Introduction
Australia’s healthcare system is predicated on strong values of universal health coverage, which espouses the availability of affordable medical care when and where people need it1. General practitioners (GPs) strongly lead this agenda. In over 80% of their consultations, they charge fees equivalent to a national Medicare Benefits Schedule (MBS), known as bulk billing, with patients incurring no out-of-pocket costs2. However, the MBS policy allows doctors the discretion to set their fees above the Medicare rebate, for some or all patients, so that these patients must make a co-payment for seeing a GP. This flexibility recognises that the income provided by the MBS may be inadequate to cover staff expenses and other overheads. Practices must weigh profitability with the duty to provide all population subgroups equitable access to their services. In addition to the business and healthcare considerations, letting doctors set their fees is important for the stability of the GP workforce, whose members’ ability to make a living is crucial to the sustainability of general practice, especially in settings where the Medicare rebate may not be financially adequate3.
During the COVID-19 pandemic, from March 2020, general practices rapidly pivoted to telephone and video call (telehealth) consultations as a means of protecting their staff and patients from infection, and ensuring the community still had access to primary care (36% of national GP consultations in April 2020)4,5. Practices were initially required to bulk bill for these telehealth consultations. Rapidly imposing a bulk billing only policy may have had detrimental effects on those practices reliant on patient co-payments as part of their business model. A national survey of general practice during the 2020 COVID-19 pandemic identified that telehealth reimbursements were among the top issues that GPs considered were having a high/medium impact on them (74% rated this as so), following other issues such as the safety of staff (86%), disinfecting (86%), lack of protective equipment (80%), and patient management (78%)6. However, there is limited contemporary information to indicate which general practices are likely to be affected by a rapid shift to bulk billing only policies. Medicare statistics on government webpages provide aggregate bulk billing counts/proportions of consultations that are bulk billed, with no data on the practices that bulk bill all, some or no patients.
Outdated evidence suggests that both patient and practice factors relate to whether GPs bulk bill. A 2002 survey showed metropolitan practices and those seeing more patients per week were more likely to bulk bill all patients7. A more recent survey (2013) showed patients were less likely to be bulk billed if they attended larger practices, had a set appointment, were based in regional centres and came from higher income households. Patients more likely to be bulk billed were those with chronic diseases, concession cards or private health insurance, irrespective of consultation duration8. Additionally, bulk billing may vary by doctors in the same practice9, and by electorate/state10.
With this background in mind, this study investigated which practices are more likely to bulk bill, to understand the potential impact of rapid shifts to bulk billing only policies.
Methods
Data
The authors sourced data from a stable period before the introduction of mandatory telehealth bulk billing policies. To explore time and locational factors related to MBS bulk billing for non-referred GP attendances, publicly available MBS data were used11. State or territory of residence was determined by the patient’s geocoded address. Rurality of residence was based on the Modified Monash Model (MMM) levels 1–712. Year of service (2012–2019) was based on processing date of the claim.
Additionally, the authors analysed data from the 2019 General Practice Supervisors Australia (GPSA) cross-sectional survey on practice bulk billing behaviours. The GPSA annual survey of GPs, who are also supervisors, is done to inform policy and practice. The survey was developed and piloted by the research team and administered by GPSA through SurveyMonkey. An invitation to participate was sent to GPSA’s regular contact email list (n=4439) in April 2019. Survey responses were anonymous.
The survey consisted of 44 multi-part questions, with a subset related to bulk billing. These included ‘Does your practice bulk bill in any of the following formats?’ Possible responses were ‘no patients are bulk billed’, ‘all patients are bulk billed’, ‘children and pension card holders are bulk billed only’, ‘bulk billing occurs at discretion of practitioners’, ‘other’. The survey also included questions about practice characteristics including location and number of general practitioners (GPs).
Analysis
First, descriptive statistics compared bulk billing rates over time by rurality, and state or territory, using the MBS datasets. Second, GPSA survey data were analysed to explore practice bulk billing patterns by rurality, state or territory, and practice size. A multivariate logistic regression model of factors significant for ‘all bulk billing’ compared with ‘not all’ was then undertaken to assess statistical significance (p<0.05), controlling for other factors.
