Introduction
The geographic maldistribution of physicians is a serious social problem around the world1,2. An increasing amount of evidence suggests that increasing the number of primary care specialists will help to improve the urban–rural gap in physician supply3. Compared with other medical specialists, primary care specialists or family physicians tend to have a more equitable distribution between urban and rural areas4. However, it is unclear whether this pattern of geographic distribution of family physicians is similar among different countries. Countries such as the USA, where the specialty of family medicine is mature, or countries in which primary care is an established academic discipline and is recognized as an important part of healthcare system, and produce a sufficient number of certified family physicians, may have a different geographic distribution of family physicians from countries in which family medicine is still emerging such as Japan.
Traditionally, Japan did not have a board certification system for primary care physicians. Domain-specific specialists, after finishing a career in a hospital, were and still are expected to provide primary care in a clinic as their second career. There was no formal retraining system for such ex-specialist primary care physicians. In 2009, the Japanese Primary Care Association (JPCA) started a board certification system for family physicians who completed a 3-year family medicine (katei-iryo) training program, and the number of certified family physicians has gradually increased5. As a part of recent reforms in specialty certification, the Japanese Medical Specialty Board (JMSB), the only formal and cross-discipline specialty board independent of each medical specialty body, referenced the content of JPCA family medicine training, and in 2021 started a new certification for general practice (sougou-shinryo) as one of 19 basic specialty areas. Beginning from 2021, the JMSB certification took the place of the JPCA certification. This reform is expected to dramatically increase the number of family physicians/general practitioners. However, the history of family medicine in Japan is much shorter than that in other countries. The percentage of family physicians compared to all physicians is less than 1%5. Japan is still excluded from the ‘generalist medical practitioners’ data in OECD Health Data due to, until recently, the lack of a generalist producing scheme6. As such, Japan is a society where family medicine is still immature as a specialty, which is quite unusual for a developed country.
In the USA, in contrast, the field of family medicine is more mature. The professional body for family physicians, the American Academy of Family Physicians, was founded in 1947, and family medicine was recognized as a formal specialty in clinical medicine in 1969. At this time, these physicians were not valued and were not produced specifically. Also, they were relegated to rural areas. However, the USA already has many board-certified family physicians. In 2017, 12.6% of medical school graduates entered a family medicine training program, and over the past decade the number of the residents has increased7. Thus, in the USA, family medicine is accepted as a part of the healthcare system.
This article reports on a pilot study to test the authors’ hypothesis that the geographic distribution of family physicians is associated with the maturity of family medicine in society. To fully prove the hypothesis, studies are required that compare various countries with various degrees of family medicine maturity, and as the first trial with an international comparison, Japan and the USA were chosen for this study. Japan and the USA are suitable for such a comparison for four reasons. First, there is a remarkable difference in the maturity of family medicine between the two countries, while both countries are developed countries in which area-based physician number data is publicly available. Second, in these two countries the geographic allocation of physicians is for the most part not regulated by the government as is done in some European countries. In the USA, there are some initiatives to recruit and retain physicians in rural areas implemented by the federal and state governments such as return-of-service scholarship or loan forgiveness programs8,9. Additionally, the National Health Service Corps (NHSC) managed by the US federal government is one of the largest such financial incentive programs in the USA, but the number of NHSC-supported physicians is small relative to the total physicians in the USA, and their impact on the overall nationwide distribution of physicians is limited10. The third reason is that in both countries a major part of the healthcare system is privately operated and owned. The medical practice of physicians in both countries is a personal business, or as employment in a for-profit private or semi-private hospital. In such a society, unlike in societies whose healthcare system is dominated by publicly owned medical institutions, the distribution of physicians is largely driven by the market11. Thus, the distribution in both countries can be interpreted as under the same dynamics, which is different from the government-led physician distribution in some European countries and Canada. Fourth, the Japanese healthcare system was modeled on that of the USA. After the Second World War, under US control, the old Japanese healthcare system was substantially remodeled based on the US system. In this historical context, the USA is a preferred counterpart for this comparative study. By comparing Japan and the USA, it is possible to assess the relationship between the maturity of family medicine and the geographic distribution of family physicians while excluding the impact of the intervention by the public sector on the distribution.
The purpose of this study is to investigate whether the geographic distribution of family physicians in Japan is equitable between rural and urban areas. Family physicians should be distributed not only to urban areas but also to rural areas because family medicine improves health indicators for all community residents, and contributes to patient satisfaction and lower health care costs12. The authors evaluated the geographic distribution of family physicians and other major clinical specialists in Japan, and compare it with distribution in the USA. Also, it is hypothesized that family physicians in Japan are more concentrated in rural areas than urban areas and the distribution is quite different from that in the USA. In addition, the distribution of all physicians in Japan is simulated, assuming that the proportion of family physicians among all the physicians increases to the level of that in the USA.
Methods
Study setting
This is a cross-sectional comparative study using publicly available online databases including all municipalities in Japan, and all USA counties and the District of Columbia.
