Introduction
Nurses are an essential and valued component of the healthcare workforce. They form the largest professional group, contribute significantly to delivering quality healthcare services and assist in the improvement of health outcomes for individual families and communities, either through preventative or curative measures1,2. To deliver effective quality care to improve efficiency of the health system and achieve all health targets, an adequate number of nurses is crucial3,4.
The shortage of nursing workforce is causing a severe burden on the quality of healthcare services due to shortage of qualified nurses to provide the effective and quality services needed to improve the health of the global population, and to achieve universal health coverage5,6. There are discrepancies in the supply of nurses to maintain an adequate number of nursing workforce as nurses retire. This relates to new recruitment of nurses, and retaining existing nurses. These discrepancies have made it difficult to respond to the growing demand for care7,8. WHO reported that health services worldwide are affected by a shortage of nursing workforce to deliver healthcare services9. The impact is posing a huge challenge globally, affecting more than one billion people, especially vulnerable populations such as women and children who desperately need quality healthcare services2,10.
There are many factors affecting the healthcare system as a result of nursing shortages. If these concerns are not addressed promptly and appropriately, the number of people requiring quality nursing care will continue to be affected. The primary goal for ministries of health to improve and protect the health of the individual will continue to be a challenge11. Challenges include decreased numbers of nursing students enrolled in nursing programs as a result of lack of proper planning and availabilities of funds, an increase in nurses retiring early due to health problems12,13, and migration of nurses due to job dissatisfaction and poor working conditions in their own country14. The main factor affecting most countries is inadequate policy direction to guide ministry of health planning and address priority health needs, and human resource workforce planning15,16.
The shortage of nursing workforce is becoming a major problem in the Pacific region as well13. In Solomon Islands, Papua New Guinea, Vanuatu, Samoa, Marshall Islands, Cook Islands, Tonga and Fiji, nurse density is far below the recommended ratio of 45 nurses per 10 000 population in order to meet the UN Sustainable Development Goals by 20309,17. Higher migration rates to other countries such as Australia and New Zealand for better job opportunities and a better working environment are common in some Pacific Island countries such as Tonga, Samoa and Fiji, and this has created challenges and gaps in their workforces that need to be addressed promptly18.
In Vanuatu, the shortage of nurses has prevented accessibility to quality healthcare services for most people. Nurses in Vanuatu constitute only 12.0 per 10 000 population.
Vanuatu is situated in the South Pacific Ocean and consists of 83 small islands, of which 65 islands are inhabited. It is categorised as a low–middle-income country with a population of approximately 272 450 people scattered over six provinces of Vanuatu: Shefa, Sanma, Tafea, Penama, Malampa and Torba. According to the Mini Census data in 2016, 80% of the population live in rural settings, with an annual population growth of 2.3%19.
Vanuatu is culturally diverse, with over 115 distinct cultures that spread across its inhabited islands. This causes significant challenges for the government and Vanuatu Ministry of Health (MoH) in meeting the health needs of the large population living in rural and remote communities19. Many health facilities have problems with the number of staff and some of the facilities are not functional due to inadequate nursing staff. This study set out to explore the perception of health leaders on factors affecting the shortage of nursing workforce in underserved areas in Vanuatu.
Methods
Study design and setting
A qualitative study was applied to gather information using focus group discussion (FGD) from nursing managers (NMs), human resource managers (HRMs) and senior clinical supervisors (SCSs) in Vanuatu on 10–12 September 2020 in three of six hospitals in Vanuatu: Vila Central Hospital in Shefa Province, Northern Provincial Hospital in Sanma Province and Lenakel Hospital in Tafea Province. FGD was considered a better approach than individual interview; it is frequently used to obtain data, and group interaction is encouraged between the individual group members. Participants were purposively selected to participate in a qualitative study to share their thoughts or perceptions about factors that cause the shortage of nursing workforce in Vanuatu. FGD is also applicable for this study because it consumes less time than individual interviews20,21.
