Introduction
The recent SARS-CoV-2 (COVID-19) pandemic brought to the fore the need for healthcare system preparedness plans and their strengthening1. Primary health care (PHC), as a first point of contact, has a fundamental role in recognizing emerging and re-emerging infections, early diagnosis and timely outpatient management. Factors determining the preparedness level of healthcare professionals during epidemics are the presence of guidelines and emergency plans, the training of professionals in the implementation of guidelines and measures, the difficulty of healthcare professionals in communicating effectively with patients and the problems caused by inadequate facilities2. Living in rural areas has been recognized, globally, as a significant factor contributing to disparities in health and access to properly organized healthcare facilities3; consequently it has been suggested that this should be considered as a health determinant and not only as a geographical variable to evaluate in the planning of health care in a given area4,5. Health emergencies, such as the COVID-19 pandemic, can accentuate the gap in health care between those living in urban and rural centres6,7. Additionally rural residents’ opposition to the adoption of preventive measures against the pandemic can further increase the disparities between rural and urban populations8,9.
Pandemics put a burden on primary healthcare workers (PHCWs) at the frontline due to the disruption in their work routine. The implementation of new protocols, lack of personal protective equipment (PPE), fear of getting infected or infecting their relatives and commitment to the duty of treating patients overburden PHCWs, especially in remote areas where a small number of understaffed facilities serve large proportions of the population10. Additional problems such as difficulty in utilizing new technologies at work, ambivalent feelings, fear of dying versus commitment, fatigue, helplessness and anger usually emerge in such situations11.
Although in some countries, PHC systems have responded well to the pandemic and contained viral spread through infection control strategies designed for primary care12, other countries’ PHC systems reported problems such as understaffing, lack of training in infection control, limited technological support 13, insufficient coordination between primary care and secondary or tertiary healthcare facilities14 and lack of emergency response protocols tailored to the needs of remote and rural PHC facilities10,15.
During the first months of the pandemic, Greek PHC was not involved to the same degree in the COVID-19 strategic planning, and health authorities focused on the reinforcement of hospital preparedness, considering it an absolute and immediate priority16. The present study explores the awareness of primary health care professionals employed in rural and urban PHC facilities in Greece regarding the management plan of the COVID-19 pandemic during its initial phase. It evaluates possible associations of health professionals’ attributes and attitudes and their impact on the overall management of the pandemic in the PHC setting, especially in preparation for the next phases.
Study setting
In Greece, PHC is primarily provided within the National Health System (NHS), which is responsible for addressing medical emergencies, both in health centers and hospitals. There are 204 health centers, mainly in semi-rural and urban settings, and 127 local health units (urban primary care local health units, founded in 2017) in urban areas staffed by 7182 employees. Services are mainly provided by general practitioners, internists, pediatricians, dentists, nurses and administrative staff. Other healthcare professionals are also present (eg physiotherapists, dieticians, social workers, laboratory technicians)17. Each health center in rural and semi-urban settings usually has a catchment of 30 000–60 000 inhabitants. In the urban primary care facilities, catchment areas are not always well defined17.
Study design
This study was a cross-sectional survey aiming to evaluate and discuss the perceptions, concerns of PHCWs in the public sector regarding the COVID-19 pandemic, and their awareness and knowledge level of the preparedness plan. Data collection took place in Greece during 11–22 March 2020.
Sampling and inclusion criteria
Due to the urgency of the research objective, a non-probability purposive sampling was used. Sampling was conducted using a pre-existing panel of the Education and Research Network in PHC of the Aristotle University of Thessaloniki18 as a sampling frame. The panel’s primary aim is to promote research and improve the quality of care in PHC and general practice through the voluntary collaboration of primary healthcare facilities and PHCWs with the Aristotle University of Thessaloniki. Members of this panel assisted in the questionnaire distribution in their facilities. The eligible study population comprised all PHCWs regardless of their professional role. Out of the 650 prospective participants, 444 healthcare workers completed the questionnaire online with a 68.3% response rate. The study sample constituted 6.2% of the PHC professionals in the public sector. A proportional quota sampling with a minimum of 5% participation in every administrative area, according to NUTS I categorization19, was achieved in three out of four areas (Northern Greece (11.6%), Central Greece (6.7%), Aegean and Crete (5.2%), and Attica (4.8%)).
Research questionnaire
A web-based 14-item questionnaire consisting of 45 subquestions was devised to collect data about:
- gender, age, profession, work related experiences and other demographic information, especially regarding health and living conditions associated with vulnerability to COVID-19
- awareness of the pandemic preparedness plan in Greece
- work-related concerns and attitudes
- personal concerns and attitudes.
