Introduction
Obesity is a complex condition with social and psychological dimensions, affects almost all age and socioeconomic groups, and threatens both developed and developing countries. Obesity, which paradoxically coexists with malnutrition today and has risen rapidly in recent decades, is a global public health problem. In 2038, it is estimated that approximately 38% of the world’s population will be overweight and 20% will be obese1. The global increase in obesity to epidemic proportions led to the emergence of the ‘globesity’ concept2,3. According to the Turkish Health Survey conducted by the Turkish Statistical Institute, the obesity rate in persons aged 15 years and above was 19.6% in 2016 and 21.1% in 20194.
Childhood obesity is also a crucial public health problem seen in all countries globally, with an increase of 59% in developing countries in the past 30 years. For example, one out of every three children in the USA is overweight or obese5,6. In line with the childhood obesity epidemic globally, 14.6% of Turkish primary school children are overweight, and 1 in 10 children are obese7. The highest prevalence of weight gain is at primary school ages, when overweight and obesity prevention interventions are most effective8.
The increasing prevalence of childhood obesity is associated with the emergence of comorbidities that were previously considered adult diseases such as type 2 diabetes mellitus, hypertension, non-alcoholic fatty liver disease, obstructive sleep apnea and dyslipidemia, previously accepted as ‘adult’ diseases. Also, it is known that childhood obesity is associated with overweight or obesity in adulthood6. Physical illnesses are not the only serious threat to children’s health and wellbeing caused by obesity. Obese children are more prone to missing school days than their normal-weight peers due to factors such as isolation, bullying and illness9.
Recent data show that the age-standardized prevalence of obesity has increased significantly globally and there are significant regional differences across the world10. Potential factors leading to regional geographic disparities include lower socioeconomic status, limited access to affordable healthy food and physical inactivity. Another factor that causes regional differences in obesity prevalence is the evaluation criteria of obesity. Recent studies found that both the International Obesity Taskforce (IOTF) and Centers for Disease Control and Prevention (CDC) BMI criteria accurately predicted overweight, but the sensitivity of the IOTF obesity criteria was poor11,12. Differences that occur according to urban and rural living areas are seen in different trends around the world13. However, most studies report that individuals migrating from rural to urban areas have a higher risk of obesity. Compared to rural areas, possible explanations for urban obesogenic environments include higher fat and energy intake and lower physical activity levels due to sedentary living and passive means of transport14-16. In developing countries, the ongoing urbanization processes and obesity risk patterns that emerge during the rural–urban migration process within a country need to be better examined.
Few studies have examined the prevalence of overweight children and adolescents living in rural areas17,18. Although studies have shown that childhood obesity is higher in rural areas than in urban areas, direct comparison has not been made between children living in urban areas and those in rural areas13,19.
This study aimed to determine the prevalence of overweight and obesity in primary school students and their parents living in rural and urban areas in Samsun province, Turkey, and to evaluate any gender-specific differences.
Methods
Sample selection
This population-based, cross-sectional study was performed in Samsun, which is one of Turkey’s largest cities. Samsun is a developed city in the Middle Black Sea region, with a population approaching 1.5 million (Fig1). The study was conducted between 1 October 2016 and 30 November 2016 on a representative sample selected from 70 660 students in 388 primary schools by a multi-stage random sampling method according to the number of district students, the number of public/private primary school students, and the number of rural/urban students. A total of 9842 students from 62 public primary schools and six private primary schools, who were available from 68 schools included in the sample and voluntarily accepted to participate in the study, were included in the study. In the preliminary evaluation of the student questionnaires, 56 students were excluded from the study because they were older than 10 years. The analyses were completed with 9786 students.
 Figure 1: Geographic location of Samsun, Turkey.
Figure 1: Geographic location of Samsun, Turkey.
Data acquisition
The students were weighed in light clothing, and with bare feet or socks, using an electronic scale (Seca Ltd; https://de.secashop.com) calibrated at the beginning of each work day and sensitive to ±0.1 kg. Height was measured with a ±0.1 cm sensitive stadiometer (SECA Ltd, https://us.secashop.com/products/height-measuring-instruments) in an upright position, feet parallel, shoulders and hips touching a wall. Height and weight were measured twice, and the averages were recorded. BMI was calculated using the formula of weight (kg)/height squared (m2). In the BMI values classification, cut-off points in the CDC’s age- and gender-specific growth charts were used20. Depending on the age and gender, students with a BMI less than the fifth percentile were classified as thin, those in the fifth to 85th percentile range as normal, those between the 85th and 95th percentile as overweight, and those with a BMI at the 95th percentile or greater as obese.
After the data acquisition was completed, a questionnaire form developed by the researchers was sent to the parents through the students. A total of 6949 parents across the province were reached, and a questionnaire was conducted that inquired about their sociodemographic characteristics, height and weight information. When the collected questionnaire forms were pre-evaluated, the questionnaire forms of 94 people that were found to be incomplete and incorrectly coded were excluded from the study, and the results of 6855 parents were evaluated. The response rate was 86.9% in parents.
Statistical analysis
The Statistical Package for the Social Sciences v22.0 (IBM; http://www.spss.com) was used for statistical analysis of the data obtained. Qualitative variables were expressed as median (interquartile range (IQR) and quantitative variables as numbers and percentages. The Kolmogorov–Smirnov test was used to evaluate the compliance of the data for normal distribution. Since the data did not conform to a normal distribution, Kruskal–Wallis test and the Mann–Whitney U-test were used to analyze qualitative data, and the Spearman test was used for the correlation between the BMI values of parents and children. The χ2 test was used in the analysis of quantitative data. Statistical significance level was accepted as p<0.05.