Study population and sample
The study population included all NMs, HRMs and SCSs working in hospitals in Vanuatu. HRMs, NMs and SCSs who were working in the three selected hospitals with at least 1 year of experience were invited to participate in the study. Purposive sampling techniques were used to select participants. Purposive sampling is usually used to select people with specific roles who have experience and special knowledge to provide vital information for a study16. An invitation letter from the principal researcher was sent to the potential participants by email and/or phone, offering an opportunity to participate in the research study.
A total of 12 participants were involved in this study: four participants in each of three FGDs (one in each of the three hospitals), involving one NM, one HRM and two SCSs. Before commencement of FGD and data collection, participants signed the consent form and returned them to the research assistant.
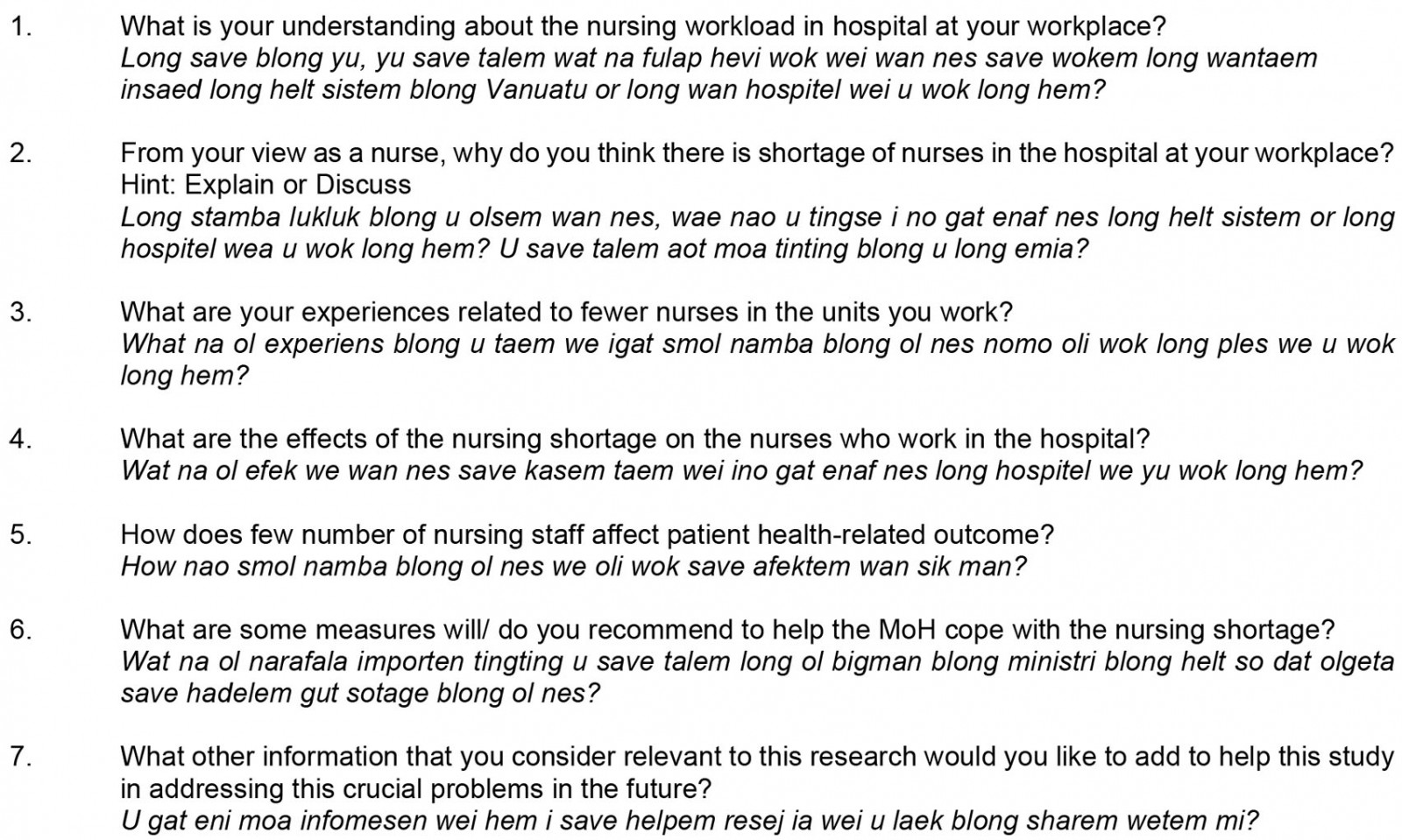
Data collection tools
FGDs were conducted among all the participants using semi-structured, open-ended questionnaires to probe and elicit information. Open-ended questions aimed to allow participants the opportunity to express their personal experiences freely22,23. The interview questions developed were based on relevant literature and research studies that fulfilled the aim and the research questions of the study. Six questions were prepared and asked during FGDs to enable the participants to explain or discuss their perceptions about the research topic (Appendix I). The demographic information form was used to collect demographic characteristics of participants such as age, gender, marital status, education level, workplace and years of working experience. The interview scripts were discussed and validated by the research supervisors using content validation to check the quality of the content and to ensure alignment with the research question.