The initial questionnaire was reviewed and adjusted for content validity by a working group of four senior researchers and practicing physicians. Then the questionnaire was piloted to 22 eligible healthcare workers of various professions in a semi-urban health center, and amendments were made accordingly, incorporating insights and verbal comments into the final research tool.
Data collection
Invitations were sent via email through the panel along with two reminder emails, on sampling days 4 and 8 after the first communication. The questionnaires were completed online at a single completion attempt and a personal code was generated for possible future use. Written consent was included in the online submission of the questionnaire for all participants.
At the beginning of data collection, WHO declared the global COVID-19 epidemic as a pandemic20 and data collection took place during the early containment phase of the pandemic response in Greece. During this period, Greece had been under the first group of community and social distancing measures consisting of school closures and public social event cancellations. The country-wide lockdown came into effect after the last data collection date21.
Data analysis
Data collected were processed using the Statistical Package for Social Sciences v25 (IBM; http://www.spss.com). Specific questionnaire items were grouped, and a Cronbach’s alpha statistic was calculated to assess internal consistency. Items regarding PHCW awareness are presented in Table 1 and items regarding PHCW risk perception are presented in Table 2.
Qualitative variables were summarized with frequencies, and percentage and quantitative variables with means and standard deviations (SD). Associations were explored between epidemic response awareness, risk perception and PHCW demographics or practice characteristics. These variables were recorded in a four-level Likert scale to state each participant’s level of agreement and for analysis purposes