Data of physicians in Japan
An online database was collected of JPCA-certified family physicians in 2018 who gave permission to the JPCA office to make their information available online13. The data disclosed each physician's name, workplace (municipality and medical institution) and area of special interest. The number of physicians in other specialties who worked as clinicians in a medical institution and were board-certified by the Japanese Society of Internal Medicine, Japan Pediatric Society, Japan Surgical Society, and Japan Society of Obstetrics and Gynecology was collected from the online database of the Survey of Physicians, Dentists and Pharmacists 2018 compiled by the Ministry of Health, Labour and Welfare14.
Data on municipalities in Japan
Japan is divided into three administrative levels: national, prefectural and municipal. The number of municipalities (cities, towns and villages) was 1741, and data were collected on 1737. Population and population density in 2015 were collected for each municipality from an online database for a population census compiled by the Ministry of Internal Affairs and Communications15. The rurality of each municipality was defined by its population density. The population density of a municipality was calculated by dividing the population (number of residents) by land area (square kilometers). Municipalities were divided into quintiles (fifths of a set) according to population density so that the number of municipalities in each group was 20% of all the municipalities (quintile 1 ≤43.4 people/km2, quintile 2 ≤140.6 people/km2, quintile 3 ≤403.9 people/km2, quintile 4 ≤1650.4 people/km2, quintile 5 ≤22 380.2 people/km2). The municipality boundary data was obtained from the National Spatial Planning and Regional Policy Bureau of the Ministry of Land of Japan.
Data on physicians and counties in the USA
The number of physicians and population density in US counties were collected from the Area Resource File published by the US Health Resources and Services Administration16. In the database, information on 3221 of the 3230 counties was available. Data on the number of physicians in 2017 was used for the analysis. The number of physicians was the sum of Doctor of Medicine (MD) and Doctor of Osteopathic Medicine (DO) who provided active patient care and were non-federal doctors. Data on the number of board-certified family physicians and that of other board-certified physicians (general internists, pediatricians, general surgeons, and obstetricians and gynecologists) were used for the analysis. Population information in 2018 and area information in 2010 for each county contained in the database were also used for the analysis. To evaluate rurality, as in Japan, counties were divided into quintiles according to population density (quintile 1 ≤4.6 people/km2, quintile 2 ≤11.9 people/km2, quintile 3 ≤24.3 people/km2, quintile 4 ≤67.4 people/km2, quintile 5 ≤18 721.1 people/km2). Census boundary data were obtained from the USA Census Bureau TIGER/Line Shapefiles.
Simulation analysis
The geographic distribution of all the physicians in Japan was simulated assuming that the proportion of family physicians among all the physicians in Japan increased to that in the USA. This analysis was based on the following assumptions: the number of family physicians increased and the number of the other physicians decreased, resulting in no change in the total number of physicians; the distribution patterns of family physicians and the other physicians remained constant.
The proportion of family physicians in Japan was 0.16% (519 of 320 084), while the proportion of family physicians in the USA was 11.8% (105 999 of 899 234). To increase the Japanese proportion to the level of the USA (11.8%), the number of family physicians in Japan was needed to increase from 519 to 37 730, which is a 72.6-fold expansion. According to this change, the number of other specialists was needed to decrease by 0.88 times (from 319 565 to 282 354), resulting in the total number of physicians holding steady. Family physicians and other physicians were multiplied as such, while maintaining the same distribution of each group of physicians among quintiles. The total number of physicians per population in each quintile group of a population density was then calculated and compared to before and after the simulation.
The distribution of family physicians can be influenced by factors that change as the number of family physicians increases. For example, the size of the population accustomed to family physicians, the age distribution of family physicians and the amount of money family physicians can save to start their private practice could change as this number increases. To simplify the calculation, this simulation does not consider these factors.
Statistical analysis
A χ2 test was used to compare the distribution of ordinal variables among five groups of areas in both countries17. Residual analysis was used to compare the real value of the number of family physicians per unit population and the expected value derived from the distribution of all family physicians in both countries.
All statistical analyses were performed using Microsoft Excel and STATA/SE v15 (StataCorp; http://www.stata.com). Data for four (0.2%) municipalities and nine (0.3%) counties were excluded because of a lack of information about the number of physicians or population density. A p-value of 0.05 (two-sided test) was considered statistically significant.
Ethics approval
This study required no ethical approval because all the data used for the analyses was publicly available online.
Results
At the time of study, the national population in Japan was 127 094 745 and that of the USA was 330 530 359. The mean population of municipalities in Japan was 73 169 and that of counties in the USA was 102 180. The mean area size of municipalities in Japan was 214 km2 and that of counties in the USA was 3057 km2. There were 320 084 physicians in Japan and 899 244 in the USA There were 672 family physicians in Japan and 105 999 in the USA. Data for 519 of the 672 (77.2%) family physicians in Japan were available online, while data were available for all family physicians (100%) in the USA. Figure 1 shows the number of family physicians per unit population in each quintile of population density in Japan and in the USA. The concentration of family physicians in Japan was relatively low in densely populated coastal areas. In less densely populated inland mountain areas, the concentration of family physicians was relatively high. In contrast, family physicians in the USA did not concentrate in certain geographic locations.
