Introduction
The prevalence and fatality rates of COVID-19 have disproportionally affected rural communities across the USA when compared to their urban counterparts. According to the Centers for Disease Control and Prevention (CDC), 7-day case incidence increased at a greater rate in rural communities from August 2020 to December 2020, and the 7-day death rate per 100 000 population in rural communities has been greater most days since 6 August 20201. Further, the cumulative death rate per 100 000 population in the USA among rural residents has been consistently greater than for urban residents since 9 December 2020 and is 13.6% greater as of 1 June 20211. These differences are exacerbated by cultural norms and lack of medical and public health resources2-5.
Longstanding systemic health and social inequities have put some rural residents at increased risk of COVID-19 infection2,6-11. Rural Americans have higher rates of cigarette smoking, high blood pressure, and obesity, are less likely to have health insurance, and have limited access to medical care services, all of which negatively affect health outcomes12-16. Similarly, African Americans, American Indians, and Latinx residents are at increased risk of COVID-19 infection and illness severity in these rural areas7.
One way that COVID-19 can be mitigated is through uptake of the currently available vaccines; however, an estimated vaccination rate of at least 70% was required to achieve herd immunity against the Delta variant17,18. Vaccine uptake rates among adults in the rural USA and rural Oklahoma are lower than in the urban USA and Oklahoma19. Further, 32% of the total rural population of Oklahoma is fully vaccinated, compared to 42% of the total urban population of the state as of 9 August 202120. One possible explanation for the difference in vaccine uptake between these populations is higher vaccine hesitancy, in general, among rural populations21. Vaccine hesitancy is exacerbated within economically marginalized rural communities that lack access to healthcare providers and receive inadequate health education, resulting in more severe disease and lower health literacy22,23.
Data from the 2017 National Immunization Survey–Child Survey suggests that a lack of childhood vaccination coverage among uninsured children and living outside of metropolitan statistical areas for diseases (eg measles, mumps, rubella, hepatitis B) could be addressed through increased awareness and use of vaccination programs, eliminating missed vaccination opportunities during healthcare visits, and minimizing health insurance coverage interruptions24. Despite being widely recommended and fully covered as a preventive service under the Affordable Care Act, data show that the overall rural influenza vaccination rate is suboptimal25. Among Medicare enrollees (ie those over the age of 65 years, younger individuals with a disability or diagnosed with end-stage renal disease), county-level flu vaccination rates range from 21% to 62%, with 18 rural Oklahoma counties reporting rates less than 40%26. A general public distrust of intrusions on individual liberty, mixed with the loss of confidence in government institutions under current social conditions, and a psychological distance (ie the degree to which people feel removed) from the risk of deadly communicable diseases has lowered US vaccination rates in recent years27-29. Further, rural areas of the USA have a higher proportion of individuals with more conservative ideologies who are less likely to accept COVID-19 vaccination30-34. Recent findings have further demonstrated that consumption of news from conservative media outlets (eg Fox News, Breitbart News, One America News) are strongly associated with unwillingness to get the COVID-19 vaccine32,35.
Although advances have been made in identifying individual, interpersonal, and contextual influences on uptake of other infectious disease vaccines, vaccine hesitancy interventions have too often narrowly focused on clinician-initiated interventions (eg clinicians recommend and discuss benefits to vaccination during a medical visit) that are unsuited to rural community norms, health behaviors, and healthcare access. Rural communities in Oklahoma encounter numerous barriers to care despite changes resulting from recent Medicaid expansion36,37; 72 of Oklahoma’s 77 counties are designated by the Health Resources & Services Administration as Health Professional Shortage Areas for primary care38. This leaves many Oklahomans with limited access to clinical services, thereby reducing the potential impact of traditional clinician-initiated vaccine interventions. Consequently, local county outreach is essential for the success of any COVID-19 vaccination intervention. To provide this kind of outreach, nuanced data on the perspectives of rural communities regarding COVID-19 specific vaccines are required.
Present study
Given the nascent literature surrounding vaccine uptake, specifically concerning COVID-19, within rural communities, the present study sought to explore perceptions regarding COVID-19 vaccination among unvaccinated residents of rural Oklahoma. The present study analyzes responses to open-ended questions evaluating the concerns and perceived benefits of vaccination against COVID-19.