Study procedures
All potential participants in FGDs in the three selected hospitals were given an information sheet explaining the purpose of and procedure for the study, the nature of the study, the duration of the interview, language to be used during the interview, the right to participate in the study, the benefits and risk of the study, information about notification to decline or withdraw from the study at any time, informed consent and the interview procedure (involving audio-recording to assist with the translation of participants’ verbatim quotes and transcription)24. The participant who were willing to participate signed the consent form.
The interviews were conducted in each participant’s preferred language (English or Bislama). The research assistant, who has a Master’s Degree in Public Health, and with experience in research study, conducted the FGDs.
Data management and data analysis
All interviews were transcribed by the principal researcher using manual cross-tabulation of the results, and later verified by the research assistant and the principal supervisor. The data were manually analysed using a thematic analysis process to identify the final themes. Thematic analysis is a method widely used in qualitative research, which involves identifying, analysing and reporting patterns of data25. The transcriptions were read and re-read closely to create different quotes or coding, and were discussed with the other researchers for possible modification as required. Then the data were coded and sorted into themes and subthemes based on the similarity of the issues identified from the result of the study. This was done by the principal researcher and verified by the principal supervisor.
Ethics approval
This study was approved by the College Health Research Ethics Committee at Fiji National University and by the Research Ethics Committee, MoH in Vanuatu (ID 254.20). The participants were provided with a consent form and information sheet regarding their participation in the study.
Informed consent was obtained from all the study respondents regarding their participation in the study. The information they provided was audio-recorded. Participants had the right to refuse to be audio-taped. Respondents were informed that their names would not be disclosed but would be reported in aggregated form so that no individual names would be identifiable.
Results
Demographic characteristics of participants
Twelve participants were involved in the FGD (four males and eight females). Six were aged 50 years or more, and nine were married. Eight participants had undergraduate qualifications while four had postgraduate diplomas (Table 1).
Table 1: Demographic characteristics of participants (n=12)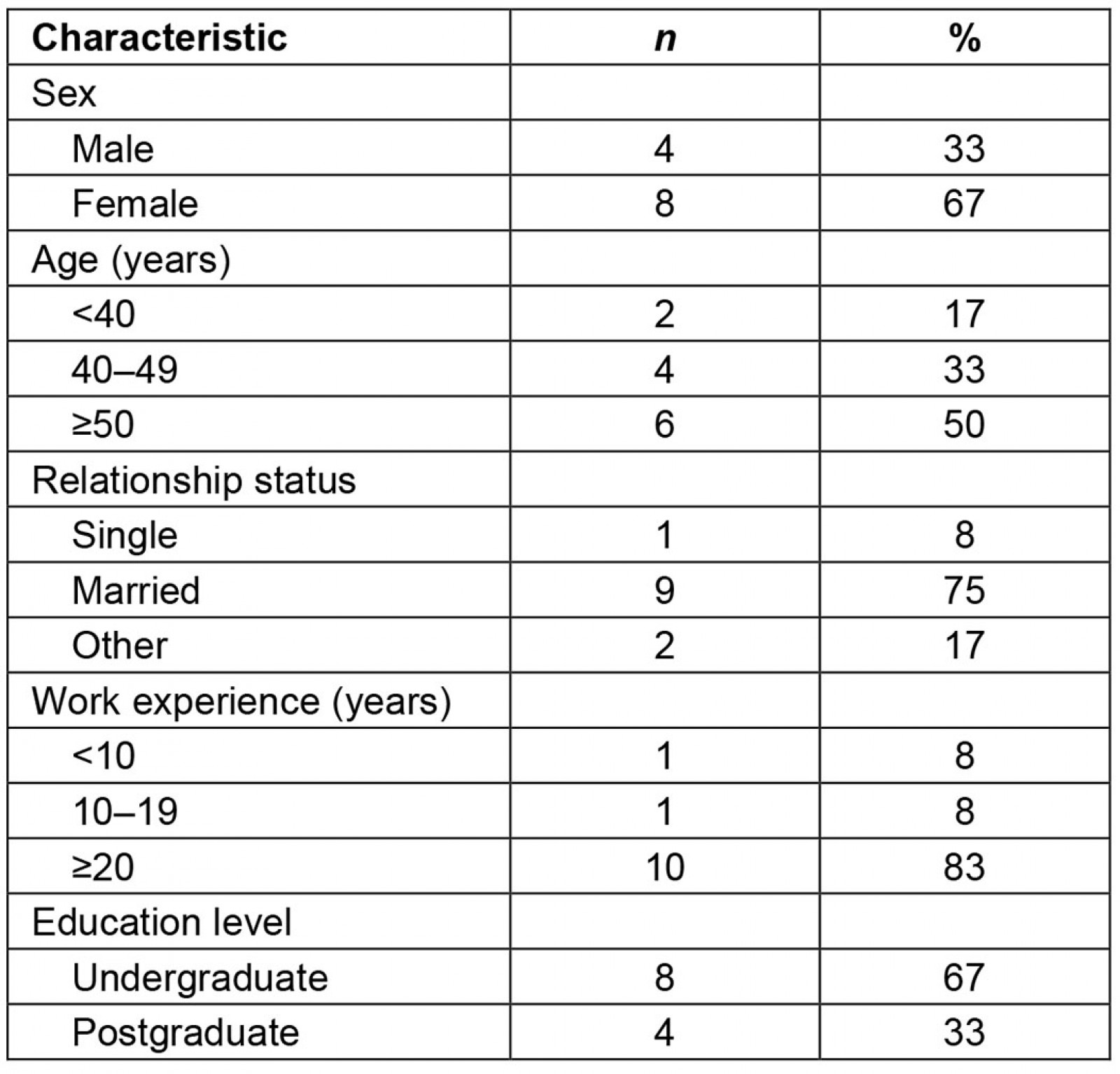
Themes and subthemes
The thematic analysis revealed four major themes emerging: lack of planning, increased population growth, nurse turnover and proposed strategies to resolve nursing shortages. The participants’ reflections were sorted into subthemes and further expanded. In this section, quotations will be presented based on the number of FGDs and participants’ perceptions.
Table 2: Themes and subthemes from interviews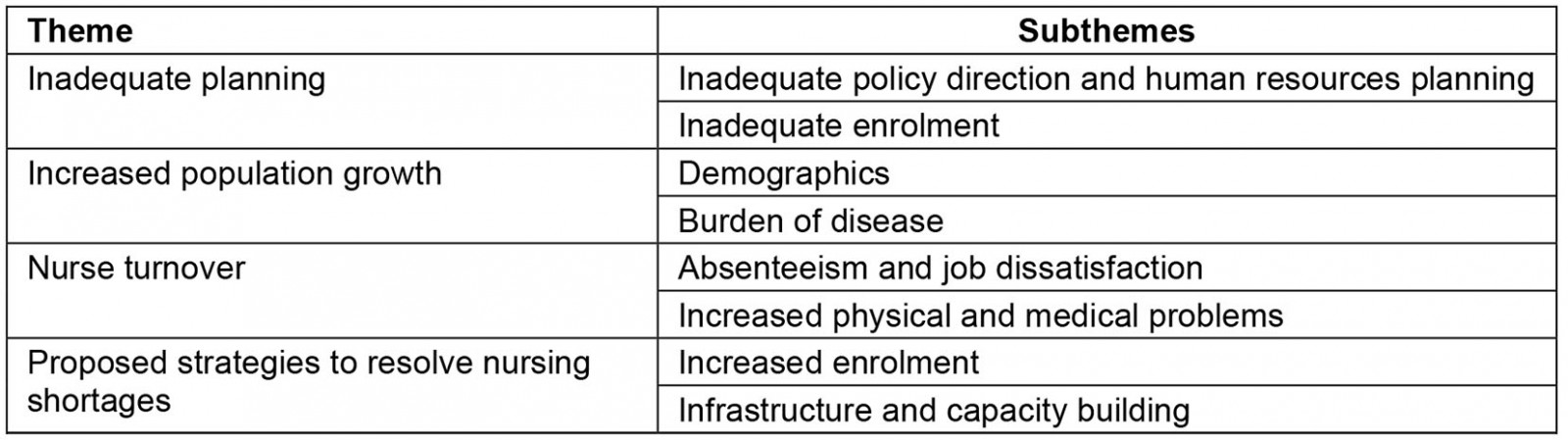
Inadequate planning: During the FGD the participants believed that ‘inadequate policy and HR [human resources] planning’ and ‘inadequate enrolments’ have influenced planning, which in turn has contributed to a nursing shortage.
