Burden of injury is a growing problem
For the last 20 years injury prevention policy in Australia has been hampered by poor consultation practices, limited stakeholder involvement, inadequate allocation of resources, poor implementation, and an absence of performance measures1. (p. 1)
Globally, injury remains a leading cause of death, hospitalisation and disability among people aged 1–44 years, and accounts for 1 in 10 deaths2. In Australia, injury was recognised as a national health priority in 1986; however, implementation efforts to reduce its incidence and impact have been slow3. In 2018, injury was the direct cause of more than 530 000 hospitalisations and 12 000 deaths, and is steadily increasing at ~1% per year3,4. Hospitalised injuries range from single fractures, falls, sprains and open wounds to polytraumas (two or more severe injuries in at least two areas of the body). Injury rates and hospitalisations are higher for males and people residing in rural or remote areas, especially in young people4. In Australia, around one in six (15%) hospitalised traumatic injury cases are classified as ‘high threat to life’4.
In 2018, the leading causes of injury in Australia were unintentional falls (37% of all deaths), transport accidents (11%), intentional self-harm and suicide (23%) and poisoning (11%)4. Self-harm and suicide rates are two times higher in Aboriginal and Torres Strait Islander peoples and in rural populations4. Economic burden is another consideration. In Australia, spending on hospitalised injury in 2015–16 was $8.9 billion, the third most expensive after musculoskeletal disorders ($12.5 billion) and cardiovascular diseases ($10.4 billion)5,6. Combined, the Northern Territory, Queensland and Western Australia provide service to 70% of Australia’s total land mass7, and therefore it is not surprising they have the highest healthcare costs per person, followed by South Australia, Victoria, New South Wales (NSW), Australian Capital Territory and Tasmania (Table 1).
Table 1: Australian injury expenditure by state and cost per person (2015–16) 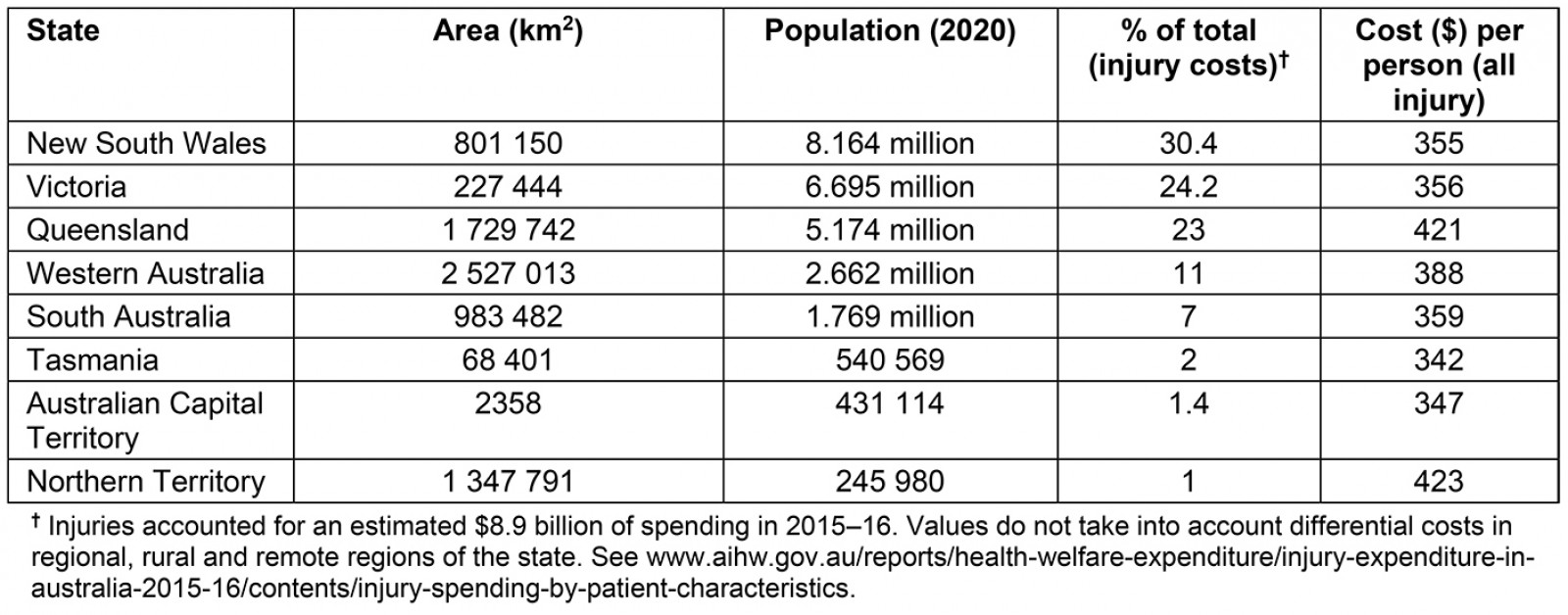
Where you live matters
Almost one-third of Australia’s population, or seven million people, reside in rural and remote regions. The term rural refers to the remoteness areas of the Australian Statistical Geographical Standard of outer regional, remote and very remote locations8,9. The further a person lives from a major metropolitan centre, the greater their risk of serious injury, the higher probability of worse outcomes and death, and the higher likelihood for self-harm and suicide, combined with poorer access to health services10. People residing in rural or remote areas have up to 2.5-fold higher hospitalisation rates and up to fivefold higher mortality rates compared to their urban counterparts. Increased focus on these disparities is particularly urgent for Indigenous Australians, who have on average a life expectancy 10 years less than non-Indigenous