Methods
Participant recruitment and data collection
Between March and May 2021, 391 residents within rural Oklahoma counties completed a cross-sectional, online questionnaire to assess health behavior changes during COVID-19. The Index of Relative Rurality (IRR) was utilized to determine the rurality of a participant’s residence, with all participants residing in counties with an IRR score greater than 0.4039. Participants were recruited through internet-based direct marketing (eg advertisements placed on social media sites), community-based organizations, and peer referral. Participants were eligible if they were aged 18 years or older and a resident of an identified rural Oklahoma county. The online questionnaire took approximately 20 minutes to complete, and participants were offered the opportunity to enter a draw to win one of 65 gift cards valued at US$50.
As part of this larger study, the authors sought to qualitatively assess perceptions, benefits, and concerns regarding getting vaccinated for COVID-19 among those participants who had not yet been vaccinated (n=222 participants from 22 counties). These counties range in population from 15 553 to 72 454 residents. As shown in Table 1, unvaccinated participants (n=222) ranged from age 18 years to 83 years (mean=43.35 years), with most respondents identifying as female (86.0%), and White (87.8%). Additionally, 50% of participants reported typically getting vaccinated for influenza.
Table 1: Sample demographics (n=222) 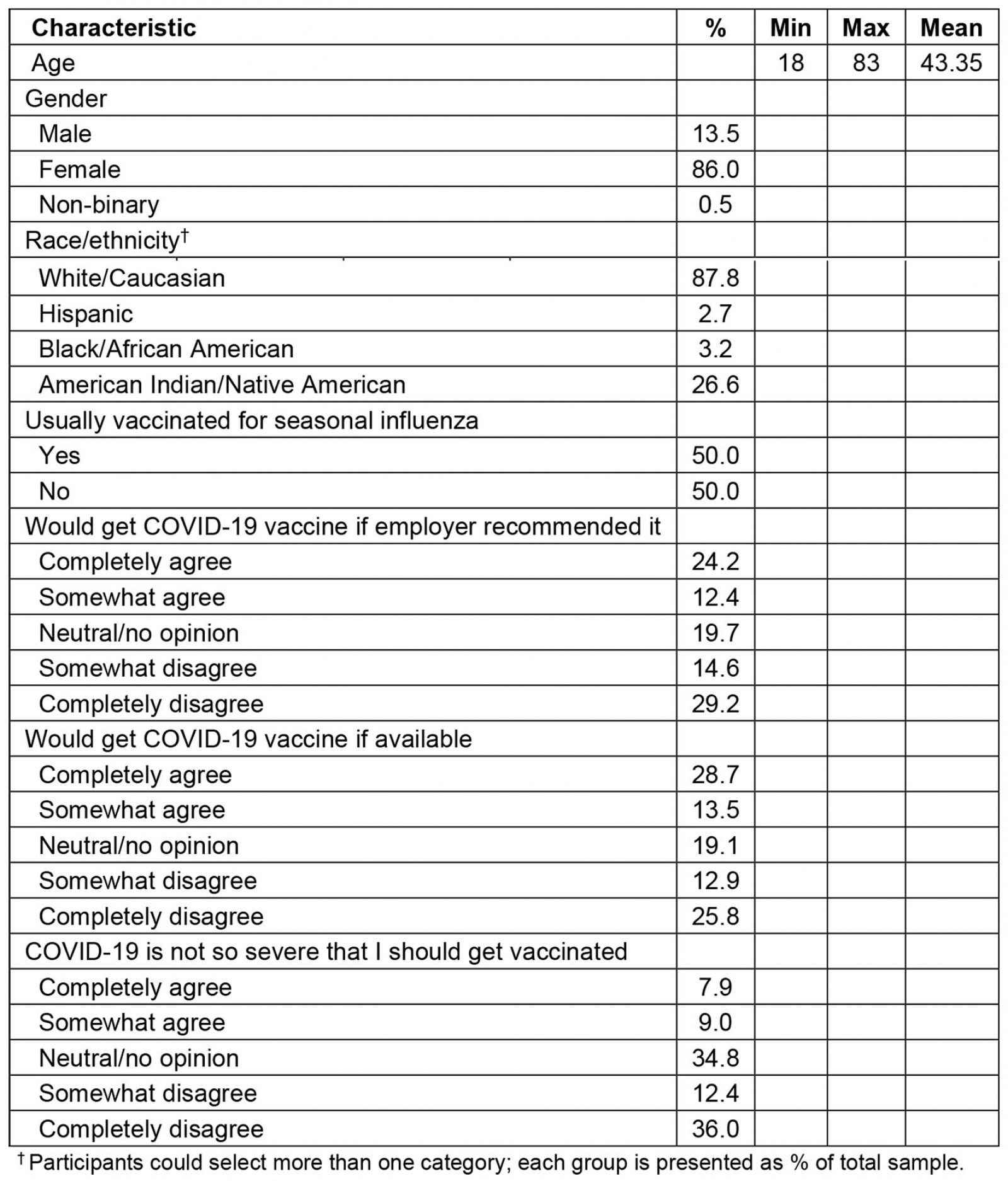
Online survey
Unvaccinated participants first responded to two open-ended questions, which qualitatively assessed barriers and benefits to vaccination: ‘What are potential benefits to getting vaccinated for COVID-19?’ and ‘What concerns do you have regarding the COVID-19 vaccine?’ Tailoring questions from the Kaiser Family Foundation COVID-19 Vaccine Monitor21, the authors quantitatively evaluated participants’ tendency to get vaccinated for seasonal influenza (ie ‘Do you usually get vaccinated for seasonal influenza?’) and potential vaccination determinants (ie ‘I would get the COVID-19 vaccine if available’, ‘I would get the COVID-19 vaccine if my employer recommended it’, ‘COVID-19 is not so severe that I should get vaccinated’).
