Introduction
The provision of health care in remote rural territories is a challenge for the most diverse social protection systems1 as it involves a set of unfavorable conditions of access to primary health care (PHC), specialized and hospital care, difficulties in attracting and retaining the workforce, and for the improvement and professional education and management of health services2,3. These conditions are associated with worse socioeconomic and human development indicators2,4, insufficient transport, long distances to be covered, long time away from home for clinical investigations and treatment, unsafe sanitary and housing conditions, and increased disease burden5. These challenges require organizational models and the provision of health services to respond to a rurality’s characteristics.
Like other countries, Brazil faces obstacles to ensure access to health by remote rural municipalities. Brazilian rural areas are characterized by diversity, which excludes any reductionist vision of rurality. The populations that inhabit rural spaces – fields, forests, and waters – are distinct in relation to race, ethnicity, and ways of life6. Such singularities demand adaptive approaches and the willingness of policymakers, professionals, and users to understand these territories’ particularities and their health needs, which differ from urban centers, especially in the Amazon region6.
In Brazil, the Family Health Strategy is the primary PHC model in the Unified Health System (Sistema Único de Saúde – SUS). It is staffed by a multiprofessional team composed of a doctor, a nurse, a dentist, nursing technicians, and community health workers in registered areas, responsible for monitoring a defined number of households7. While many results have been achieved through the Family Health Strategy7-9, rural areas still have poor access to health care, high infant mortality, prevalence of tuberculosis, verminosis, diarrhea, respiratory infections10, and economic and transport barriers to access PHC units11.
The diverse barriers sometimes condition users to seek alternative answers to their health problems, outside the formal care circuit, including medicinal herbs, foods with curative power, and care offered by family, friends, and non-professional healing specialists12,13. Furthermore, based on the framework of medical anthropology, Kleinman14 indicates that the sociohistorical-cultural context also determines the search for health care, and not only by the conditions of access and availability of formal services. Studies show that the use of multiple therapeutic modalities or ‘medical pluralism’ is usual in contexts where medical and alternative care are available15.
From this perspective, the service organization models, the choices and the evaluation of therapeutic practices and socially accepted behaviors, including power relationships and social roles of the different workers, are a cultural health system14,16 in societies. Each health system would comprise three interrelated subsystems: the informal, popular, and professional subsystems. Subsystems are widely used in an overlapping and non-exclusive way, interacting per an individual’s needs14,16.
Popular culture, common sense, family, social network, beliefs, and community activities are manifested in the informal subsystem, establishing a link between the professional and popular subsystems16. The popular subsystem is based on informal healing specialists, secular or religious workers, not legally certified, but with significant recognition by society. Those practicing in this system are often called lay people, and their therapies use herbs, teas, medicinal foods, and alternative practices, including spiritual healing rituals15,16.
Significant barriers linked to the availability and use of services are recognized in the professional subsystem, and this article analyzes how the informal and popular health subsystems are featured, under Kleinman’s perspective14, in a remote rural municipality of the Brazilian Amazon region. The author argues that health, illness, and care are part of a cultural system and must be understood in their mutual relationships. Examining them in isolation distorts the understanding of each other’s nature and how they work in a given context. In this sense, while the formal system’s expressive nature is recognized, both concerning the focus of publications and research and policies, the author aimed to emphasize other dimensions that underpin the popular culture of rural communities and are in the daily life search for health care. It is hoped that this study can contribute to the understanding of the dynamics that determine and motivate the use of health services in remote rural municipalities, in the light of broader references that can inform health policies, actions, and practices that are more appropriate to the needs of rural contexts, so far partially addressed by national health policies in Brazil4,6.
Methods
This is a single, exploratory, qualitative case study carried out at the remote rural municipality of Assis Brasil, in the state of Acre, Brazil. The main aim was to understand how the informal and popular systems are featured and related in the experiences of care and the organization of health services, especially those of PHC. The concept that guides this work is based on the assumption that geographical, environmental, political, economic, historical, cultural, and social characteristics, in a conjugated manner, directly affect the lives of the people who live in these locations and determine health conditions17.
Data collection
Data were collected in May 2019 with an onsite visit to the municipality of Assis Brasil, through semi-structured interviews. The roadmaps were adapted to each type of key informant, and allowed capturing the care customs, beliefs, and habits, and identifying the population’s health services.
Research participants
Sixteen interviews were carried out with three informant groups: municipal, regional, and state health managers, Family Health Strategy professionals, and users. Managers are responsible for the provision and organization of PHC in the SUS, which, according to the Brazilian federative system, establishes the public and universal provision of health services under the responsibility of the three governments: federal, state and municipal7. A second group was composed of physicians, nurses, and community health workers who, in accordance with the Family Health Strategy, are the main agents of care. It is noteworthy that community health workers are community residents and, in this sense, also represent the diverse health perspectives present in the territory. Users composed the third group of informants privileged to characterize the health subsystems present and used in Assis Brasil.