The distribution also appears in Figure 2, which depicts the number of family physicians per unit population in each quintile of population density. The distribution of family physicians in Japan shifted substantially to quintile 1 (the lowest population density) municipalities (Fig2A). In contrast, family physicians were uniformly distributed across quintiles in the USA (Fig2B). Chi-square tests showed that the distribution of Japanese family physicians among the quintile groups differed significantly from that of American family physicians (p<0.001). The residual analysis showed that the number of family physicians in quintile 1 in Japan (117 per 10 000 000) was significantly higher than the number expected from the distribution of all family physicians (total of Japanese and US family physicians) (73.5 per 10 000 000) (p<0.001). The number of family physicians in quintile 5 in Japan (31 per 10 000 000) was significantly lower than the number expected from the distribution of all family physicians (56.8 per 10 000 000) (p<0.001).
Figure 3 shows the distribution of family physicians and other specialists per 100 000 population classified by population density quintile in Japan and the USA. Japanese generalists include both general internists and family physicians in this figure because the number of family physicians in Japan was very small and, historically, general internists have substituted as family physicians in most communities. The distribution of general internists plus family physicians shifted markedly to urban areas in Japan, while that of family physicians in the USA shifted to rural areas. The number of family physicians per 100 000 in the USA was approximately four times as large as that of general internists plus family physicians in Japan in the lowest population density areas. Other specialists in both Japan and the USA tended to be biased toward urban areas.