were divided into the computed ‘agree’ variable (sum of ‘agree’ and ‘somewhat agree’) versus the ‘disagree’ variable (sum of ‘disagree’ and ‘somewhat disagree’). Each question used to consider participant awareness and preparedness level was rated with one point whenever a participant agreed and with no points when they disagreed. For each participant an awareness and preparedness score was calculated as the sum of the relevant questions presented in Tables 1 and 2, with higher scores indicating more awareness and preparedness respectively. PHCWs were grouped and analyzed by profession and place of work (at a NUTS III level)19. Participant occupation was considered the main independent variable and was categorized to three levels: a reference group of first-line physicians, including general practitioners (GP), GP residents, internists, pediatricians and doctors in rural service; first-line non-physicians, including nurses, health visitors and paramedics/ambulance crew; and second-line PHCWs, including dentists, microbiologists, administrators, midwives, laboratory technicians, nutritionists and social workers. Univariate logistic regression was used, followed by multivariable analysis, adjusting for age, gender, working experience, occupation, workplace type, location and proximity to a tertiary hospital, and vulnerability to the virus regarding participants or their families. Odds ratios (ORs) with the respective 95% confidence intervals (CIs) were presented. Linear regression was performed to examine the effect of participants’ awareness of the preparedness plan to their working area attributes, adjusting for the same variables as the multivariable logistic regression mentioned above. All p-values were two-tailed at 5% significance level.
Table 1: Primary healthcare worker awareness about the preparedness and response plan of the Ministry of Health and the National Public Health Organization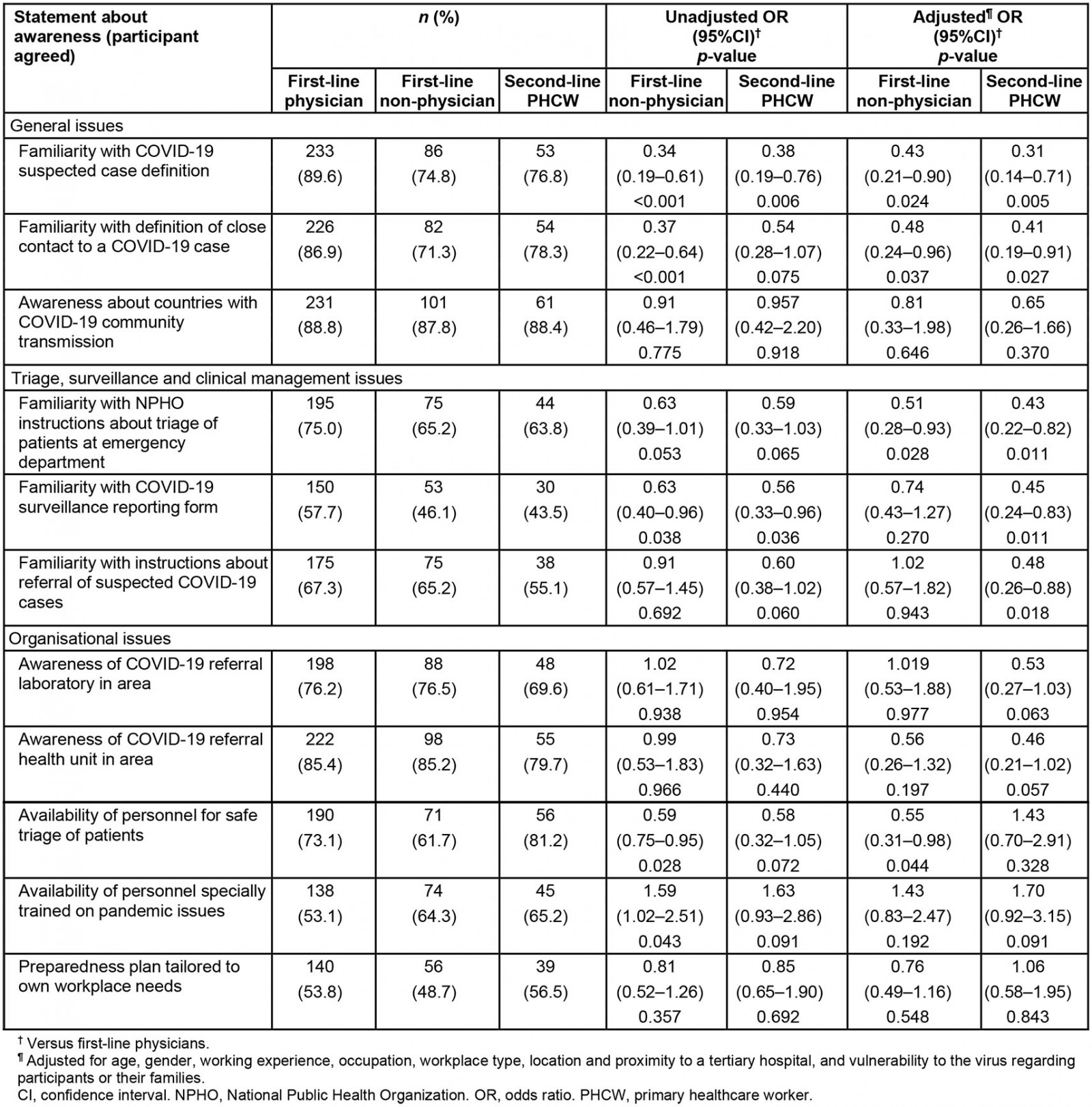