Inadequate policy direction and human resources planning Inadequate policy direction and HR planning at the national level have had major impacts on the number of nurses to fill nursing gaps with regards to the number of enrolments. Participants explained the effects of poor policy and HR planning:
Poor policy direction affects the nursing supply in the Vanuatu healthcare system in the past till now. The HR at the national level is not proactive to address the expansion of the nursing college to cater for the increased number of students each year. 100 students per intake per year is better so that after three years of training we will have the right number of nursing workforce. (FGD 1; male HRM, age 38 years)
One of the respondents mentioned the implications of lack of planning and budget plans, which contributed to nurses leaving their jobs due to job insecurity:
… One of the main reasons for nursing shortage are no proper planning from the national level and no effective budget plans to cater for all the nursing positions and new recruitments. Nurses leave their job because their jobs are not secured. (FGD 1; male SCS, age 44 years)
Some participants responded that there is no continuous monitoring of the workforce structure or databases at the national level to identify the ageing workforce exiting each year:
Now that the populations of aging nurses have increased and when they exit there are no nurses to replace them due to no proper human resource and workforce planning and no records at the national level to prepare nurses to fill the nursing gap. So, to meet the demand, effective planning and monitoring is particularly important to identify shortages and the need to have regular nursing intake to replace the retired nurses and fill up the gaps. (FGD 1; male NM, age 57 years)
The majority of respondents stressed that inadequate human resource planning affects the fair distribution of the nursing workforce; therefore, to prevent a nursing shortfall, human resource planning must be effective. Furthermore, a succession plan is needed to identify gaps and train the required number of nurses:
Vanuatu MoH always has a shortage with the nursing workforce because the human resource management unit at the national level does not have an effective successful plan to identify the number of nursing gaps in the workforce and to recommend the number of nurses needed for training or recruitment to maintain the supply of nurses at all times. (FGD 2; female SCS, age 52 years)
It was added that an ineffective succession plan meant that an increased number of nurses retire without being replaced:
In 2017 there are a massive number of retirees and it causes a huge impact to the service delivery as there are not enough nurses to replace the retirees which I guess is from the poor succession plan to prepare nurses for replacement. (FGD 1; female SCS, age 55 years)
Inadequate enrolment Low enrolment numbers in nursing college have implications for the nursing supply due to inadequate planning at the national level. A participant stated:
Nursing college always enrols less number of nurses which affects the number of nursing supplies in all the hospitals and other health facilities today. This is due to poor planning from the national level to recommend nursing college to increase the number of enrolments. (FGD 2; female HRM, age 52 years)
The effects on the low number of enrolments have a huge impact on the nurse-to-patient ratio in hospital wards:
… when we look at the ratio of nurse to patient in Vanuatu which is 1:10 or 1:15 compared to other countries of which they have 1:4, there is a huge difference. (FGD 1; male NM, age 55 years)
One respondent gave the reason for low nurse enrolment as due to limited space in the nursing college, which subsequently affects the nurse supply:
One reason for low enrolment at the nursing college is due to the fact that the space in the nursing college is too small and cannot accommodate the increased number of student nurses that is why we still have problems with low number of nurse supply. (FGD 2; female NM, age 50 years)
Increased population growth: The participants in FGD believe that increased population has a major influence on the nursing workforce and the care they provide. The factors that influence increased population growth include ‘increased demand of workload’ and ‘increased disease trend’.