Data analysis
Two research team members independently open-coded participant responses. Consistency checks were conducted to assess reliability among the coders. Responses were analyzed separately for each question using an inductive approach, assessing observations to detect patterns and regularities, to identify and interpret concepts and themes that emerged from these data. Concepts were the most basic unit of meaning from which results developed. Related concepts were grouped together to form overarching themes. The Statistical Package for the Social Sciences v24 (IBM; http://www.spss.com) to analyze demographic characteristics and descriptive statistics.
Ethics approval
All protocols were approved by the institutional review board at Oklahoma State University Center for Health Sciences (#2020025), and each study participant completed an informed consent process.
Results
Several factors were identified that could affect the acceptability of the COVID-19 vaccine. The identified themes and illustrative quotes are provided in Tables 2 and 3.
Perceived barriers to COVID-19 vaccination
Participants viewed there to be a lack of scientifically accurate COVID-19 information being disseminated within their communities, which led some to make vaccine decisions based on commonly disseminated disinformation and misinformation (Table 2).
Rapid vaccine development, efficacy, and lack of long-term data: Lack of research and of long-term safety studies were the most frequently identified concerns related to receiving the COVID-19 vaccine. This included skepticism related to long-term potential outcomes, the use of mRNA technology in an expedited manner, and a lack of clarity as to why the vaccine was only approved under the Emergency Use Authorization of the US Food and Drug Administration (FDA). In rare instances, such concerns were exacerbated by vaccine misinformation and conspiracies, for example that the use of mRNA technology would ultimately alter the genetic make-up of vaccinated individuals. Respondents noted that their medical providers (eg physicians, nurses) shared their own concerns about the vaccine, ultimately decreasing the participants’ willingness to schedule a vaccine appointment at a local site.
Efficacy was noted by participants as a driving factor in their COVID-19 vaccination decision. Among these participants, there was a tendency to perceive the vaccine as less efficacious than reported by government agencies and even more so against emerging new strains. Similarly, participants viewed the COVID-19 vaccine as comparable to the seasonal influenza vaccine in which yearly shots or potential boosters would be required. Respondents noted decreasing vaccine protection over time would require semi-annual or annual shots, which they thought could lead to further vaccine complications.
Vaccine complications: Participants noted that potential adverse reactions and side-effects from vaccination limited their intention. Concerns ranged from missing work due to feeling unwell after receiving a dose to fearing an anaphylactic reaction. Most notably, respondents expressed the potential for adverse long-term side-effects yet to be discovered within current clinical trials. Relatively few participants mentioned a pre-existing condition and possible complications as a barrier to vaccine uptake, with most expressing concern about potential interactions with their prescribed medications or limited data on how vaccination could impact their health condition.
Vaccine availability: Fewer than 20 participants perceived lack of availability of COVID-19 vaccines within rural communities to be a barrier. In these instances, individuals noted the need to drive longer distances to receive vaccination or viewed themselves, at the time of responding, as not yet eligible for vaccination.