Australians11, and 15 years less if they live in remote or very remote areas12. Similarly, children living in rural areas have higher injury-related mortality rates and significantly more hospital admissions compared to children who live in metropolitan areas13. Addressing this inequality has been an ongoing challenge for federal and state governments and healthcare providers for decades. While some progress has been made, more needs to be done to improve health care beyond major metropolitan cities.
Brief history of aeromedical retrieval: servicing life in the outback
The most eloquent cry for a Flying Doctor is a silent one: The whole of the outback is a pageant of graves and their stories of men, women and children who departed this life without the hope of loving-kindness in medical care ... too often mother and baby lie together14. (p. 23)
Disparity of healthcare services in inland Australia was recognised nearly a century ago by Reverend John Flynn (Fig1). During his travels, Flynn wrote about the daily struggles of living in remote areas, and observed that the seriously injured had to travel hundreds of kilometres by horse, cart, camel and, later, trucks to reach a doctor, and most of them died on the way15. These observations had a long-lasting effect on Flynn, which led to his vision for a ‘mantle of safety’ comprising the building of mission hostels/hospitals in the outback, and an aeromedical service, which began as an experiment in 1928. A year before the experiment, Flynn travelled to Longreach, Queensland, where he met aviator Hudson Fysh, a founder of Qantas, and together with ex-CEO Dr Fred Michod (who coined the term flying doctor), the Royal Flying Doctor Service was born on 2 August 1927. Originally, it was called the Aerial Medical Service, and in 1942 changed to the Flying Doctor Service, and then to the Royal Flying Doctor Service (RFDS) in 1955 after Queen Elizabeth II’s visit. In its first year (1928), Flynn’s experiment included 50 flights to 26 destinations, treating 225 patients. Today, the RFDS, on average, transports 31 patients a day in Queensland alone, and has more than 320 000 total patient contacts through clinics, aeromedical transports and telehealth consultations across Australia every year16. The RFDS is the world’s largest aeromedical organisation, with a national fleet of nearly 80 aircraft, 180 healthcare road vehicles and 23 operational air bases scattered throughout Australia. Since its inception, RFDS in Queensland has been integrated into a federal- and state government-funded aeromedical network. This service, which is coordinated and governed by Retrieval Services Queensland (a unit of the Aeromedical Retrieval and Disaster Management Branch of the Queensland Department of Health), includes 10 fixed wing (RFDS), 11 rotary wing and 3 jet aircraft. Since 2015, there has been an increase in aeromedical retrievals in Queensland, with more than 21 000 people requiring transport per year, about 57 people per day9.
