Introduction
First introduced in the 1970s, the longitudinal integrated clerkship (LIC) curriculum model focuses on patient-centered care and continuity of clinical and cultural learning through patients, peers, health providers, community, and social resources. The definition of LICs by the Consortium of Longitudinal Integrated Clerkships in 2007 includes participating in the comprehensive care of patients over time, continuing learning relationships with these patients’ clinicians, and meeting core clinical competencies across multiple disciplines simultaneously through these experiences1. It can be implemented in urban or rural settings, and the components of community-based medical education and apprenticeship-based training are thought to mitigate the disproportionate distribution of doctors in rural and remote areas2-5. Rural LIC students are expected to have an interest in rural medicine, participate in the community, have the maturity to work independently, and display resilience. Many schools in the USA, Canada, and Australia have implemented LICs in undergraduate programs in different ways6-11. However, a few published reports in Asia are available12.
Due to the scarcity of rural doctors in Thailand, the study authors were interested to modify LICs in undergraduate curricula and to engage rural communities in education processes. It is expected that students will become familiar with rural contexts and be more likely to return to rural areas after graduation. The program responsible for learning environments in rural settings was launched in 2019. Being in the medical teaching profession, the authors were interested to find out student views on this new program in medical education as a way of monitoring outcomes and addressing any issues.
The educational environment evaluation is one of the main factors that regulates student learning. It acts as a hidden curriculum and has a major impact on student learning. An excellent environment is reflective of a quality curriculum. Various methodologies have been utilized to investigate educational climate including the Dundee Ready Education Environment Measure (DREEM) and the Medical Education Environment Measure (MEEM). Several subsequent tools have been designed to measure the educational environment in specific postgraduate medical settings, for example the Postgraduate Hospital Educational Environment Measure (PHEEM), Surgical Theatre Educational Environment Measure (STEEM) and Anaesthetic Theatre Educational Environment Measure (ATEEM)13. A specific tool to measure the educational environment of rural LICs is not available.
For the present study, the DREEM was selected because it is a highly generic and internationally validated study tool used to assess student perception in all educational systems14-16. It has been translated into various languages and used in different countries. Questionnaires can be modified to be compatible with many learning climates. It is used to diagnose deficiencies in the current educational environment, to compare different group experiences, and to compare actual experiences in the same group. However, few reports using DREEM for LIC programs are available17. It is interesting to extend the use of this tool to a rural LIC, with a setting different from conventional medical schools.
This is the first report in Thailand to evaluate students’ perceptions and factors associated with favorable educational environments in rural LICs. The objective of this study was to assess the educational environment of rural LIC using DREEM questionnaire and to compare students' response assessed by this on the basis of the year of study and the different size of hospitals.
Methods
Study design
This cross-sectional study was conducted in 2020. The study population comprised 75 fourth- and fifth-year students at Hatyai medical center. Eight rural hospitals participated, consisted of two large hospitals (90–120 beds), three medium hospitals (60–90 beds), and three small hospitals (30–60 beds). The hospitals are located 50–120 km from the medical center. The ratio of medical staff to students was 1–2:1.
Characteristics of principal preceptor in rural hospitals
Most large hospitals have staff responsible for attending physicians and principal preceptors in ward settings. When staff are busy, co-preceptors such as interns and ward nurses supervise instead. In the present study, most small hospitals had interns responsible for attending physicians in patient wards and acted as principal preceptors for students instead of staff. Sometimes students could learn from nurses in the wards, the emergency department, and during self-learning. In the outpatient setting in all hospitals, students were under staff supervision.
Modified LIC program
The modified LIC was implemented as part of integrated multidisciplinary rural clerkships for fourth-year students, and for fifth-year students undertaking clinical placements. It took place over 12 weeks for fourth-year students and over 14 weeks for fifth-year students. Practical exposure to several clinical areas included internal medicine, psychiatry, surgery, pediatrics, obstetrics and gynecology, emergency medicine, and family medicine in outpatient and inpatient settings. The structure gave students the opportunity to follow specific patients throughout their entire treatment. Each student became a member of an interdisciplinary team providing comprehensive care to patients under staff supervision and near-peer teaching by interns. Learning timetables and teaching on the run were suitably arranged by rural sites. Regarding weekly schedule, students had an inpatient ward round with staff or interns in the morning and then attended other activities at outpatient clinics, the maternity department and emergency department according to timetables. Home visits for continuing palliative care were performed mid-week. Supplementary online lectures and teleconsultation were provided once a week.