Table 2: Perceived barriers to COVID-19 vaccination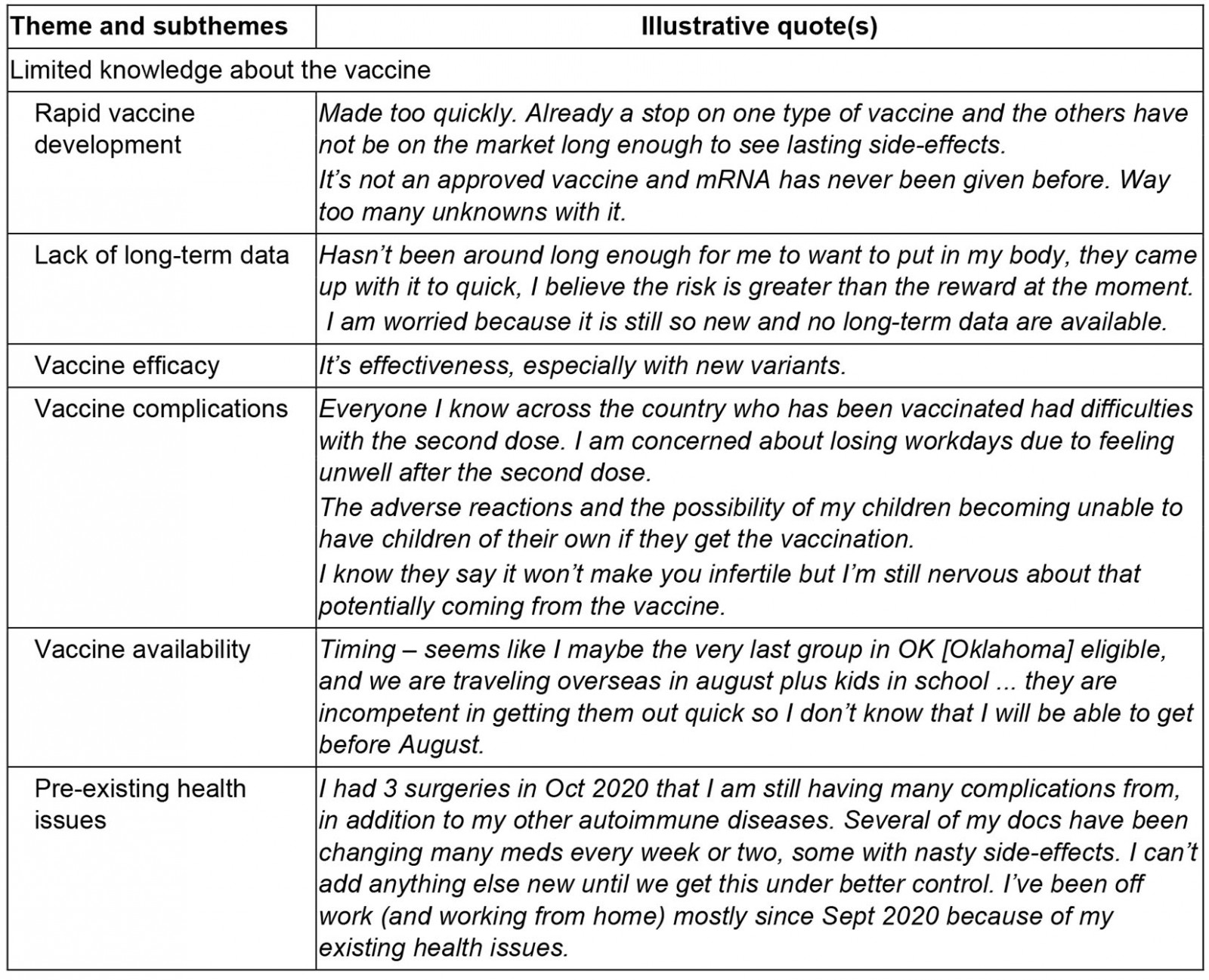
Perceived benefits of COVID-19 vaccination
Individual level prevention of COVID-19: The most commonly reported benefit of COVID-19 vaccination was to lower the risk of acquiring COVID-19 (Table 3). Several respondents also mentioned decreased severity of symptoms if they were to contract COVID-19 in the future. On a few occasions, respondents indicated that higher risk populations could benefit from vaccination (eg elderly, immunosuppressed), although they did not specifically mention themselves as a candidate for vaccination.
Community-level prevention of COVID-19 transmission: Respondents emphasized that vaccination would lead to decreased COVID-19 transmission. Some mentioned protecting family, ‘loved ones’, and vulnerable populations, especially older adults, as potential motivators. Others provided a more general reference to preventing spread within the community, with several indicating achieving herd immunity could be a prospective benefit of vaccination.