Table 1 shows the profile of the participants and their identification, later used to identify the statements. The local PHC coordinator indicated two PHC units to carry out the interviews with professionals and users. One was located at the municipality’s headquarters, and another in a rural, inland area. Three tracer events were chosen18, appointed by the respective Family Health Teams: cervical cancer; prenatal, childbirth and puerperium care; and systemic arterial hypertension. The interviews lasted for 1–2.5 hours, and were fully recorded and transcribed.
Table 1: Characterization of research participants, Assis Brasil, Acre, Brazil, 2019 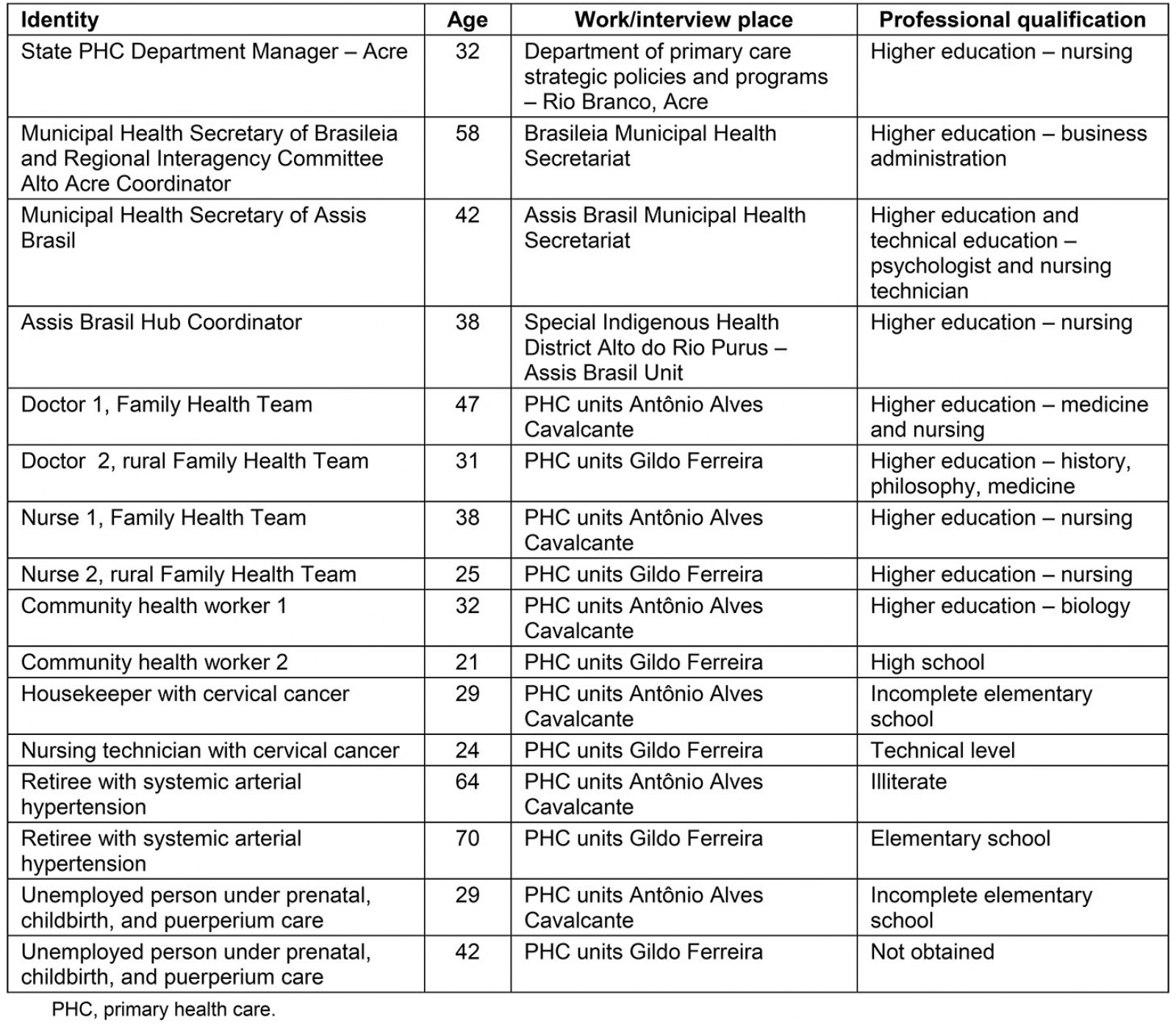
Data analysis
The thematic analysis19 was guided by categories inspired by Kleinman’s framework14,16 and emerging in the field, and focused on dimensions of the informal and popular subsystems: informal – role of the family, community, network of friends, crossing of politicians, presence of non-governmental organizations, armed forces and religious entities; and popular – specialized secular or religious agents (shamans and healers), performance of midwives, multiculturalism, and use of medicinal herbs. The aim was to understand how these elements come together, whether there is a counterpoint vis-à-vis the formal system, or they are triggered independently, timely, or non-continuously in the face of the several challenges in the search for health care in rurality.