Demographics The increased growth rate of the population today causes significant effects on the workload in the hospital setting as well as in other rural health facilities due to increased demand and inadequate number of nurses:
Not enough nurses working mainly in the hospital settings cannot cater for the fast-growing population today. When we talk about population, we also talk about workload which is too much for the nurses to cope with. (FGD 3; female SCS, age 51 years)
Another participant added:
In my experience I can see that the population in the urban areas and also in the rural settings is increasing rapidly now but the supply of nurses is too low. (FGD 2, female SCS, age 39 years)
A major contributing factor to the nursing shortage is the rapid increase towards retirement age of the current nursing workforce, especially those who have almost reached retirement age (55 years) and will soon exit from the workforce. A participant explained that an ageing workforce makes replacement of the older nursing population more challenging as a lot of young people are not interested in enrolling in the nursing program:
Young generation today don’t see nursing as an important profession, they want to go for a higher profession like doctor, laboratory technician, pharmacy and dental. Because of that not many young people are attracted and interested to enroll in nursing to replace nurses who will be retiring and exit the workforce. (FGD 1; male HRM, age 38 years)
Increased population growth does not correlate with the supply of nurses from the nursing college. A participant described the current workload compared with the population growth and the increase of disease prevalence:
The population growth is increasing compared to the number of workforce on the ground which does not match with the current number of population and the increase number of diseases example NCDs [non-communicable diseases] etc., also when … you compare the number of graduating nurses from the Vanuatu College of Nursing Education, it does not meet the demand. (FGD 1; male SCS, age 44 years)
Conversely, the increased population would also mean an increase of people with diseases and increase admission, which can cause a greater workload for nurses:
When the population increases the number of people with diseases will also increase and there will be more clients or patients visiting outpatients department and more admissions of people with different conditions and diseases which causes more workload to the very limited number of nurses we have at the moment. (FGD 3; male NM, age 48 years)
Burden of disease All members of the FGD agreed that increased demands are due to greater prevalence of emerging diseases, especially lifestyle diseases. FGD 1 stressed that the increased demand is due to the high number of patients admitted with lifestyle diseases:
Today the increased demand is due to the high number of patients admitted in the ward with lifestyle conditions such as diabetes and high blood pressure, and also a high number of them visiting the SOPD clinic. (FGD 1; male SCS, age 44 years)
Half the participants reported that the increased in demand on nursing workforce is related to the nurse-to-patient ratio. FGD 1 stated that increased demand of workload occurs when the nurse-to-patient ratio decreases:
The increased demand is categorized when we see the ratio for nurse to patient is increasing. In Vanuatu our ratio is 1:30 which is quite huge. That means that the number of patients is increasing compared to the number of nurses working. (FGD 1; male NM, age 56 years)
Participants responded with concerns over the increased demand due to more medical orders and new nursing skills. FGD 2 stated that in the ward there are increased demands due to more medical orders and new nursing practices:
As a SCS, I’ve noticed that there is more work demand in the hospital ward due to the new introduction of nursing skill practices and too much of medical orders from the medical officers that increases the demand of work added to the routine nursing practices for nurses. (FGD 1; female SCS, age 55 years)
Moreover, the increased number of hospital admission requires special facilities or clinics (eg ear, nose and throat; eye; psychiatric; non-communicable disease; cardiac) to manage and treat conditions effectively, but specialised training is required for nurses to manage the special clinics to prevent movement of nurses within the hospital wards:
Before with less population we don’t have many health conditions that requires special clinic like ENT [ear, nose and throat], eye, mind care, NCD [non-communicable disease], cardio and many more, but currently, with the increased population and new emerging diseases, it requires more special clinics which stretches the number of nurses to manage those special clinics therefore causes shortage in the hospital wards. (FGD 2; female SCS, age 51 years)
Nurse turnover: Nurse turnover is one of the themes that emerged from the FGD from increasing absenteeism due to job dissatisfaction and nurses who are suffering more medical problems believed to be caused by increased workload.