Return to normal: For many participants, vaccine uptake within their community was related to the desire to ‘return to normal’, in which an incentive to being vaccinated was the ability to engage in activities enjoyed pre-pandemic. Specific activities mentioned included traveling, returning to work, attending events, and not having to adhere to COVID-19 precautions, such as wearing masks or quarantining.
Table 3: Perceived benefits of COVID-19 vaccination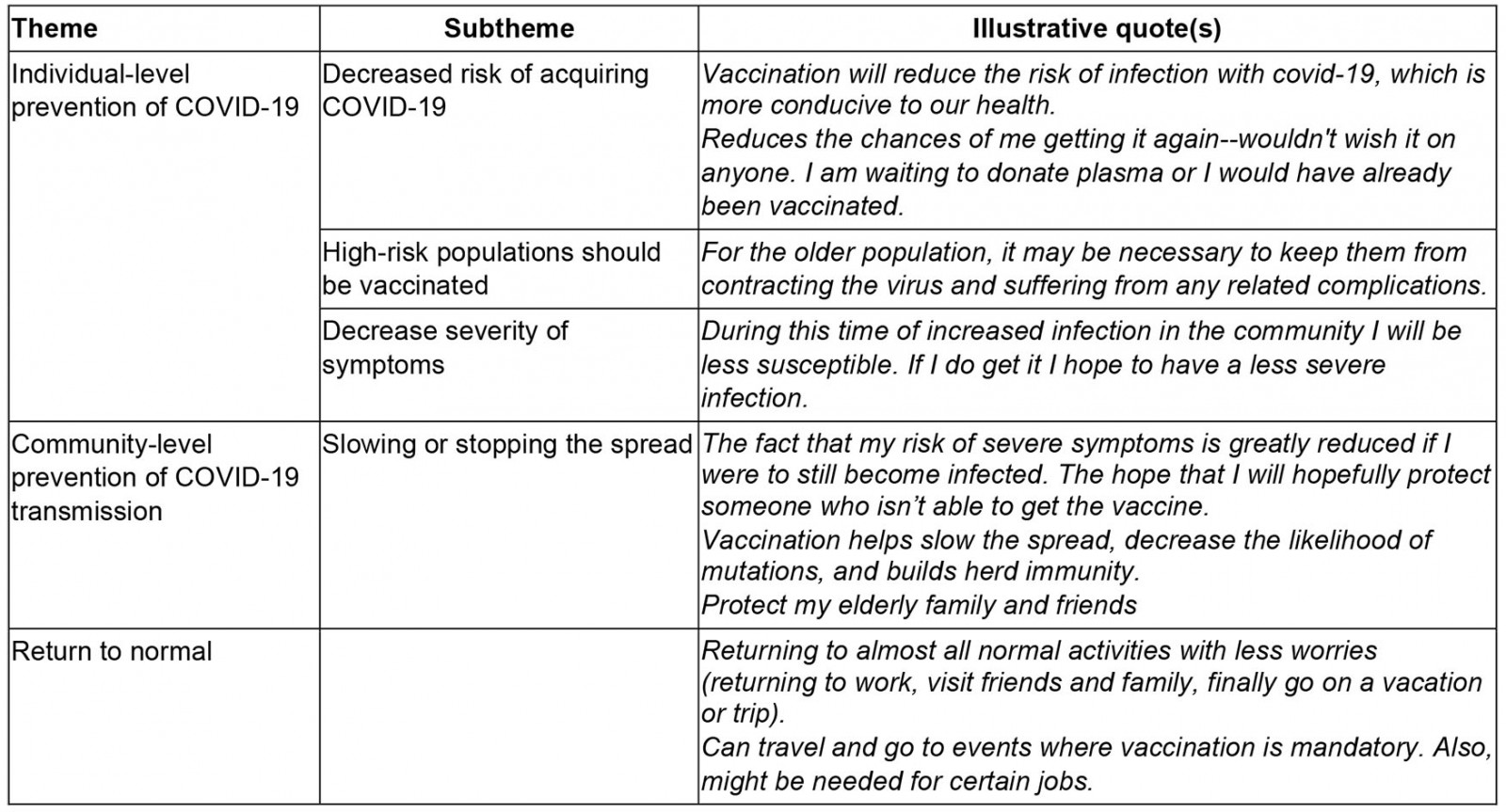
Discussion
The present study investigates people’s perceptions regarding vaccination against COVID-19 in rural Oklahoma between March and May 2021. These results suggest that the general, unvaccinated, adult population of rural Oklahomans have mixed reactions regarding vaccination against COVID-19 despite three vaccines (Pfizer and BioNTech, Moderna, and Johnson & Johnson) having emergency use authorizations in the USA at the time of the study.