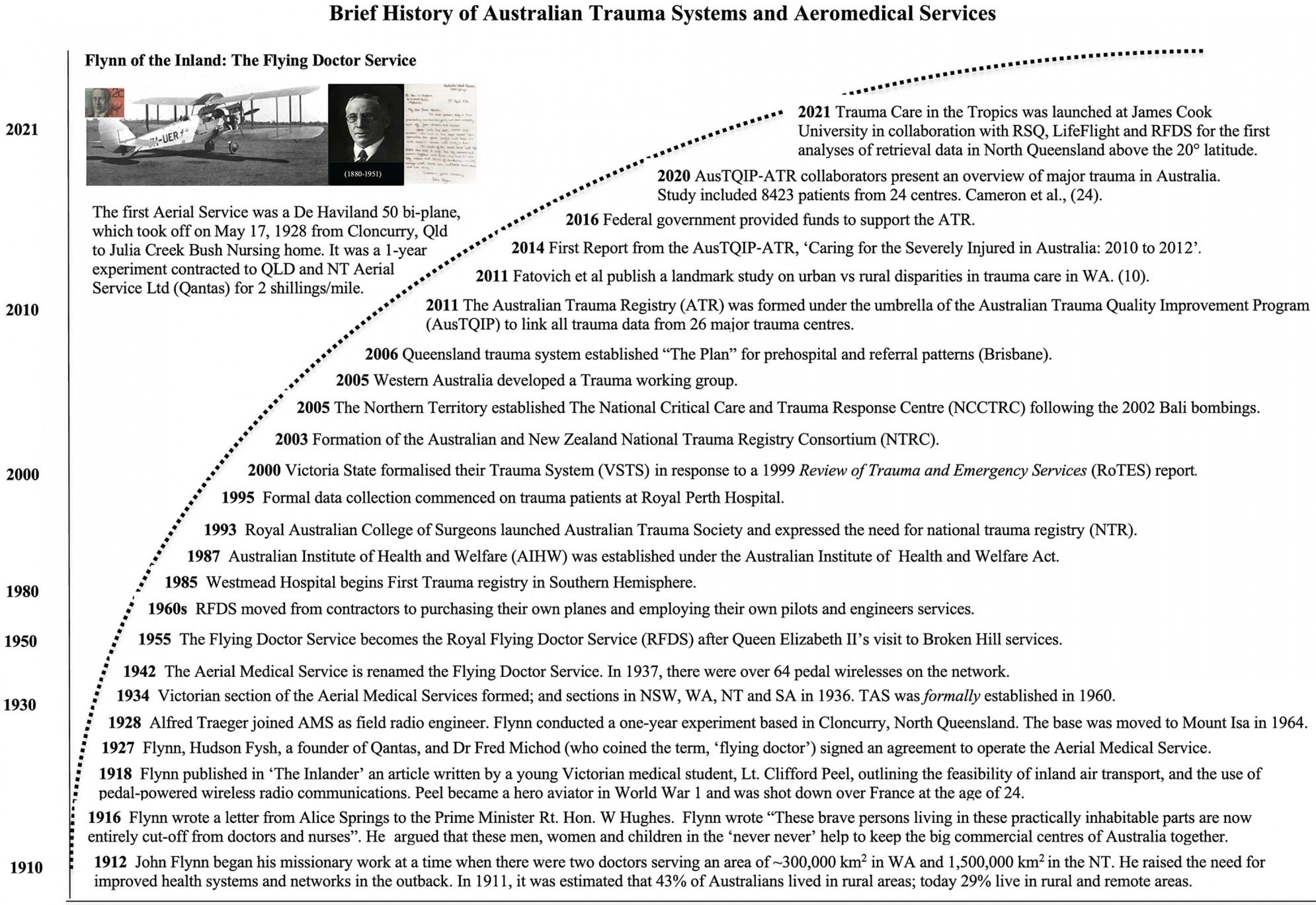 Figure 1: A brief history of Flynn’s vision for a ‘mantle of safety’ throughout inland Australia, the early formation of the Royal Flying Doctor Service, and the formation and ongoing challenges facing the Australian trauma registry founded in 2011.