In the simulation analysis, assuming an increase in the number of family physicians in Japan, the geographic maldistribution of all physicians in Japan would improve if the number of family physicians increased from its current level (0.16%) to the US level (72.6 times greater: 11.8%) (Fig4). For example, the number of physicians in quintile 1 increased by 1.64 times from 2558 to 4199 if the number of family physicians was increased to the US level.
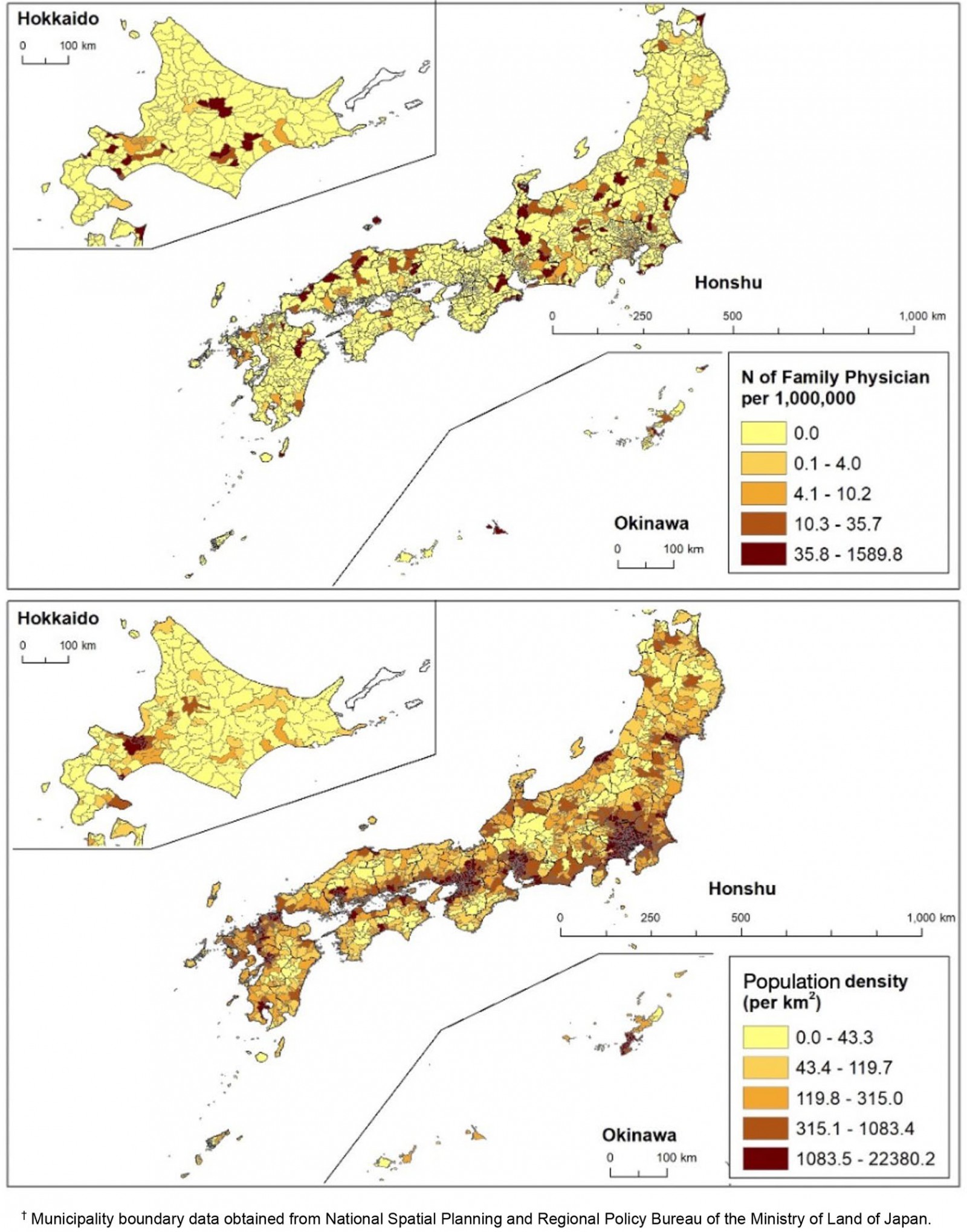 Figure 1A: Japan. Upper: Number of family physicians per 1 000 000 population each municipality. Lower: Population density in each municipality.†
Figure 1A: Japan. Upper: Number of family physicians per 1 000 000 population each municipality. Lower: Population density in each municipality.†
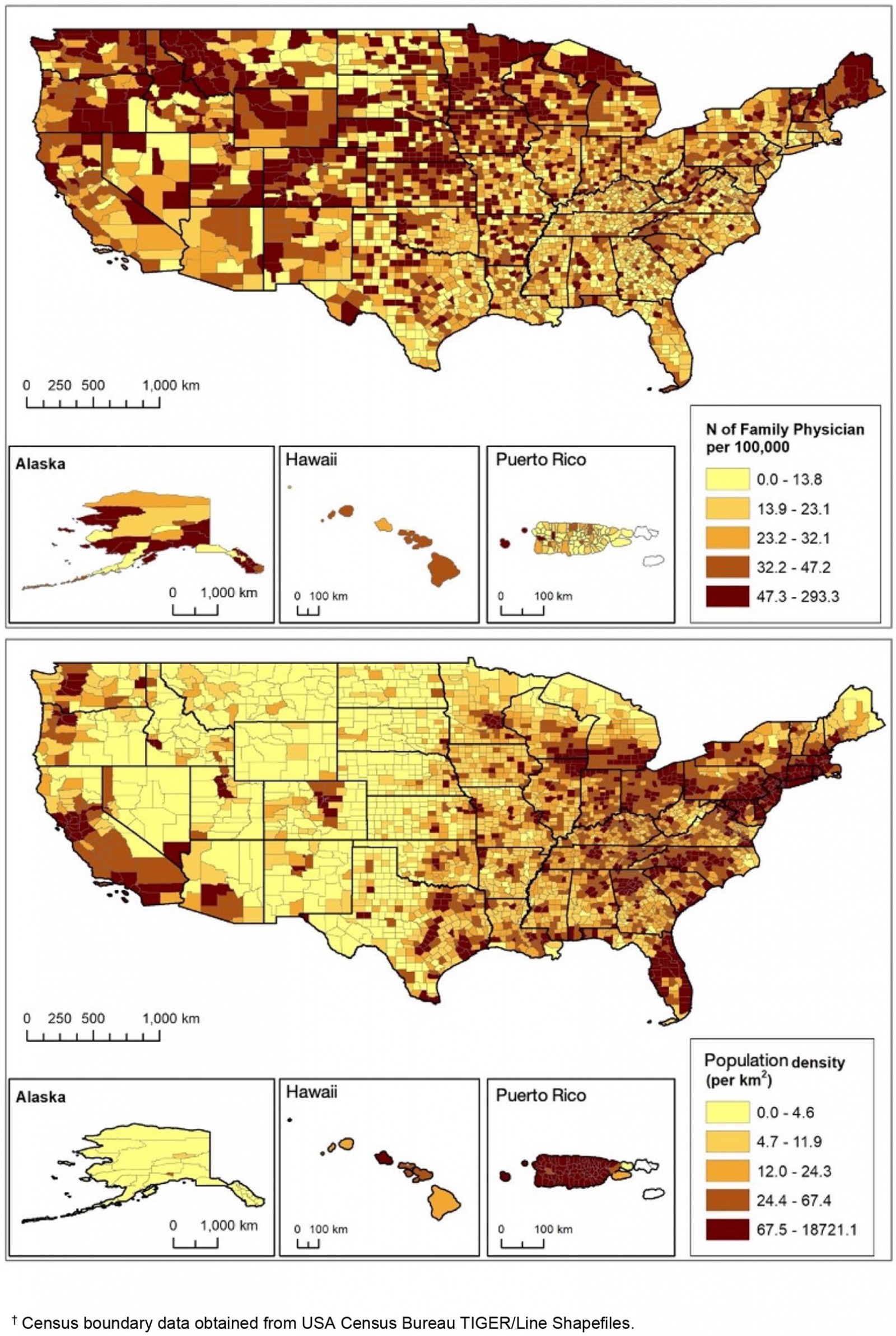 Figure 1B: USA. Upper: Number of family physicians per 100 000 population in each county. Lower: population density in each county. †
Figure 1B: USA. Upper: Number of family physicians per 100 000 population in each county. Lower: population density in each county. †
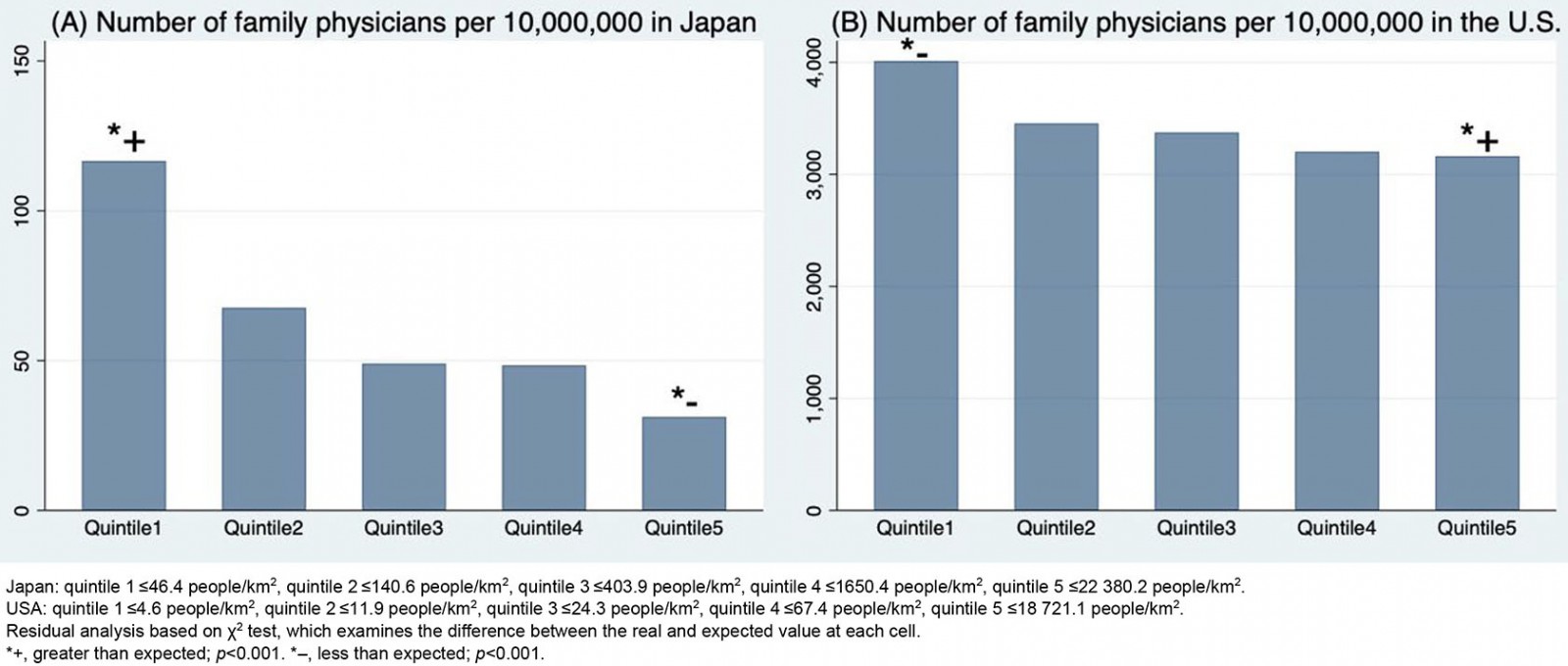 Figure 2: Number of family physicians per 10 000 000 population in each quintile group of municipalities (A)/counties (B) sorted according to population density.
Figure 2: Number of family physicians per 10 000 000 population in each quintile group of municipalities (A)/counties (B) sorted according to population density.
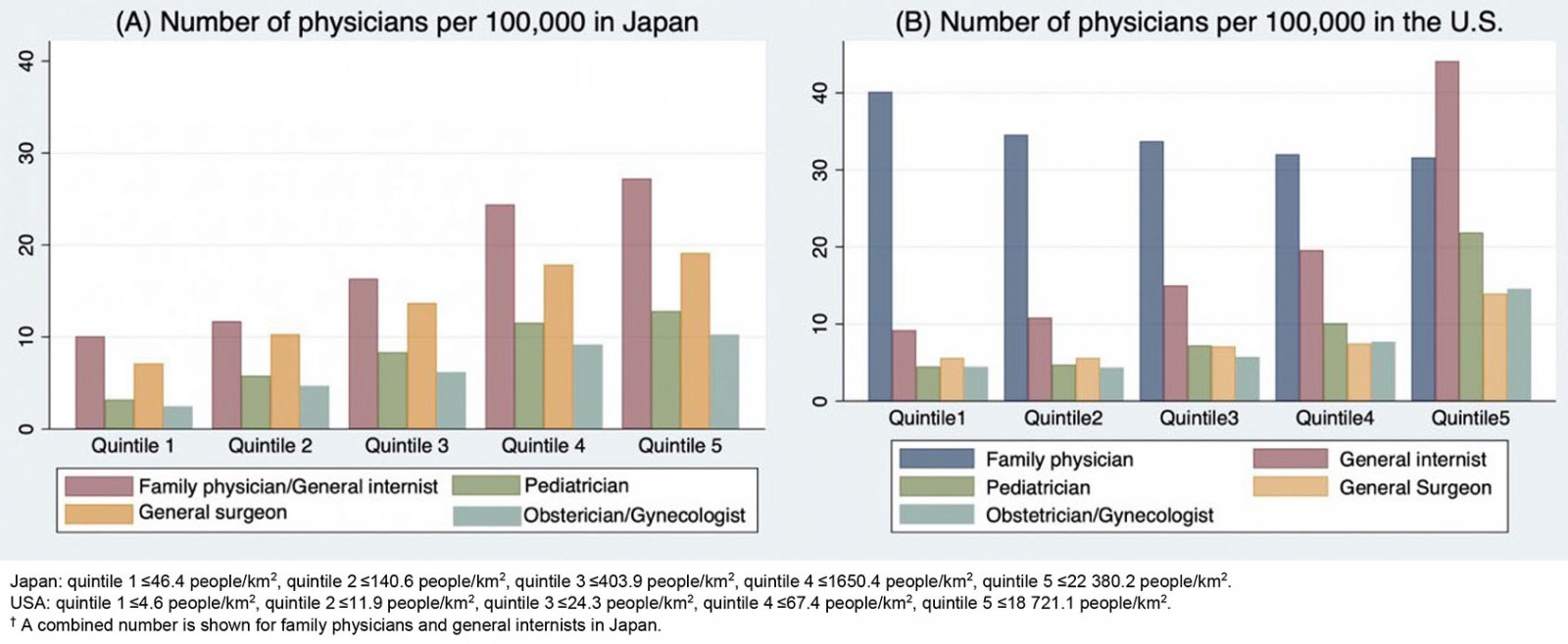 Figure 3: Number of other specialists per 100 000 population in each quintile group of municipalities (A)/counties (B) sorted according to population density.†
Figure 3: Number of other specialists per 100 000 population in each quintile group of municipalities (A)/counties (B) sorted according to population density.†
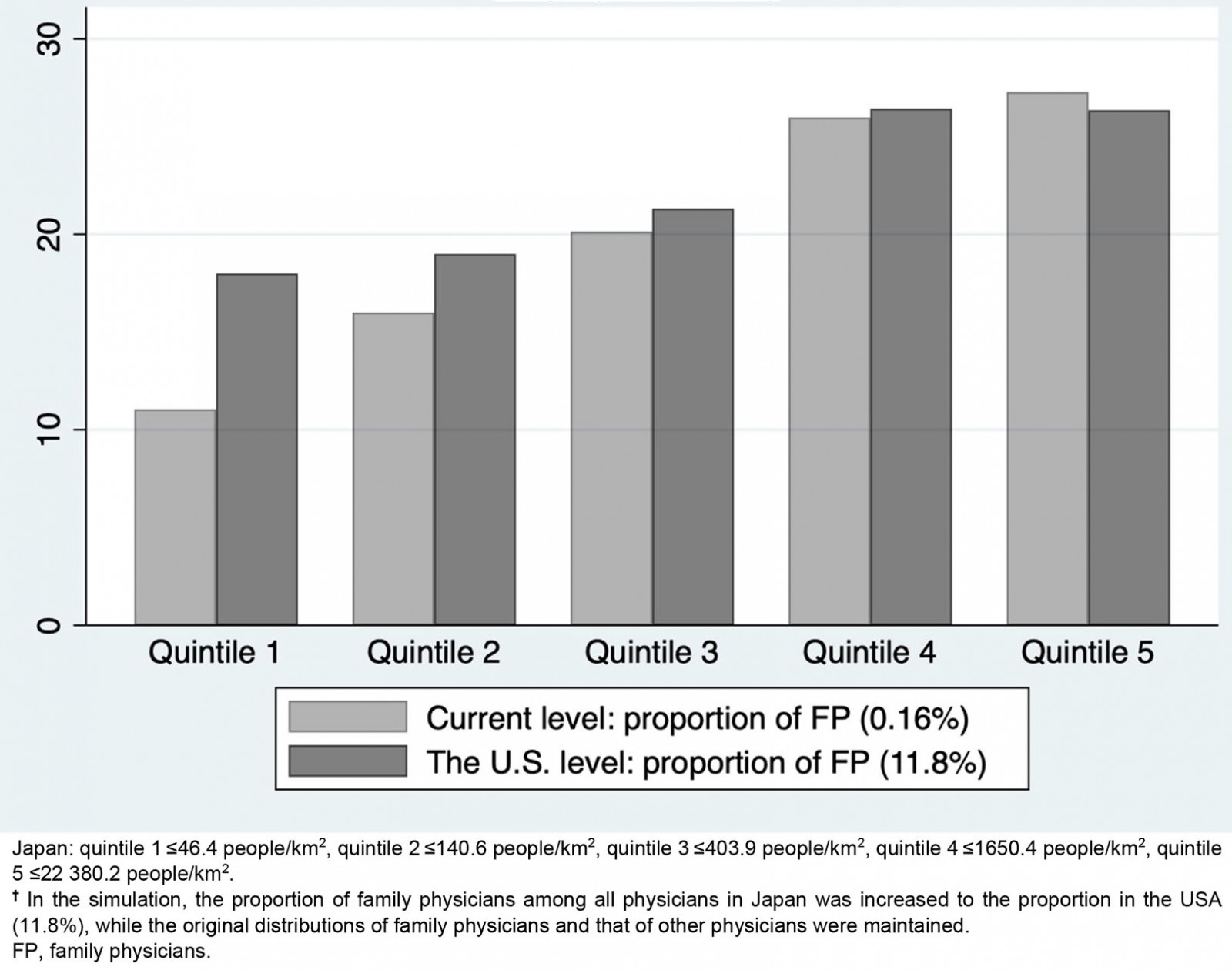 Figure 4: Simulated number of all Japanese physicians per 10 000 population in each quintile group of municipalities sorted according to population density. †
Figure 4: Simulated number of all Japanese physicians per 10 000 population in each quintile group of municipalities sorted according to population density. †
Discussion
