Introduction
Aboriginal and Torres Strait Islander peoples have a shorter life expectancy than that of non-Indigenous Australians1. It has been estimated that 80% of this disparity is due to chronic diseases that increase morbidity and shorten life2. In 2018, 65% of Aboriginal and Torres Strait Islander peoples were estimated to have at least one chronic health condition3.
On the North Coast of NSW, Aboriginal and Torres Strait Islander peoples have the highest rates of hospitalisations in the state for all health issues including chronic disease4. The higher prevalence of multiple chronic diseases is associated with poorer health outcomes, shorter life expectancy, and with complex medication regimens3,5. Low medication adherence rates in chronic disease are common among all population groups6. For the purpose of this study, medication adherence is defined as the extent to which a patient follows their medication regimen as determined by their doctors and pharmacist. An alternative term could be ‘concordance’7-9.
Personal management of medication regimens, complex or otherwise, and improvement of medication-taking behaviours may require various levels of support, education, engagement and barrier reduction from health services and/or pharmacists.
Dose administration aids (DAAs) are specific types of unit dose medication packaging, initially used in aged care facilities, and now also in the community, to assist with the safe provision of medications to patients. Many types of DAAs are available to patients; their aim is to improve patient-driven medication management. Devices include hard plastic packs (often known as dosette boxes) with sections for each day of the week, that are usually packed by the patient, or sometimes by a clinic nurse. Some DAAs consist of sachets or blister packs of tablets that can be packed by a machine or by a pharmacist10. All of these DAAs enable medication to be repacked from original manufacturers’ containers into a daily dosage system, where medication is split into morning, midday, evening and night-time doses, with the aim of supporting patients to take the right medications at the right times. The DAAs referred to in this study were mainly the pharmacist-packed blister packs.
Two programs currently provide subsidised DAAs to Aboriginal and Torres Strait Islander peoples. The Indigenous Team Care (ITC) program – established in 2009 originally as the Chronic Care and Supplementary Services program, funded through the Australian Government’s Indigenous Australians Health Program, and managed by Primary Health Networks – is responsible for a stream of funds allocated to supporting Aboriginal and Torres Strait Islander peoples with chronic disease by providing (1) dedicated care coordination for management of chronic disease and (2) supplementary service funds to pay for costs associated with specialist appointments, including transport to attend and provision of a specified list of medical aids, including DAAs.
Prior to 2021, the Quality Use of Medicine Maximised (QUMAX)11 program, funded through the Australian Government Department of Health, provided funds to Aboriginal Community Controlled Health Services (ACCHSs) to broker DAAs for patients with a chronic disease. This program aimed to support best use of medications, and facilitates relationships between the ACCHSs, patients and pharmacists. In 2021 the Pharmacy Guild negotiated for funds for DAAs to go directly to pharmacies rather than for ACCHSs to determine who provides the service with the patient.
The use of DAAs may improve medication management for some people, and therefore can facilitate positive health benefits for patients12,13. However, research regarding the experience and importance of the provision of DAAs to Aboriginal and Torres Strait Islander peoples in Australia appears to be scarce despite the potential of DAAs to assist with adherence and management of complex medication regimens. The literature review underpinning this study12 found that what is known about this subject is based predominantly on the perspectives of clinicians and pharmacists, with no published empirical data reporting Aboriginal and Torres Strait islander peoples’ lived experiences and preferences in relation to the use of DAAs.
It is important to evaluate government programs that subsidise DAAs and to understand the use and uptake of DAAs.
A goal of the study, and of this article, was to explore Aboriginal and Torres Strait Islander peoples’ lived experiences and preferences in relation to the use of DAAs. It is envisaged that the results be used to inform or support policy development, improvement and possible program redesign.
Methods
A mixed-methods approach was used that included quantitative and qualitative data collection from a questionnaire and a series of focus groups.
Study setting
The study took place with Aboriginal people living rurally on the North Coast of New South Wales (NSW), specifically the area from Tweed Heads in the north to Port Macquarie in the south. This area, encompassing the Bundjalung, Yeagl, Gumbayngirr and Dhungutti nations, is within two local health districts: the Mid North Coast NSW Local Health District and the Northern NSW Local Health District. According to the 2016 Census, these districts included 25 033 Aboriginal residents, accounting for 5% of the overall population in the region14, compared to the national average of 3% in 201615.