Ethics approval
The survey had ethics approval from Monash University (project ID 19442), ratified by The University of Queensland (project ID 2019002835).
Results
National Medicare Benefits Schedule data
Figure 1 shows the percentage of general practice attendances bulk billed, by rurality and for Australia as a whole, from 2012 to 2019. Nationally, bulk billing rates steadily increased from 82% in 2012 to 86% in 2017–2019. They varied by rurality: highest in very remote (Modified Monash Model (MMM)7) (89–91%) and metropolitan areas (83–87%), and lowest in regional centres (MMM2) (76–82%). MMM3–6 ruralities had intermediate bulk billing rates (79–85%). Bulk billing rates rose in all ruralities from 2012 to 2017 but declined slightly in rural areas (MMM2–7) from 2017 to 2019.
In 2019, the MBS bulk billing rates were highest in New South Wales and the Northern Territory (89%), and lowest in the Australian Capital Territory (ACT) (64%) and Tasmania (75%) (Fig2). Other states were clustered at the national average rate of bulk billing at 85–86%. From 2012 to 2019, bulk billing rates declined slightly in Tasmania, but increased for all other states/territories.
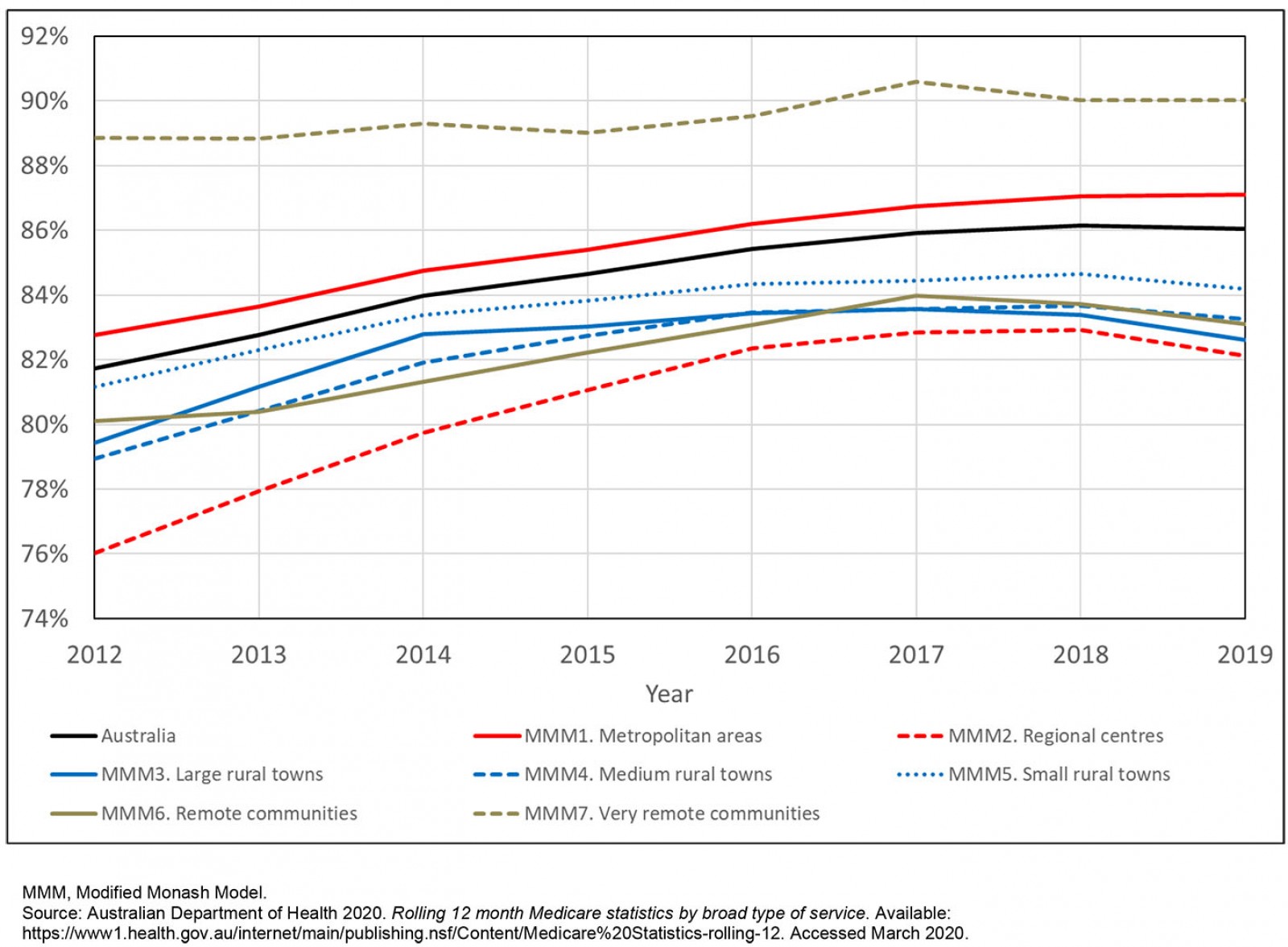 Figure 1: Percentage of annual general practice non-referred attendances that are bulk billed, by rurality, Australia, 2012–2019.