The distribution of family physicians in Japan has significantly shifted to rural areas compared with the distribution of family physicians in the USA, while in both countries other specialists were concentrated heavily in urban areas. If the proportion of family physicians in Japan was increased to that in the USA, the geographic maldistribution of all physicians improved substantially. These results have two implications. One is that the distribution of family physicians is roughly equitable among the population in any society compared with that of other specialists, but the distribution can be biased substantially to rural areas in a society in which family medicine is emerging. The equal distribution of family physicians in the USA, which was proportional to the distribution of general population, may not actually be equitable because there is a greater need for family medicine in rural areas than in urban areas. In this sense, the concentration of Japanese family physicians in rural areas does not necessarily mean they are ‘biased’ or ‘pushed-in’, but suggests that the distribution is a desirable one to meet the need in rural areas. The second implication is that, based on the concentration of family physicians in rural areas of Japan, increasing the number of family physicians can resolve the urban–rural imbalance in the supply of physicians.
Family physicians are distributed equitably among the population in most societies with a mature primary care system. One reason for the equal distribution is that family physicians can make the most of their expertise in a rural healthcare environment18,19. In urban areas, there are many more medical facilities, including highly specialized ones, and the geographic accessibility to medical care is much higher than in rural areas20. This gives patients in urban areas more choices when it comes to their care. They can go to medical institutions that specialize in their health conditions21. In contrast, in rural areas, healthcare providers are required to provide holistic and comprehensive care22. The absence of nearby healthcare facilities also