Consistent with the rest of Australia, the burden of chronic disease remains relatively high in the NSW North Coast Aboriginal population compared to the non-Indigenous population, with disproportionate rates of hospitalisation due to various conditions, including cardiovascular, respiratory and renal disease and diabetes1,16. In 2016–2017 the rate of hospitalisation of Aboriginal patients for respiratory diseases was 2.3 times higher than for non-Aboriginal patients, and the rate of hospitalisation for circulatory diseases was 2.1 times higher16. In 2016–2017, 18% of the dialysis hospitalisations in the region were for Aboriginal patients and in 2012 the hospitalisation rate for diabetes for Aboriginal patients was nearly four times the rate for non-Indigenous patients17.
Participant recruitment
Participants were recruited in two ways. First, patients who required DAAs through the ITC program were offered the opportunity to participate in the questionnaire. Only a small number of participants were recruited this way (n=10). Second, three focus groups were arranged with the support of local ACCHSs. Two of the three ACCHSs employed non-dispensing pharmacists, and they assisted with the recruitment of the participants by allowing the researchers’ attendance at existing group meetings, with the approval of the group. The pharmacists attended the focus groups but did not participate. Two of the focus groups took place at existing group/meetings, which were essentially regular social meetings, although sometimes a health promotion activity was undertaken.
Inclusion criteria were Aboriginal and/or Torres Strait Islander people who were prescribed multiple medications and obtained services via the ITC or QUMAX programs, ideally using DAAs, or who had used DAAs in the past or who were thinking of using DAAs. The exclusion criteria comprised non-Indigenous people, Aboriginal and/or Torres Strait Islander people who did not receive support through any of these programs and Aboriginal and/or Torres Strait Islander people who had not been prescribed multiple medications.
Questionnaire design
The questionnaire was designed based on the aims of the research study, with the support and guidance of senior researchers with questionnaire design experience. The questionnaire was then trialled with the Executive of the Regional Aboriginal Health Advisory Group, who then provided some advice and suggested minor language changes. The questionnaire was then taken to the wider community through the Bundjalung Elders Council and the Bugalwena Advisory Group for final comments and changes.
Sections in the questionnaire included demographic information (age, gender and location); questions about whether the individual had used DAAs in the past, whether they were currently using DAAs, whether they had used DAAs in the past but had stopped using them, and also whether they wanted to start using DAAs again. It also elicited information about participants’ medication-taking behaviours at the time of data collection, and whether this would change if financial subsidisation of DAAs was ceased due to funding changes.
Using Likert-type scales, participants were asked how they felt about their medications, the convenience of DAAs, whether DAAs supported taking their medication at the right times, how helpful the pharmacist packaging process was and whether they were given options regarding how their medications would be packaged. Two final questions related specifically to the effects of funding for the DAAs, and participants were offered an opportunity to make comments or provide additional notes. The frequency of medication requirements was established through a free-text option.
From the researcher’s personal knowledge and experience from working in ACCHs, it was known that pharmacists who pack patients’ medications in DAAs usually keep and manage patients’ prescriptions. One question related to the helpfulness of pharmacists managing scripts, and another to DAAs as a tool for managing medication-taking, both of which relate to the requirement of patients to attend the same pharmacy regularly to procure their medications/DAAs.
Focus groups
Focus groups began with most participants completing the questionnaire. The researcher then read and briefly collated the responses before the discussion began. The focus groups were guided by a core set of questions (developed by the researcher after analysing the initial 10 questionnaires), and follow-on questions dependent on responses from each group’s answers to the questionnaire at the start of the focus group. This approach stimulated contributions throughout the discussion, providing support for the building of a pragmatic narrative to answer the key questions.
Focus groups provided an opportunity to discuss individual and group responses to the questionnaires and expand on individual answers to build a sense of group experience as well as individual experience.
Analysis
For this study, three stages of descriptive deductive analysis were used to answer the study questions. They occurred:
- after the initial 10 questionnaires were collected
- after completion of questionnaires at the beginning of each focus group, when responses were summarised, and frequencies noted by the researcher who subsequently conducted group discussions informed by these questions and answers
- after the collation of all the data from questionnaires and all focus group responses, as a summative analysis.
The data collected by questionnaire at the start of each focus group were subsequently aggregated with other data collected through the questionnaires and focus group data. Then audio-recordings from the focus groups were professionally transcribed and checked for accuracy by the researcher. Responses from all questionnaires were aggregated into a single table, and notes and responses to questions raised in the focus groups were added to this table in corresponding sections to analyse and explain questionnaire responses. In this way, examples from focus groups added context and nuance to aggregated questionnaire responses.