Table 2: Risk perception of primary healthcare workers in Greece during the COVID-19 pandemic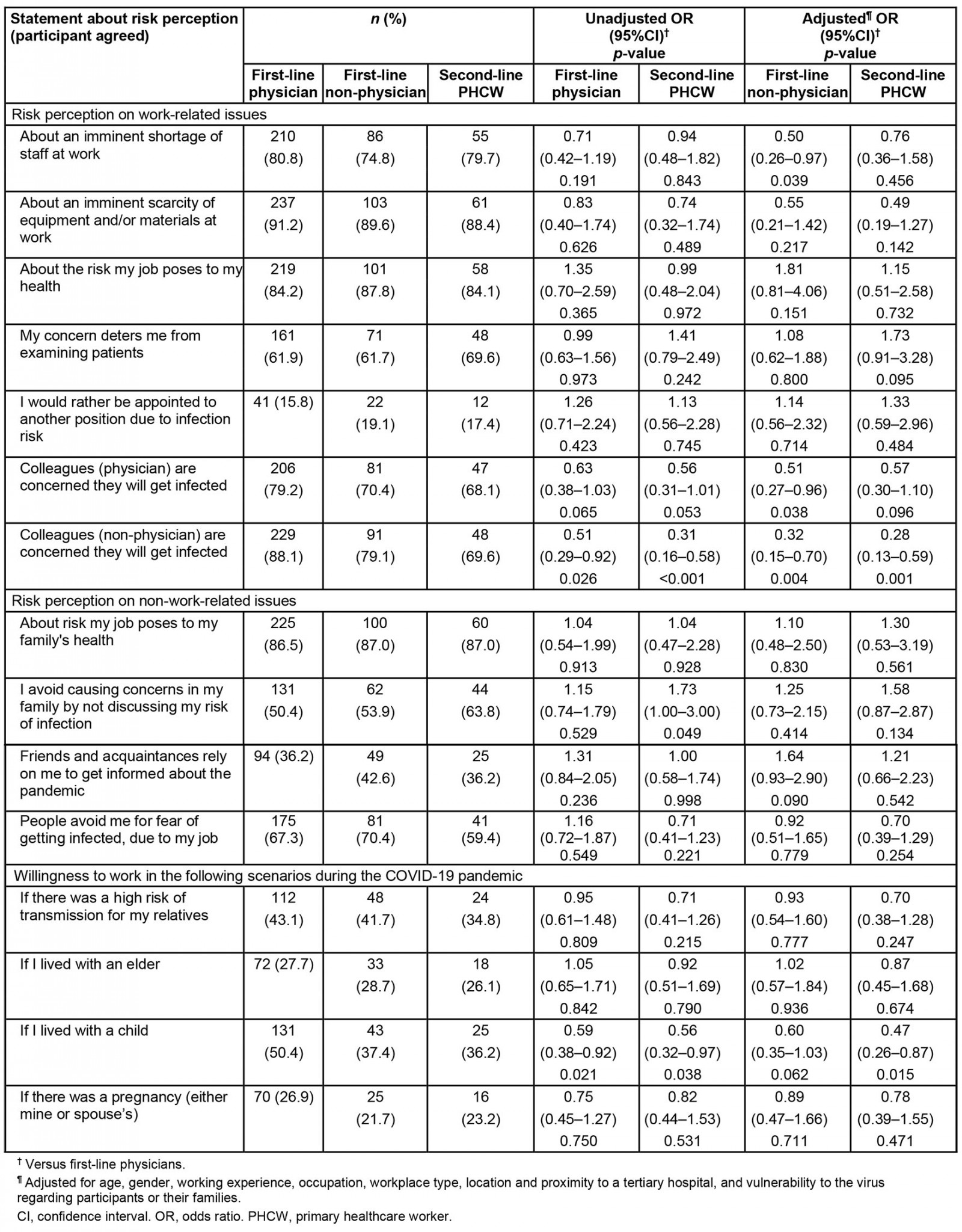
Ethics approval
Ethics approval for this project was obtained by the Bioethics Committee of the Medical School of Aristotle University of Thessaloniki (reference number 173/11-3-2020).
Results
Background of study participants
The majority of the 444 PHCWs who took part in the study were female (67.1%) with a mean age of 44.4 (SD 9.2) years and a mean working experience of 11.9 (SD 9.8) years. Regarding their occupation and workplace, over a third (34.5%) were GPs and 18.9% were nurses. They were mainly working in health centers (72.5%), 25% in semi-urban areas and 32.2% in rural areas. The majority (66%) were parents, living with at least one child (60.4%), and almost half (42.8%) were living with a person at high risk of severe COVID-19 infection. Finally, 55 (12.4%) respondents belonged in a high-risk group at risk of severe COVID-19. Further details are depicted in Table 3.
Table 3: Demographic characteristics of healthcare workers participating in study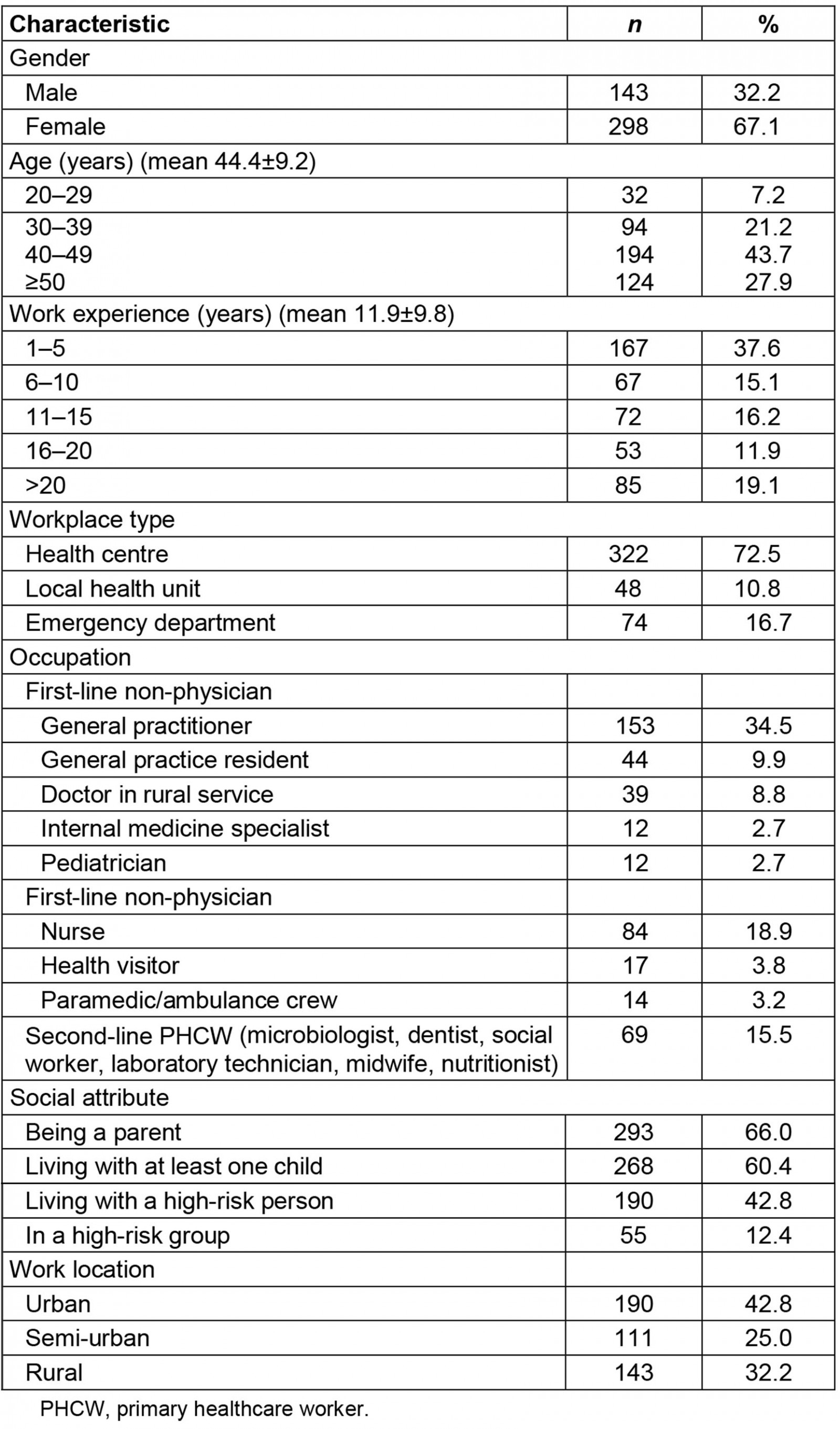
Perceived awareness of the preparedness plan
Items grouped to depict PHCWs awareness yielded a Cronbach’s alpha of 0.80 while items referring to their concerns about the pandemic gave a Cronbach’s alpha of 0.70. Preparedness is the main aspect of the health system’s response to the pandemic, and awareness of PHCWs is of critical importance. The vast majority of PHCWs reported they were familiar with issues generally related to the pandemic response, such as the National Public Health Organization (NPHO) instructions about suspected cases (83.8%), close contact definition (181.5%) or about countries with community transmission (88.5%).
Regarding issues that relate to everyday management and surveillance of patients, over half of the PHCWs felt prepared. Specifically, 52.5% responded that they knew how to report a case for surveillance, 64.9% responded that they knew when to refer a suspected case to the hospital, and 70.7% were familiar with safe triage of patients in the emergency department.