Ethics approval
Institutional approval was obtained from the Directorate of National Education to perform the research in schools, and ethics approval was obtained from Ondokuz Mayis University Clinical Research Ethics Committee (OMÜ KAEK: 2015/2070).
Results
Of the 9786 students participating in the study, 5005 (51.1%) were male, and 4781 (48.9%) were female, and the mean age in both groups was 8.2±1.2 years. It was observed that the distribution of students according to age groups was similar in both genders. A total of 77.8% of the study group consisted of students from schools in urban areas and 22.2% in rural areas (Table 1).
The median BMI of the students was 16.2 (15.1–17.9). The median BMI values were 13% higher in boys than girls, while in urban areas they were 39% higher than in rural areas (Table 2). Considering BMI values, 7106 (72.6%) of the students were in the normal BMI group, 1650 (16.9%) were in the overweight group and 1030 (10.5%) were in the obese group. According to gender, as seen in Table 3, both overweight and obesity rates were found to be statistically significantly higher in boys than in girls (p<0.001). When BMI measurements were evaluated as per the place of residence, the rate of overweight and obese was found to be statistically significantly higher in urban than in rural areas (p<0.001) (Fig2).
Table 1: Distribution of students by location, gender and age group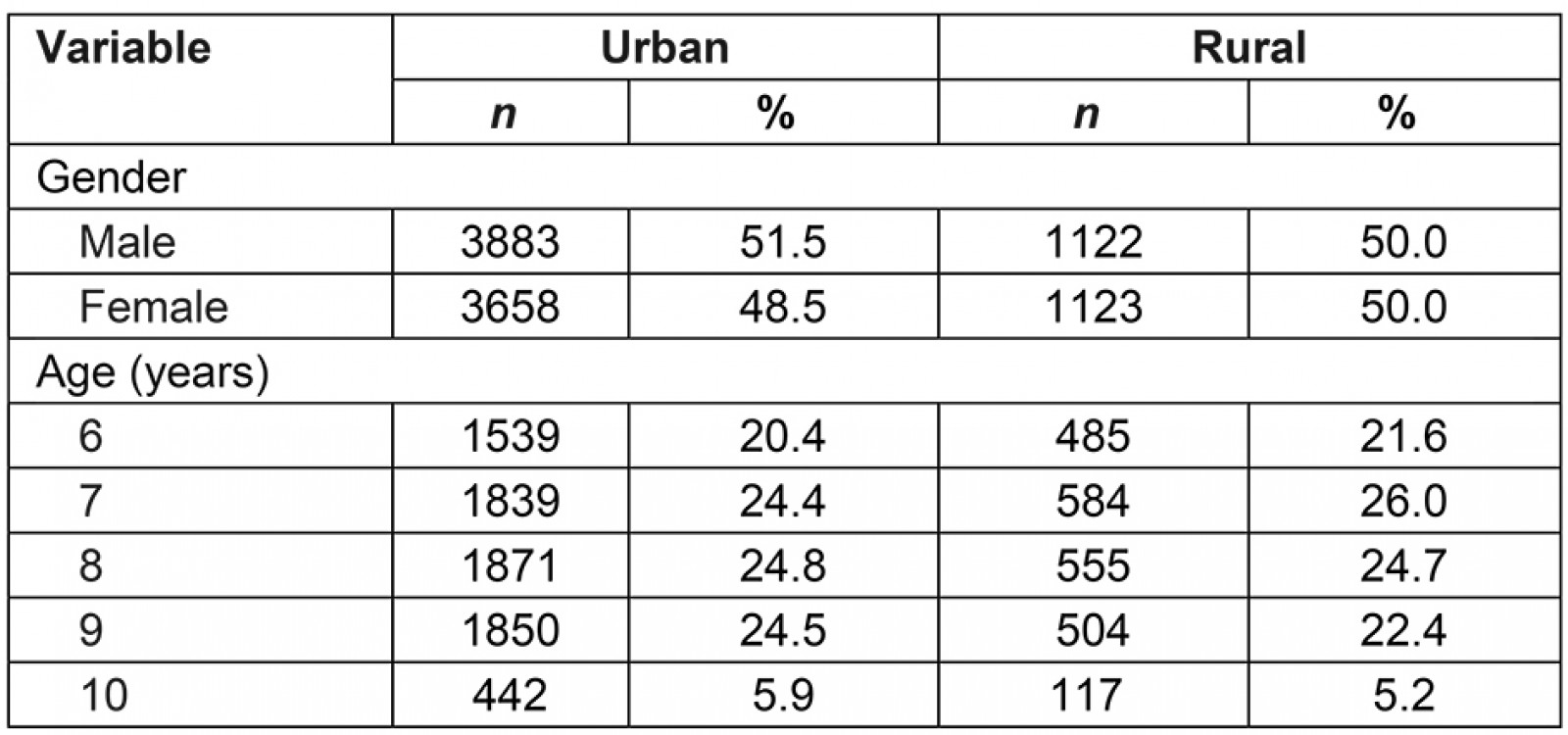
Table 2: Median student BMI values by gender and place of residence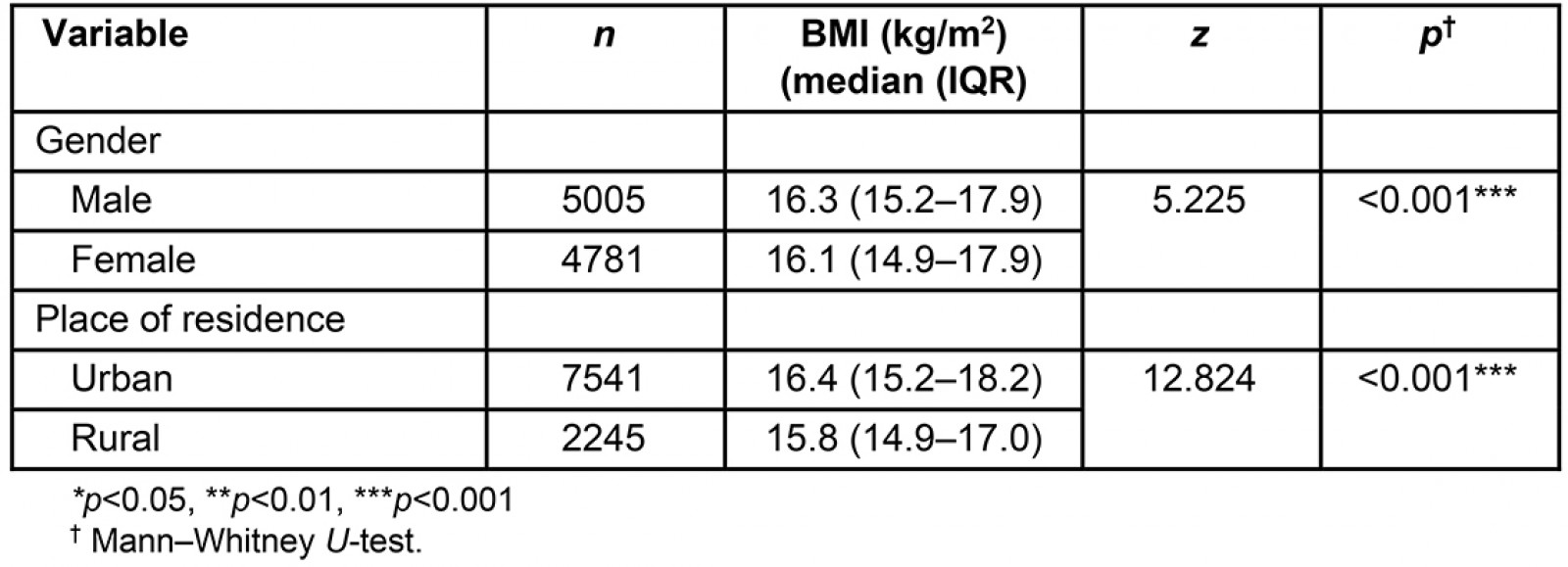
