Introduction
It is common for elderly people to experience functional decline because of a general physiological and metabolic decline, and the accumulation of risk factors for ill health throughout their lives. Global AGEing and Adult Health (SAGE) studies in six low- and middle-income countries (China, India, Russia, South Africa, Ghana, and Mexico) have shown that between 42% and 76% of people aged 65 years and over report difficulties with walking 1 km1. A study conducted in eight low- and middle-income countries (China, Cuba, Dominican Republic, India, Mexico, Peru, Puerto Rico, and Venezuela) found that the proportion of remaining life spent disability-free at age 65 ranged from the lowest in Peru (76% for men and 69% for women) to the highest in China (92% for men and 89% for women)2. In addition, low- and middle-income countries experienced the fastest-growing prevalence of non-communicable diseases that increase the rate of disability3.
Under the International Classification of Functioning, Disability and Health scheme4, age-related disabilities can be minimized by enhancing a person’s ability to function and improving performance by adjusting the social and physical environment. Previous studies have shown that living with others can reduce cognitive deterioration5. Conversely, living in disadvantaged communities poses a risk of cognitive decline in elderly people6. An age-friendly environment is required to improve mobility and the productivity of day-to-day activities7-10. Leisure activities, such as visiting a friend, relative, or tourist attraction, can reduce the risk of physical and cognitive disabilities11,12. Other studies have shown that a high protein consumption and physical activity are beneficial for the cognitive stability, muscle mass, and mobility of the elderly13-17. Paid employment can reduce the chance of functional disability among the elderly18. As a result, age-related disabilities and the onset of chronic conditions might be avoided or postponed.
East and South-East Asia were home to the largest proportion (37%) of the world’s elderly population in 2019, and about 16 million people aged 65 years and over lived in Indonesia19. Elderly Indonesian people were confronted with income instability, where assets and labor income were the primary sources of support in their old age19. The high incidence of non-communicable diseases and increasing age-related disabilities increased older Indonesian people’s vulnerability20. In people aged 65 years and over, 46.5% had a form of disability21.
In 2018, 49.8% of elderly Indonesian people were still working22. Participation of elderly rural people in the labor force was primarily motivated by a desire for financial security23. The proportion of elderly rural people (6.8%) receiving social security was roughly one-third of that of urban elderly (19.5%)22. Among elderly rural labor force participants, 73.9% worked in the traditional agricultural sector22.
Evidence has shown that elderly Indonesian people living in cities have a better functional capacity than elderly rural Indonesian people24,25, which might be attributed to the adequacy of health services provided. However, another study found that older Indonesian people with the worst functioning, quality of life, and health status lived in more economically developed semi-urban areas26. A safe and comfortable place to live was required to support the lives of the elderly. Elderly Indonesians are inclined to live with their children and grandchildren27. Data showed that in 2018, 42.5% of elderly urban people and 43.9% of elderly rural people lived with three generations22. Differences in urban–rural characteristics could contribute to the difference in disability experienced by the elderly in Indonesia.
A study on urban–rural differences was carried out to predict the functional status and disability of elderly people in Indonesia. This study used functional status questionnaires of the National Socio-Economic Survey that had adopted the short set of questions of the UN Washington Group on Disability Statistics4. The degree to which the disability of elderly Indonesian people in urban and rural areas limited their participation in society was examined.
Methods
Data and participants
The cross-sectional design used the National Socio-Economic Survey 2018 dataset of the National Socio-Economic Survey, the Socio-Culture and Education Module (Susenas-MSBP)28, conducted by Statistics Indonesia (BPS). The 2018 Susenas-MSBP samples were drawn by using a two-stage stratified sampling design. Selecting census areas with census blocks stratified by urban and rural areas, and wealth index, was the first stage. Stratification was based on the master sampling frame, the 2010 Indonesia national census. The second stage was selecting households in each census block from the updated household listing. In total, 75 000 households were sampled. This study identified 16 054 elderly people aged 65 years and over for the analysis.
Measures
The outcome variable was disability. The set of questions included in the Susenas was consistent with the short set of questions of the UN Washington Group on Disability Statistics, with six functional domains: (1) seeing, (2) hearing, (3) walking or climbing steps, (4) remembering or concentrating, (5) self-care, and (6) communicating. Each question has four response criteria: (1) no difficulty (no); (2) yes, some difficulty (moderate); (3) yes, severe difficulty (severe); and (4) yes, cannot see, hear, walk or climb steps, remember, self-care, or communicate at all (extreme). In this study, an elderly person was defined as having a disability if they had ‘some difficulty’ in at least two of the six domains, or had ‘a lot of difficulty’ or ‘cannot do at all’ in at least one domain. This threshold has been reported in several studies conducted in other countries29-31.