makes it easier for physicians to provide continuity of care to a single patient18. Therefore, family physicians can provide continuous and comprehensive services in rural areas, two of the core values of primary care18,23,24. In contrast, for other specialists, rural areas may not be an ideal place to apply their expertise. They need to treat a narrower spectrum of diseases, and thus need to cover a wider geographic area with a larger population to stay in business25. As a result, the distribution of other specialists tends to shift to urban areas26.
In Japan, however, the distribution of family physicians has shifted to rural areas. This can be linked to the immaturity of family medicine in Japan’s healthcare system. In Japan only about 10 years have passed since family medicine was established as a clinical discipline with a board certification system. Only 0.2% of all physicians in Japan are board-certified family physicians. Urban primary care providers were other specialists originally employed by a hospital, who then opened their own private clinics27. These former specialists treat some patients within their specialty, and also offer primary care services without being trained in primary care or certification as a family physician. In such societies, specialoids (domain-specific specialists who provide primary care services without a qualification as a primary care provider) have already established a solid position in the primary care market. In other words, it is difficult, if not impossible, for family physicians, all of whom have been recently board-certified, to enter this specialoid-saturated market. Therefore, they might prefer to work in rural areas where competition with these specialoids is less severe. In fact, when the number of general internists, who have traditionally provided a large part of primary care in Japan, was combined with that of family physicians, the geographic distribution of Japanese generalists shifted markedly to urban areas. This suggests that new family physicians have been forced out of urban areas by specialoid physicians. In a society like Japan’s, with immature family medicine, family physicians are at a disadvantage in the health professional market.
