nursing in general
|
?? small
group/numbers
Due to
the lengthy time of research the program may have been tweaked to
improve it over time which may have biased the outcome?
? based
in the US do not know if it compares across other
countries OR training with educational content etc
|
|
Developing
telepsychiatry services in KwaZulu-Natal - an action research
study
|
Chipps
(2012)[18]
South
Africa
|
Psychiatrists,
medical offers and other staff in the rural province of
KwaZulu-Natal (UKZN)
|
To
develop telepsychiatry services in the province and to facilitate
change to the current psychiatric outreach services
Note:
Paper structure was hard to follow
|
12
participants
8
completed surveys
4
medical officers
1
medical student
1
manager
2 Other
3
hospitals
2009 -
2011
|
Mixed
methods
Action
research study
Cycle 1
& 2: Participant satisfaction survey
Cycle 2:
Qualitative Interviews
Pre-/post-test
surveys
Statistical
analysis
Teaching
staff from Department of Psychiatry at the University of UKZN and
a consultant psychiatrist and registrar from two hospitals
Intervention:
Telepsychiatry service including specialist and non-specialist
education in psychiatry and the provision of clinical
videoconference consultation as part of the routine clinical
outreach service.
Cycle
1:
Telepsychiatry -online remote interactive system of multiple
PowerPoint presentations
Cycle
2:
DVD sessions
|
5 mental
health professionals rated satisfaction with different bandwidths
and reported that 128Kbsp is suitable for education and 384Kbps is
preferred for clinical consultation
Videoconference
and DVD sessions were beneficial to health staff without
post-qualification psychiatry training
|
|
|
Building
capacity to reduce disparities in diabetes: training community
health workers using an integrated distance learning model
|
Colleran
(2012)[20]
USA
|
Community
health workers (CHWs) including paraprofessionals, promoters, lay
health workers and community health representatives in native
communities across New Mexico with direct involvement with
diabetes patients
|
To
determine whether the ECHO integrated distance training program
will increase CHW competence related to diabetes care
|
23
participants
21
completed
All
female
61%
Native American
35%
Hispanic
|
Mixed
methods
Pre-/post-test
surveys
Focus
groups
Statistical
analysis
Project
ECHO infrastructure delivered the teleECHO program
Intervention:
Two,
2-day, on-site training session and weekly teleECHO sessions of
didactics on program syllabus, case presentations and discussion,
informal discussions, question and answer, and resource sharing
6-month
program
|
Significant
improvement in participants' diabetes knowledge (p = 0.002),
diabetes attitude (p = 0.04), confidence in clinical and
nonclinical skills, respectively (p < 0.001 and p = 0.04)
Focus
group discussion reported that participant organisations and
systems currently do not provide the needed support and resources
Focus
group discussions indicated that participants gained competency,
confidence and resources for their work and communities
Studies
are ongoing to determine how participation affects the advancement
of role of CHWs and whether the training has a positive impact on
patient outcomes
|
Many
participants had trouble connecting to the weekly TeleECHO
sessions due to computer or internet access and they connected by
telephone instead
6-month
format created the potential for participant dropout - 2/23
dropped out due to retirement or relocation
|
|
Bridging
the distance: a prospective tele-oncology study in Northern Norway
|
Donnem
(2012)[22]
Norway
|
Cancer
health care providers including physicians, nurses, and others at
1 local hospital and in 5 remote communities in Alta (distance
from University Hospital of Northern Norway (UNN), 309 km), Vadso
(748 km), Honningsvaag (517 km), Karasjok (502 km), and Porsanger
(481 km) in Northern Norway
|
To
evaluate the feasibility and benefit of the use of
videoconferences (VCs) as a tool to support cancer health care
providers
|
106 VCs
101
patients
167
patient cases discussed
1
tertiary level hospital providing cancer services
1
smaller primary local hospital as well as
5 rural
area communities of health services
18-month
period from Spring 2009
|
Prospective
registration study
Descriptive
data, individual patient discussion via VC
Survey
Clinicians
at UNN deliver the teleconferences
Intervention:
Weekly,
VCs where clinicians discuss patient cases with specialist cancer
care service providers from a major tertiary facility
|
Days
waiting for a VC consultation was significantly shorter (p =
0.001) than the estimated waiting time for an alternative
consultation
Patients
stayed at their home facility in 82% of cases after VC
Transfer
and admission to tertiary facility reduced 13% to 6% with primary
health care providers expressing that VC improved patient care in
85% of cases
There
were minimal technical issues (77% of cases)
VC
appears to be a useful supplemental tool to support health care
providers in rural communities and primary local hospitals
Clinicians
felt that VC improved quality of patient care, made them feel more
confident that the care that they provide is adequate
Due to
significant difference in waiting times (VC versus alternate
consultation) it was felt that VC provided a more efficient
service for the patient
Use of
VC made local clinicians feel more confident in the delivery of
adequate care
|
Small
scale study that needs to be replicated before being able
generalise to greater population
|
|
Role of
telehealth/videoconferencing in managing cancer pain in rural
American Indian communities
|
Haozous
(2012)[28]
USA
|
Rural
health care providers including MDs, PAs, NPs, RNs, pharmacists
and health assistants caring for American Indian /Alaskan Native
(AI/AN) cancer patients at rural tribal clinics and hospitals in
Washington State and Alaska
|
To
determine the feasibility and effect of using telehealth/VC to
deliver cancer-related pain management education and case
consultation to health care providers in rural AI/AN communities
|
52
providers
11 sites
(62-922 miles from the nearest pain management specialist)
4
educational sessions
Average
17 providers/session
Average
5 sites/ session
93
providers from 16 non-duplicated sites (74-1127 miles from the
nearest pain management specialist)
9 case
conferences
Average
10 providers/session
Average
4 sites/ session
32
providers who did not attend the case conferences (comparison
group)
|
Cross-sectional
Descriptive
Surveys
Telehealth
satisfaction survey
Perceived
competence scale - 7-point Likert scale
Statistical
analysis
Consulting
pain management specialist at the University of Washington
delivered the educations sessions
Intervention
1:
Monthly video-conferenced educational sessions in cancer -related
pain issues
Intervention
2:
Case conferences - 15 min expert presentation; brief Q & A;
case presentations; management recommendations
|
46%
educational session attendees completed surveys
34% case
conference attendees completed surveys
Educational
and case conference participants both reported a high level of
satisfaction with the telehealth system
Case
conference participants scored a higher self-perceived competence
in treating pain compared with the comparison group
Future
studies with focus groups or interviews may provide a greater
analysis of program impact on participants, and strengths and
areas for improvement
|
Pre-tests
and post-tests were not implemented
No
randomisation of providers into telehealth and comparison groups
|
|
Project
ECHO: a model for complex, chronic care in the Pacific Northwest
region of the United States
|
Scott
(2012)[50]
USA
|
Clinicians
from (sparsely populated, rural) Pacific Northwest
|
To teach
rural providers how to evaluate and treat complex, chronic health
conditions including hepatitis C, chronic pain, integrated
addictions and psychiatry, and HIV/AIDS by using telehealth and
case presentations
|
900
clinicians
700
patient cases
2009 -
June 2012
|
Pilot
UW
clinicians presented the videoconference clinics