Health conditions were used to define the state of health (yes, no). Health conditions were measured by medical symptoms, such as fever, cough, colds, diarrhea, recurrent headaches, or other illnesses, followed by assessing the inability to perform their daily routine, such as work and chores, because of the health conditions.
Individual characteristics included age (65–74, 75–84, ≥85 years), sex (male, female), marital status (currently married, other), employment status (employed, unemployed), educational attainment (low, medium, high), leisure activities (yes, no), protein consumption, physical exercise32 (150 minutes or more per week of moderate-intensity aerobic and muscle-strengthening activities, less than 150 minutes per week of moderate-intensity aerobic and muscle-strengthening activities, and no physical exercise), and household wealth index (low, middle, high). ‘Other’ in the marital status was never married, divorced, or widowed. Work was defined as an activity to obtain or help to earn income or profit for at least 1 hour in the week preceding the survey. In 2018, the mean years of schooling in Indonesia was 8.34, equivalent to middle school33. Thus, educational attainment in this study was divided into three categories: low (primary school or no formal education), medium (middle school), and high (high school and university). Leisure activities were defined as a family/relative visit or a trip to a tourist attraction, or both, during the 6 months prior to the survey. Protein intakes in this study were based on the brief Food Frequency Questionnaire, which was not designed for clinical use but rather to identify trends in the consumption of food groups derived from animal and plant sources34. Because the survey included a question about weekly consumption, intake was considered high when each type of protein was consumed seven times (representing daily intake) or more per week (high plant and high animal content), and low when consumed fewer than seven times per week (high plant and low animal content, low plant and high animal content, and low plant and low animal content). Household wealth index was computed with a multivariate approach using the polychoric principal component analysis based on the type of dwelling floor, the primary source of lighting, the primary source of cooking fuel, the primary source of drinking water, the facilities for defecating, the final place for feces disposal, telephone ownership, the presence or absence of internet accessibility for household members, and the educational attainment of the head of the household35. The decile of household wealth index was then determined to create cut-offs defining three wealth index categories35.
The environmental factor was Java–Bali and outer Java–Bali, decided by considering the infrastructure development of the region. Urban–rural areas were used to stratify other disability predictors.
Statistical analysis
The Susenas sample was drawn using a two-stage stratified sampling design (census block stratified by urban/rural and wealth index classifications as the first stage, then households within each census block as the second stage), and the survey design as well as the sampling weight were always incorporated into analysis35.
Descriptive analysis was used to show (1) the distribution of functional difficulties for elderly people aged ≥65 years, stratified by urban–rural areas; and (2) the sociodemographic characteristics of elderly people, stratified by urban–rural areas. It was recorded in percentages for all categorical variables. The χ2 test was performed to evaluate the significant correlation between the disability and each explanatory variable.
Multivariate logistic regression analysis was used to identify the association between a binary outcome variable and independent variables. This analysis was carried out separately by the place of residence (urban–rural) and the total elderly, respectively, to determine their general disability status. Data analysis was conducted using STATA package v15.1 (http://www.stata.com, StataCorp, College Station, Texas, USA). The adjusted odds ratios were reported with 95% confidence interval (CI) (p<0.05).
Data availability
The 2018 Susenas-MSBP datasets are available in agreement with the Statistical Dissemination Directorate of Statistics Indonesia (BPS), No. 20/LADU/0000/09/2020. The BPS is an Indonesian Government institution responsible for conducting statistical surveys. This dataset obtained from the BPS is without any personal identity, such as name or address. The BPS has imposed legal restrictions that prevent the public sharing of data.
Results
Table 1 shows that the disability prevalence of 16 054 participants was 35.1% (ie 35.1% of elderly people had a disability). Seeing (32.8%) and walking/climbing steps (29.0%) were the most common. Disability among the elderly who lived in rural areas (36.1%) was higher than among elderly who lived in urban areas (34.3%).
About 70% of participants were aged 65–74 years (Table 2). A high 80.9% of the participants had only a low level of education. Most of the respondents were unemployed (64.4%), did not do physical exercise (87%), and lived in the Java–Bali region (67.4%). Only 30.5% consumed a high balanced protein intake daily.