Figure 1: Percentage of annual general practice non-referred attendances that are bulk billed, by rurality, Australia, 2012–2019.
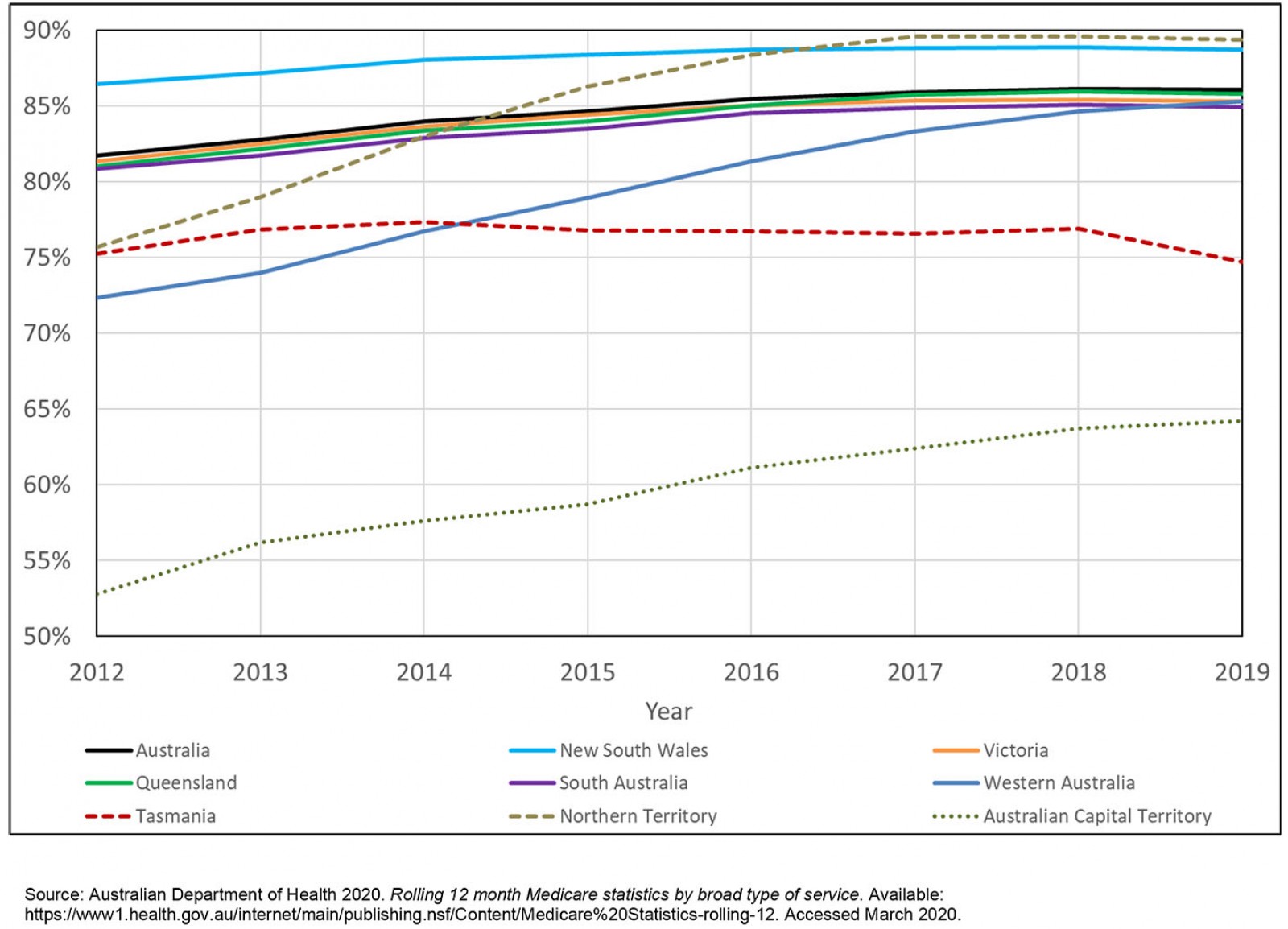 Figure 2: Percentage of annual general practice non-referred attendances that are bulk billed, by state or territory, Australia, 2012–2019
Figure 2: Percentage of annual general practice non-referred attendances that are bulk billed, by state or territory, Australia, 2012–2019
General Practice Supervisors Australia survey
Of 4439 emails circulated with the GPSA survey, 4410 were delivered, 1687 were opened, and 621 recipients clicked on the survey link (14% of those contacted and 37% of those who opened the email). Between 444 and 452 GP-supervisor respondents answered the relevant questions and were included in analyses.
Figure 3 shows that practice billing behaviour varied by rurality. Practices in metropolitan areas were most likely to bulk bill all patients (28%), and those in regional centres and large rural towns least likely (16%). Most practices limited bulk billing to selected patients – such as children and/or pensioners – ranging from 70% in metropolitan areas to 80% in rural areas.