Research scenario
In Brazil, the definitions of rural and urban space gained a new typology in 201720 in line with international methodologies from the OECD and the European Union. Demographic density, distance from the main urban centers, and population size are among the criteria for classifying municipalities into five types: urban, adjacent intermediate, remote intermediate, adjacent rural, and remote rural. According to the new classification, 76% of the Brazilian population lives in predominantly urban areas (26% of the municipalities). A total of 60.4% of the total number of municipalities (5570) were classified as predominantly rural, with 54.6% adjacent rural and 5.8% remote rural20.
The Assis Brasil remote rural municipality is located on the boundaries of the Brazilian territory and borders two other countries, Peru and Bolivia, with a large movement of people. Traditional populations such as the riverside and a large concentration of indigenous peoples of the Jaminawá and Manchineri ethnic groups live in the Mamoadate Indigenous Land21. The territory is divided into an urban area or headquarters, where trade and services are located – and where most of the population is concentrated – and the rural or inland areas, with small villages22.
The network of health services in the municipality comprises three PHC units, all located at the headquarters, an Indigenous Health Base Hub of the Indigenous Health subsystem, two health gyms (equipment for physical activities and health promotion), a clinical analysis laboratory, and a mixed unit (belonging to the state government) with general, obstetric, and pediatric beds, with low resolution of actions and intermittent presence of a doctor23.
Ethics approval
This research was approved by the Human Research Ethics Committee of the Sérgio Arouca National School of Public Health, the Oswaldo Cruz Foundation, under CAAE 92280918.3.0000.5240 and approval opinion No. 2.832.559.
Results
Informal subsystem
Family, community, friends, politicians, armed forces, NGOs, churches – care crossings: Family, community, and friends have played an important role in facilitating the search for health care for users in Assis Brasil headquarters and rural areas. Friends and acquaintances lent credit cards to purchase medications that were not available in the public network, and children organized their parents’ appointments and tests. Rural dwellers who had to seek care at the PHC units of the headquarters stayed with relatives and friends, who accompanied them to visits and took care of the children:
A large number of people stay at a relative’s home. Then do the treatment. In my micro area, we had a woman ... She stayed here at her relative’s home. She was undergoing leishmaniasis treatment ... Then, the doctor prescribed her 30 vials. In this case, she stayed here for 30 days. After the treatment, she returned to the rural area. (community health worker 1)
When a health condition or traffic on the roads and rivers hindered travel from the rural area to the PHC unit headquarters, users were carried in hammocks for up to 2 days by relatives, friends, and community people, which was a common and recurring practice among rural residents:
When it rains, we cannot reach the branches [small secondary roads] due to the amount of mud. Patients sometimes arrive on hammocks, as we have to have traction trucks in order to arrive. And we often cannot. The situation is unfortunate. (municipal manager)
It is complicated where I lived. It is 44 km from here [headquarters] to there [rural area]. It is tough in winter; it is loads of mud ... If people get sick, they have to be brought in on hammocks from there to here, and it takes a lot of time .... My wife came around three times from there [rural area] to here [headquarters] carried on hammocks. It took two days of travel (on foot). (systemic arterial hypertension patient 1)
The reference for specialized and hospital services was the state capital, Rio Branco, 343 km from Assis Brasil, with no municipal support house for patients and their companions. In these cases, once again, assistance from family and friends was required for hosting, or, when not possible, users returned to Assis Brasil on the same day and, on the following day, again traveled back to the capital:
My trip to Rio Branco was by municipal van. They sent me with seven months of gestation to Rio Branco because of my health. It was very risky to be here because I have no resources, and high blood pressure ... I stayed at a husband’s cousin’s house. I stayed there .... (prenatal, childbirth and puerperium care patient 2)
When patients arrive in Rio Branco and have to make an appointment today and another tomorrow ..., some have relatives and stay in Rio Branco. The others go back and forth [from/to Assis Brasil] on the same day, and the next day they go back again [to the capital]. (regional manager)
Users without physical and financial conditions to travel or stay at the municipal headquarters and in cases of emergency, especially in the rural area, directly accessed the municipal health secretary and mayor:
Hence today the secretary was going to pay a visit there to deliver the medication. When we left this visit, we spoke directly with the Mayor, asking for support to provide a house because a lady from the rural area would not be able to continue the treatment .... (nurse 2)
Family Health Teams’ actions were sometimes captained politically, despite opposition by professionals. Local politicians took advantage of their status to request priority care to acquaintances and relatives, which restricted access for other users. Services provided by NGOs and armed forces were present on a residual basis and filled gaps of the public system. The work of an NGO hired by the Health Secretariat to outsource health professionals with temporary contracts was pointed out. In general, the armed forces and NGOs carried out itinerant health actions in the rural area and provided medication, which complemented the services provided by the SUS:
We even have it regarding itinerant health. The secretary signed another partnership with the army and firefighters to strengthen care because they have other transport types. So, it allows providing care in these areas ... NGOs are also very present, and this connection is very positive. (state manager)
The churches gave up their headquarters to carry out itinerant health actions in the rural area and for the production and sale of medicinal products consumed and manufactured by the population:
... the syrups and these medicines they make in the Catholic church have a selling place there. There is a little place that sells syrup ... People go there. (nurse 1)
The popular subsystem
A multicultural territory: Assis Brasil is a multicultural territory. It borders two countries and has a large flow of indigenous, riverside, Bolivian, Peruvian, and Venezuelan people, both from Brazil to these countries and vice-versa. The diversity of ethnicities and cultures has given the territory various languages, customs, and health practices.