Intervention:
1-hour,
weekly videoconference - 15 min didactic session on a topic
relevant to the disease being discussed
|
23
videoconference clinics for Hepatitis C - 263 clinicians,
representing 399 patient cases
167
patients started antiviral therapy for Hepatitis C
Project
expanded to include:
16
clinics in addiction and psychiatry
97
clinics in chronic pain
13
clinics in HIV/AIDS
Plan to
provide clinics in other chronic, complex conditions, including
rheumatology, cardiovascular disease, chronic pulmonary diseases
and child psychiatry
|
Reluctance
of some participating clinicians to present cases
Unknown
methodology
|
|
Partnering
urban academic medical centres and rural primary care clinicians
to provide complex chronic disease care
|
Arora
(2011)[11]
USA
|
PCCs
including physicians, nurses, pharmacists, nurse practitioners,
physician assistants, health educators and community health
workers in underserved, rural areas
|
To
describe the Project ECHO model and discuss early results
|
34
participants in 12-month survey
94
participants in 2010 Project ECHO annual meeting surveys
|
Descriptive
2 survey
types
12-month
participation survey
Annual
meeting survey
Likert
scale
Statistical
analysis
Specialist
HCV team at UNMHSC, including a hepatologist, pharmacologist,
mental health specialist a nurse delivers the telemedicine clinics
Two-day,
in-person orientation in HCV treatment protocol as well as ECHO
model format
Intervention:
Weekly
2-hour telemedicine clinics - case-based learning, case
management, brief didactic presentations
|
12-month
survey:
88% of
PCCs agree with the importance of becoming well-trained in
hepatitis C care
58%
agree with the importance of becoming the local hepatitis C expert
91%
agree with importance of support of teleconference network
73%
agree with the importance of providing consultation to other PCCs
in the care of hepatitis C patients
1-day,
ECHO annual meeting survey:
94 PCCs
provided mean ratings of 3.66 - 4.73 associated with best
practice care, connecting with peers and enhancing professional
development and
60-72
PCCs strongly agreed with benefits to patients
The
model needs to be incorporated into the health care system so that
reimbursement mechanisms are created to pay for the various
services it provides
|
|
|
Enhancing
access to cancer education for rural healthcare providers via
telehealth
|
Doorenbos
(2011)[23]
USA
|
Healthcare
providers including physicians, nurse practitioners, nurses,
physician assistants and community outreach workers for AI/AN
people in rural Washington and Alaska
|
To
demonstrate that telehealth technology is a feasible method for
delivering real time, interactive cancer education to multiple
rural sites
|
368
participants (some participants attended multiple sessions
131
sessions
28
tribal clinic sites in Alaska and Washington State, mean of 5
sites joined the VC presentation
|
Open
ended survey
Written
satisfaction survey after each of the first 10 monthly sessions
Survey
used Likert scale questions to gather information about use of
telehealth for professional education sessions
Responses
were anonymous
Healthcare
providers were engaged in selecting topics
Experts
from Native People for Cancer Control Telehealth Network (NPCCTN,
including physicians, a nurse scientist, a nurse practitioner, a
clinical psychologist, a legal expert, and an Alaskan native
healer delivered the presentations
Intervention:
Monthly,
45 min cancer education series and 15 min Q&A
|
54%
returned the survey
Health
care providers in rural areas face barriers to obtaining
continuing education including geographic isolation, distance from
tertiary care, lack of financial resources for travel, inability
to take time away from work due to lack of coverage
Overall
satisfaction with telehealth was high, mean rating 3.6 on a
4-point scale
Participating
providers rated their feeling about telehealth prior to and after
their first educational session. Scores increased from 3.0 -
3.48, indicating use of telehealth improved in satisfaction
ratings
Usefulness
of information provided by educational sessions rated high with a
mean of 3.59
Open
ended responses supported the use of VC technology in making
continuing professional education a reality for rural healthcare
providers
The
cancer education series demonstrated that telehealth technology is
a feasible method for delivering real-time, interactive cancer
education to multiple rural sites
Telehealth
is a viable solution to the barriers faced by rural health
providers in obtaining continuing education
Incorporating
participant input during program planning enhances content
relevance for providers, and ultimately may enhance the delivery
of quality cancer care
|
Results
depend of the technology used
Technical
difficulties with VC delivery of education are typically minor
Lag in
audio transmission can hinder discussion when learners are from
two sites respond simultaneously
|
|
No
clinic left behind: providing cost-effective in-services via
distance learning
|
Knapp
(2011)[35]
USA
|
MD, PhD
and BA staff based at remote-located clinics (RLC) and
full-service medical centres (FSMC)
|
To
implement and examine the cost-effectiveness of a
distance-learning model to offer provider education in HIV to
geographically remote sub(facilities)
|
91
online participants
30 RLC
sites
129
in-person participants (control)
10 FSMC
sites
|
Descriptive
Comparative
study - Online training package vs in-person training for HIV
point of care testing
Surveys
Likert
scale
An RLC
clinical manager delivered the presentations
Intervention:
20-minute
power point presentation with 5 min Q&A and discussion
|
Participants
rated in-person presentations higher than online, however mean
scores for both methods were > 80%
Online
presentations were found to be considerably more affordable than
in-person
A
significant increase in HIV testing with a 200-300% increase in
testing among at-risk patients compared with the control site
which showed no improvement
Cost of
initiating in-person presentation in one state was five-fold
compared with the remote approach
|
A
potential limitation is that all states were already doing HIV
testing, so study was directed at tools and techniques to help
increase HIV testing
It is
unclear if remote learning would work for introducing a completely
novel intervention
|
|
Expanding
access to Hepatitis C virus treatment - extension for community
healthcare outcomes (ECHO) project: disruptive innovation in
specialty care
|
Arora
(2010)[12]
USA
|
PCPs in
federally qualified health centres (FQHCs) in rural and
underserved areas of New Mexico state and prisons
|
To
describe the ECHO model and its application in Hepatitis C virus
(HCV) care in detail and present data from initial surveys of
participants
|
415 HCV
telehealth clinics
21
participating HCV agencies
More
than 5000 patient consultations for HCV
69% of
patients are from rural areas and prisons
|
Descriptive
2 survey
types
6-month
participation survey
Annual
meeting surveys for 2006, 2007 and 2008
Likert
scale
Statistical
analysis
Multidisciplinary
specialists from UNMHSC in medical specialties, mental health and
substance abuse deliver the ECHO model
Intervention:
Weekly
2-hour telemedicine clinics - case-based learning, case
management, brief didactic presentations
|
HCV
providers reported after 6-month participation a significant
improvement in providers' knowledge (n=52); a source of learning
(n = 38), and professional satisfaction
Annual
meeting survey (2006) (n=17) reports a reduction in sense of
professional isolation, expanded access to specialists and
providers' professional enhancement
Annual
meeting survey (2006/2007) (n=25) reported an increase in
competence and ability to serve as local consultants about HCV to
other providers
Annual
meeting survey (2007) (n=25) reports a large degree of transfer of
knowledge to benefit care of other patients (with diseases not
represented at ECHO) and to clinical staff
Annual
meeting survey (2008) (n=23) reports a transfer of knowledge to