Figure 1: A brief history of Flynn’s vision for a ‘mantle of safety’ throughout inland Australia, the early formation of the Royal Flying Doctor Service, and the formation and ongoing challenges facing the Australian trauma registry founded in 2011.
The Golden Hour: an aspirational goal in the chain of survival
The stark reality of our outback history (is that) … Sickness relating to lack of clean water, poor living conditions, the climate, trauma, infections, infectious diseases and the isolation were commonplace. There was a desperate need for emergency as well as everyday health care15 (p. 52).
The Golden Hour is a concept proposed in 1960s by R. Adams Cowley, founder of the now-famous Shock Trauma Institute in Baltimore, USA. Cowley originally introduced the term as a medical retrieval goal and marketing tool for funding of his new trauma facility17. Today, the Golden Hour is more of an ‘aspirational’ goal or management objective where ‘prompt medical treatment improves survival after severe trauma or acute sickness’18. In stark contrast to urban retrieval times, which may range from 15 to 90 minutes, rural and remote retrieval times may be up to 12 hours or longer10. A recent study of RFDS retrievals of stroke patients from rural and remote Australia found a median transfer time of 4 hours from first call to patient delivery at a hospital airstrip, which is commendable but well beyond the therapeutic window for standard thrombolysis therapy19. Thus, the Golden Hour is rarely met in rural environments10,18,20, and some studies have estimated a 19% increase in risk of death per hour for severe trauma patients21. Increased rurality shifts the needle of care from a ‘scoop and run’ approach in an urban setting to a ‘continuum of care’ plan. Thus, the scale of remoteness requires a different kind of service delivery, with many moving parts, which is normally planned and implemented by an emergency medical specialist from a centralised base.
The moving parts of a retrieval flight plan include:
- clear communications between the central administrator to a first responder or victim (if conscious) at or close to the point-of-injury
- clear understanding of the type and severity of injury
- when and where the injury occurred
- onsite treatment options and pain relief
- assessment of remoteness and quickest path to medical assistance, possible therapies and telehealth options
- need for triage, if more than one patient
- logistical plan for the most efficient retrieval service/transfers
- initiation of the plan
- implementation of en-route treatment protocols, continuous monitoring of vital signs, stabilisation, resuscitation, use of fluids or blood products, analgesics, hospital preparedness
- transfer to the designated hospital or transfer to another hospital
- hospital admission and definitive care.
Optimal patient outcomes critically depend on skilled personnel and resources, and accurate records at every stage of plan implementation.
Development of trauma systems in Australia: not all are created equal
The vision for a national trauma registry in Australia has been championed by committed individuals and organizations since 199322. (p. 288)
A brief history of the development of trauma systems in Australia is shown in Figure 1. Advances in trauma care have largely been driven by state and territory efforts to improve patient outcomes, foster collaborations, research, formation of trauma-based societies and injury prevention programs22,23. These efforts eventually led to the development of the Australian Trauma Registry in 2011, which was a national program to advance the quality and safety of trauma care. Today, the registry receives data input from more than 30 major trauma centres in Australia and New Zealand3,22,24. The binational dataset includes but is not limited to details of the injury event, prehospital observations, injuries sustained, treatments received, in-hospital observations and discharge status. A critical issue currently facing trauma registries in Australia is the lack of consistency and quality of data sent from the various hospitals. Robust patient record-keeping and storage from point-of-injury to hospital discharge (or mortality) ensures implementation of current guidelines and practices, helps to identify gaps in knowledge, allows ways to improve decision-making procedures and treatments, serves as a basis for evidence-based research and education and assists stakeholders to streamline costs. High-quality data, linkage and analysis can only be achieved with strong state/federal support and adequate funding.