Brazilian health professionals struggled to speak with indigenous users, which required the presence of Portuguese-speaking relatives or technicians from the National Indigenous Foundation for the translation and mediation of visits:
And the language of indigenous people too. Some indigenous people don’t speak Portuguese and always come with a translator. If relatives don’t speak the language, they come in with a translator. (doctor 2)
Specialized secular or religious agents – shamans, healers, midwives: Health professionals and managers indicated specialized healing workers such as shamans, healers, and prayers in the healthcare process. Like shamans, members of indigenous ethnicities in the region, some popularized their practices among the entire population of the municipality, integrating themselves with it. Others, such as prayers and healers, had their practices legitimized and culturally accepted.
Traditional healing practices were not opposed to those of the formal health system and were accessed differently by the population: occasionally, in search of a specific cure and momentary relief; throughout life, concomitantly with treatment in the formal health network; or as an alternative. Sometimes, the population showed a preference for these practices, making them their first choice of care, and, according to professionals, arriving at the health service after their condition had deteriorated:
We have prayers and mainly indigenous people. Furthermore, we have prayers that sometimes people say, ‘doctor, I took my son who was vomiting for two days to the prayer, but it seems that it didn’t work’ until they came in with their dehydrated boy. (doctor 2)
Medicinal herbs were part of the health care of the popular subsystem with the use of teas, syrups, bottled preparations with medicinal plants in rural and urban areas:
They use many teas. There is resistance, especially from diabetics. They want to drink tea and not take medicines. (nurse 2)
At other times, medicines based on medicinal plants were the only resource adopted by users in times of illness and given the impossibility of accessing the health service due to geographical or economic barriers. Such practices were especially more frequent in rural areas due to distance from the PHC units and intermittent itinerant actions, which left part of the population unattended:
... rural area so they can come [to the PHC units], they have to pay for a motorcycle taxi or a private car freight. It is expensive for people in the rural areas ... Many of them there [rural areas] opted for medical treatment with their knowledge. They only come here as a last resort. Furthermore, many choose it due to the lack of financial resources. (community health worker 1)
Secular healing practices were more prevalent among the indigenous population who used herbs, prayers, and shamans concomitantly, even with access to health services from the Special Indigenous Sanitary District:
The two ethnic groups here, Jaminawá and Manchineri ... Some have that prayer and even come here for care and say they will also visit the shaman. Some others just want the shaman. We record the refusals so that we are not held accountable in the event of any occurrence. We have a patient with a heart problem we are monitoring here. He informed us that he was going there for a prayer in an indigenous Peruvian community and that he would return. I said, ‘okay, but your return is scheduled for that day’. (indigenous health manager)
The role of midwives in the region was recognized, especially in rural and indigenous areas, where folk healing traditions and traditional care are strongest. Most births between indigenous and rural women were carried out by midwives at the users’ preference, as was monitoring in the first days of the baby’s life. For this reason, formal health services were offered in conjunction with midwives in some indigenous communities, and the Family Health Team promoted training courses and set up a group to exchange experiences to foster greater integration.
Conflicting positions were identified, especially when health professionals identified the replacement or postponement of formal treatment using medicinal herbs and other informal practices. Even so, teas and other natural resources, such as ‘clay’, were incorporated and shared into community life, and were part of the local tradition and flora since the municipality belonged to the Amazon region:
This child with leishmaniasis that I talked about. Her grandmother was treating leishmaniasis with pure clay and putting the clay inside the wound. I said: ‘no, but the issue is in the blood; we will kill the blood’s parasite. Then it will close normally’. Furthermore, many choose this treatment because of a lack of financial resources. (community health worker 1)
When I was in Rio Branco with my sick wife, I saw a man there at the hospital saying that the doctor disillusioned him. He had a prostate problem that had no cure. Then he said: ‘Do you have faith in forest tea?’, I said: ‘I do’; and he said: ‘I’ll teach you a medicine that if you take it properly, you will be just fine’. So, he taught me. He took it, and his condition improved. Today, he is well. Then I went, and thank God it was useful. When I went to Rio Branco, they told me he was healed and did not even have to see the doctor. (systemic arterial hypertension patient 1)
Figures 1, 2 and 3 summarize the care trajectories of users between the healthcare subsystems in a remote rural municipality.