Smaller general practices of up to five GPs were more likely to bulk bill all patients than were larger practices (of more than five GPs) (Fig4).
Table 1 shows the multivariate modelling of the relationship between bulk billing ‘all patients’ compared with ‘not all’. Practices in metropolitan areas, smaller practices (up to five GPs), and practices in the Northern Territory were significantly more likely to bulk bill all patients, controlling for other variables.
Table 1: Multivariate logistic regression exploring propensity of practices to bulk bill all patients, by rurality, state or territory, and practice size, General Practice Supervisors Australia supervisor survey, 2019 (n=444)†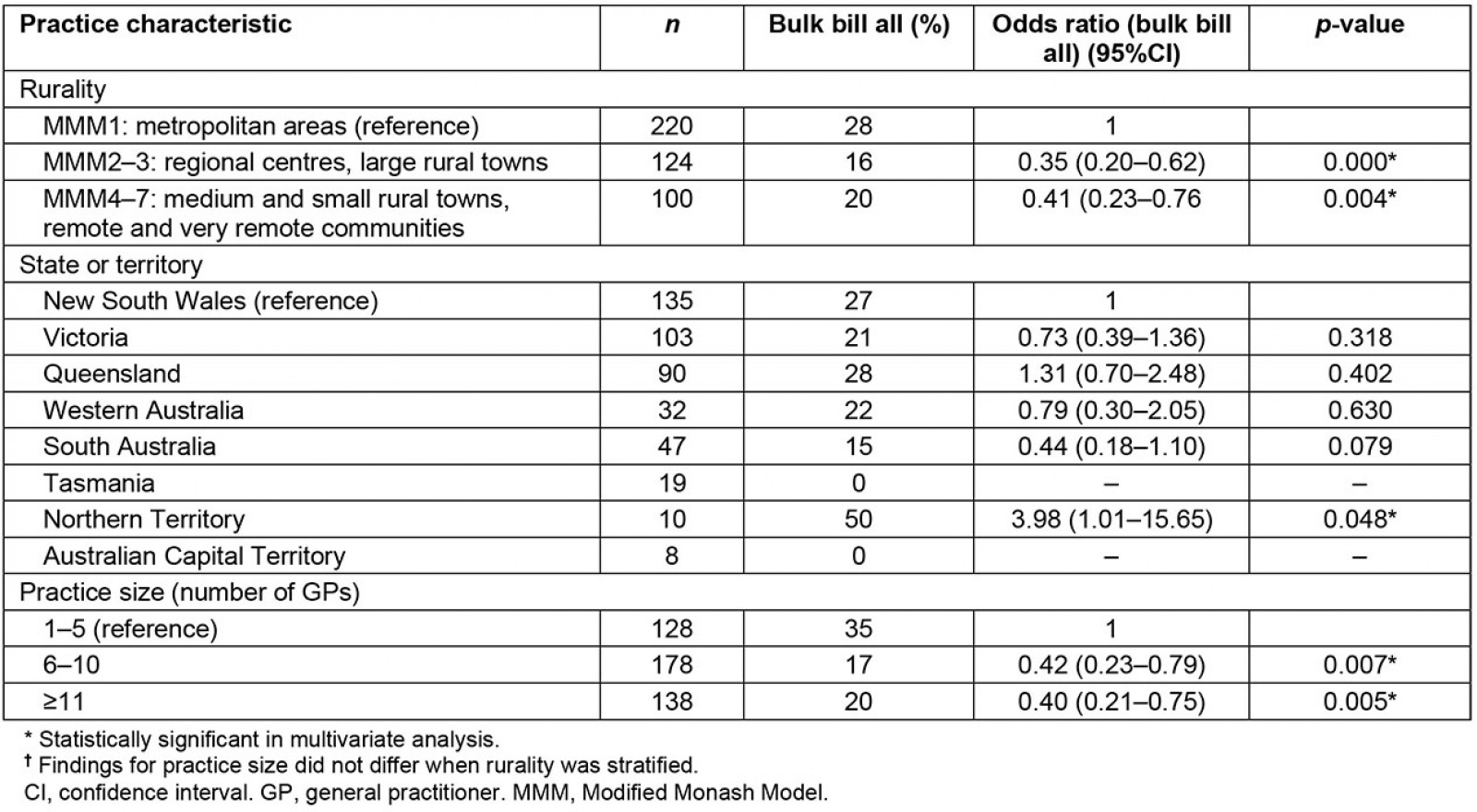
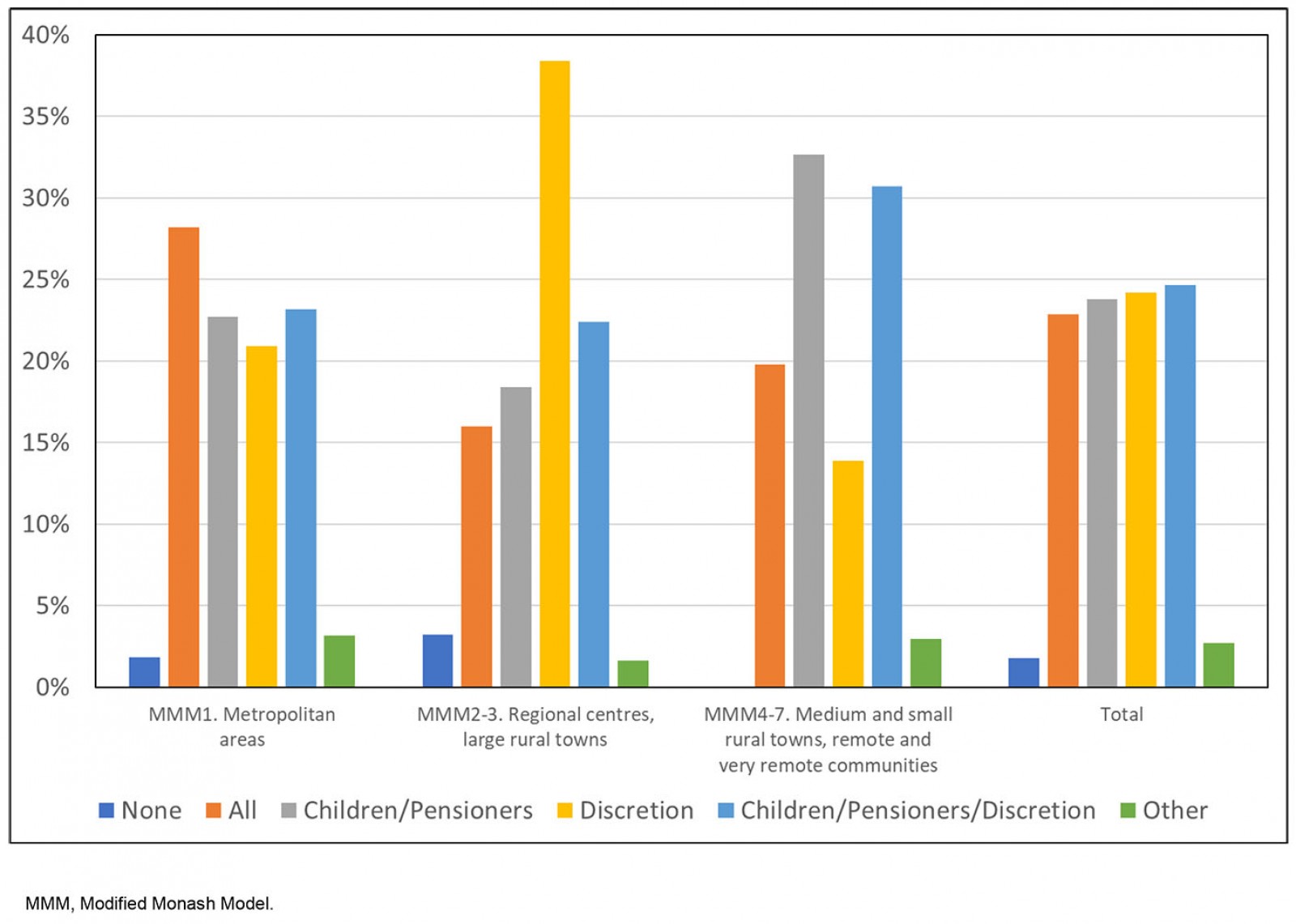 Figure 3: ‘Does your practice bulk bill in any of the following formats?’ Percentage distribution by rurality, General Practice Supervisors Australia supervisor survey, 2019 (n=446).