Using a combination of questionnaire responses, both qualitative (from the open comments) and quantitative, through focus group discussions, the researchers began to build descriptions of the experiences of Aboriginal peoples on the North Coast of NSW with DAAs and the programs that provide them.
Ethics approval
The first author is an Aboriginal researcher, bound not only by research ethics, but also by community protocols, because the researcher is a community member. Consultation occurred with Elders from the community from the beginning of the study. Contact was made with two Aboriginal health advisory groups, 16 community members and Elders, and five ACCHSs in the region. The initial study proposal was met with positive responses from all these groups, and letters of support were provided by communities and organisations for the ethics application. The ACCHSs supported the study and recruitment of patients for the focus groups throughout.
Ethical approval was obtained from the New South Wales Aboriginal Health and Medical Research Council’s Ethics Board in 2014 (HREC Approval number 1050/14).
All participants gave informed written permission for their involvement in the study.
Results
Data were collected between 2015 and 2019. This time lag was due to accessibility of times that suited the ACCHSs and community, and the work commitments of the researcher undertaking the study part time. Of the 30 participants in this study, 10 completed the questionnaire only, 16 completed the questionnaire and attended a focus group, 4 only attended a focus group without completing a questionnaire. The focus groups comprised 12, 4 and 2 participants, and total number of questionnaires completed was 26 (Table 1).
Reasons for not completing a questionnaire were related to literacy, or preference by these participants not to participate in the questionnaire part of the study.
Each focus group contained a mix of genders and ages, with members known to each other as community members but also, in two of the focus groups, as Elders who met regularly and were comfortable to talk as a group. The majority of the participants in the third group knew each other well and were considered Elders in their community. This resulted in open conversation, with no obvious shame or discomfort from any of the participants. Two of the three focus groups were recorded and transcribed. One member in the third focus group declined audio-recording, and therefore notes were made of the discussion and responses to the questions by the researcher.
It is important to note that these respondent figures do not include two Elders who attended one of the focus groups, with verbal permission and agreement of the participants for their attendance. They did not want to actively participate in the study but permitted some comments they made to be noted.
Table 1: Numbers of participants for focus groups and questionnaires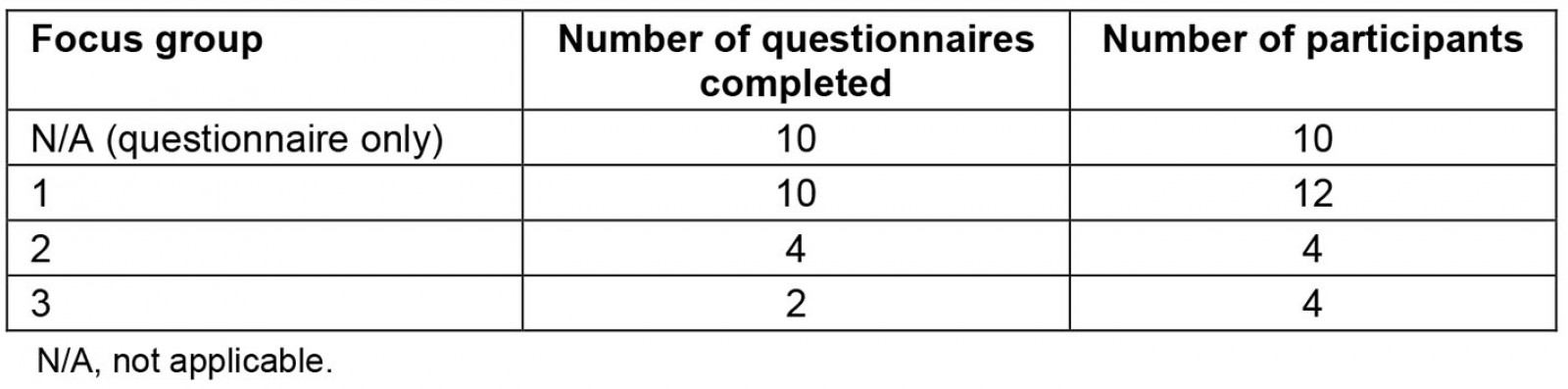
Participant demographics
Participants were from six geographical areas across the region that are incorporated in the North Coast Primary Health Network. This network crosses the Mid North and North Coast health districts of NSW (Fig1). Participants were ACCHS patients taking multiple medicines, and the majority were DAA users.