Approximately 52% of the respondents lived in urban areas. Of these, 29.2% were employed, 29.6% had a medium-to-high level of education, 36% had a high balanced protein intake, and 54.6% took part in leisure activities.
Approximately 48% of the respondents lived in rural areas. Of these, 42.5% were employed, but only 7.9% had a medium-to-high level of education, had a high balanced protein intake daily (24.6%), and participated in leisure activities (44.3%).
The χ2 test (Table 3) shows that the differences in disability were significant in all the predictors (p<0.05).
Table 4 shows the results of logistic regression. The elderly who were ≥85 years old (odds ratio (OR) 4.57; 95%CI 4.54–4.59) were 4.6 times more likely to have a disability than those 65–74 years old. The elderly who were unemployed (OR 2.48; 95%CI 2.47–2.49) had a higher risk of disability than those who were employed. Compared with respondents who did leisure activities, those who did not (OR 1.77; 95%CI 1.76–1.78) were 1.8 times more likely to have a disability. The variables female, unmarried status, low protein intake, and health conditions were risk factors for disability. Physical exercise among the elderly was a protecting factor.
Table 1: Disability status of the elderly, stratified by urban–rural areas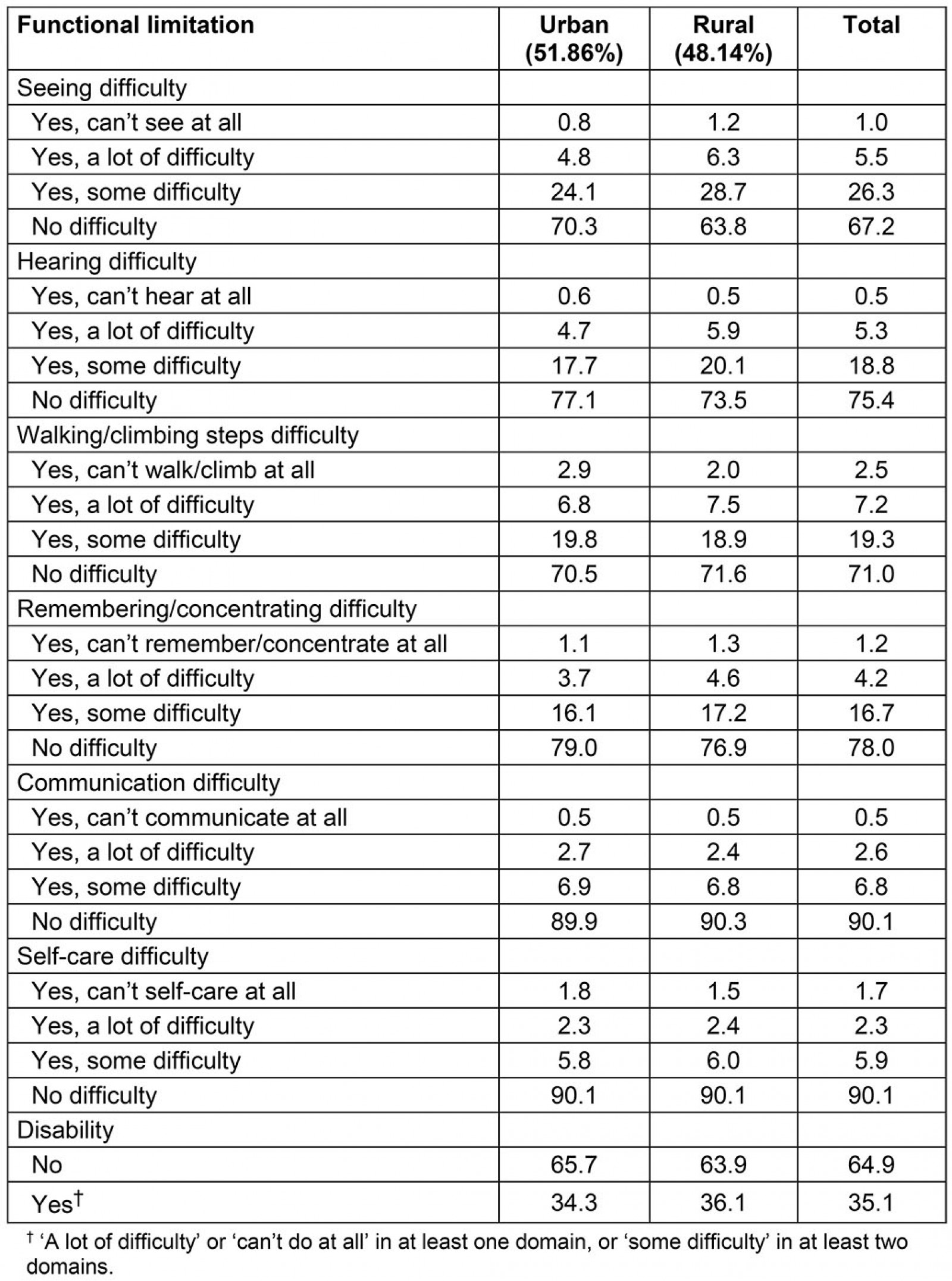
Table 2: Sociodemographic characteristics of the elderly, stratified by urban–rural areas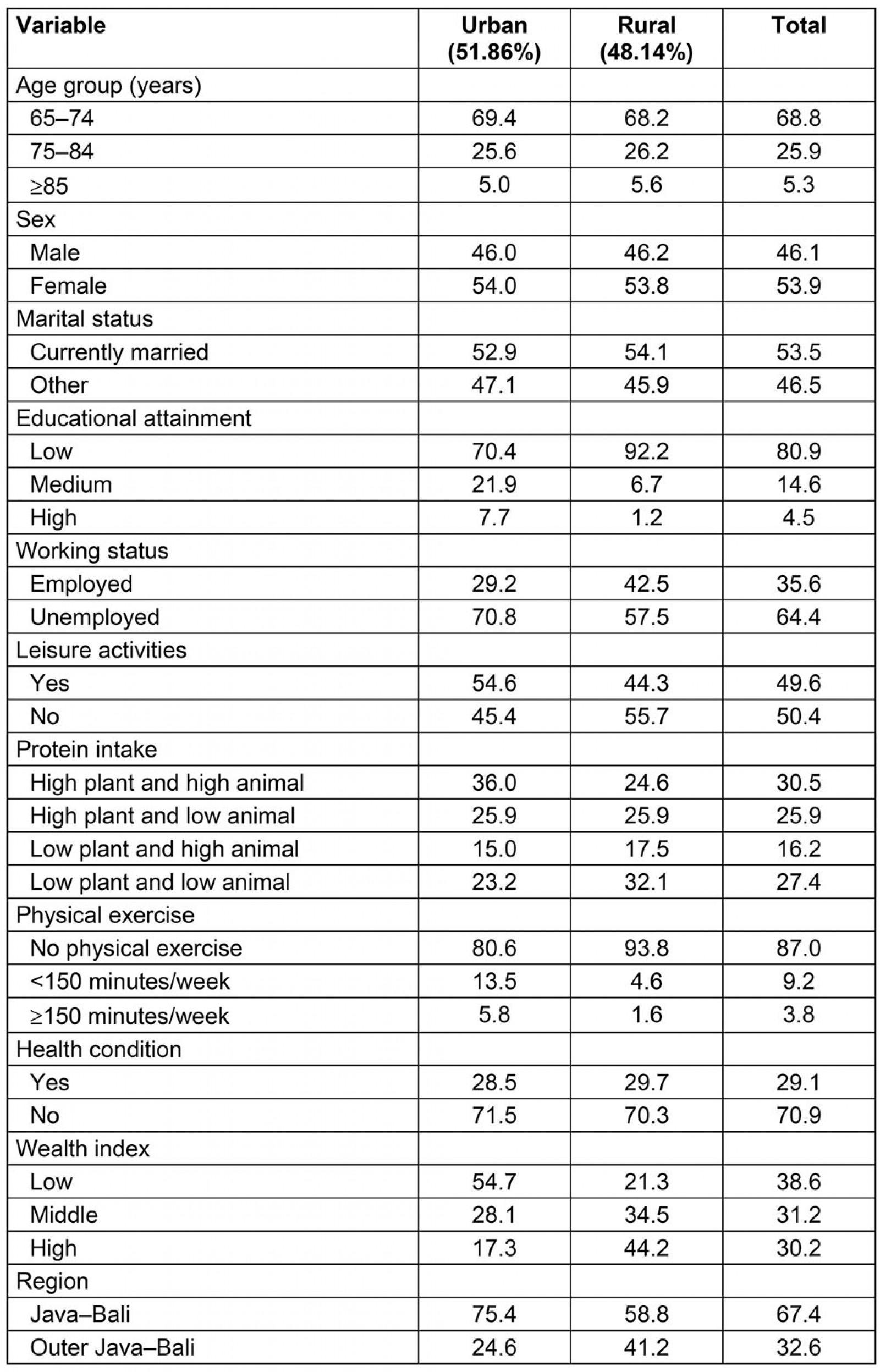