clinical care, confidence in patient safety and quality of care
and support in their clinical environment
Model
can be adapted to a broad range of chronic health issues
ECHO
model has expanded to cover 12 additional diseases
255
partner teams
More
than 10,000 patient consultations
|
Potential
of self-selection bias of respondents
The
number of ECHO HCV providers is small
|
|
Rural
professionals' perceptions of interprofessional continuing
education in mental health
|
Church
(2010)[19]
Canada
|
Mental
health professionals including community development workers,
doctors, nurses, nurse practitioners, occupational therapists,
recreational therapists, paramedics, dietitians, pharmacists,
police, school counsellors, social workers, youth workers and
clergy in 6 rural Newfoundland and Labrador (Canadian) communities
|
To
design and assess the impact of the Rural Mental Health
Interprofessional Training Program (RMHITP)
|
125
mental health professionals
37
nurses
35
social workers
8
community development workers
7 nurse
practitioners
7
police/justice
7
physicians
4
clergy/pastoral care
4
clerical staff
3
ambulance attendants/paramedics
3 school
counsellors/psychologists
3 youth
regional co-ordinators
2
dieticians
2
occupational therapists
2
recreational therapists
1
pharmacist
4 did
not indicate profession
45
completed a confidence questionnaire
15
professions
Sep 2006
- Dec 2007
|
Mixed
methods
Pre,
during, post
questionnaires
5-point
Likert scale
Written
feedback
Focus
groups
Interviews
Field
notes
Statistical
analysis
A
psychologist from the primary health care team in each rural
community delivered the sessions except for the one on crisis
intervention which was led by an outside expert
Intervention:10-session
program primarily via videoconference; 8 domains of mental health
practice
First 2
domains were presented on-site in 1 day
|
Program
had a beneficial effect on professionals with mental health
training and they attended more regularly
High
levels of satisfaction for all topics and all aspects of the
presentations, and opportunity to interact with other
professionals
Participants
reported developing a more reflective mental health practice,
integrating new knowledge and skills into their work
Increased
confidence using a range of mental health interventions
Interprofessional
referrals, inter-agency linkages and collaborations had increased
Least
satisfaction with videoconference technology was mitigated by the
strong connection between the facilitator and participants
Future
research will measure the impact of such a program on
professionals'
practice
and patient care
|
Not
possible to have a control group as study was one group,
pre-test/post-test
|
|
Virtual
grand rounds: A new educational approach in social work that
benefits long-term care providers and patients in rural Idaho
|
Cunningham
(2009)[21]
USA
|
Social
workers and residential care co-ordinators in rural Idaho
|
To
examine participant satisfaction of the Telehealth Idaho virtual
grand rounds (VGRs) education delivered via interactive
videoconferences and to promote retention in their workforce of
social workers and residential care co-ordinators
|
359
participants
July
2002 - Dec 2006
|
Quantitative
Questionnaire
Five-point
Likert scale
Specialist
presenters (often located outside Idaho delivered the VGRs
Intervention:
Telehealth
Idaho Program - Nine, 2.06 hours (per participant) sessions of
VGRs
|
79%
evaluation forms returned
Participants
approved of the delivery method and the overall satisfaction
rating was 4.1 out of 5
Whether
the information presented would result in a change in practice'
scored lower at 3.25
Overall
a positive score
Model of
education could easily be duplicated throughout regional centres
in the USA
This
model provided education to a cohort that may not have received or
been able to access previously; therefore, increasing knowledge
and decreasing cost for travel
The
program was expanded to include other facility staff and other
topics
|
Unclear
how many episodes of education was provided as individual episodes
Numbers
presented as a total of 359 attendees x 2.06 hours
The
familiarity of using the technology (set up and dialling in) and
the interaction would increase with the frequency of telehealth
education episodes and therefore improve the level of satisfaction
and potentially impact 'change of practice'
Content
was discussed but not how it was transformed into content that was
meaningful and relevant - as such a slightly lower 'change in
practice' score
|
|
Survey
of a videoconference community of professional development for
rural and urban nurses
|
Newman
(2009)[42]
Australia
|
Healthcare
professionals including registered nurses, clinical nurse
specialists, clinical nurse consultants, clinical nurse educators,
nurse managers, students, allied health professionals, mental
health workers and aboriginal health workers in rural and urban
regions of New South Wales (NSW)
|
To
present findings of a survey of a videoconference community in NSW
in 2008
|
75
participants
55%
completed the survey
4
hospital sites in NSW
Macquarie
- 46 participants
Wyong -
15 participants
Gosford
- 3 participants
Broken
Hill - 11 participants
|
Quantitative
Salmon's
principles of building online communities
access
and motivation, socialisation, information exchange and knowledge
construction
Surveys
Four-point
Likert scale
Intervention:
Videoconference
symposium (focus on videoconferencing) to build a learning
community among leading academic, researchers and clinicians in a
more accessible ways than by attendance at traditional conferences
|
56
attendees (55%) completed the survey
VC
technology has the potential to enable rural and remote healthcare
professionals to participate in a community for professional
development
Thorough
preparation, rehearsals and the presence of technicians minimised
possible technical difficulties that could be faced as cited in
literature
There
was overall success with respondents across the 4 areas indicating
positive results
The
attempted move toward knowledge construction was not successfully
achieved, despite encouragement of an interactive environment
It was
identified that more research needs to understand how to engage an
interactive environment, suggesting that a naturalistic approach
to communication that avoids a mediator at each site repeating
questions and channelling information may be productive
|
The
convenience nature of the sample and the response rate of 55% must
be factored into the interpretation of survey results
Temporary
loss of visual link with Broken Hill and Wyong which impacted on
timing of the symposium
Limitations
to the ability for those on screen to see the full audience at the
larger site of Macquarie
Questions
form the audience must be restated by the speaker or site convenor
for all community members to hear
|
|
Electronic
mentoring: an innovative approach to providing clinical support
|
Stewart
(2009)[55]
UK
|
Physiotherapists
in paediatric clinical practice in rural British Columbia, Canada
|
To
implement and evaluate a pilot e-mentoring programme to provide
support of rural physical therapists
|
1
experienced physiotherapist mentors
2 sole
charge physical therapists with no paediatric experience
3 months
in 2007
|
Pilot
Mixed
methods
Pre-test/post-test
questionnaires
Field
notes
Final
group meeting
7-point
adjectival scale
Action
research design
The
primary researcher, a physical therapist with 24 years of
paediatric experience assumed the role of mentor and delivered the
program
Intervention:
iChat -
2 times/week
Case
study -monthly videoconference meeting involving all 3
participants
|
Mentees
reported feelings of isolation dissipated with mentoring
Videoconferences
were helpful in developing clinical reasoning
It was
more difficult to type complex clinical questions than
articulating the questions verbally
Enabling
factors: technology (lack of technological problems), logistics of
communication flexibility and timing, attitude and commitment of