PHCW perspectives on organizational issues were rather ambivalent. While they were aware about the referral laboratory, and secondary and tertiary hospitals in their working area (75.2%, 84.5% and 71.4%, respectively), the majority of them believed they had available personnel for performing triage in their facilities.
Little more than half reported having in their workplace a designated staff member trained in infections and pandemic control (57.9%) or having a preparedness plan tailored to their facilities’ needs (52.9%). Table 1 depicts how the above situations about pandemic preparedness are perceived by study participants according to their line of work. In multivariable analysis, first-line non-physicians and second-line PHWCs were less familiar than first-line physicians with COVID-19 suspected case definition, with the definition of a close contact to a COVID-19 case and with NPHO instructions about the triage of patients at the emergency department (p≤0.037 for all associations). Only second-line PHWCs were less familiar than first-line physicians with the COVID-19 surveillance reporting form (OR 0.45; 95%CI 0.24–0.83) and with the instructions about the referral of suspected COVID-19 cases (OR 0.48; 95%CI 0.26–0.88). However, only first-line non-physicians were less aware than first-line physicians regarding availability of personnel for the safe triage of patients (OR 0.55; 95%CI 0.31–0.98).
In general, older PHCWs were more aware regarding pandemic preparedness (B=0.03, 95%CI 0.01–0.06; p=0.016), than younger PHCWs. The same applied for more experienced PHCWs (B=0.03, 95%CI 0.00–0.05; p=0.049) compared to less experienced ones. Participants working in the local health units did not feel as well prepared as those working in health centers (B=–0.94, 95%CI –1.77– –0.11; p=0.027).