Regarding formative assessments, online quizzes and mock objective structured clinical examination (OSCE) were performed at the mid-way point. Workplace-based assessments including mini-clinical evaluation exercises, direct observation of procedural skills, and case-based discussions were performed at intervals. Skills at writing patient reports were assessed online. The fourth-year students conducted small-group research on community health at various rural sites. Eight research projects were presented when they returned to Hatyai medical center at the end of the rural rotation. Summative assessments using written tests and OSCE were conducted at the end of the 12 or 14 weeks. All hospitals were monitored monthly by site visits. Aligning the program with assessment allows for the same objectives and tools to be assessed, regardless of the geographical location or format of the clerkship.
Tools to assess educational environment
The DREEM questionnaire, consisting of 50 closed questions, was used. Due to concern about content validity, learning experience in a rural LIC was defined as the climate of clinical clerkship in patient wards, outpatient clinics, maternity department, and emergency department. Because there was no traditional lecture classroom in rural hospitals, some words such as ‘classroom’ and ‘lecture’ (questions 1, 23 and 33) were changed to ‘teleconference and teleconsultation sessions’. These items of DREEM fall into one of the following five subscales: students’ perceptions of learning (12 items), students’ perceptions of teachers (11 items), students’ academic self-perceptions (8 items), students’ perceptions of atmosphere (12 items), and students’ social self-perceptions (7 items). Each of the 50 statements was scored on a five-point scale, with the following labels: ‘strongly agree’ (4), ‘agree’ (3), ‘unsure’ (2), ‘disagree’ (1) and ‘strongly disagree’ (0). Reverse coding was required for negative items 4, 8, 9, 17, 25, 35, 39, 48 and 50 before analysis. Higher scores indicate a more positive evaluation. The maximum score is 200, representing an ideal educational environment. Interpretation is considered at three levels: individual items, subscales and overall DREEM. Regarding individual items, those with a mean score of 3.5 or more were regarded as especially strong areas, items with a mean score of 2.0 or less need particular attention, and items with mean scores between 2 and 3 need to be improved promptly16. Overall DREEM scores of 0–50 were regarded as very poor, 51–100 indicate many of problems, 101–150 were regarded as more positive than negative, and 151–200 were regarded as excellent.
Data collection and analysis
Independent variables included student year, gender, hospital size (number of hospital beds), type of principal preceptor (staff, intern, nurse, self-learning). Primary outcome was overall DREEM score. Univariable analysis was performed using χ2 test, t-test or Mann–Whitney U-test depending on type and distribution of data. Multivariable regression analysis was performed to determine factors associated with overall DREEM score.
Ethics approval
This protocol was approved by the independent ethics committee of Hatyai Hospital (protocol number HYH-EC 071-64-01).
Results
Educational environment evaluation by DREEM questionnaire
The response rate to the DREEM questionnaire was 96%. Mean overall DREEM was 137.7/200 (range 84–182). Students’ mean score for perceptions of learning was 30.1/48 (range 15–41). Students’ score for perceptions of teachers was 35.7/44 (range 25–44). Students’ academic self-perceptions scored 18.7/32 (range 8–32). Students’ perceptions of atmosphere scored 30.4/48 (range 20–48). Students’ social self-perceptions scored 18.3/28 (range 9–28).
Four items regarded as perception of teacher were rated more than 3.5. Fifteen items regarded as interpersonal relationship were rated 3–3.5. Twenty-eight items regarded as atmosphere and academic environment were rated 2.1–2.9. The remaining three items, regarded as teacher centered teaching, were rated 2.0 or less. The academic subscale regarding confidence in knowledge gain scored the lowest in all hospitals. Median scores of overall DREEM and subscales were higher in large hospitals than in small hospitals (Fig1).