Ages ranged from 44 to 79 years (mean 61.5 years). There were 14 men and 16 women, and all the participants lived in the area between Tweed Heads and Port Macquarie and received health services from ACCHSs.
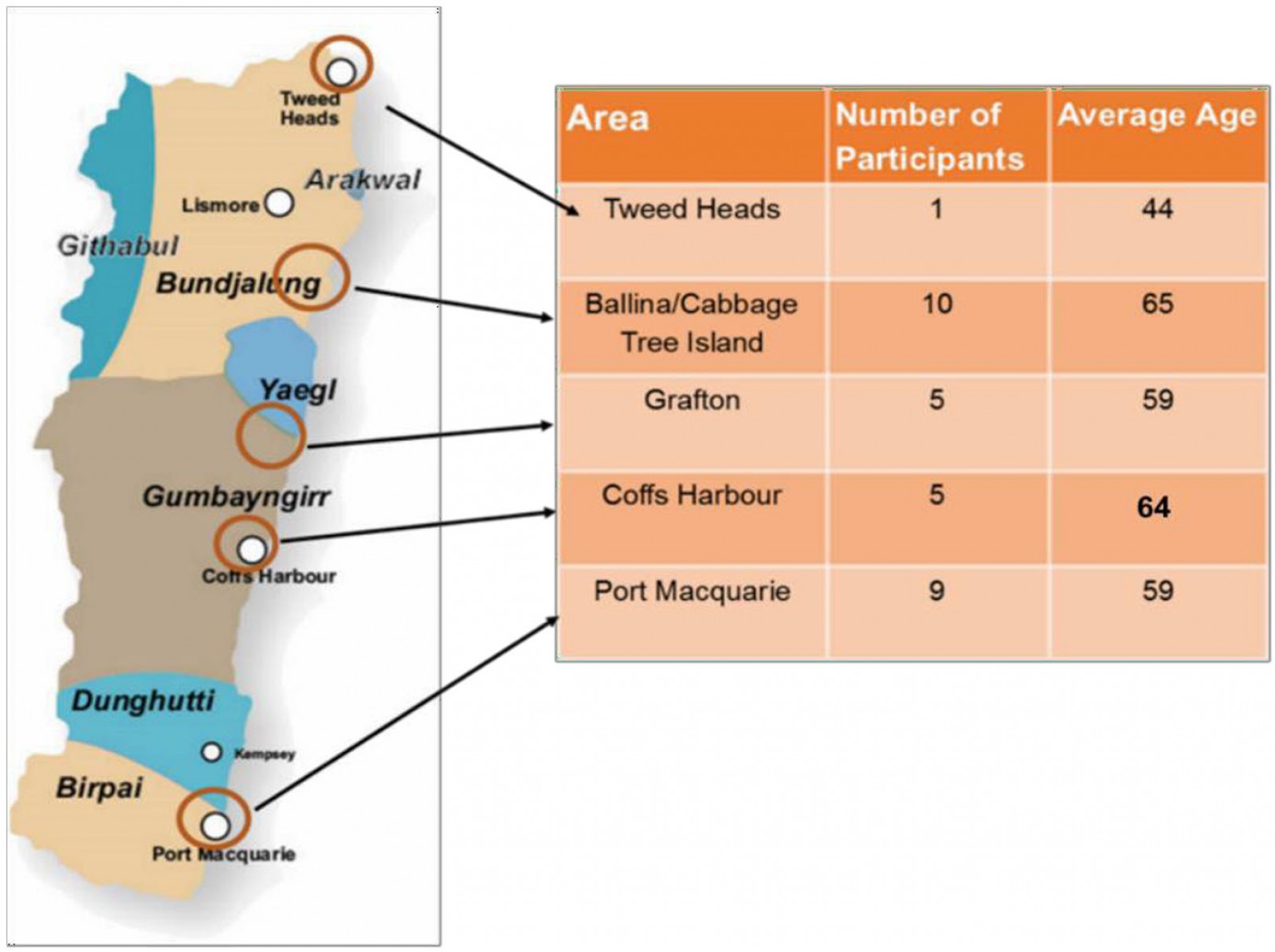 Figure 1: Location, number and average age of participants in the study.
Figure 1: Location, number and average age of participants in the study.