the mentor and mentee, the colleague-supporting-colleague
relationship
Mentor/mentee
interaction facilitated outcomes - communication through group
learning, improved clinical reasoning, confidence in clinical
decision-making and knowledge translation through skill building
and access to resources
Further
research is needed to evaluate long-term benefits and
effectiveness of e-mentoring
|
Sample
size and program length were chosen for pragmatic reasons -
conducted as part of a master's program
|
|
Continuing
professional development for Australian rural psychiatrists by
videoconference
|
Greenwood
(2008)[27]
Australia
|
Rural
psychiatrists and trainees in rural and remote areas of Australia
|
To
decrease professional isolation and facilitate opportunities to
obtain credit in ongoing professional registration and to provide
peer review for psychiatrists working in isolation
Overall
aim: to improve retention and recruitment of psychiatrists to
rural and remote areas
|
106
participants
67%
consultant psychiatrists
17%
trainees
16%
allied health professionals
6
seminars
June
2006 - June 2007
|
Mixed
methods
Online
surveys - evaluations were completed following each seminar
Qualitative
data was also obtained by telephone interviews with randomly
selected psychiatrists from each state and territory
Royal
Australian and New Zealand College of Psychiatrists (RANZCP)
members were surveyed for topic and speaker preferences
Intervention:
6
video-conferenced seminars - interactive participation between
rural psychiatrists and specialists
West
Australian Pilot peer review group - 6
participants/6 meetings: case presentations and discussions of
supervision issues
|
83% of
respondents found all six events they attended via VC beneficial
and preferred to attend seminars from remote sites than to travel
significant distances
84%
agreed that participating via VC reduced their feelings of
professional isolation
Concluded
that VC is now a proven, effective and accessible training mode
for the delivery of education to rural health practitioners
VC
enables live and synchronous exchange
|
Focus on
psychiatrists
Two
pieces of work included in the one article The National Program
and the WA Program
|
|
Bridging
the distance: Educating nurses for Telehealth Practice
|
Sevean
(2008)[52]
Canada
|
Registered
Nurses
(preoperative
and oncology) in remote communities of North-western Ontario
|
To
explore the impact of telehealth technology on health assessments
performed by nurses delivering health services to isolated
populations
|
5 nurse
educators
37
registered nurses
13
communities
|
Mixed
methods
Pre-
post- test
Pre-
workshop survey and a 42- item questionnaire to identify
demographics and learning needs was completed
Post
survey consisting of open- ended questions
Likert
scale
Statistical
analysis
Nurse
educators from the regional teaching hospital delivered the
presentations
Intervention:
1-day,
telehealth (videoconference) workshops included telehealth
protocols and policies, physical assessment skills, perioperative
skills and oncology assessment skills
|
Outlined
the advantages of using telehealth not only for nurses working in
remote locations but the benefits for families and community
members that reside in geographically isolated areas
Example:
Oncology - 2-year study - tele-hospice model
Highlighted
the need for a confidential learning environment, to create a
sense of space for both parties - a head and shoulder view of
participants and to provide a feeling of being 'up close and
personal'
Location,
room, background, audio, lights and power included as part of the
recipe for success
Approx.
50% of nurses indicated a need for orientation and hands on
practice with the telehealth equipment
All
nurses indicated that the education session exceeded their
expectations in terms of being interesting, informative, practical
and well organised
The
Nurse educators had difficulty adapting their teaching style to
the VC classroom More refinement required to cover high priority
topics for future workshops
Highlighted
that there is 'format' required and style' to deliver
successful content via telehealth
|
Lacked
depth in design. Could have gained more insight if conducted face
to face interviews for participants and nurse educators
Unsure
of the level of expertise of nurse educators; highlighted a need
that there is a 'format' needed to deliver successful
education via telehealth
No
details are given about the format of the videoconference
|
|
Academic
health centre management of chronic diseases through knowledge
networks: Project ECHO
|
Arora
(2007)[10]
USA
|
PCPs
including nurse practitioners, physicians, physician assistants
and pharmacists in rural community clinics in underserved areas
|
To
demonstrate how a partnership of academic medicine, public health,
corrections and community health centres can foster the capacity
of rural physician partners to provide safe and effective
treatment of HCV infection in any population, consistent with the
accepted standard of care.
|
29 PCPs
Aug 2004
- June 2005
|
Descriptive
Annual
survey (2006)
5-point
Likert scale
Intervention:
Weekly,
2-hour, short didactic sessions and case presentations
|
96%
reported enhanced knowledge about management and treatment of HCV
patients
84%
cited access to expertise in behavioural and mental health
resources as helpful when treating HCV patients
92%
believed they had obtained competence in treating HCV patients
From
July 2016 Project ECHO has been expanded to substance abuse
disorders, rheumatology, gestational diabetes, and management of
health disorders
The
methodology of Project ECHO can be generalised to many common,
complex and chronic conditions
|
|
|
A pilot
evaluation of distance education modalities for health workers in
the US - affiliated pacific islands
|
Chen
(2007)[17]
USA
|
Healthcare
workers including doctors, nurses, dentists and
others
in US affiliated pacific islands (USAPI) participating in the 2004
American Pacific Nursing Leaders Council (APNLC) and the Pacific
Basin Medical Association (PBMA) annual conferences in Pohnpei,
Federated States of Micronesia (FSM)
|
To
assess the effectiveness of various distance education modalities
for health workers in the USAPI
|
59
participants
13
hospital nurses
1 public
health nurses
2 nurse
midwives
2 nurse
practitioners
15
doctors
3 dental
(other)
3 health
assistants
3
teachers
2
dentists
4 others
(1
missing)
|
Pilot
Pre-test/post-test
questionnaires
Statistical
analysis
A
physician from University of Hawaii presented the modules from the
main library at FSM national campus
Intervention:
Training
modules in diabetes/oral health and metabolic syndrome
3
distance education modalities:
live
videoconference
live
audioconference
Recorded
computer-based slide presentation
Control
live lecture - 45 min educational presentation
All
"live" participants were able to ask questions
|
Comparison
of pre-test and post-test scores for tested knowledge gain showed
statistically significant score increases among live lecture and
videoconference groups for diabetes/oral health modules and for
all 3 modalities for the metabolic syndrome module
Computer
based training was well-accepted
Results
are used to guide ongoing development and evaluation of distance
education resources
|
Lack of
power in determining differences between modalities due to the
relatively small numbers in each group
Limited
ability to measure differences in knowledge gain between the
groups due to small numbers of test questions and participants
Limited
ability to generalise the findings to allied health workers in the
region
Anonymous
feedback was not provided so opinions may not be representative of
the group comment session in the presence of the facilitator
The
study did not attempt to address technical limitations
|
|
Education
for regional health professional using mobile videoconferencing
|
Harris
(2007)[29]
Australia
|
Clinicians,
mostly nurses in Emerald and Mount Isa
|
To
determine the feasibility of this form of distance professional
education.