Japan’s unique system of healthcare provision may also have affected the distribution of family physicians. Almost all physicians who have completed postgraduate clinical training are employed by a hospital as a domain-specific specialist early in their career. Even if these physicians, including younger family physicians, would prefer to work in a clinic, it is financially impossible for them to do so, because most clinics in Japan are private solo practices that require approximately US$880 000 to establish28. Therefore, it is extremely difficult for younger family physicians to work in their own clinics. To continue practicing family medicine, a substantial proportion of them must be employed by a public clinic set up by the local government to provide medical care in Japan’s rural, remote and underserved areas. These are, however, a small fraction of all clinics in Japan.
In the USA, in comparison, family physicians were not more distributed in small population areas than in Japan. This is probably due to the unique situations in the USA as well as the maturity of family medicine, which differs from Japan. First, there are enough family physicians to cover the entire country. The present study’s results showed that US family physicians in the USA were widely distributed in the nation’s land area regardless of the area’s population size. Second, family medicine is provided in the form of group practice, and even young family physicians who have just completed their training can continue their careers as family physicians by being employed by a group, regardless of whether they work in an urban or rural area. In the USA, the proportion of solo and smaller-sized practices of family physicians is higher in rural areas than that in urban areas29, and thus young family physicians might have a larger barrier to entry in a rural rather than an urban practice in terms of economic capability.