Also, PHCWs in rural settings presented with more preparedness awareness, compared to PHCWs in urban areas (B=0.98, 95%CI 0.39,1.58; p=0.001), a finding that remained significant after multivariable analysis (B=1.10, 95%CI 0.28–1.92; p=0.008; Table 4). Moreover, belonging in a high-risk group or living with high-risk individuals was a significant parameter, with those participants showing less awareness about the pandemic preparedness plan (B=–0.55, 95%CI –0.95– –0.16; p=0.006). Gender did not play a significant role, even though female PHCWs seemed more aware than male participants (B=0.31, 95%CI –0.02– –0.85; p=0.246).
Risk perception regarding the pandemic
Risk perception was a parameter investigated in the study as a factor that influences PHCWs’ ability to cope with pandemic response. Work-related concerns were highlighted by PHCWs, who worried about staff shortage (79.1%) or equipment and material shortage (90.3%). They also believed that their colleagues, both physicians (75.2%) and non-physicians (82.9%), were worried about getting infected. While most PHCWs feared about the health risk they underwent at work (86.1%) and they might be unnerved examining patients (63.1%), only a minority considered asking to be appointed to another position (16.9%). On the other hand, not many PHCWs would have been willing to work during the pandemic if they or their spouses were pregnant (25.0%), living with a child (44.8%) or with older people in the same household (27.7%), or if there was a high risk of transmission in their household (41.4%).
Dealing with the pandemic is an issue that concerns PHCWs away from work too. The majority (86.7%) were worried about the infection risk they might impose to their family and avoided discussing work issues with them (53.4%) to alleviate their concerns. Over one third (37.8%) believed that their social circle would rely on them for information about the pandemic and an alarming 66.9% feared stigmatization from people, who might avoid them due to their line of work.
Table 2 shows an analytic approach to PHCWs’ perception on pandemic risks according to their line of work. In multivariable analysis it was shown that only first-line non-physicians were less concerned than first-line physicians regarding an imminent shortage of staff at work (OR 0.50; 95%CI 0.26–0.97) and whether physicians would get infected (OR 0.51; 95%CI 0.27–0.96).
Female participants seemed to perceive risk more lightly than their male counterparts (B= –0.54, 95%CI –0.10– –2.11; p=0.035) and the same applied for second-line PHCWs against their first-line physicians (B= –0.68, 95%CI –0.10– –2.02; p=0.045). This finding remained significant in multivariable analysis, risks were perceived at a lower level by second-line PHCWs compared to first-line physicians (B=–0.78, 95%CI –1.49– –0.08; p=0.028; Table 4). Moreover, older PHCWs had fewer concerns than their younger colleagues (B=–0.04, 95%CI –0.08– –0.01; p=0.025). Concerns in general escalated as the working experience of the participants increased (B=0.04, 95%CI 0.00–0.07; p=0.050).
Table 4: Multivariate linear regression analysis of primary healthcare worker awareness and risk perceptions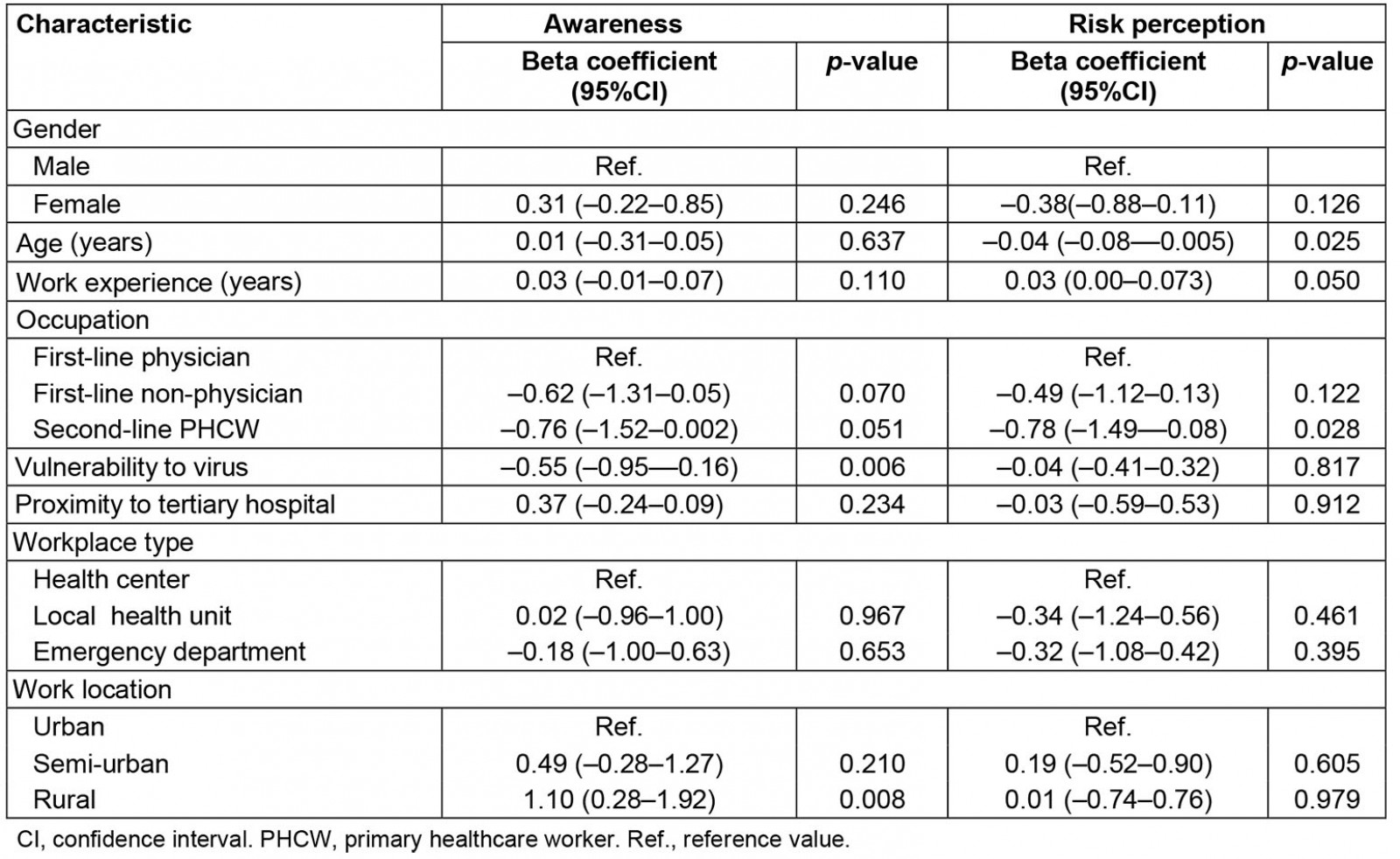
Discussion