Table 3: The proportion of disability for elderly urban and rural people 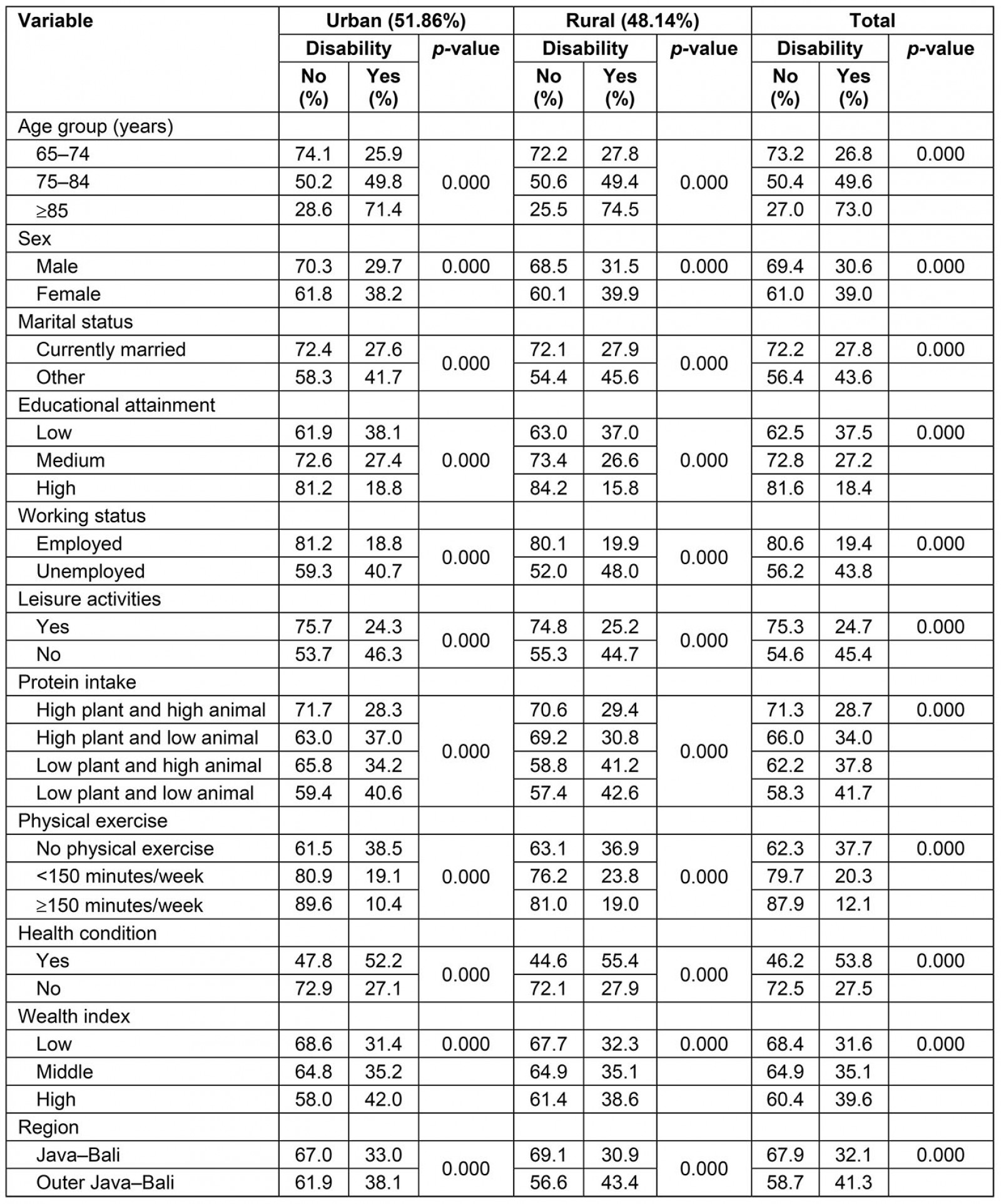
Table 4: Adjusted odds ratios for the multivariable logistic regression model for the predictors of disability among elderly people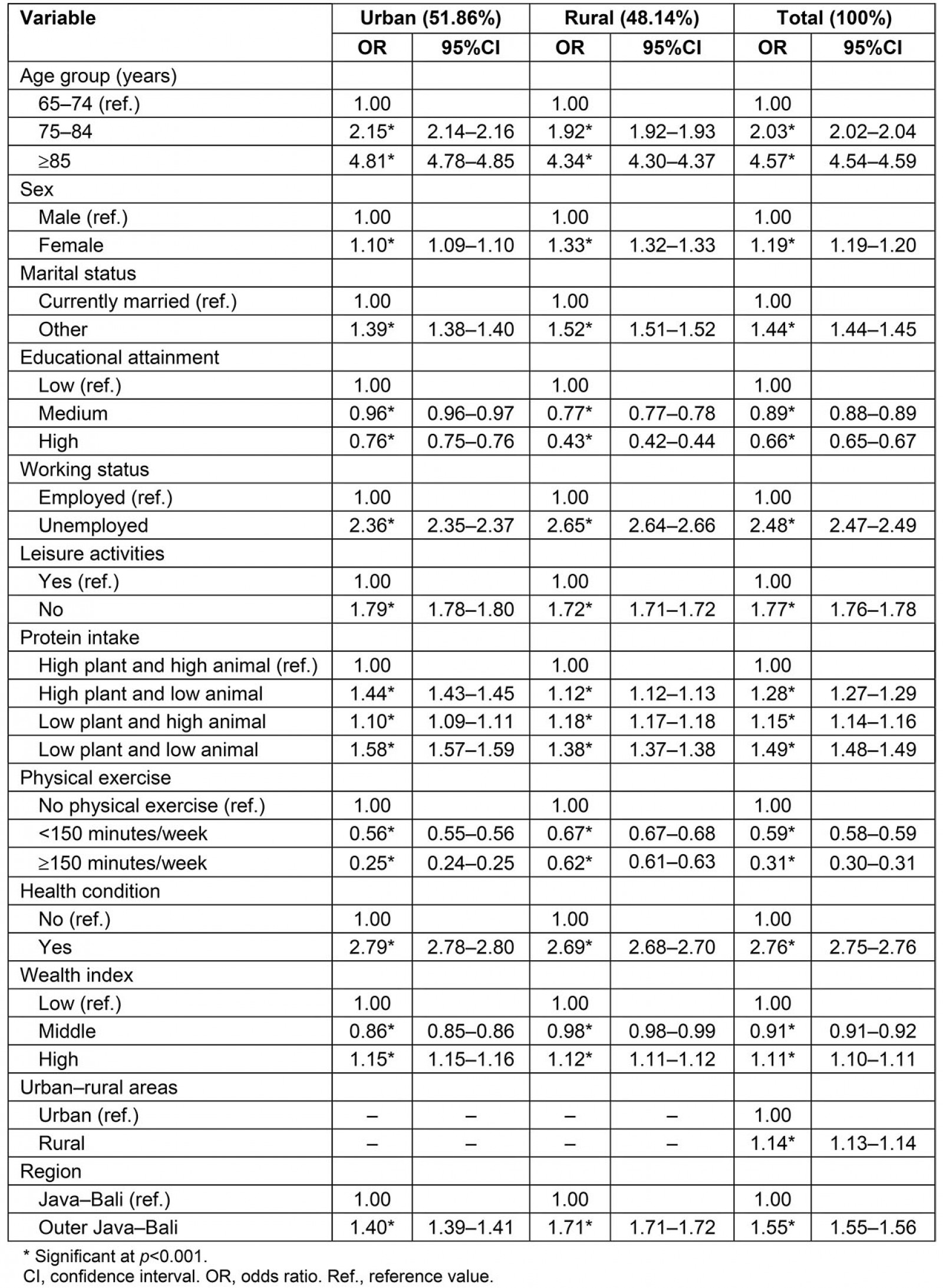
Discussion
As indicated in the model, disability in the elderly was associated with several factors, but age was the most important factor. Functional disability was positively associated with increased age of the elderly29,30,36.