Finances in rural areas could have influenced the geographic distribution of family physicians, and this would have been more obvious in the USA than in Japan. In the USA, physicians tend to be concentrated in areas where people with good health insurance plans live (ie in affluent areas, which are often urban and suburban areas). High revenues are gained for highly specialized care, procedures and surgeries, but prices for medical services by family physicians are much lower. Therefore, family physicians in the early phase of the family medicine development, just like those currently in Japan, used to have difficulty in finding jobs in urban areas and tended to be concentrated in rural areas. The design of Medicare and Medicaid, which were newly established in the USA at that time, accelerated the concentration of family physicians in rural areas because the additional funding from state and federal levels arising from the programs of Medicare and Medicaid was specific to rural populations as they involved concentrations of poor, elderly and disabled people. Also, a significant and positive change in funding was specific to the years between 1965 and 1978, and involved new federal and state spending via Medicare and Medicaid with regular increases of the payments for services to adjust for the higher inflationary costs of delivering care. However, after this period, cost cutting has been the major focus with the closures of hundreds of rural hospitals as well as closures and compromises of primary care practices. That is because since the 1980s, for family physicians, the revenue has remained stagnant and has not annually increased to keep up with the ever-higher costs of delivering care. In such context, family physicians in the USA have had new career choice opportunities that have better financing. These include emergency room, hospitalist and urgent care employment in urban areas30. In addition to the maturity of family medicine, such a financial background facilitated family physicians to be more accepted in urban areas than before, and their movement into more profitable positions in affluent areas. Japan might follow the process of the USA.
The simulation analysis showed that the geographic maldistribution of physicians in Japan improved with a larger number of family physicians. The geographic maldistribution of physicians has been a serious social problem in Japan31. To compensate for the shortage of doctors in rural areas, public medical institutions in rural areas were established by the national and municipal governments. Jichi Medical University, established solely for the purpose of training rural physicians, was established in 1972, and a regional quota, a special admission quota for producing rural physicians, was spread among most of the medical schools in Japan for the past 10 years32,33. Even with these ambitious national policies, the maldistribution of physicians has not changed. Instead, there is an even greater disparity in the supply of physicians between rural and urban areas29,34,35. The unique distribution of family physicians in Japan could contribute to ameliorating the maldistribution of physicians. Based on the results of this study, policies to increase the number of family physicians and general practitioners and reining in the number of other specialists is a plausible solution for national and local governments36.
Limitations
This study has several limitations. First, data could not be obtained on all JPCA-certified family physicians because individual information for some of them was not available on the JPCA website. The authors considered, however, that selection bias for Japanese family physicians was minimal given the high (77.2%) covering proportion. Second, the simulation analysis assumed the distribution of family physicians did not change, when it actually increased dramatically. If the number of family physicians increased to such an extent, it is possible that the geographic distribution substantially changed because of changes in government incentives, savings, supply–demand balance and recognition of family physicians among the population. This change would enable family physicians to replace specialoids in urban areas and lead to a total distribution of physicians different from that shown by the simulation. Above all, it is not realistic for the number of family physicians in Japan to increase by 72 times over a short period. The simulation was a thought experiment under an extreme assumption that showed, in a simple manner, the magnitude of the effect of the policy to increase the number of family physicians.
Two other important issues are the comparability of Japan and the USA and the limited generalizability based on a two-country comparison. The healthcare systems of Japan and the USA are quite different, especially in terms of their medical insurance systems. The results should therefore be interpreted cautiously. Adding another country or two to the comparison would make the conclusion more robust. For example, the maturity of family medicine is even higher in the UK and the Netherlands than in the USA; the percentages of general practitioners (GPs) among all doctors are 26.2%, 45.4%, 11.7%, respectively6. These two European countries have a system of population registration at each GP practice and seem to have a smaller disparity of the GP supply between urban and rural areas than Japan and the USA, although there is still some difficulty in recruiting physicians to work in rural areas26,29,37-39. Adding these countries as an international comparison would reveal the effect of such a socialized system of primary care provision. Further studies comparing many countries with various levels of maturity of family medicine are also needed to confirm the authors’ hypothesis on the relationship between the maturity of family medicine and the geographic distribution of family physicians.
Conclusion
The distribution of family physicians is more equitable than that of other medical specialists and can be affected by the maturity of the field of family medicine in a society. In countries like Japan, in which family medicine has only recently emerged, the distribution can be biased equitably to rural areas. In such countries, increasing the number of family physicians and controlling the number of other specialists may be a way to rectify the urban–rural imbalance of physicians.
References
You might also be interested in:
2016 - Doctors as street-level bureaucrats in a rural hospital in South Africa
2015 - Analysis of barriers to adoption of buprenorphine maintenance therapy by family physicians