Figure 3: ‘Does your practice bulk bill in any of the following formats?’ Percentage distribution by rurality, General Practice Supervisors Australia supervisor survey, 2019 (n=446).
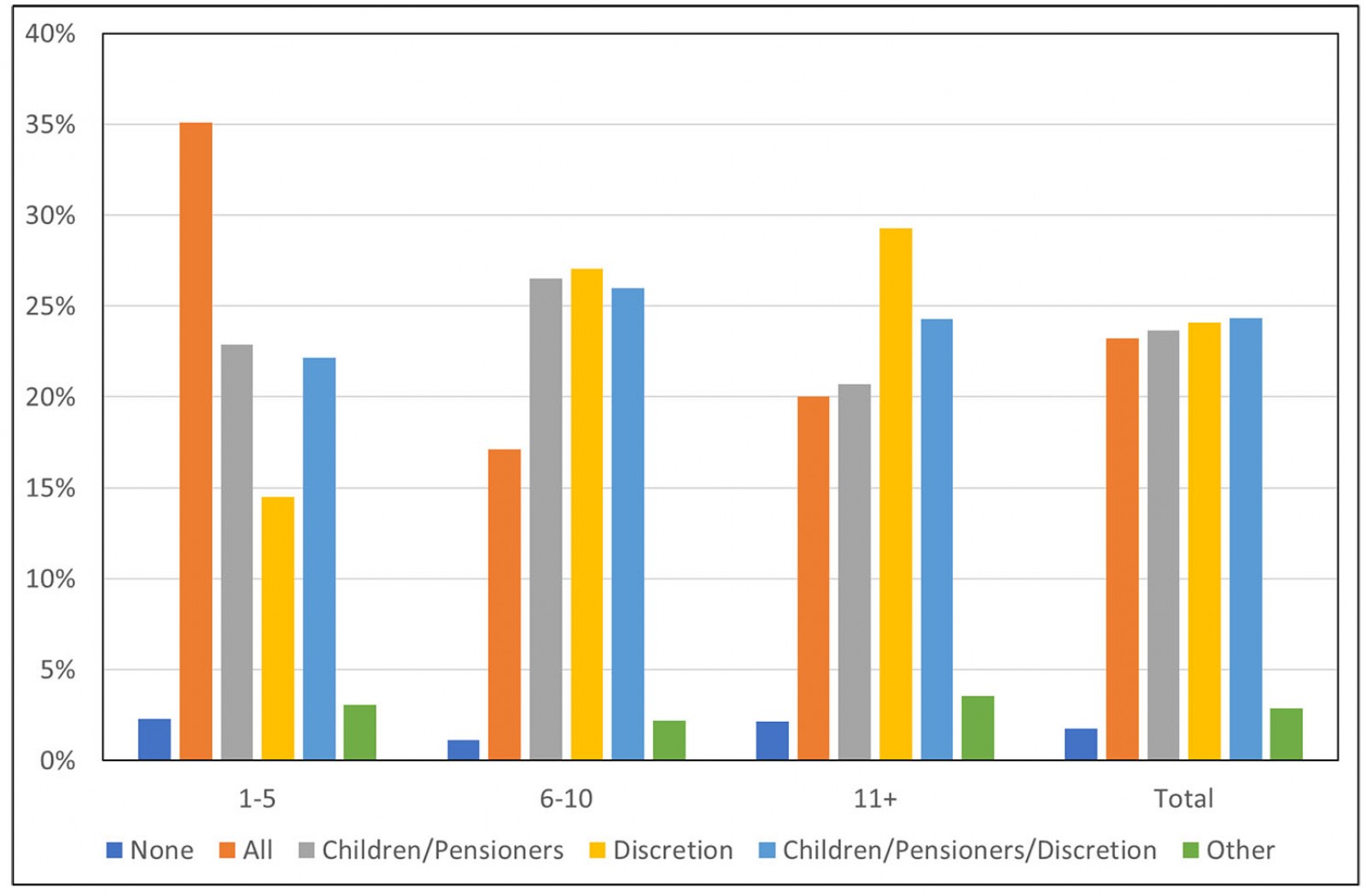 Figure 4: ‘Does your practice bulk bill in any of the following formats?’ Percentage distribution by practice size (number of general practitioners), General Practice Supervisors Australia supervisor survey, 2019 (n=452).
Figure 4: ‘Does your practice bulk bill in any of the following formats?’ Percentage distribution by practice size (number of general practitioners), General Practice Supervisors Australia supervisor survey, 2019 (n=452).
Discussion
Although various Medicare data are made publicly available, these are not necessarily used in general practice research. In fact, in conducting this study, it was discovered that Medicare – although it is the most substantial national reimbursement policy in Australia’s public health care – is substantially under-researched, or it is supported by outdated research, with regard to bulk billing patterns by practice context.