Table 3: Distribution of student BMI values by gender and place of residence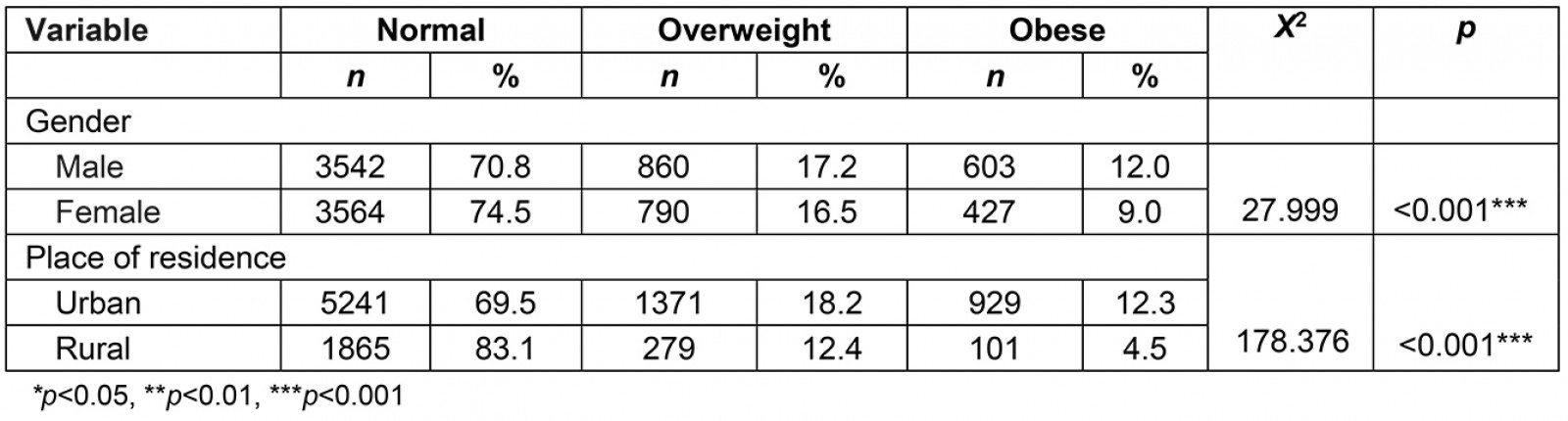
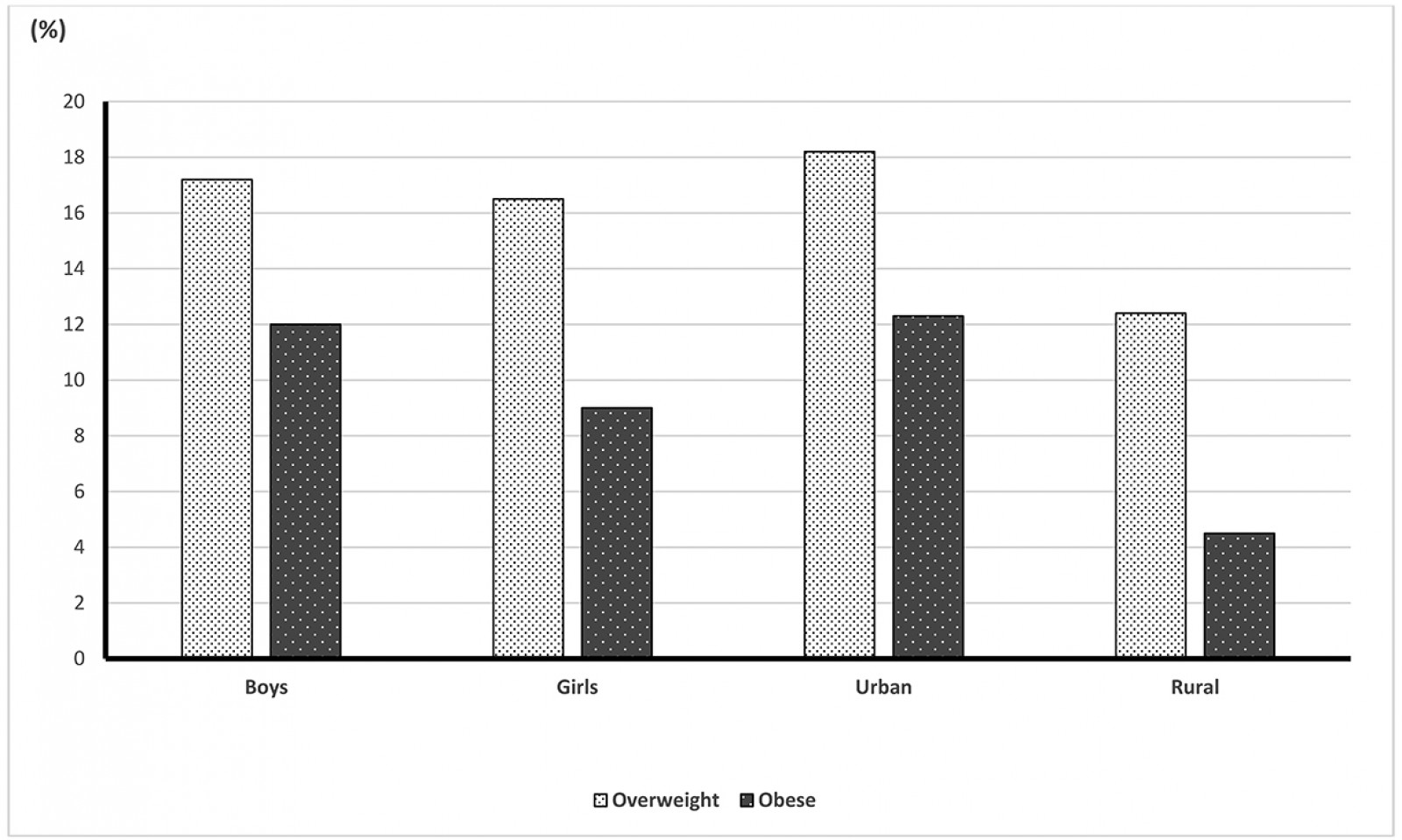 Figure 2: Prevalence of overweight and obese children by gender and place of residence.
Figure 2: Prevalence of overweight and obese children by gender and place of residence.
When the students’ BMI values were evaluated together according to age and gender, it was found that obesity was higher in boys than in girls in all age groups (Table 4). BMI values increased after the age of 8 years in both sexes (Fig3). A trend that showed a linear increase with age was observed in the rates of obesity in boys. The obesity rates in girls, which tended to increase until the age of 8 years, stagnated at the age of 9 years and showed a decreasing tendency at the age of 10 years (Table 5).