This study used a multi-centered, quantitative, cross-sectional design to evaluate perceived awareness, preparedness level and risk perception of PHCWs in Greece during the initial phase of the pandemic. The results of this research showed that, during the first months of the COVID-19 pandemic, the majority of the participants were aware of the theoretical background regarding the infection, such as NPHO instructions, case/ close contact definition and countries with high community transmission. The majority of participants felt confident about procedures such as referral of suspected cases and safe case triage. Although most participants felt their facility was prepared to perform triage and were informed of the main reference healthcare facilities in their area, only half of the participants reported working in an adequately organized facility with trained personnel and having an active contingency plan. Primary care in rural settings can face challenges, especially during emergencies and pandemics and it is suggested that facilities should have preparedness plans tailored to their needs and information systems, enabling communication with patients and other reference facilities10, especially in short-staffed primary care settings15. PHCWs in rural areas presented with more preparedness awareness, compared to their colleagues working in urban areas (B=0.98, 95%CI 0.39–1.58; p=0.001). This finding could imply that working in facilities that did not offer the opportunity for COVID-19 testing, such as in rural areas, increased PHCWs’ need to be up to date with procedures and concerns about case management.
Participants’ risk perceptions related to their contribution to the pandemic response. Concerns about future shortages in personnel or equipment were reported by the vast majority of participants, a finding in line with other studies, where most healthcare workers (83.8%) consider it one of the most important reasons for their higher susceptibility to COVID-19 infection22 and one of the most frequently suggested sources of anxiety23. In the present study, profession played a significant role, with first-line non-physicians being less concerned than their physician colleagues (OR 0.50; 95%CI 0.26–0.97). Differences according to occupation were highlighted as well in a study conducted in Italy, in which physicians and nurses were more worried about personnel shortages than other staff (68.3% and 64.8%, respectively)24.
Participants were also concerned about their colleagues getting infected, but first-line non-physicians seemed more reassured than first-line physicians (OR 0.51; 95%CI 0.27–0.96). Other studies also support these findings, with perceived risk reported as significantly higher for physicians and nurses, probably because of their occupational categories identifying their workplaces as having the higher degree of infection risk24,25, a fact consistent with the higher risk of infection due to frequent exposure to COVID-1926. This level of concern, however, does not stem from lack of knowledge regarding the pandemic – these professionals are the ones who score higher for knowledge in the present study and in others24. This concern could have emerged from the fact that, during the initial phases of the pandemic, many countries had not introduced recommendations for the protection of health workers such as staff rotation for those working in high-risk areas (eg emergency departments) in order to decrease the exposure time to COVID-19 cases27. Regardless of the risk they might have, only a minority of PHCWs would consider asking for a different job appointment, a finding that suggests a high level of ethical commitment, and this is in accordance with other studies25.