The authors relied on two data sources to triangulate findings, neither being perfect but providing complementary views of the problem. Both were from a stable period prior to the rapid rollout of bulk billing only models of care for telehealth GP consultations during the 2020 pandemic response4,13. The present study’s findings show that although national GP bulk billing rates tend to be high (86 of 100 GP appointments were bulk billed in 2019), bulk billing behaviour varies widely by practice factors (state, rurality and practice size). This suggests that an initiative to shift to bulk billing only should consider the varying degree of impact on different practices. Potentially, such a shift would have a greater deleterious impact on practices that routinely charge a co-payment for some or all patients, in comparison with practices that bulk bill all patients currently.
The national data identified that the rates of bulk billing are lowest and declining for practices based in rural areas (with the exception of very remote communities). The multivariate analysis of GPSA survey data also confirmed that practices most likely to rely on mixed or private billing are larger practices, and those based in rural areas.
The impact of mandatory bulk billing could be quite contained if policy shifts are short term and/or gradually introduced, whereby practices are given the opportunity to tailor telehealth consultations to the available MBS rebates and consider how to offset any losses. Loss of income might be considered acceptable if the policy has strong practice benefits such as reducing risks to staff and patients, which were urgent needs in the face of the COVID-19 pandemic. The adjustment of Australia’s Medicare policy later in 2020 to allow GPs to charge fees above the bulk billing rebate for telehealth consultations was well received, although this opportunity was given to GPs later than it was to other specialists14.