Table 4: Distribution of student BMI values by age group and gender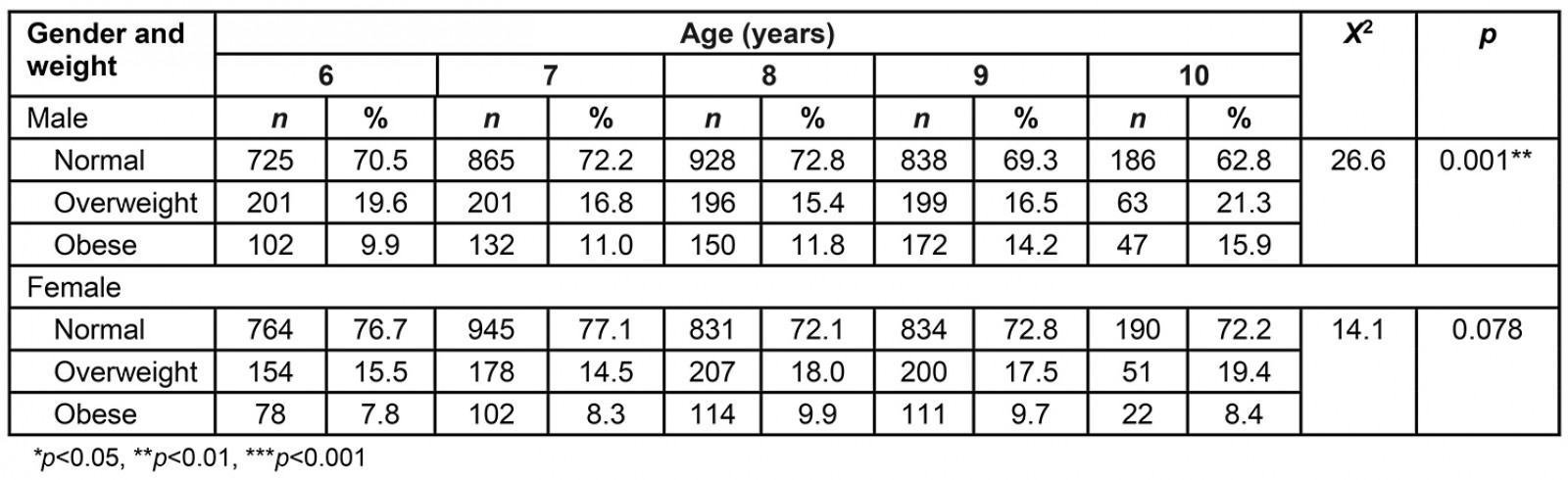
Table 5: Median student BMI values by age and gender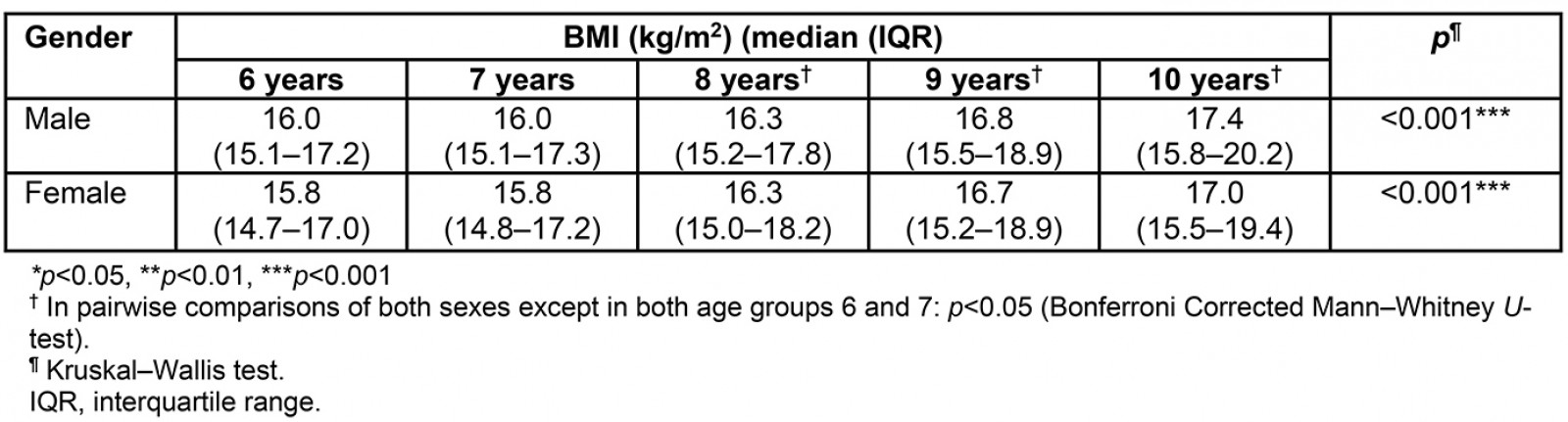
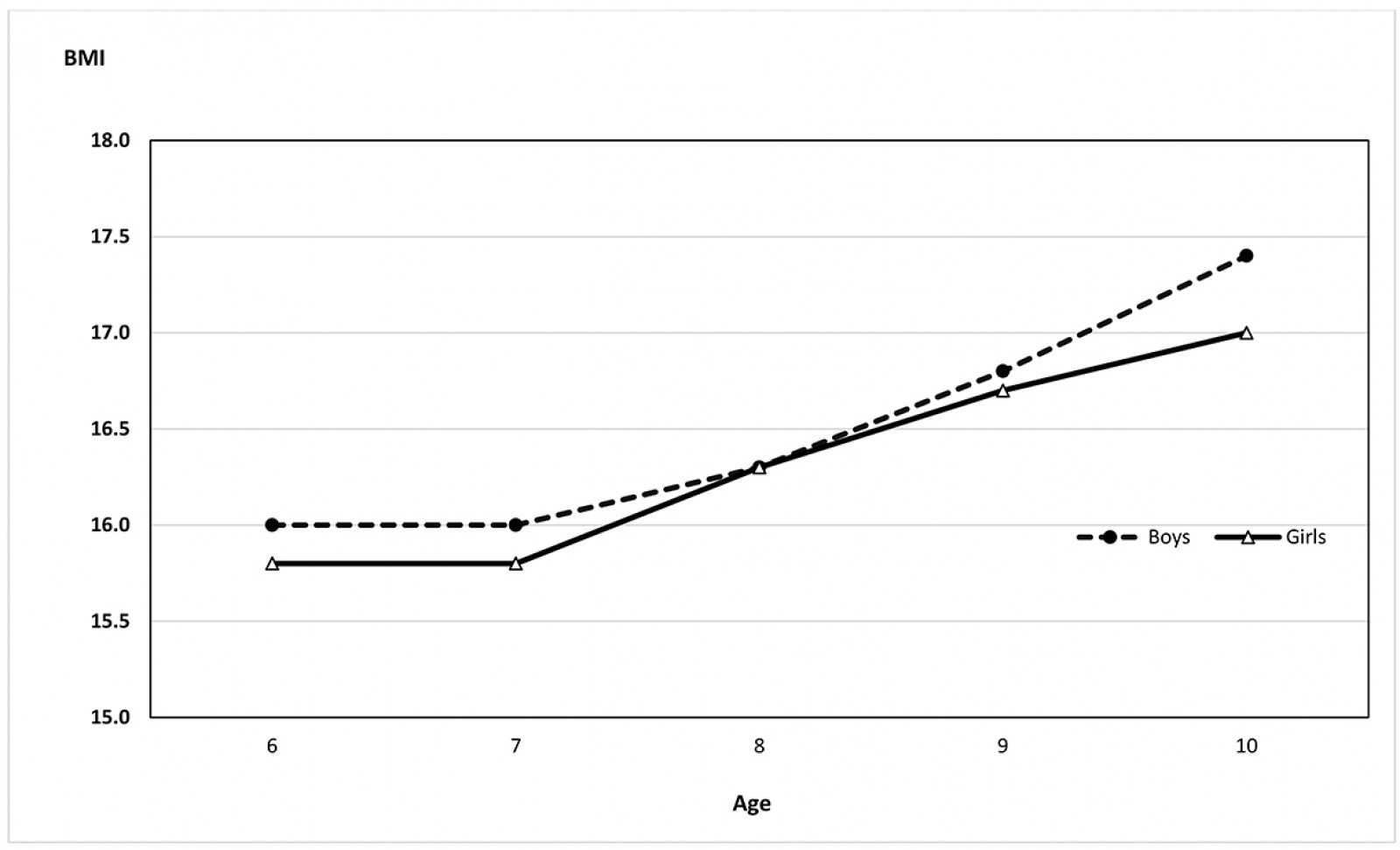 Figure 3: Trend of BMI value in the children by age and sex.
Figure 3: Trend of BMI value in the children by age and sex.
Of the total of 6855 parents, 5258 (76.7%) were mothers and 1597 (23.3%) were fathers. They had a mean age of 36.2 years (36.3 years for urban, 35.9 years for rural). The frequency of high school graduates or less was significantly higher in rural than in urban areas (p<0.001) (97.7% v 85.3%, respectively). The percentage of those who did not work was 64.3% in urban areas, while those who had any income-generating job constituted 33.8%, and the percentage of retirees was 1.9%. In rural areas, these percentages were 74.6%, 23.3% and 2.1%, respectively. The rate of non-working people living in rural areas was significantly higher (χ2=51.1, p<0.001).
According to the BMI values, 2453 (41.2%) parents were found to be normal-weight, 2293 (38.6%) were found to be overweight and 1202 (20.2%) were found to be obese (Table 6). While the frequency of overweight was higher in males than females, the frequency of obesity was higher in females than males. In terms of residence, both prevalences of overweight and obese parents were higher in rural areas than in urban areas (p<0.05). Median BMI values in parents were 25.9 (23.2–29.2). They were also higher in males and in urban areas (Table 7).
A positive and significant correlation was found between BMI value in the children and in their parents (r=0.183, p<0.001). There was a positive and significant correlation between the BMI values of parents and their children living in both urban (r=0.184, p<0.001) and in rural (r=0.209, p<0.001) areas.