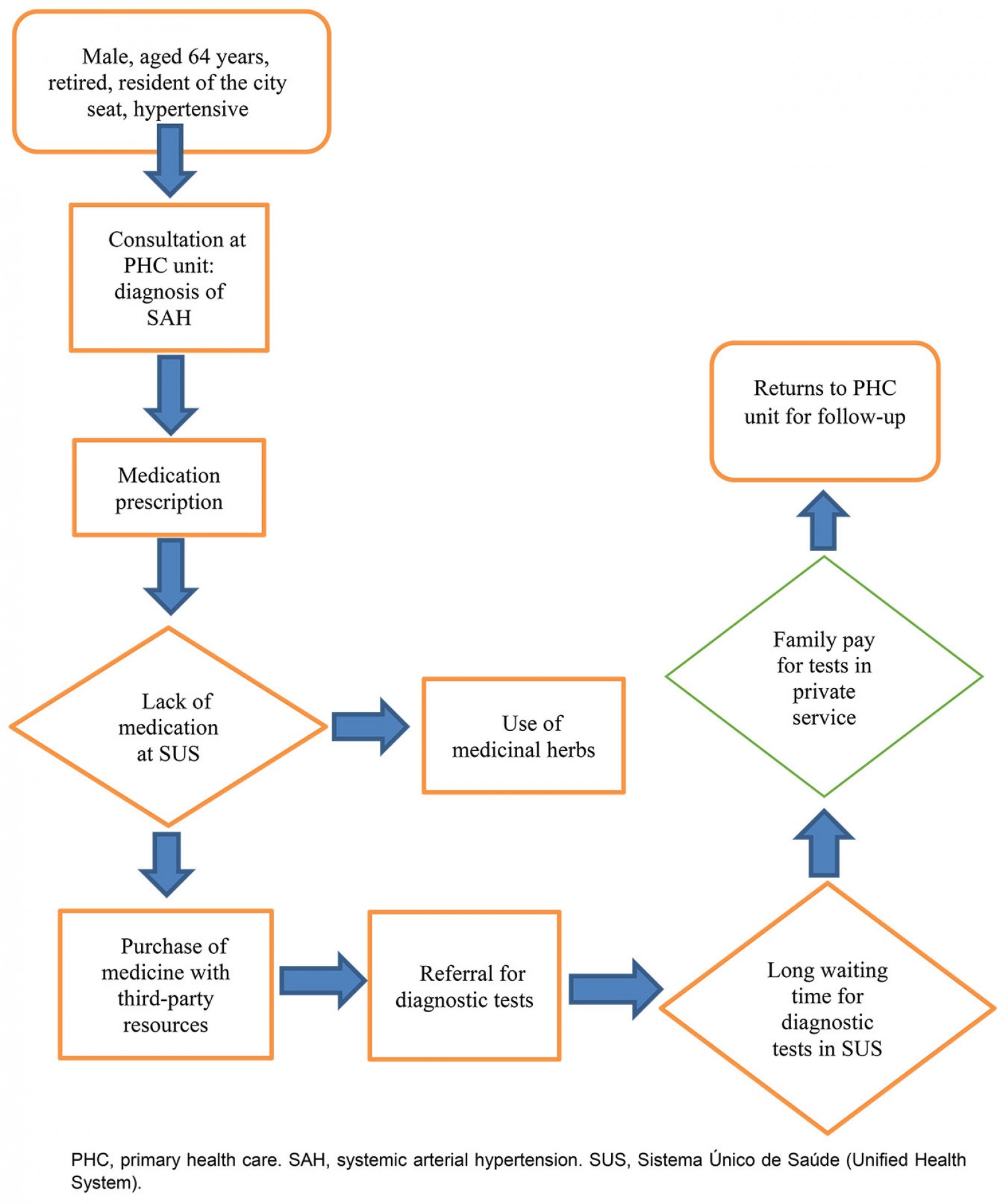 Figure 1: Care trajectory of a user with systemic arterial hypertension, Assis Brasil, Acre, Brazil, 2019.
Figure 1: Care trajectory of a user with systemic arterial hypertension, Assis Brasil, Acre, Brazil, 2019.