A point of emphasis is that not all trauma systems are created equal. Mixing data from metropolitan cities with that of regional and rural hospitals and health centres will continue to mask ongoing issues relating to remoteness. In a recent study by the Australian Trauma Quality Improvement Program of 8423 trauma patients, 66% were found to have been transported from the point of injury to definitive care in a median time of 1.42 hours24. Most trauma was transport- or falls-related (81%) with approximately 11% in-hospital mortality, and 14% of these were in the emergency department24. However, these data from 26 hospitals did not address retrieval delays or the effect of remoteness. Admittedly, the study’s inclusion data were limited to sustained major trauma (injury severity score >12) or to those who subsequently died in major trauma centres, and excluded patients with hospital admissions delayed longer than 7 days24. Future subgroup analysis from the same database, and others, at the Australian Trauma Registry may shed more light on the problem of rurality and remoteness to properly inform healthcare stakeholders and government of ongoing inequalities. Addressing these matters is strategically important for the health of a nation because investing in regional and rural communities ties the metropolitan cities together culturally and commercially (agriculture, renewable energy and resources). Capacity building from a health perspective includes recruitment and retention of medical professionals (general practitioners, nurses, specialists, allied health professionals and others) in rural hospitals and healthcare centres and supplying them with appropriate training and the basic medical equipment and consumables required to service the people.
Way forward for rural and remote communities
Ensuring the system of care is targeted, efficient, accessible, safe and responsive to clinical demands requires accurate data24. (p. 115)
It is remarkable that nearly a century after Flynn conducted his first ‘flying doctor’ experiment from Cloncurry (Fig1), little or no accurate trauma data analysis is available from the ‘mantle of safety’ region of North Queensland where the first De Havillands flew (Fig2). This deficit of injury data analysis needs to be urgently addressed in this region, and for other rural and remote emergencies requiring retrieval in North Queensland. This is the primary focus of our current project, Trauma Care in the Tropics (Fig1), which will also include an examination of the dynamics of a retrieval flight plan as a function of increased remoteness (discussed earlier).