Medications and how participants felt about taking them
Participants took multiple medications between one and six times each day. Participants also included injectable insulin in their lists of medications, with some taking insulin up to four times a day. The numbers of medications and individual tablets ranged from 9 to 23 tablets a day, with one participant taking 10 tablets and four insulin injections over 24 hours.
During the focus groups, conversations were prompted by questions such as 'Do you know what your medications are for?' This led to participants frequently listing their medications by name or colour and describing what conditions they treated and how. Only two focus group participants were unable to state the purpose of all of their medications.
The majority of questionnaire respondents (21/26) reported that they 'liked taking' their medications. Only two participants completing questionnaires said they 'strongly disliked' taking their medicines. There were three non-respondents to this question.
Use of dose administration aids
Twenty-six of the 30 respondents currently used DAAs. Most (n=25) had been using DAAs for more than 1 year, with only one participant relatively new to using DAAs (less than 1 year). Four participants were not currently using DAAs.
Nineteen participants responded to the questions in the survey regarding the helpfulness of DAAs in taking medications on time. Of these, 17 responded that they were very helpful, and two said they were somewhat helpful.
Three-quarters of all the participants found that access to and delivery of DAAs was convenient overall. Some participants’ DAAs were delivered to them occasionally if they were unable to get to the pharmacy, while other participants were happy to pick up their packs. A minority (n=3) of participants who completed the questionnaire found picking up the packs from the pharmacy was difficult, while two reported that they sometimes did not pick them up at all, meaning that, periodically, they went without their medications.
One of the two Elders who wanted to be in the room at the time of the focus group and gave permission for their comments to be used commented very strongly about his dislike for DAAs. 'I don’t like them because they waste medications.' He then went on to explain: 'My sister had them and when she died, I had all these packs of tablets. I didn’t know what to do with them.' For this reason, he had chosen to not use DAAs because he didn’t want to have to worry about his family cleaning them up after he passed on.
Experiences of missed medications
Of the 20 participants who attended the focus groups, 45% (n=9) missed their medications regularly. They were asked why they might not have taken their medications. Several practical barriers emerged: if participants were late or rushed, they would forget to take their medication; and, if travelling, taking all medications, including injectable insulin, could prove difficult. One participant commented:
When I am out or travelling, we can’t stop. I must take my injection every four hours. It can be hard on the train to take my medications, both injectable and tablets. So sometimes when travelling I don’t take them.
Some participants in the focus groups also felt that they could not mix medications with alcohol and did not take them if drinking. As one focus group participant noted:
If I have a few beers, then I don’t take my tablets. This might be for a night or two. Not that often but I don’t take my tablets and drink together.
One focus group participant stated that if tablets weren’t taken it was only by mistake, it wasn’t a choice and that they would never double-up on medications if they forgot in order to catch up:
Oh no, just if I’m busy. Oh damn! Oh well, I’m not going to die because I haven’t taken one tablet. But I don’t double on it, never ever.
Participants who did take their medications regularly noted that using the DAAs made this easier because the days were listed and numbered so they couldn’t forget.
Use of personal reminder systems
It was interesting to note in the focus group discussions that the people who did not use DAAs (n=4) had developed very specific reminder systems of their own. In order to remember a complex regimen of medications, two participants had developed their own systems before being prescribed a DAA and didn’t see that it was necessary to change. The system of one of these participants involved managing tablets in bottles and blister packs to ensure tablets were taken morning and night. Tablets in bottles were sorted and placed in a jar in advance, with the lid on and placed next to the tablets in blister packs:
In the morning when I take a tablet, I use the silver paper flap left on the blister and stand it up, straight in the air. When I take my tablet again at night, I flatten them down, so when I wake up the next day, I know I have taken my tablets if the flaps are down. If I have forgotten them, I will know because the flap [of silver paper] is still standing. For medications in the jar, I will turn the jar upside down, when I take it [medications] in the morning and down it with a cup of tea. And then I’ll just turn the jar upside down. Late in the afternoon when I finish taking the tablets, I’ll turn it back up so I’m ready for the next morning. Sometimes I get a little tricked up, with some medication, if I forget to flatten the tabs, but I can check the other way [jar] and it tells me if I have done it.
Pharmacist role and relationship
In response to the questionnaire regarding how helpful it was to have the pharmacist manage and retain the prescriptions within the pharmacy, the majority (n=21) reported that it was very helpful, two replied it was somewhat helpful, and one felt it was not helpful. Two people did not respond to this question in the questionnaire.