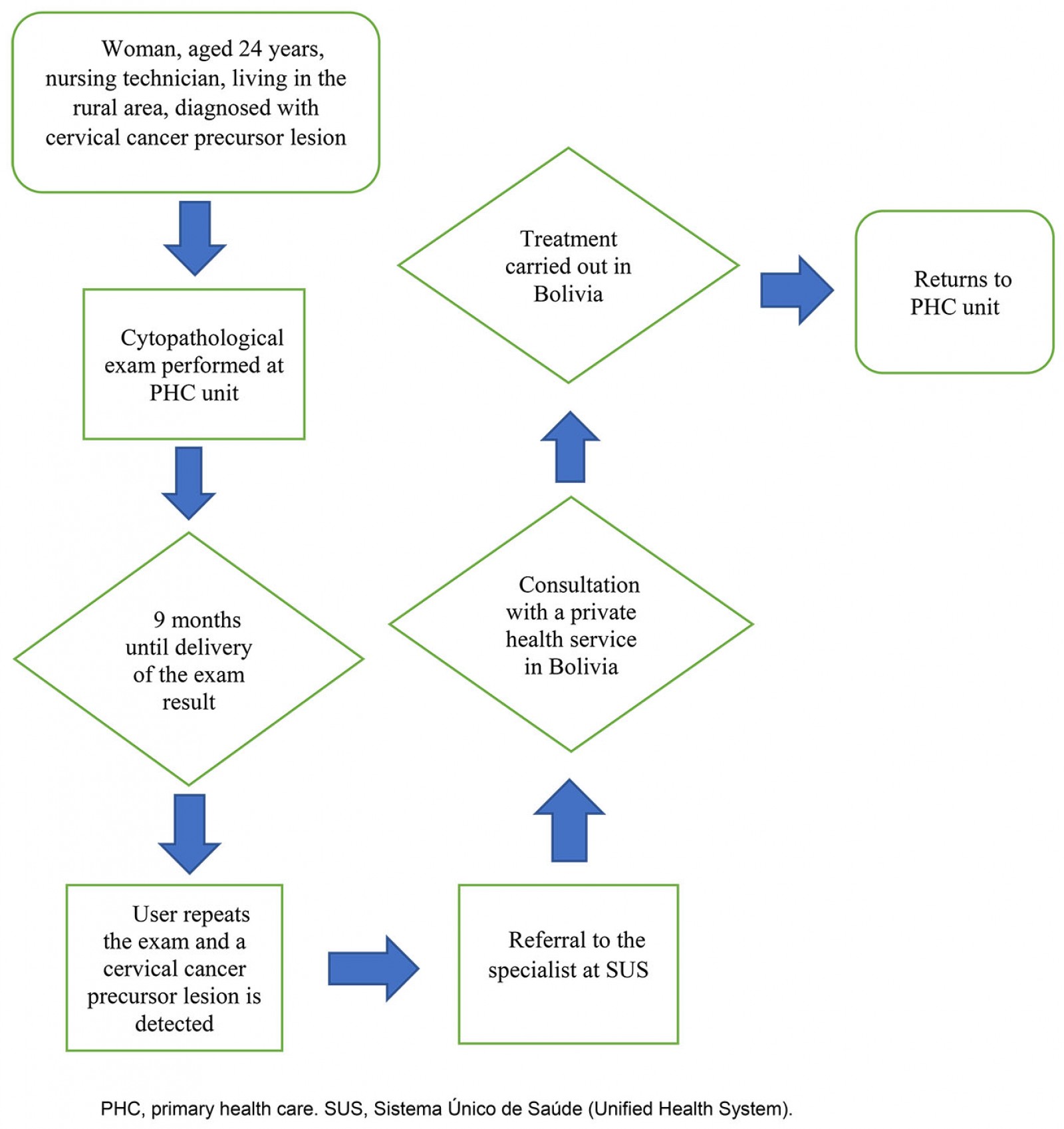 Figure 2: Care trajectory of a user with precursor lesion of cervical cancer, Assis Brasil, Acre, Brazil, 2019.
Figure 2: Care trajectory of a user with precursor lesion of cervical cancer, Assis Brasil, Acre, Brazil, 2019.