To
encourage use of telehealth / VC to augment health practice
To
support remote / regional hospital staff
To
provide opportunities for case discussions and facilitate inter
professional dialogue
To
promote closer working relationships between physicians, nurses
and allied health practitioners in remote regions and colleagues
at tertiary hospitals
|
201
participants
2
hospitals
23
clinical forums
March
2007 - June 2007
|
Short
article
Quantitative
Surveys
5-point
Likert Scale
Statistical
analysis
Paediatric
consultants, clinical nurse consultants and allied health
professionals with expertise in paediatrics presented the forums
from Royal Children's Hospital, Brisbane
Intervention:
Weekly,
telePaediatric clinical forums involving formal and informal
presentations, clinical case discussions, demonstrations and
questions and answers.
|
166
participants completed surveys
88%
participants agreed or strongly agreed that the sessions were
relevant, of adequate depth (86%) and provided new content (100%)
Participants
consistently indicated that they had opportunity for questions and
discussions
Participants
also appreciated the opportunity to access specialists located in
the tertiary hospital
These
sessions were delivered in the ward which was viewed as an
advantage for engagement of staff
97%
agreed or strongly agreed that the sessions should be continued
routinely
|
Limited
to two hospitals
|
|
Hepatitis
C videoconferencing: The impact on continuing medical education
for rural healthcare providers
|
Rossaro
(2007)[48]
USA
|
PCPs
including doctors, nurse practitioners, physician assistants and
registered nurses in rural clinics in Northern Carolina
|
To
compare the impact of VC(VC) versus standard lecture (ST) on
education regarding natural history, diagnosis and management of
HCV
|
175
participants
68
physicians
27 nurse
practitioners/physician assistants
80
registered nurses
62 VC
113 ST
14 sites
|
Prospective
study
Quantitative
Pre-
post- test
Surveys
Statistical
analysis
A
gastroenterologist and educator at University of California
delivered the VC and ST lectures
Intervention:
VC
and ST lecture
|
All
types of learners improved their knowledge scores following
intervention via VC
Registered
nurses showed the greatest improvements
Results
demonstrate that VC is equivalent, if not better than standard
continuing medical education
VC can
potentially improve clinical education regarding the history,
diagnosis and management of HCV VC has the potential to eliminate
the financial and geographic barriers to professional education
for rural practitioners
To
ensure consistency the standard lectures and VC content were
delivered by the same person
|
A robust
quantitative method employed which demonstrated improved learning
However,
more depth would have been gained if face to face interviews were
conducted to evaluate the perception and true impact of VC and how
the knowledge gained is transferred into clinical practice
|
|
Using
the project extension for community healthcare outcomes model to
train rural primary care clinicians to deliver child mental health
services in Oregon
|
Cheng
(2017)[58]
USA
|
PCPs in
rural areas of Oregon
|
To
demonstrate that the Project ECHO model is an effective means for
providing child psychiatry education to rural primary care
providers
|
31
participants
Aug 2016
- Mar 2017
|
Conference
abstract
Pre-test/post-test
Surveys
No
description of intervention - ECHO consultation and education
model
|
23/31
completed the pre-program survey
19/31
completed the post-program survey
27/31
participants (87%) completed the program
Post
training 26% provided mental health psychoeducation in their daily
practice compared to 9% prior to ECHO
Post
training 76% of participants felt comfortable treating patients
with mental health disorders compared to 43% prior to ECHO
Improved
confidence in using psychotropic medications increased from 47% to
89%
|
|
|
Project
ECHO: Bringing palliative care consultation to rural New Mexico
through a novel telemedicine format
|
Marr
(2012)[60]
USA
|
Multidisciplinary
PCPs in rural areas of New Mexico
|
To
determine the feasibility of a telemedicine curriculum, Palliative
care ECHO clinic, to educate rural PCPs about palliative care
|
Number
of participants is not provided
Number
of sites is not provided
Initiation
in April 2011
|
Conference
Abstract
An
interdisciplinary team delivers the ECHO program
Intervention:
Weekly, 2-hour short didactic, case presentations, and case
discussion and recommendations by an interdisciplinary team at UNM