The majority of participants express fear about their health in relation to their clinical duties, particularly while examining patients. Similar findings were reported in other studies, where 83.1–85% of respondents were afraid of getting infected22. At almost the same rate (86.7%), participants were worried about the burden of infection on their families, and more than half tried to alleviate their families’ fears by avoiding any discussion related to work, findings consistent with a Singapore study, although not at such high proportions (74.7% and 21.5% respectively)25.
In the same study and in another in Egypt22,25, fear of stigmatization was reported at the same rate as in the present study, where two-thirds of participants (66.9%) reported that their acquaintances would avoid them because of their work environment. Avoidance of healthcare workers, an under-recognized form of stigmatization during the COVID-19 pandemic, was also experienced by participants of an Egyptian study even if their work was not directly related to caring for COVID-19 patients28. Stigma impacts PHCWs’ everyday lives, even away from the work environment, which might be expected because people are following preventive strategies and are actively avoiding those they see as possible COVID-19 carriers29.
Research showed a direct negative association between healthcare professionals’ psychological wellbeing and their fear and risk perception of COVID-19, even after controlling for coping strategies30, with risk perception of COVID-19 being among the main sources of anxiety23.
Limitations
Some limitations might be taken into consideration due to implementation of this study during the ongoing COVID-19 pandemic. The non-randomized sampling strategy employed does not ensure the generalizability of findings, since an initial panel of PHCWs was used for the distribution of the questionnaire. However, the obtained response rate was satisfactory, and there was sufficient participation of PHC facilities from every administrative area of Greece. The design included only public PHC services, leaving out the private practices, which at that time were not actively involved in the pandemic response. About 67% of the participants are female, which is line with the figures reported by Eurostat in 2020 that in Greece about 61% of healthcare workers are women31. Awareness level was obtained only from self-reported answers. However there was a high correlation with objective knowledge items, showing that the evaluation of awareness through questionnaire items could yield significant responses. Another limitation is that the questionnaire in this study, used to explore the awareness and risk perception of PHC professionals, has not been validated as a tool, since this was not the aim of the study. Finally, the quantitative design of this study might have masked PHCWs concerns or issues that were not included in the questionnaire.
Conclusion
From the early months of the pandemic, PHCWs revealed high awareness of the response measures and management protocol requirements that were in place by the NPHO. In order to preserve their up-to-date knowledge, guidance should be communicated promptly with consideration to the need to be inclusive of all primary care professionals and their diverse needs according to their work setting and population needs32. This is important for remote areas and countries with particular geographical characteristics, such as Greece. Populations in mountainous parts of the country and islanders may have access only to PHC facilities and not to specialized units operating in urban centres. In these settings and particularly during crises, such as the COVID-19 pandemic, more effort should be expended in order to reinforce PHC services and avoid inequalities in the management of acute and chronic diseases in the rural population. Moreover, PHC facilities should be further empowered with all required human, material (eg personal protective equipment) and non-material resources (eg training for the management and recognition of post-COVID syndrome, vaccine-induced thrombosis with thrombocytopenia syndrome) in order to achieve clinical adequacy during this particularly demanding period, while COVID-19 vaccination is also part of the PHC facilities’ routines.
Assessing the needs and concerns expressed by PHCWs during every phase of the pandemic should be part of strategic planning. In this study, participants’ concerns were related mainly to their workplace but they maintained their sense of commitment. Since the beginning, the psychological burden of the pandemic on first-line PHCWs, who experienced the fear of uncertainty, was significant. PHC, as part of health systems, has been operating at maximum capacity for more than a year and it is clear that healthcare workers need to have their safety and mental wellbeing ensured because they are the most valuable resource in every health system33.
Implications
Further research could be undertaken on wellbeing and resilience of PHCWs. Factors that determine their awareness of preparedness plans or lack of it should also be studied along with implementing interventions that would strengthen PHC’s response to crisis. These responses need to adjust in a timely way to provide high quality healthcare services and contribute to the COVID-19 pandemic containment, even in remote areas.
As the pandemic continues, the spotlight shines on primary care, not just because of its critical position in augmenting initial response, but also regarding the need to adapt amendments and services to respond holistically and more effectively.