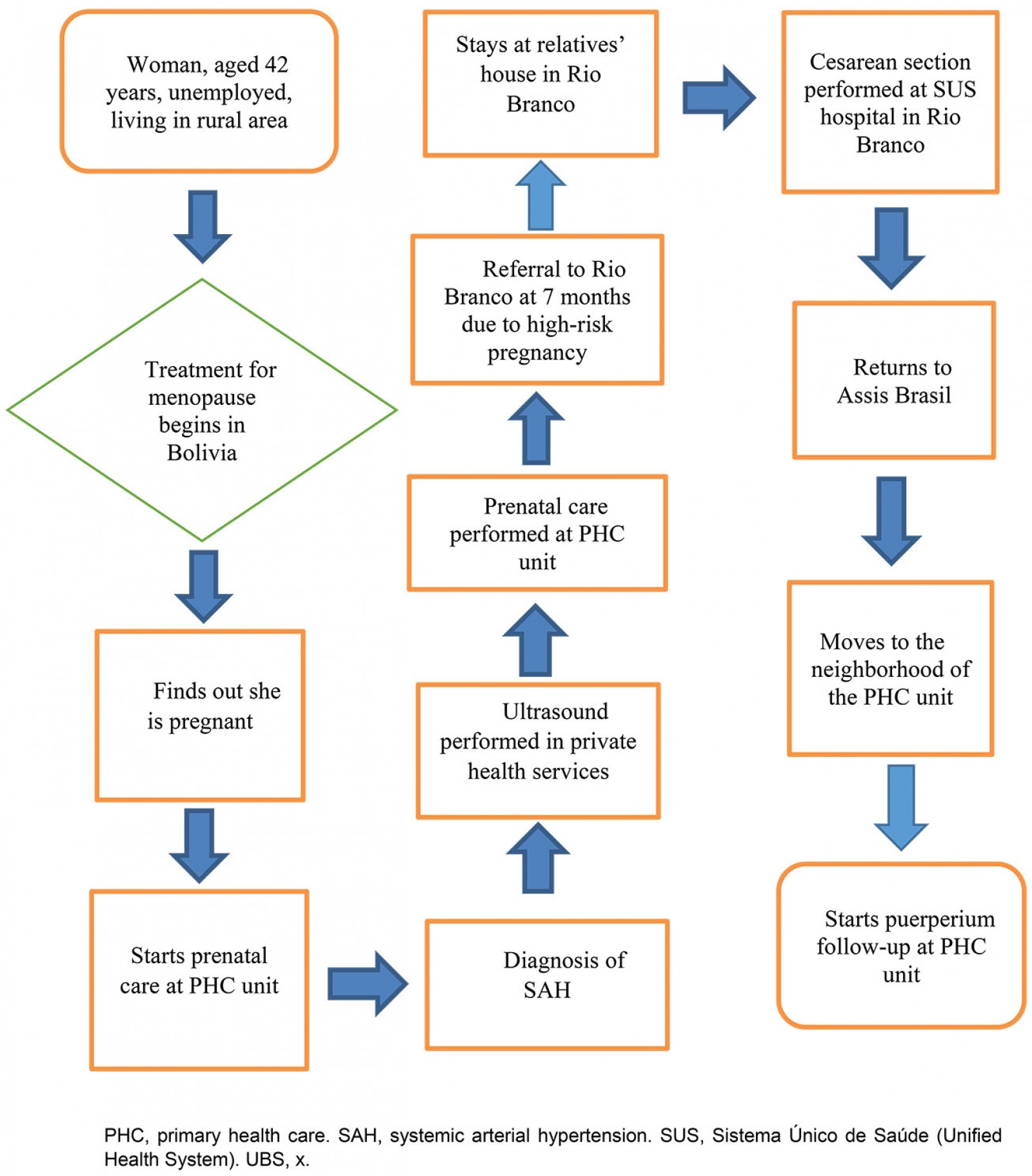 Figure 3: Care trajectory of a user of prenatal, childbirth and puerperium care, Assis Brasil, Acre, Brazil, 2019.
Figure 3: Care trajectory of a user of prenatal, childbirth and puerperium care, Assis Brasil, Acre, Brazil, 2019.
Discussion
The results of the study ratify that the care practices conform to a hybrid pattern of health system composition, in which the subsystems are activated in an overlapping, non-exclusive, and interactive way according to individual and community needs, and the insufficiency of the responses by the public health system. The model proposed by Kleinman14 does not ignore macrosocial (economic, political, and epidemiological) aspects of health care. It recognizes that, in all societies, care actions are more or less interrelated, and should be studied holistically4. The categorization is an analytical device.
Many and diverse informal system components are found in the search for health care. Family, friends, and community seem to play broader roles in care (accompaniment in visits and children care), underpinning the social support network that realizes the use of health services. It is not a rare phenomenon in rural areas, especially when women seek care13,24. On the other hand, such support also filled gaps not provided for by health policies, such as operationalizing adequate transportation from the rural area to the municipality’s headquarters, to which people are carried in hammocks for days. Thus, the informal network is a survival strategy, with many contacts, proximity to families, groups of relatives, neighbors, and friends, who are the primary social support source24.
Even in Nordic countries, with universal healthcare services, family members and caregivers of the elderly voluntarily assume the role of intermediaries between patients and healthcare services, seeking information, establishing dialogue, and negotiating with formal provider strategies to ensure more adequate care25. In this study, there were few reports of friends and relatives acting directly to facilitate access to health services, contrary to what some studies show26 – perhaps because they have the same scarce social capital as users, which is ratified by the profile of great poverty featuring the population of the municipality case. To a lesser extent, management and policy subjects were present, mediating access to health services, assuming functions either as direct service implementers (once again, transport), or facilitating their acquaintances’ access, as found in other national studies26.