|
Feasibility
was demonstrated
Provider
satisfaction was high
Self-efficacy
improved
Sense of
isolation decreased
Further
expansion to other regions of the country
|
Not
enough detail in this abstract to gauge strengths or limitations
|
|
Project
ECHO: improving asthma care in New Mexico with telehealth
technology
|
Harkins
(2011)[59]
USA
|
PCPs in
FQHCs in rural and underserved areas of the state, prisons,
schools and NM Dept of Health
|
To
engage providers and allied health personnel as partners to follow
the national guidelines for asthma treatment and education
|
200
participants
50 sites
|
Conference
abstract
Pilot
Specialists
at UNM deliver the clinics
Intervention:
Bi-weekly clinics, didactic sessions and case presentations and
hands on training at Adult and Paediatric Asthma Clinics at UNM
|
Increased
number of nationally certified asthma educators from 22 to 40
|
Not
enough detail in this abstract to gauge strengths or limitations
|
|
Dermatology
ECHO - an innovative solution to address limited access to
dermatology expertise
|
Lewis
(2018)[62]
USA
|
PCPs in
rural Missouri
|
To
identify practical applications and utilization of telemedicine
VCtechnology for treatment and management of various skin
conditions
|
1
participant
Patient
case study from rural Missouri
|
Observational
Clinical
case report
The
Dermatology ECHO hub team at the University of Missouri consisted
of general dermatologists, Paediatric dermatologists, a
dermatopathologist, a clinical psychiatrist and an advanced
practice nurse
Intervention:
Weekly, 1 hr long sessions including brief didactics and 3-5
de-identified case discussions
|
Dramatic
improvement in specific patient's condition to PCP participation
to guide diagnosis and treatment of bacterial skin infection
Further
investigation will assess pre- and post- Dermatology ECHO
treatment outcomes as well as participation referral rates to
dermatology speciality clinics
|
1
patient case study
|
|
Making
connections: using telehealth to improve the diagnosis and
treatment of complex regional pain syndrome, an underrecognized
neuroinflammatory disorder
|
Katzman
(2013)[61]
USA
|
PCPs
from varying clinical backgrounds in rural areas of 10 states
|
To
partner the UNM Project ECHO Chronic Pain telehealth clinic with
the Reflex Sympathetic Dystrophy Association (RSDSA) and UNM
Clinical Pain Center to develop a month-long curriculum dedicated
to chronic regional pain syndrome (CRPS) to increase the knowledge
and self-efficacy of primary care clinicians in treating CRPS
|
62
unique attendees
153
participants
August
2012
|
Case
study
Descriptive
Surveys
Clinician
specialists from the UNM interdisciplinary Pain Center deliver
ECHO Pain
Intervention:
CRPS themed month of weekly sessions of didactics and
de-identified patient cases
|
95% of
the items rated by participants in each weekly session were 4.0 or
higher on a 5-point rating scale implying strong agreement that
the sessions were effective, relevant to their practice and that
they were likely to apply information in the future with their
patients
|
|
|
Clinical
services and professional support: A review of mobile
telepaediatric services in Queensland
|
Smith
(2010)[63]
Australia
|
Clinicians
in rural and regional hospitals in Gladstone, Mt Isa, Emerald,
Gympie, Nambour, Hervey Bay and Townsville
Providers
across the multidisciplinary team were able to access services for
general paediatric support, sub-specialist support and education
and training
|
To
describe clinician experiences using mobile (robot) VC systems for
the delivery of paediatric support in the clinical setting
|
7 sites
966
consultations
465
sessions
228
hours of VC
Jan 2005
- July 2010
44
remote education sessions
3 sites
- Mt Isa, Emerald and Gympie
Average
7 participants
Mar 2007
- Jun 2008
|
Descriptive
Retrospective
review and case studies
3 case
studies - consultation only
Specialists
at Royal Children's Hospital (RCH), Brisbane delivered the
education sessions
Intervention:
35-40 min robot education sessions involving informal case
conferences providing support in paediatrics
|
The
telehealth mobile systems served three key functions, provision of
general paediatric support, sub specialist paediatric support, and
professional education
Some
outcomes supported by case studies showed increased communication
and inter facility teamwork
Decreased
travel times and increased efficiency for senior clinicians
Potential
decreased incidences in transferal of patients to tertiary centres
The
mobile telehealth units provided a convenient mechanism to deliver