Focus groups included discussion of relationships that patients had with their pharmacists, how people interacted with their pharmacists and whether they thought this had improved since their use of the DAAs. The general feeling from participants was that they had good relationships with their pharmacists due to regularly attending the pharmacy to pick the packs up, providing an opportunity to talk about their medications.
Participants in two of the groups had a non-dispensing pharmacist located in their ACCHSs and 12 out of 14 of these participants said they regularly talked to their pharmacists. Both ACCHSs with pharmacists had regular group sessions every 4–6 weeks, and these were specifically designed to allow the pharmacist to spend time with these clients and discuss medications. They also noted that, because the pharmacist was in the service, they could talk to the pharmacist any time they needed to.
The participants in the third focus group all used the ACCHS, but this service did not have a pharmacist on staff. These participants all used specific pharmacies for their medications. One of the participants who saw their pharmacist in the community pharmacy said, ‘They sit me down and explain how to take medications’. One participant provided the researcher with a copy of the list of medications provided by the pharmacist, which was carried in case of emergency.
Only one participant in a focus group had not heard that the pharmacist could assist with medication information. This participant said that, if advice on medications was needed, it would be sought from their doctor.
Others involved in care
In the focus groups, participants were asked who else was involved with their care. The question gave rise to various responses, including from one person whose son assisted her, but the responses were usually that they had little help, and often they were also responsible for other people. ‘I help Mum and she helps me’ and ‘I also have to keep an eye on my husband’s medications’.
Financial considerations for participants
Most of the participants either did not know or did not answer the question about which program funded their DAAs (Fig2). The researcher was aware that three participants had their DAAs funded by the QUMAX in full or a briefer version program, and 11 participants had their DAAs funded by the Primary Health Care Network program. One participant was a Department of Veteran Affairs card holder and was entitled to medications at no cost.
This high rate of non-response made it hard to make any determinations in terms of the programs that provided DAAs to participants (Fig2). Although most people did not know how their DAA program was being funded, they did know their health services had arranged for DAAs to be supplied to them by the local pharmacy.
There were 20 responses to the question within the questionnaire ‘Would you keep up with DAAs if the funds were no longer available to pay for the DAA packaging service?’ Eleven participants answered ‘no’, one participant was unsure whether the cost would be prohibitive, and eight said they would continue to purchase their DAAs because they found them useful for taking their medications. Six participants did not respond to this question.
The focus groups provided an opportunity to discuss the issue of cost further. There were various discussions in all the groups about not being able to afford medications or DAA devices if the funding changed or was removed. When asked if they would continue to use DAAs if the funding ceased, one participant replied, ‘People are educated with their tablets … removal of the supports would mean they would be less likely to take or even purchase their medications.’
One participant in a focus group said, ‘How different things are now that the funding is around. Particularly the Aboriginal Medical Service where before people would get their tablets because they couldn’t afford them. Then QUMAX and the scripts came in and made a big difference. If funding was removed a lot of Aboriginal people would stop taking their tablets.’