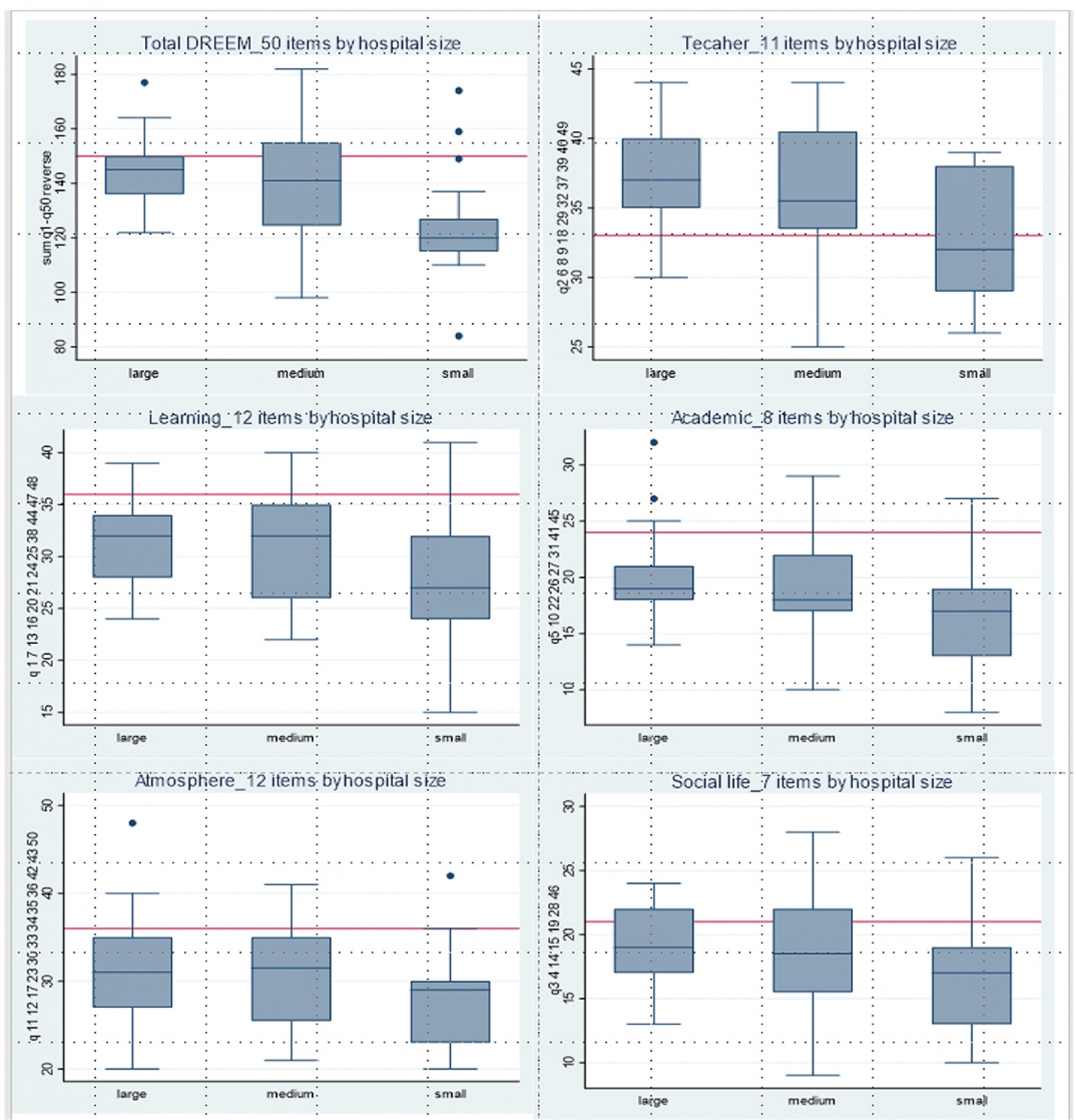 Figure 1: Comparisons of overall DREEM scores and subscales by hospital size.
Figure 1: Comparisons of overall DREEM scores and subscales by hospital size.
Analysis of factors associated with overall DREEM scores
By univariate analysis, fourth-year students rated scores higher than fifth-year students in the same rural hospitals. Differences of scores were found for hospital size and type of principal preceptors (Table 1). By multiple regression analysis, staff as principal preceptors and large hospitals were associated with favorable overall DREEM scores (Table 2). For subgroup analysis of five subscales, both factors were associated with four subscales except academic environment.