Table 6: Distribution of parent BMI values by gender and place of residence†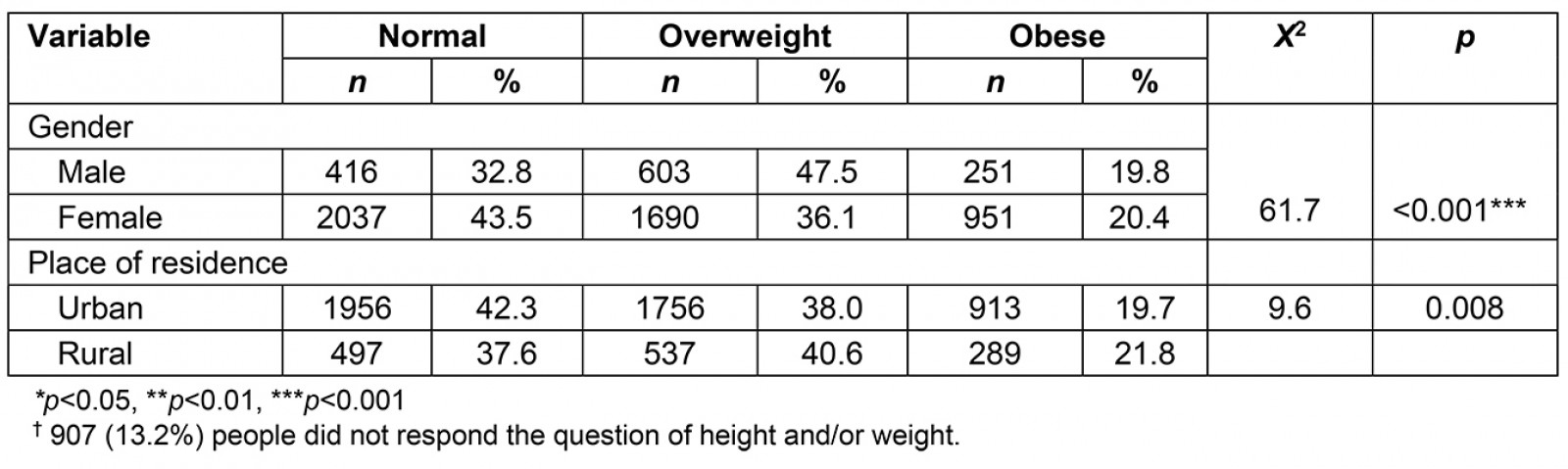
Table 7: Median parent BMI values by gender and place of residence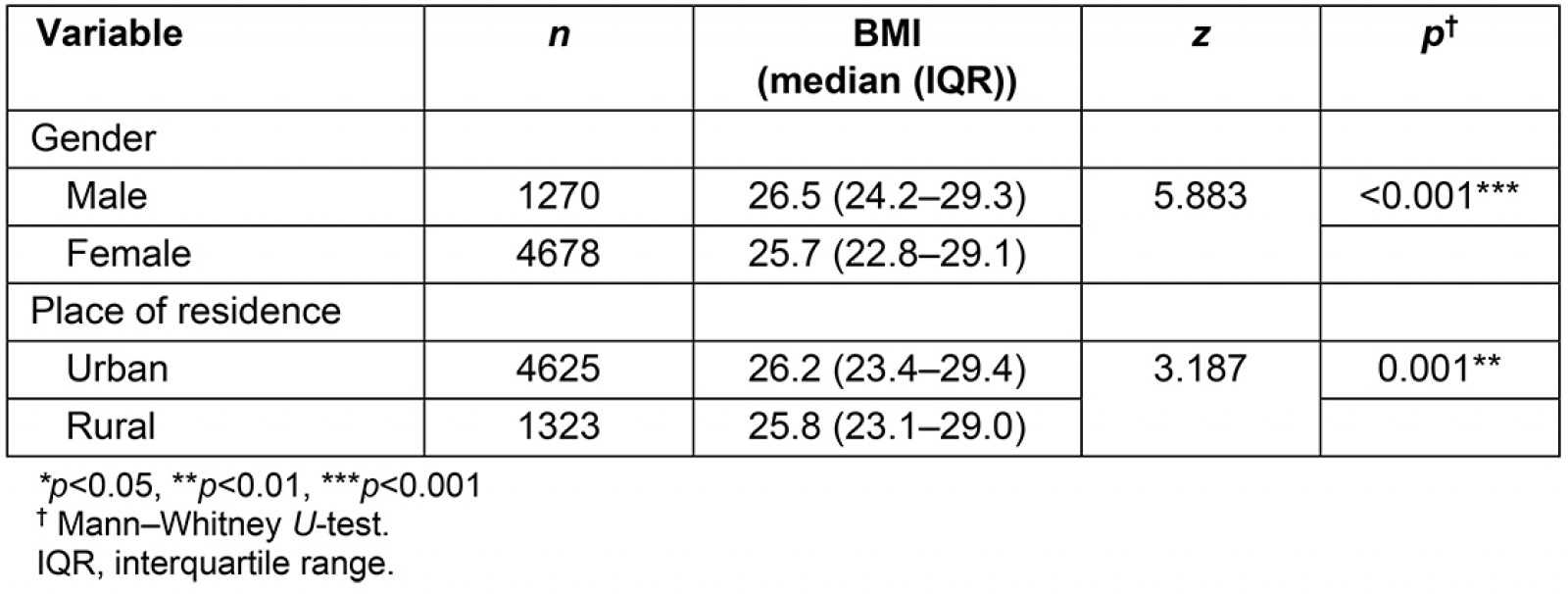
Discussion
Obesity prevalence was found to be 10.5% in students, and it was higher in boys and those living in urban areas. The rate of obesity in parents was higher in females and those living in rural areas.
Overweight and obesity among students
According to WHO, the number of obese children between the ages of 5 and 19 years was more than 124 million, while 8% of males and 6% of females were obese in 201621. In studies conducted in Turkey, the prevalence of obesity in children was found to be 7.3–16.5%7,22,23. When evaluated by gender, obesity was higher in boys than girls globally and nationwide21,24. Except for differences between samples in the studies conducted, it is thought that there may be various factors related to the higher incidence of obesity in boys. As well as factors such as environment, genetics, family and school associated with obesity, boys spend more time in screen-based sedentary behaviors associated with less physical activity. Lower prevalence of obesity in girls can also be associated with the fact that, overall, girls need and consume fewer calories than boys and they are more conscious of their body shape6,22,25.
Overweight and obesity among parents
The prevalence of overweight was higher in males, while obesity was higher in females. This result was in line with the data obtained in the Turkey Nutrition and Health Survey conducted by the Ministry of Health at the national level. According to WHO 2016 data, 11% of males and 15% of females in the world’s adult population were obese, and, similar to the present results, overweight was found to be higher in males, and obesity prevalence was higher in females as in many countries on the World Obesity Federation’s Prevalence of Adult Overweight and Obesity list21,26-28.