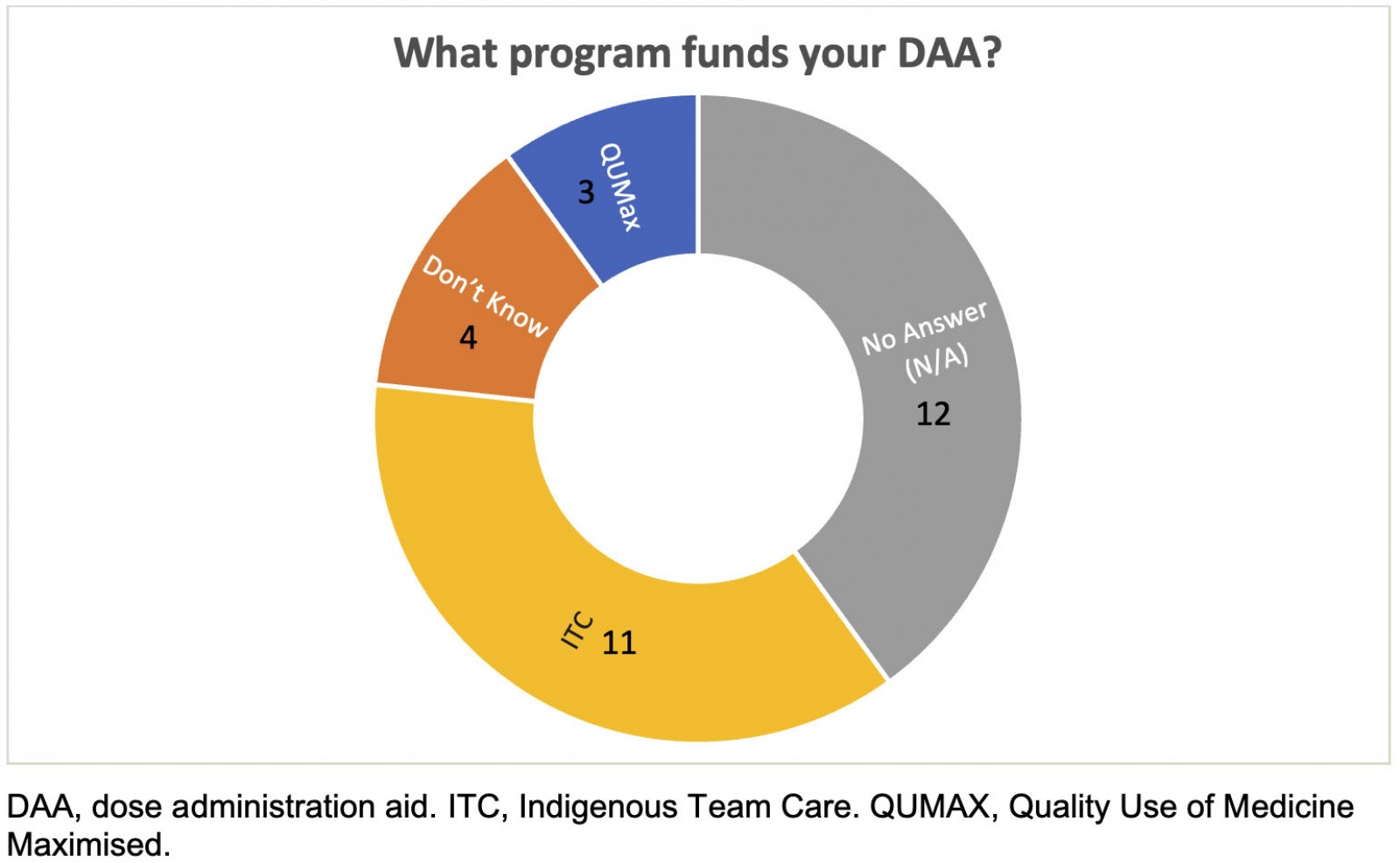 Figure 2: Participants’ knowledge of the program that funds their dose administration aids.
Figure 2: Participants’ knowledge of the program that funds their dose administration aids.
Discussion
This study sought to better understand the experience of Aboriginal people using DAAs, how effective the provision of them was, and whether DAAs supported positive medication-taking behaviours. The strengths of combining qualitative and quantitative data, even in a small study, have resulted in one of the few empirical studies exploring complex medication behaviours in a rurally distributed group of Aboriginal people.
The majority of participants (n=28) were aware of the purpose of DAAs and understood what their medicines were for. This contrasts with the findings of previous studies that many Aboriginal people found managing medicines difficult and confusing9,18,19. It does confirm that mechanisms such as picking up DAAs or, as Swain and Barclay identified, home medication reviews increase interactions between pharmacists and their clients, which increase opportunities for education20.
The disparity between clients’ perceptions of medication adherence and actual behaviours is an important finding of this study. Participants had a good understanding of the importance of medication-taking even though almost half semi-regularly missed taking their medications. Participants’ reasoning behind not taking medications at certain times made sense to them. Most of the reasons for not taking one or two sets of medications in the previous weeks were decisions the participants made, rather than forgetfulness.
While numerous studies explore barriers and facilitators to medication adherence and interventions to improve adherence21-24, there is little literature on patient perceptions of what constitutes medication non-adherence. There is also a scarcity of data available to help understand current medication-taking rates within Aboriginal populations in Australia25.