Individual- and community-level prevention of COVID-19 transmission and returning to normal were the most commonly reported perceived benefits of vaccination. These findings are consistent with the motivating factors reported by other studies. In a survey of hospital employees, Kuter and colleagues40 found that protection of one’s self and family were the most perceived benefits of vaccination. A swift return to normal was also highlighted by Geana and colleagues41, who found that women leaving jails thought that vaccination would help life return to normal within a year. These findings suggest that there is a fraction of the population that believes vaccination against COVID-19 is beneficial, but they are still hesitant to receive the vaccination themselves.
The desire to protect others and return to normalcy has been shared by government organizations, companies, politicians, universities, celebrities, and individuals across social and traditional media to boost an array of COVID-19 mitigation behaviors (eg mask-wearing, physical distancing, vaccination)3,42-44. Despite the plethora of public health campaigns to increase COVID-19 vaccination45-47, and the majority of adults in the USA having received at least one dose of the vaccine1, many are still hesitant21. Potential adverse reactions and side-effects following vaccination were a concern among vaccine-hesitant participants in the present study. Individuals may have more of an emotional response to the potential of having adverse reactions even though there may be a greater benefit from vaccination48. Only half (48.4%) of participants in the present study believed that COVID-19 is so severe that they should get vaccinated. This is particularly concerning among populations with comorbid conditions. Recent work has noted such populations are ambivalent to vaccination despite being at higher risk of severe infection49.
A lack of accurate information disseminated within local communities regarding COVID-19 vaccination remains a driver of vaccine hesitancy among unvaccinated rural Oklahomans. This gap has exacerbated skepticism over the development and use of mRNA vaccines, instilled distrust in government agencies including the CDC and the FDA, and led to ideologically disparate groups coming together around their shared skepticism, which is further spreading inaccurate information49-51. Similarly, healthcare providers in these rural communities are not immune to their own skepticisms and ideologies and may share these with their patients. Future research should further examine the role rural providers play in spreading vaccine misinformation.
Implications
The present study’s findings indicate that new and modified interventions responsive to rural communities must be developed to address vaccine hesitancy. For example, efficacy and side-effect concerns can be addressed by local health clinics providing historical information about vaccine side-effects and the science behind mRNA vaccines. Such approaches have been utilized to educate parents when considering COVID-19 vaccination for their children52. Similarly, transitioning away from government-led vaccination clinics to offering the COVID-19 vaccine at rural health clinics and through primary care providers may facilitate discussion of vaccine concerns with a local and trusted provider48,53,54.
Rural communities often comprised small populations and tightly knit social structures55,56. Rural social networks are critical to supporting behavior change. The Popular Opinion Leader model, utilized to promote HIV risk reduction, posits that behavior change is achieved when new risk-reducing methods are disseminated by opinion leaders through personal contacts in their social network57. In response to the COVID-19 pandemic, rural community influencers should be trained and given resources to reduce disease stigma, increase perceived disease severity, discuss the benefits of vaccination, and provide accurate, up-to-date epidemiologic information in their area58-60. Faith leaders are one such group that have been shown to effectively disseminate public health information in rural communities61-63. Adapting the Popular Opinion Leader model to enhance vaccine uptake is one example of adapting existing interventions to complement other public health efforts during the COVID-19 pandemic.
Limitations
The present study is not without limitation. First, participation was voluntary and focused largely on health concerns and perceived needs within Oklahoma. The views of those volunteering to complete the online questionnaire may not reflect the larger rural population in Oklahoma. Second, the sample largely comprised rural White and American Indian individuals, thus limiting the authors’ ability to evaluate vaccine hesitancy concerns specific to various racial/ethnic groups. Third, as all data were collected using online methodologies, these findings may not include rural residents with limited or no internet service. Lastly, as an exploratory study, the findings may not be representative of the larger rural population in Oklahoma.
Conclusion
COVID-19 vaccination is a preventive strategy that reduces disease transmission and decreases mortality. Despite this, vaccine uptake varies widely by geography and rurality. The present study highlights key determinants of vaccination hesitancy among a population disproportionately impacted by the pandemic. This is particularly concerning as COVID-19 rates are increasing due to new predominant variants (eg Delta). Public health activities and health messaging campaigns should engage local rural community leaders while focusing on the unique strengths and assets of rural communities.