staff education and to promote networking opportunities
The
system had a single point of contact allowing for easier access
and greater uptake of the resource
This
also allowed for deceased training time to become familiar with
the resource
|
Technical
difficulties with VC delivery of education are typically minor
No
indication of user satisfaction of the resource and what feedback
the end user was required to provide
|
|
The
impact of Project ECHO on participant and patient outcomes: a
systematic review
|
Zhou
(2016)[65]
Canada
|
PCPs
from remote areas
|
A review
of the evidence of the impact of all Project ECHO programs on
participant and patient outcomes
|
39
Project ECHO studies addressing 17 medical conditions
Jan 2000
- Aug 2015
|
Systematic
review
Quality
assessment of outcomes based on Moore's evaluation framework
Level of evidence: Level 1: participation, Level 2: satisfaction,
Level 3: learning, Level 4: competence, Level 5: performance,
Level 6: patient health, Level 7: community health
Specialists
at academic health centres deliver Project ECHO
Intervention:
All Project ECHO programs
|
30
studies addressing populations in remote areas
2
studies met criteria for high fidelity
28
studies reported at least 1 outcome from Moore's evaluation
framework
13
studies used surveys and/or semi-structured interviews
4
studies assessed PCPs knowledge with pre-/post-test comparison and
thy reported a high level of satisfaction with the intervention
7
studies reported an increase in PCP competence
It is
unclear whether self-reported confidence is a good measure of
clinical competence
1 study
tested participants' performance however there was no control
group
6
studies suggested changed patient outcomes
2
studies suggested it was cost effective
Further
research examining efficacy is needed and identifying and
addressing potential barriers
|
Inclusive
approach for studies regardless of quality
Studies
comparing outcomes with subspecialist care alone have been limited
to Hepatitis C Virus and few have looked beyond level 5 outcomes
Little
verification has been done for studies stating they implement
"evidence-based" treatment methods
No
studies included used of a randomised controlled trial methodology
Database
search limited to: PubMed, MEDLINE, EMBASE, PsycINFO and ProQuest
|
|
The
reported benefits of telehealth for rural Australians
|
Moffatt
(2010)[64]
Australia
|
Primary
studies of health professionals in rural areas
|
Literature
review to identify the reported benefits attributed to telehealth
for people living and professionals working in rural and remote
areas of Australia
|
147
studies
1998 -
2008
|
Narrative
review
|
Health
professionals have benefited from: access to continuing education
and professional development, provision of enhanced local service,
experiential learning and networking and collaboration
The use
of telehealth appears to be a path to up-skilling for rural and
remote practitioners
Review
of Qld government telehealth VC network showed over 2 years 60%
was for education and professional support services, in WA this
was 40%, and for mental health nationally (except Vic) 83% of
telemedicine programs provided education programs via telehealth
Benefits
include increased access with reduced travel, increased access to
variety of education
|
Limited
information about systematic review process and analysis
Database
search limited to Scopus, websites and government documents
|
|
The use
of synchronous videoconferencing teaching to increase access to
specialist nurse education in rural KwaZulu-Natal, South Africa
|
Chipps
(2010)[4]
South
Africa
|
Registered
nurses in rural South Africa
|
Review
the literature and evaluate the current use of VC education for
nurses in KwaZulu-Natal
|
81
papers in literature review
2 nurse
VC education programs
Clinical
Antiretroviral therapy (ARV) - 186 participants at 3 sites
Advanced
Midwifery (ADM) - 53 participants at 5 sites
|
Literature
review
Program
evaluation of 2 nurse education programs delivered via VC
Questionnaires
Audit
log
Enhancing
Care Initiative (ECI) staff at the Medical School at UKZN deliver
the first education program and School of Nursing staff deliver
the second education program
Intervention
1: 2-day ARV - Two, 8-hour sessions
Intervention
2: One, 3-hour session/week over 6 months
|
80% of
ARV participants were from remote non-Durban sites
Participants
reported that VC training is comparable to face-to-face training,
once technology is established and staff are comfortable there is