Overweight and obesity among students by residence
When the students’ BMI values were evaluated in terms of residence, it was found that, similar to the Monitoring the Growth of School-Age Children in Turkey study, the rate of overweight and obese people living in urban areas was high24. The higher prevalence of obesity in urban areas has been associated with having easier access to foods and beverages with high saturated fat and sugar contents, lack of suitable sports or playgrounds, ready availability of non-active transport, and spending more time in front of screens such as those of televisions, game consoles and smartphones29-31.
In recent years, it has been reported that industrial food marketers specifically target children through television or internet advertisements32. Repeated exposure to advertising for unhealthy food and beverages from all sources, such as on television, on social media, in-store, and in the outdoor environment, contributes to the consumption of these unhealthy products33. The proportion of all food and beverage advertisements were found higher in urban areas than those in the peri-urban or rural areas34,35. Therefore, it may be considered that children in urban areas are more exposed to these types of obesogenic food and beverage advertisements than children in rural areas36. They reach and consume these products readily by spending their own money or influencing their parents. WHO reported that childhood overweight and obesity, which was previously considered a problem of high-income countries, have increased today in low- and middle-income countries, especially in urban areas21. Consuming more calories in the form os packaged products and fast food, consuming less energy due to limited movement caused by urbanization and spending more time with screen media devices are some of the major problems that children in urban environments face, and alternative solutions need to be created to address them. Examples are development of school gardens, parks and other recreational areas for walking, cycling, and other physical activities for children and their parents. Activity-friendly routes can be created for families to go to regular destinations by foot, bicycle or other transportation systems. Local governments can create fun physical activity places to increase daily calorie expenditure, especially for children32,37.
Overweight and obesity among parents, by residence
Unlike students, when parents in the study group were evaluated in terms of residence, the frequency of being overweight and obese was higher in rural areas. This situation was similar in some studies conducted in other countries38-41. However, there are also studies in the literature suggesting that the prevalence of obesity is not different between rural and urban areas, or that the prevalence of obesity is higher in those living in urban areas15,42. Considering that parents’ education level in the present study was mostly secondary school or below, one of the reasons for the higher rate of obesity in parents living in rural areas is thought to be having lower education levels than those in urban areas. Similar to the present results, studies conducted in Turkey and other countries showed a negative relationship between education level and obesity28,43,44. Concerning low education levels in rural communities, health knowledge levels and healthy lifestyle behaviors may be less likely to occur. However, there may be a lack of awareness or the need to seek the correct information regarding health needs in rural societies. A study conducted in the USA stated that access to resources to address critical health problems is limited in rural communities45. They cannot benefit from nutrition education and services adequately due to the distance of health facilities or the lack of nutritionists in the facilities46. In this context, the primary healthcare units and personnel in rural areas should provide information on healthy nutrition and physical activity within the scope of combating obesity.
The difference in the prevalence of obesity in rural versus urban areas may also be related to income status. The frequency of obesity, which tends to increase significantly in developing countries as income levels decrease, because people prefer low-cost but high-calorie foods as income levels decrease, change their eating habits, and adopt a sedentary lifestyle38,47,48. Also, the migration of young people from rural areas to industrial areas and the decrease in agricultural-livestock activities in rural areas may have increased the proportion of the non-working population in rural areas. Due to reduced agriculture and livestock farming, access to primary protein sources, such as meat and milk, and the fresh vegetables and fruits required for adequate and balanced nutrition, is restricted. Lack of income may also have led to the increasing consumption of some unhealthy but cheaper carbohydrate products in the rural population. Policies to increase access to healthy and inexpensive food should be developed to combat obesity in rural areas. An example of this is some policies developed in Mexico, such as the provision of government-sponsored shops selling cheap, healthier food in remote rural areas46.
Similar to the studies conducted in Turkey and other countries, it was found that there is a relationship between BMI values in the parents and their children49. The high prevalence of obesity in children of obese parents could be caused by genetic factors, as well as by their similarity of everyday nutritional and physical activity habits. Therefore, in the fight against obesity, environmental rather than individual factors should be taken into account.
Strengths and limitations
The good balance of the present study sample regarding age, gender, public/private and rural/urban school student distribution increases the generalizability of the study findings. Working with a sample constituting all primary school students in the province and standardized measurements by trained personnel are considered strengths. Limitations are that the height and weight values used to calculate the parents’ BMI values were based on their self-reports, and some of them did not record all values, so there were incomplete data.
Conclusion
This study showed that the prevalence of obesity in Turkish children aged 6–10 years increased with age and there was a positive correlation between the BMI of children and the BMI of their parents. In addition, the BMI values were found higher among males gender and those living in rural areas. Combating obesity requires further multidisciplinary research to reveal the reasons for the differences based on place and gender, especially on nutrition and healthy lifestyle behaviors.
Acknowledgement
The authors thank Samsun Provincial Health Directorate, Samsun Provincial National Education Directorate; the management team of the ‘The tree can be bent only when it is young’ project; Dr Hatice Öz, who worked devotedly and diligently at every stage of the project; and the field study group formed by Samsun Provincial Health Directorate, for their valuable cooperation in the data collection process.