In addition, much can be learned by rural and remote health systems from advances in military systems. The US military tactical combat casualty care guidelines, which were first published in 199625, are regularly updated with evidence-based interventions, procedures and therapies that may be applicable for pre-hospital trauma, haemorrhage and en-route stabilisation. Far-forward military environments share many similarities with resource-limited rural environments and require therapies that are effective, small-volume, inexpensive, have long shelf lives and wide temperature stabilities, and can resuscitate and stabilise trauma patients for up to 7 days when evacuation is delayed26. In these environments, the military assemble portable field hospitals are located as close to points of engagement as possible. While deployable field hospitals are impractical for single-trauma events in rural and remote communities, their rural equivalent could be the small health centres with telehealth capabilities that are scattered throughout Australia. Nurses, Aboriginal health professionals and doctors at these centres could be trained and resourced for polytrauma diagnoses, resuscitation and major trauma stabilisation similar to a special forces medic while waiting for retrieval services.
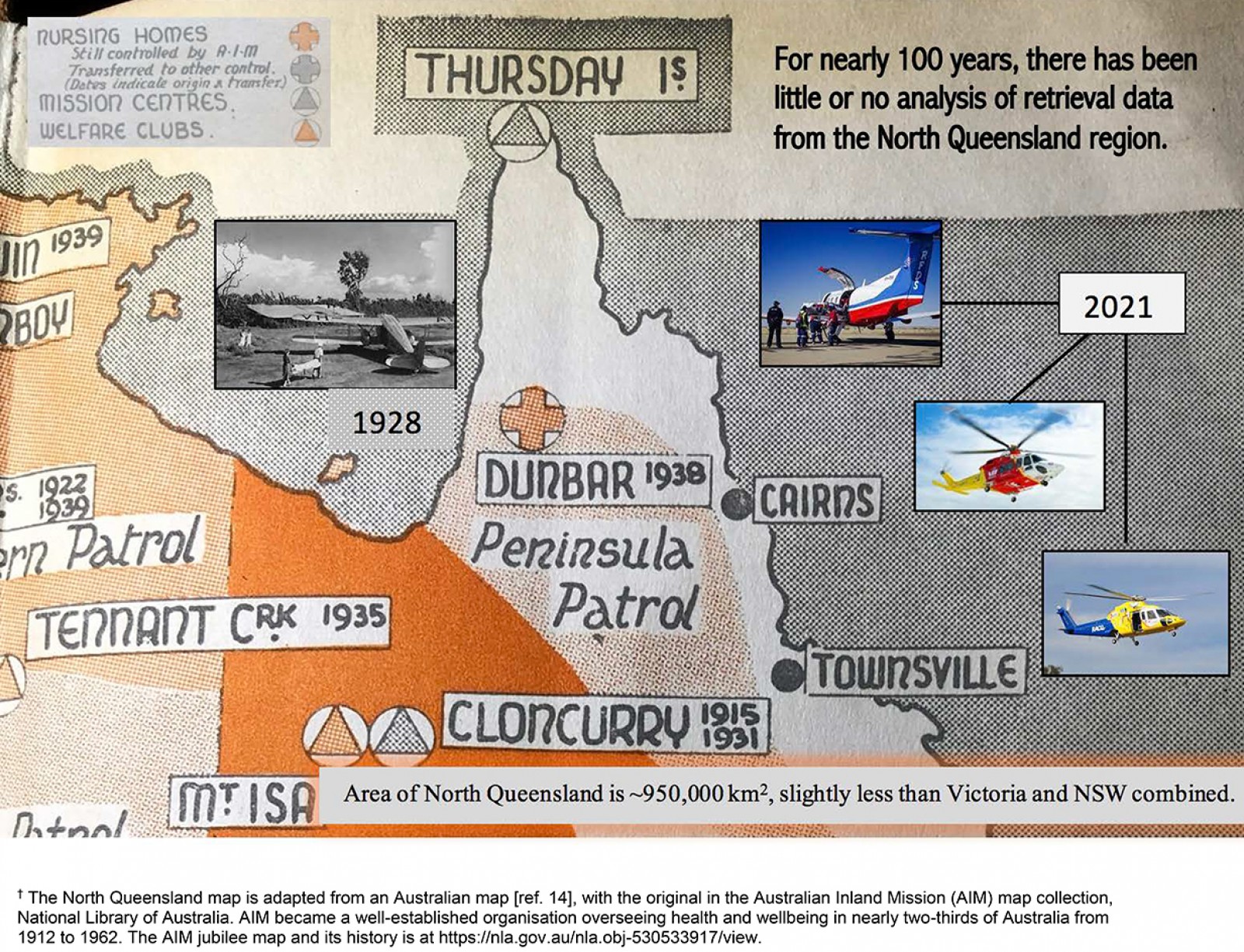 Figure 2: North Queensland Patrol of the Australian Inland Mission and Flying Doctors map† in the 1940s with pictorial insets of present-day aeromedical services in North Queensland.
Figure 2: North Queensland Patrol of the Australian Inland Mission and Flying Doctors map† in the 1940s with pictorial insets of present-day aeromedical services in North Queensland.
Conclusion
Providing effective emergency care to rural and remote patients remains challenging. The long distances, changing geography and topography, limited resources and high retrieval costs continue to be obstacles. Improving healthcare service delivery in general, and trauma care in particular, is an essential investment for urban and rural regions for the benefit of all Australians. Key to progress in rural and remote communities is accurate data from point of injury to definitive care that specifically identifies issues of rurality, the need for advanced training in rural and remote trauma management, and learning from other systems, for example the military, that share many of our challenges. Such initiatives have the potential to save lives and reduce costs in the healthcare system.
Acknowledgements
We thank Queensland Emergency Medicine Foundation; Retrieval Services Queensland; Lifeflight Retrieval Medicine; Royal Flying Doctor Service; Queensland Health Aeromedical Retrieval and Disaster Management Branch Research Committee; and Townsville, Cairns and Hinterland, Mackay, North West, and Torres and Cape Hospital and Health Services for supporting this Trauma Care in the Tropics initiative. We thank College of Medicine and Dentistry, James Cook University, for their continued support.
Funding for the study is from the Emergency Medicine Foundation under Award No. EMLE-149R33-2020-GIBBS. Townsville Hospital and Health Service Study, Education and Research Trust Account Fund under Award No. ION 90001135. GPD and HLL are also supported by USSOCOM under Award No. W81XWH-USSOCOM-BAA-15-1. The opinions, interpretations and conclusions are those of the authors and are not necessarily endorsed by the US Department of Defense.