The informal system comprised NGOs, armed forces, and the church. NGOs have had a long tradition in municipalities in the Amazon region. They have been working extensively in the health sector since the 1960s, from the training of indigenous health professionals to the provision of services27. With the constitution of the special indigenous subsystem, which makes up the formal public care system for this population, in the public and SUS sectors, the role of NGOs has become more restricted to partnerships with public bodies, such as projects for the mobilization of traditional midwives. With the establishment of the special indigenous public subsystem, the NGOs’ role has become more restricted to partnerships with public bodies, as in projects for the mobilization of traditional midwives27. In the case studied, they play a role in recruiting health personnel – in many cases, with unstable work and job insecurity.
The armed forces, which are not part of the formal system, have a tradition of providing health services in remote regions of the country, albeit from a campaign perspective28. In the case studied, the actions complement the SUS as they became the leading provider of health care for the population with the public system’s strengthening. Specific PHC policies such as the fluvial Family Health Strategy began to play an important role in assisting the riverine population6,29, sometimes previously served by health facilities via philanthropy6 or by the armed forces.
Churches also played a complementary role, providing logistical support, such as providing space for health activities. Hosting the production and sale of home-made medicines at their headquarters could indicate an approach to culture and support for local healing traditions. Studies show that in territories with scarce health resources, such as rural communities, religious institutions represent one of the most reliable and sustainable community resources that can be added to efforts to develop health promotion activities30.
Many intersections of the popular system were observed in the care mosaic in the remote rural municipality of Assis Brasil. The region itself is a multicultural territory. Secular healers such as shamans, prayers, and midwives, and the use of medicinal herbs and other natural resources, are part of the care scene, especially among the traditional populations of the territory. As found in other researches15, the narratives produced by users about their positive experiences encourage the use of practices of the popular system by other members of the community.
In some regions of the world, health practices linked to traditional medicine have widespread use in the prevention and treatment of communicable and non-communicable diseases, with phytotherapy sometimes being the most widely used resource31. Different experiences and perceptions were observed between users and professionals, especially when the use of such resources delay or replace the search for care in the formal network or when used concomitantly with formal treatments, which could bring drug interactions. On the other hand, professionals recognize certain herbs’ therapeutic potential and the relevance of empirical and traditional knowledge, as found in other studies in the Amazon region6, which may avoid omission about its use for fear of negative attitudes from healthcare providers15,31. In this sense, especially in rural territories, considering care practices while also caring for the cultural bond and the interactions that people establish with the environments is an expression of cultural competence32. Professional training directed toward culturally appropriate care has been advocated as a strategy to overcome communication failures between health professionals and people with diverse sociocultural backgrounds, in addition to favoring greater interaction between knowledge and health practices33,34.
Another aspect identified is that, sometimes, popular resources, considered inappropriate care35 in some studies, are triggered due to mainly geographic and economic barriers to access to formal health services15,36, such as in rural territories. However, the preference for traditional care also derives from attitudes aligned with a patient’s sociocultural, religious, and spiritual values regarding health and illness, which may act as an ‘attraction factor’36. While such therapeutic practices occupy spaces due to gaps in the country’s public health system, it is observed that popular medicine is found in places with access to official services. Its own body of knowledge is in constant transformation and incorporates formal medicine elements and part of certain territories’ health worldview37.
Limitations
In this article, the perception of three important actors for the provision, organization and practices of care in a Brazilian rural scenario were considered. Traditional agents of care were not included, this being one of the limits of the study and an open field for future research. The inclusion of such actors can contribute to the proposition of more cooperative policies and practices between the popular and biomedical subsystems and to the achievement of greater cultural competence.
Conclusion
The informal subsystem was identified to have a triple role in the composition of health care: from the perspective of solidarity and empathy, in filling gaps in health policies and services, and in the complementarity of actions developed by the formal system (the SUS). In the popular system, users make greater use of their autonomy and compose their buen vivir, based on traditions, spirituality, and ancestry38. Two patterns of relationship with the popular system were identified: in complementarity with the formal system, with specific or longitudinal use of its resources; and replacing formal practices. Indigenous and rural populations show greater adherence to traditional and secular practices. The level of resistance of health professionals varied according to the substitutive or complementary nature of such care in users’ therapeutic trajectories.
Complicated policies and processes such as health care have been implemented across the country, in general, with a poor understanding of rural communities’ context and culture. In this sense, identifying how the health system is organized and activated from the perspective of subsystems allows identifying which circumstances guide the search for care in the informal, popular subsystem and its substitutive and complementary relationships with the professional system. Understanding the dynamics and distribution of power among the subsystems, and their interrelationships in contexts of profound social inequality, can help to identify more appropriate policies and practices that respond to the needs and guarantee the full right to health of rural populations.
References
You might also be interested in:
2018 - Lack of Medical Resources and Public Health Vulnerability in Mongoliafs Winter Disasters
2014 - Gestational diabetes in a rural, regional centre in south Western Australia: predictors of risk