Previous studies have identified the value of strong patient–pharmacist relationships18,20,26. Some of the nuances of the relationships between participants and pharmacists, and the important role of pharmacists, became clear throughout the course of this study. Of the 20 participants who attended the focus groups, 14 spent regular time in programs and meetings where pharmacists were in attendance. Participants in all the focus groups noted they had ongoing relationships with a regular pharmacist. These good relationships may explain participant knowledge and understanding of their medications, which was evident in the focus groups and ran counter to findings in the literature. Participants seemed more confident in their medication-taking and their interactions with the pharmacist than the literature previously indicated. This finding was also reported as an outcome in Swain and Barclay’s research, which examined home medication reviews18,20.
Overall, the participants in the present study reported that they found DAAs a positive tool that assisted accurate and regular medication-taking. Most participants confirmed that DAAs helped them to manage their often complex medication regimens. A few limitations of DAAs were reported during the focus groups and these were consistent with the literature, which described the inability to package all medicines in a DAA13. The participants in this study reported that DAA-packaged medications were bulky and not ‘complete’ as a number of medications such as insulin and inhalers were external to DAAs. The bulkiness and quantity of medicines were especially inconvenient when participants were travelling. The need to collect DAAs from the pharmacy on a weekly or fortnightly basis was also problematic for some participants. The literature also discussed wastage of medications when automatic dispensing occurred and patients failed to collect their medications11,13,25.
The financial subsidisation of DAAs was very important to participants. Numerous programs fund DAAs, but understandably there is little awareness by participants about which programs their primary healthcare clinicians and pharmacists are accessing for this funding. Costs of medications were reported as potential barriers by participants to regular medication-taking, reflecting financial barriers identified in other studies2,27. Affordability of DAAs and medicines was important to all focus group participants, particularly for those who took a number of different medications each day. Participants stated that, if funding subsidies were to be removed, they would be unable to afford DAAs.
These findings relating to financial burden highlight the importance of policy and programs that mitigate these costs.
The current programs, while confusing in terms of how they are delivered at an organisational level, were seen by participants to be working well. The complexity of delivering multiple DAA-subsidised programs appears overly complicated. The ACCHSs provide subsidy through the QUMAX program, the Primary Health Networks administer the subsidisation through the ICT program and pharmacists receive some funding through Community Pharmacy programs. Further analysis is needed as to whether streamlining of these federally funded programs would enable more Aboriginal and Torres Strait Islander peoples to receive DAAs and medication support services.
Understanding the various barriers that can affect a patient’s adherence to medications provides important information when designing policy supports and programs to improve this process of successfully taking medicines, particularly in populations such as these with complex and multiple medications required and prescribed. It could be reasoned that the relevant policy initiatives and programs themselves – QUMAX and the ITC through the Primary Health Networks – have played a key role related to these findings. These programs are designed to reduce barriers to accessing medications and DAAs, and to increase occasions and quality of pharmacy services provided to Aboriginal and Torres Strait Islander peoples.
Strengths and limitations
The author acknowledges some limitations with the study. It is important to note that all participants in the focus groups were ACCHS patients and didn’t use mainstream general practice, it would be interesting to identify if there was a difference in the level of access to funded DAAs compared to those who do use ACCHS services. Further research is needed to quantify how many Aboriginal people on the North Coast of NSW use DAAs and to further explore their perceptions of medications and how DDAs support their medication-taking behaviours.
Despite the small sample size, the findings of this study are useful, adding to the literature on this topic and improving understanding of the value and importance placed on DAAs and medicines by Aboriginal patients.
Conclusion
‘Poor medication adherence’ is a phrase used often in relation to Aboriginal patients26,28. Given the complexity and burden of the medication requirements for many in the study, the level of attention the participants gave to their regimens, and their understanding of the purpose of each medication, suggests that the opposite is true. In fact, the participants who contributed to this study worked hard to adhere to their medication regimens the majority of the time and understood their medications. DAAs were seen as very important tools to assist medication adherence.
More extensive qualitative studies of the patient experience, as well as longitudinal studies tracking the results of improved medication adherence to the disease process as a result of DAA use, would add to understanding of attitudes, knowledge and behaviours related to medication-taking for Aboriginal and Torres Strait Islander peoples across Australia. Given that DAAs are available to wider populations, this study also supports the use of DAAs generally for assisting with medication-taking behaviours.
Acknowledgements
To Dr Jenn Johnson, Associate Professor Megan Passey and Dr Larisa Barnes – thank you. Thank you for all your support, help, advice, critical appraisal, reading, teaching and discussions.
References
You might also be interested in:
2006 - SEAM - improving the quality of palliative care in regional Toowoomba, Australia: lessons learned