no downside to VC training and potential cost savings are
significant but mostly increased access was the greatest positive
Comfort
of presenter was commented on and their ability to engage
participants within the training affected the training outcomes
Therefore,
orientation to teaching using this method is essential and
increasing interaction with remote sites during training and using
PowerPoint slides to support that Clear protocols for technical
support are needed
Not
enough research for outcomes of VC being equal to face-to-face
teaching
|
Reporting
only on what was found in the literature, not of how articles were
included or excluded or quality etc
Not a
lot of information about rigour or ability to replicate
|
|
Telehealth
and the recruitment and retention of physicians in rural and
remote regions: a Delphi study
|
Duplantie
(2007)[66]
Canada
|
Telehealth
experts including managers, users and researchers/evaluators
|
To
identify a reliable list of recruitment and retention factors on
which telehealth could impact
|
2
literature reviews
Delphi
study - 12 participants
|
Questionnaires
Delphi
study - compared the degree of written agreement among experts,
who were not in contact at any time
A
minimum of 2 questionnaires were used to get consensus from the
experts
|
Good
review of the literature identifying 7 factors (including
educational) of telehealth that could be related to medical
workforce recruitment and retention
The
experts agreed that telehealth could favour recruitment and
retention by facilitating contact with peers, enforced with a
system that is easy to use with human faces and connectivity for
all
Identified
traits and characteristics of remote physicians that were deems
important
The
highest consensus was: liking challenges, the capacity to work in
collaboration, being helpful for the community and having a
facility of adaptation
The
consensus reached by the experts through the Delphi study shows
the potential that telehealth could have on a set of individual,
professional, organisational and educational factors related to
recruitment and retention of physicians in rural and remote areas
|
Brief
summary only of literature review findings
Decreased
response to the second round of questionnaires sent out to experts
which could challenge the robustness of the method used
|
|
Telementoring
for improving primary care provider knowledge and competence in
managing chronic pain: A randomised controlled trial
|
Eaton
(2018)[67]
USA
|
PCPs
including physicians, physician assistants, nurse practitioners
and registered nurses in University of Washington (UW) Medicine
Telehealth network communities in rural and underserved areas of
Washington, Wyoming, Montana, Oregon and New Mexico
|
To
evaluate the effect of a telementoring intervention, TelePain, on
knowledge and perceived competence related to chronic pain
management
|
41 PCPs
23
intervention group
18
control group
22
physicians
13
physician assistants
3 nurse
practitioners
3
registered nurses
12-week
study
|
Cluster
randomised clinical trial (RCT)
Questionnaires
Knowledge
and Attitudes (regarding pain)
Know-Pain-12
Perceived
competency scale
Statistical
analysis
Specialists
with expertise including pain medicine, internal medicine,
anaesthesiology, rehabilitation medicine, psychiatry, addiction
medicine, nursing and complementary and integrative pain
management provided the telementoring consultations
Intervention:
90-min TelePain: Weekly, 30-min didactic presentation and 60-min
patient case consultations, discussion and symptom management
recommendations
|
First
study to use RCT to evaluate pain management telementoring
78% of
the intervention group presented at least one case
89%
attended at least one TelePain session
4
control group PCPs attended an average of 6 sessions (see
limitations)
Knowledge
and perceived competence did not increase for the intervention
group compared with providers in the control group
Future
research is recommended to test the effectiveness of the
intervention
|
Not able
to prevent control group from attending TelePain sessions,
therefore findings may not be a true reflection of intervention's
effect
Considerable
variability in the number of TelePain sessions attended by
intervention group
|
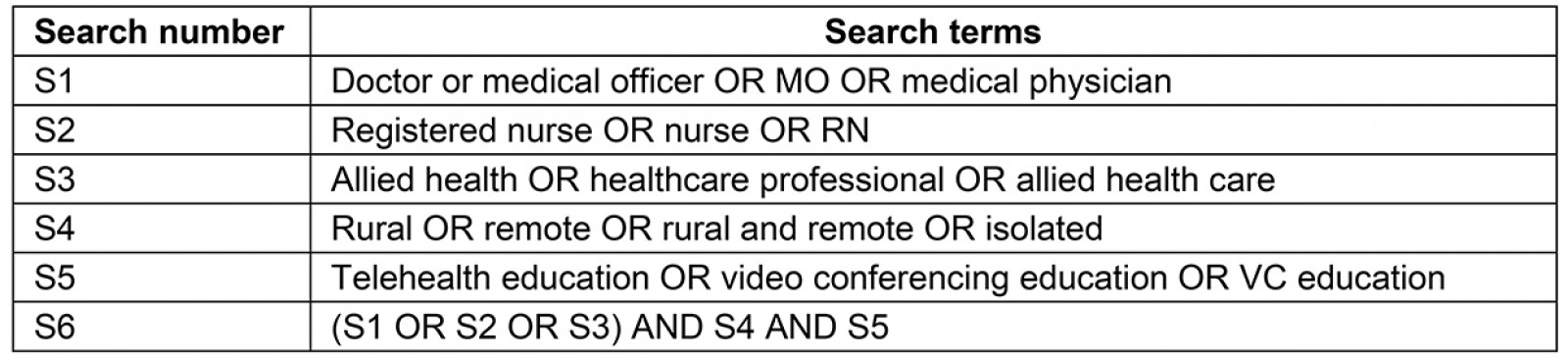
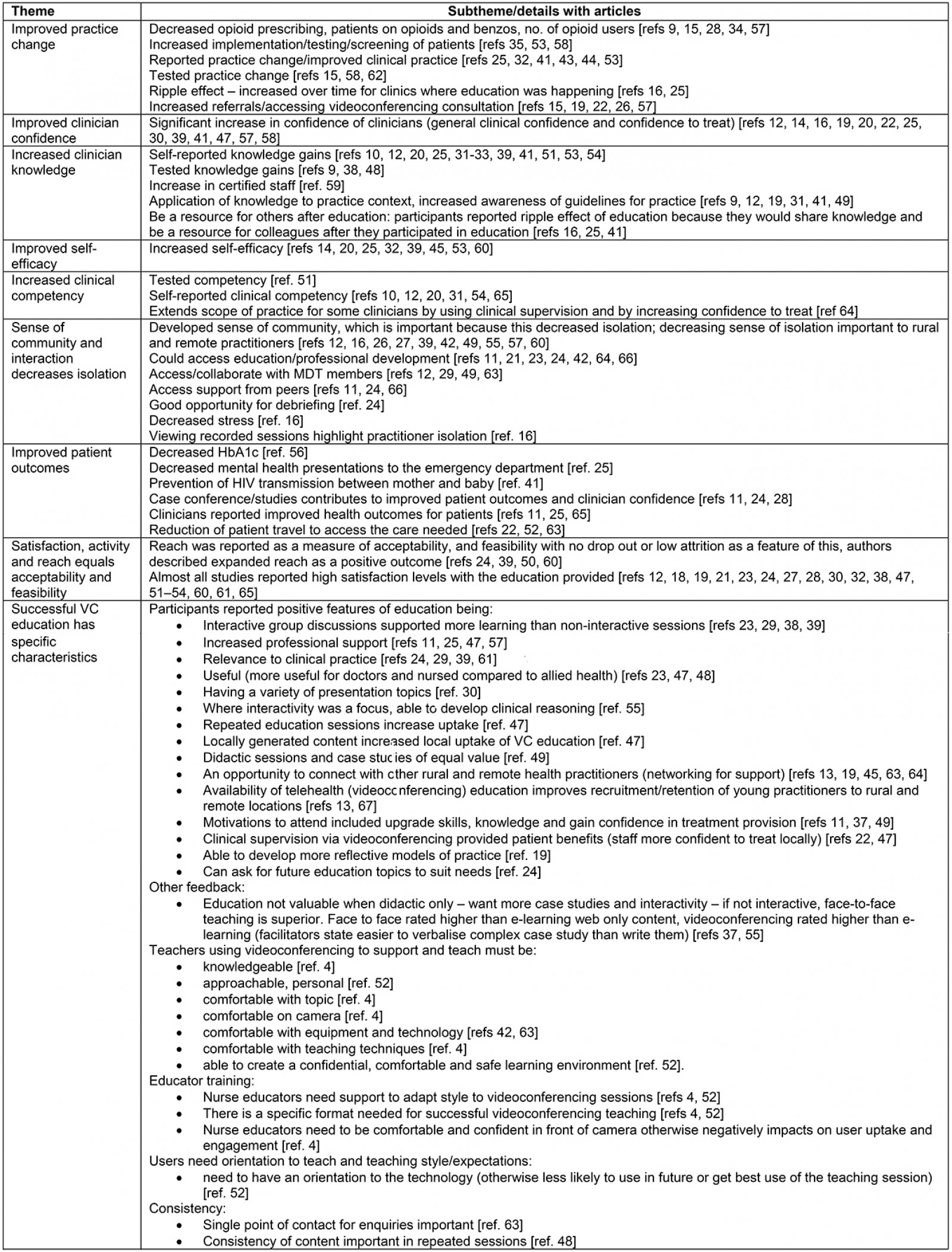
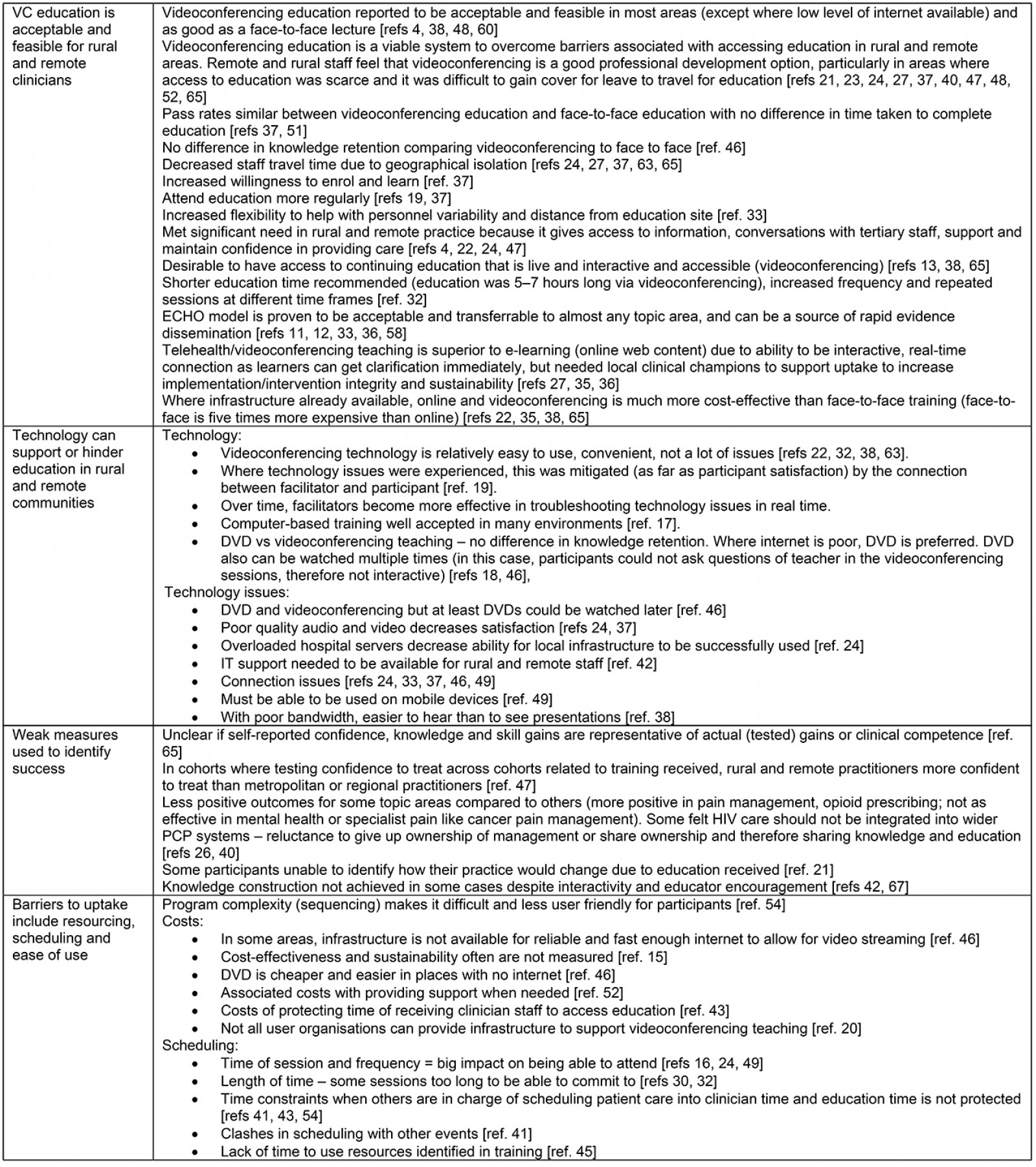
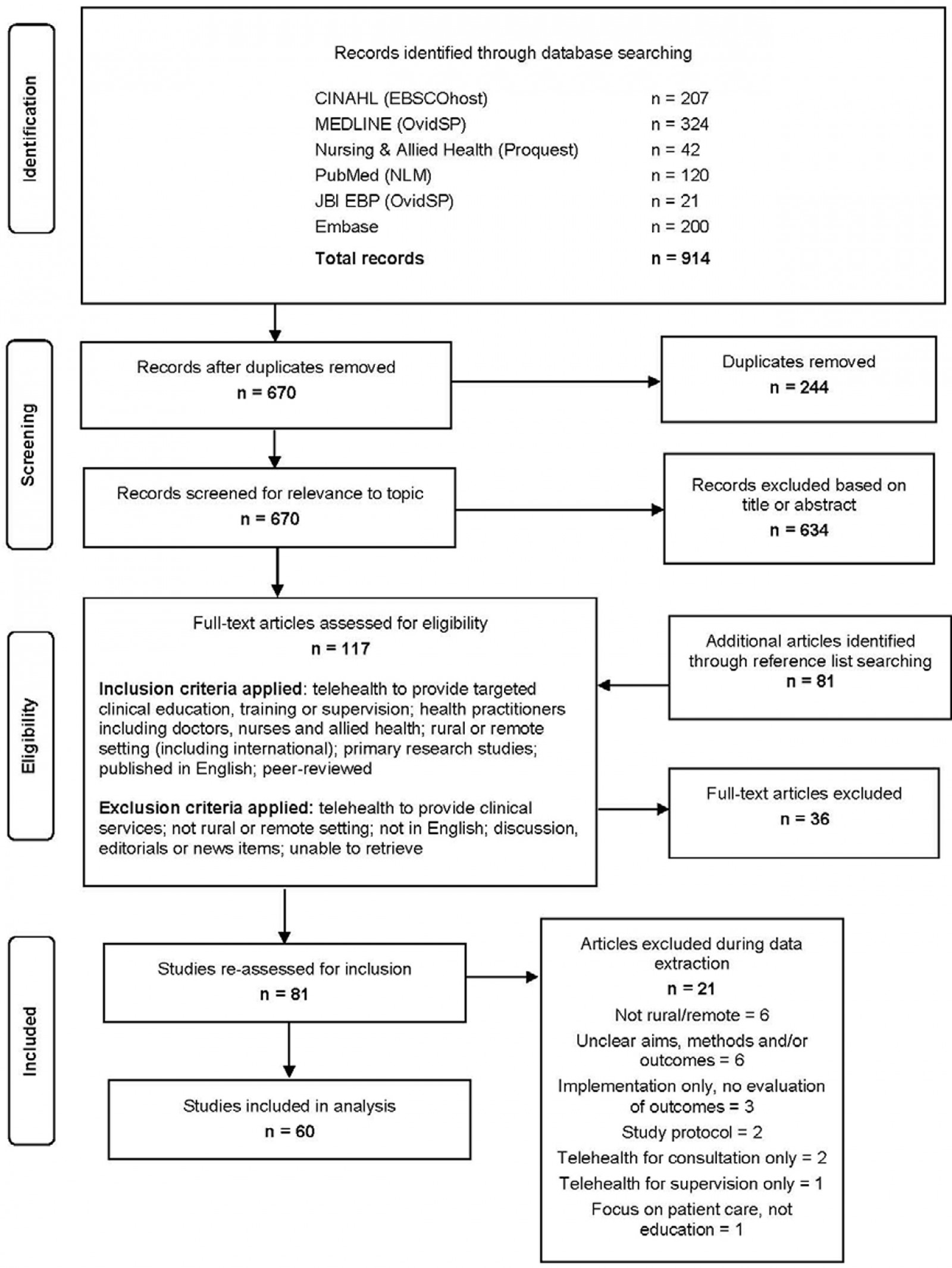 Figure 1: Modified PRISMA flow diagram of included studies.
Figure 1: Modified PRISMA flow diagram of included studies.