Table 1: Univariable analysis of factors associated with overall DREEM scores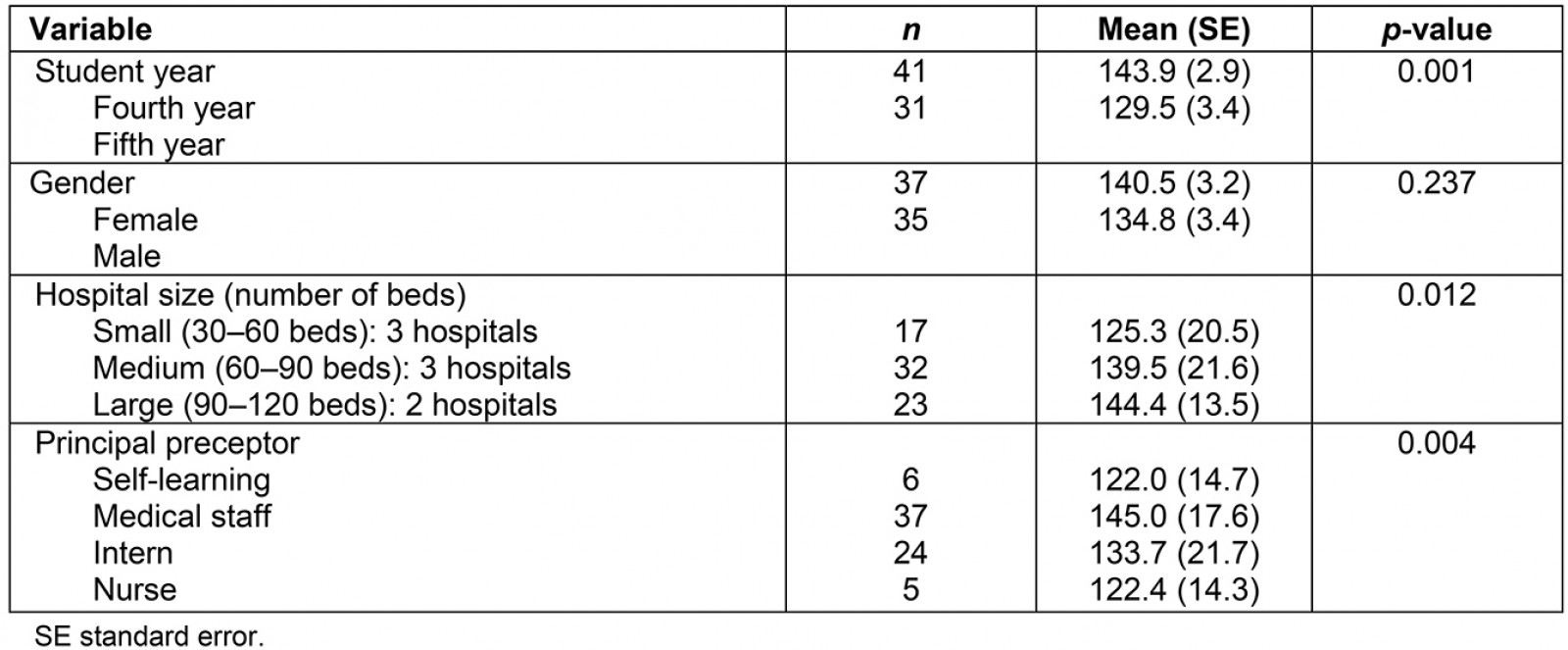
Table 2: Multivariable analysis of factors associated with overall DREEM† scores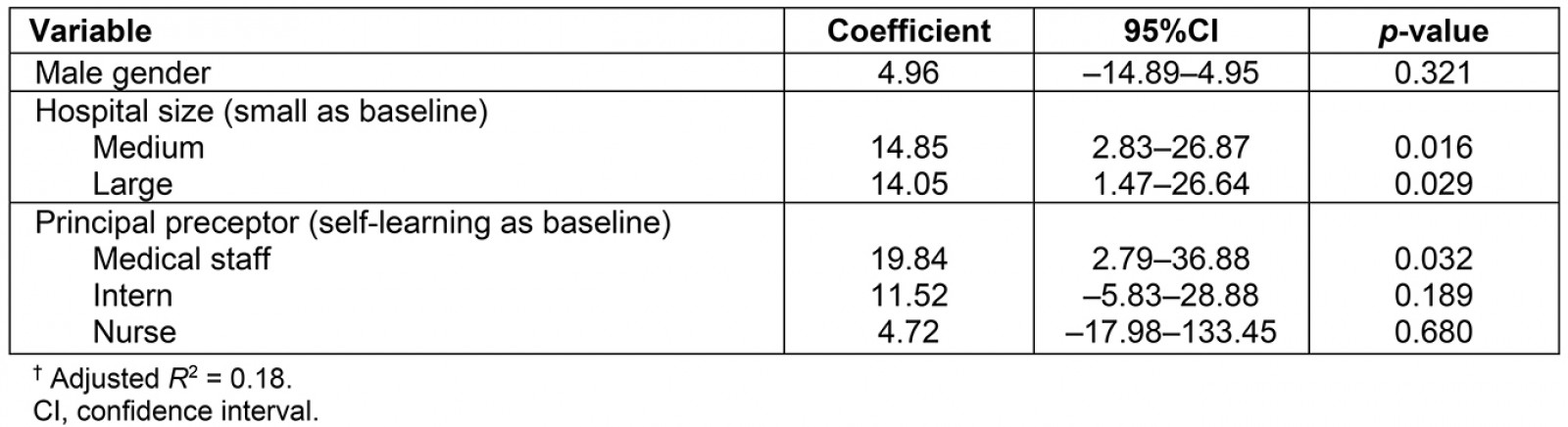
Discussion
The evaluation in this study was for educational environment. Assessment of learning outcomes has not yet been done. It showed a mix of positive and negative scores for educational environment. The lowest score in all hospitals was the academic subscale related to confidence in knowledge gain. Students felt isolated and needed more contact time with supervisors. On the other hand, some local staff felt overburdened with additional responsibility and needed more time to adapt to new roles. Additional effort is required for preceptors to updating practice guidelines, upskilling teachers for teaching on the run and clinical reasoning18,19. Resistance among existing faculty in medical centers and rural staff can be another barrier to running this program in the beginning. Some subspecialty faculty may not believe that students will be able to meet their clerkship objectives. The key persons within the faculty are important to organize the LIC interfaces with the rest of the program, and align with the dynamics of the model. Mutual benefits for academic medical centers and community health systems need to be clarified for all stakeholders.
The duration of this rural clerkship is 40% of total curriculum, which seemed too long to students. They were anxious about fear of missing out in knowledge gain due to less diversity of patients. They were not confident to pass summative assessments and the national license examination. How long a rural clerkship needs to be to constitute sufficient time for continuity of care is still a matter of debate. The range is 6–54 weeks for different models20,21. The longer duration seems better to extend time in a clinical setting through a continuity care and cultural learning22. Thus, this area needs more study.