The next significant factor that was found to be negatively associated with functional disabilities in the elderly was at least 150 minutes per week of moderate-intensity aerobic and muscle-strengthening activities. Performing physical exercise for at least 150 minutes per week was associated with a 75% reduction in disability status among elderly people living in urban areas (Table 4). However, in rural areas, performing 150 minutes or more of physical exercise per week was associated with only a 38% reduction in disability status among elderly people. The ‘disadvantage’ of elderly rural people could be due to a variety of factors. This ‘disadvantage’, along with other physiological and environmental factors, contributed to a higher overall prevalence of disability among the elderly in rural areas.
As previously stated, elderly rural people were primarily employed in the traditional agriculture sector22, which typically requires vigorous physical labor20. Seventy-five to 150 minutes of vigorous intensity activity per week is equivalent to 150–300 minutes of moderate physical activity per week, which is beneficial for older adults32. The model showed that paid work was negatively associated with disability among the elderly18. However, while employment status was associated with a reduction in functional disability among the elderly, work with strenuous physical labor as a means of survival from economic pressure must be reconsidered, especially in rural areas of developing countries, such as Indonesia.
The findings revealed that elderly rural people had a less balanced daily protein consumption than elderly urban people and participated in fewer leisure activities. As elderly rural people were more likely to be involved in strenuous physical labor in traditional agriculture areas, they required a high balanced protein intake to support their physical activity and reduce the risk of functional disability16. In addition, leisure activities were important for the promotion of physical and mental health37,38. As a result, it is necessary to emphasize the importance of socialization with family and friends and leisure activities in assisting the elderly in rural areas with disability issues. Mental activities, such as reading, writing, and cultivating cultural interests (singing, playing music, and painting), could be used as leisure activities by elderly rural people who have limited mobility and live in areas with limited infrastructure development39.
A lower percentage of elderly rural people had a high level of education. Findings show that higher education level is negatively associated with disability among the elderly. A study found that people with disabilities who have higher educational attainment had higher economic and social coping levels to deal with their disability40.
Elderly people living in outer Java–Bali areas were positively associated with functional disabilities. The provinces of Jakarta, Banten, West Java, Central Java, Yogyakarta, and East Java make up Java island. The Public Health Development Index was designed to monitor the coverage and inequity of health services in Indonesia. Bali Province and five provinces on Java island (Yogyakarta, Jakarta, Central Java, East Java, and West Java) were at the top of the 2018 Public Health Development Index41. Previous studies have reported the benefits of infrastructure development in using health services42 and reducing mobility difficulties10 for older people. Rural areas in the Java–Bali region are more developed than those in the outer Java–Bali region; for example, electricity is available in all rural areas of the provinces of Jakarta, Yogyakarta, Banten, and Bali43.
The model showed that, among the elderly, having a health condition was positively associated with disability. Vision and mobility difficulties were the most prevalent among the elderly in Indonesia.
The model also indicated that marital status was associated with a functional disability26,30. In line with other studies, being an older woman was positively associated with functional disability29,44.
After controlling for other predictors, the model found that disability reported by elderly people with a middle household wealth index was 9% lower than for those with a low household wealth index (Table 4). However, elderly people with a high wealth index were significantly associated with the highest risk of disability (Table 4). The model cannot supply reasons for this. A longitudinal study in the UK found some older people living with disability had accumulated assets while they were still in good health in their youth45. As a result, it was possible that elderly people who had become disabled later in life lived in households with a high wealth index. Also, a study in Indonesia found that older people preferred to be cared for by their children27. According to a report, nearly half of Indonesia's elderly lived with three generations22. If the head of the household has a higher educational status and better living conditions, older adults living with disability and living with three generations might have a high household wealth index.
The strength of this study is the large, nationally representative dataset that makes it possible to generalize the results to a national level. However, data on disability status may have been reported by the respondent’s family if it was difficult for the respondent to provide an answer; this could be a source of bias. It is also difficult to establish a cause-and-effect relationship because the cross-sectional design analysis only measures the association of variables.
Conclusion
This study shows that in Indonesia, elderly rural people are more vulnerable to functional disability than elderly urban people. This finding can be attributed to rural older adults having a lower education level, having a less balanced protein intake, and taking part in fewer leisure activities. Promoting a higher protein intake and more leisure activities with family and friends might allow rural elderly people to maintain their physical and mental health. Leisure activities for elderly rural people with mobility difficulties and living in areas with limited infrastructure development could be directed towards mental activities.
References
You might also be interested in:
2022 - COVID-19 fosters social accountability in medical education
2019 - A case report suggestive of strongyloidiasis infection occurring in temperate Australia.