Rural practices may rely on discretionary billing (not wholly bulk billing) to maintain practice viability in locations where longer appointments are needed to manage clientele who travel long distances to access health care (potentially stacking several issues into one appointment). This aligns with evidence that rural patients have fewer GP appointments per year15. Further, in rural areas, patients are also more likely to have complex healthcare needs that must be coordinated between providers across a large geographic area16. This increases the administrative and referral burden that may need to be offset by fees charged. Despite research showing that bulk billing is more often used for patients with chronic diseases8, which are relatively prevalent in rural communities17, rural patients may have less access to appointments (due to fewer doctors and lower GP workforce stability), potentially disrupting this pattern15,18.
With this in mind, it has been positive to see that rural bulk billing levels were adjusted by the government in 2020 (50% higher rebate for three selected items in MMM2–7), but it is unclear whether these items align with the range of services that rural GPs deliver19. The recently released Recommendations of the Medicare Taskforce Review suggests that financial loadings within Medicare are not an appropriate or efficient mechanism to target rural access20, and financing options such as voluntary patient enrolment should be considered21. Voluntary patient enrolment is expected to give patients aged 70 years and older (50 years and older for Aboriginal and Torres Strait Islander people) who have chronic and complex conditions the option to enrol with a practice and nominate a regular GP, in return for a quarterly practice payment. This would circumvent a reliance on fee-for-service billing for complex patients, but the level of fee provided, and the doctor’s autonomy to set that fee to fit the viability of practising in their own context, may be relevant considerations based on the present study’s findings.
The present study found that larger practices are less likely to use bulk billing only policies, which aligns with existing evidence8. Small practices may have higher throughput of regular clients as would be supported by a bulk billing-only model. This may differ from larger practices where various GPs can offer more specialised services, charging out-of-pocket costs or using bulk billing selectively.
In multivariate state/territory analyses, it was found that GPs in the Northern Territory were more likely to bulk bill. This propensity toward GPs bulk billing8 is potentially related to higher proportions of Indigenous clientele22 with more morbidities and challenges affording medical care than non-Indigenous people17. The Northern Territory also has a unique primary care model that is largely a mix of Territory Health Services and Aboriginal Community Controlled Health Services, which promotes affordable care through bulk billing.
This study had a range of limitations. It was exploratory only, using convenient data sources that may not have been optimal for addressing the research aim. Available MBS data did not provide unit-level information on practices, patients or caseload. This information would have allowed more in-depth consideration around tailoring of GP bulk billing policies. Further, the GPSA survey relied on self-reported data with a 14% response rate, although this response rate is in line with other national surveys of doctors23. Finally, the study was not able to directly assess the impact of mandatory bulk billing policies on practices, only providing a point of reflection about potential impacts. It might be interesting for more research to delve into the issues around rurality and bulk billing, and to explore variation by the mix of corporate practices in different ruralities.
Conclusion
This study was relatively exploratory but sought to build contemporary evidence about which practices use patient co-payments and may therefore be negatively impacted by bulk billing only policies. It was identified that pivoting to mandatory bulk billing is likely to impact rural and larger practices, and those outside of the Northern Territory. Policies that allow for a range of billing arrangements may be important for practices to fit billings to their local context of care including services in rural areas, thereby supporting business viability and the availability of sustainable primary care services. This evidence could be used to stimulate further research on Australia’s Medicare policies, including how such policies might impact rural health care.
Competing interests
All authors were paid by GPSA, however they had full independence for producing and interpreting the data.
Acknowledgements
We acknowledge GPSA, which commissioned this research using funding from the Australian Government under the Australian General Practice Training Program. Authors received other research grants from the Australian College of Rural and Remote Medicine and the Royal Australian College of General Practitioners, outside the submitted work. We also acknowledge all of the GPs and practices who gave their valuable time to participate in the GPSA annual survey. We acknowledge Ms Carla Taylor from the GPSA team for copy-editing this manuscript.