The present study suggests predictors of positive educational environment such as type of principal preceptor and size of host hospital. Large hospitals can arrange learning environments better than small hospitals. This relates to the number of staff and infrastructure of hospital. However, these findings are discordant with a previous report from Western Australia, which found that student performance and perceptions of experience at smaller sites were more satisfactory than those at the larger sites17. Small sites with close-knit rural communities promote students’ sense of belonging in a longitudinal clerkship more than urban sites23.
The principal preceptor should be medical staff in outpatient and inpatient settings, and they should take active roles as mentors and coaches. Mentors are responsible for providing support and feedback by listening and advising. Coaches partner with students to enhance professional potential by asking, teaching and correcting. Near-peer teaching is an additional support to mitigate staff burden. The limited breadth of patients’ clinical presentations in a particular rural hospital can be met, if preceptors ensure that, each time a similar case is encountered, students should approach it at progressively higher levels of complexity.
A lesson learned from this study is to trust the process. Barriers may slow it down, but are not reasons to stop. Clarified learning objectives and a structured academic approach to the complexities of curriculum to staff and students are essential. Rural staff are the key success factor to support students, concordant with the recommendation of 12 tips for designing the program and a practical guide for successful implementation2,24. Staff development should be more focused to increase teaching skills, enthusiasm and engagement.
Conclusion
LIC implementation in a community health system can be a model for expanding clinical clerkships. A good infrastructure of the host hospital and enthusiastic preceptor are key success factors. Staff supervision is essential to encourage students’ learning, especially in the academic environment. Large hospitals have better infrastructure to support learning processes than small hospitals.
Acknowledgements
The authors thank consultants Aruparp Lekhakula and Kanyika Chamniprasas, Faculty of Medicine, Prince of Songklanakarind University, Thailand.