Absenteeism and job dissatisfaction One respondent highlighted that nurses left their profession due to a poor working environment:
Most nurses run away from the jobs and look for other job elsewhere due to the poor working conditions when posted to remote facilities which include poor accommodation, very limited access to communication and difficulty to access transportation etc. (FGD 1; male NM, age 57 years)
Some reasons emerged during discussions about why nurses left their jobs, especially for those working in very remote health facilities due to poor working conditions, along with a lack of leadership support from nursing management:
Most nurses in the rural or remote health clinics run away from their job due to no remote allowances and poor working equipment and environment. Also, there is no leadership support from the nursing management to visit the nurses and provide support and to assess their working environment. (FGD 2; female SCS, age 52 years)
Another reason given was nurses’ job dissatisfaction due to grievances and salary anomalies:
Unresolved salary anomalies and grievance for nurses for quite a long time causes nurses to leave their job early before their retirement age due to job dissatisfaction. (FGD 2; female SCS, age 51 years)
One of the respondents reiterated that the reason why nurses left their jobs was because of low motivation. There are no effective career pathway and ineffective professional development and advancement for nurses:
No career pathway and no professional development for nurses cause low motivations which leads to nurses migrate to other sectors for job opportunities. These again affect the number of nursing workforce in the hospitals or other health facilities. (FGD 2; female HRM, age 52 years)
Absenteeism is increasing among nurses, especiall those who work in the hospital setting, due to job dissatisfaction. The managers stated that hospital wards were severely affected due to increased absenteeism and ‘sick calls’ from nurses:
As a nursing manager in a hospital, I always receive complaints from the ward charge nurses from increased absence of nurses from work and sick leaves which affect the wards from being short staffed. With few nurses working, continuous absenteeism and sick calls affect the services in the wards. (FGD 1; male NM, age 57 years)
A senior clinical supervisor stated the main reason for absenteeism and the challenges to reorganise staff to ensure continuity of services:
The continuous absenteeism is due to increased workload with very limited staff in each ward. The challenge we encounter is to reorganise staff to ensure that services must continue. Sometimes we have to fill in to cover the nurses who are absent and on sick calls. (FGD 1; female SCS, age 55 years)
Increased physical and medical problems Physical problems such as injuries are common causes of poor attendance among nurses who work in a busy unit with increased workload:
Physical and medical issues are common for nurses who work in a very busy ward with increased workload which results in poor attendance. Some nurses have injuries when providing care to patients who cause them to remain at home for a long period of time for recovery. (FGD 2; female SCS, age 47 years)
Other nurses were granted early retirement due medical reasons. (FGD 2; female HRM, age 52 years)
Medical health conditions are increasing in health facilities, especially in hospital settings, due to pressure from work on nurses. A response in FGD 3 was that nurses who are working in hospitals are more at risk of developing medical health issues due to work overload:
In our hospital more nurses have medical problems which cause absenteeism and continuous sick leaves from workload. (FGD 3, male NM, age 48 years)
Work overload causes mental health issues. FGD 2 reported that stress causes psychological disturbances for the nurses, which not only affects their health but may result in medical errors that jeopardise the nurses’ integrity:
Increased workload causes psychological disorder which affects us due to moral distress and pressure from work. This may result in medical errors which can affect our integrity. (FGD 2; female SCS, age 51 years)
Distress due to overworking affects not only the physical and mental health of nurses but also social and family relationships. In FGD 3 it was reported that long hours and fewer days off affected nurses’ social and family relationships:
Many nurses in the hospital where I work have limited time to spend with their families. They also don’t have time for other community activities like church activities, sports activities and community involvement which affected their social relationship. (FGD 3; female SCS, age 47 years)
Proposed strategies to resolve nursing shortages: Some strategies were proposed by the participants to resolve the nursing shortage. The strategies were categorised as increased enrolment, and infrastructure and capacity building.
Increased enrolment Effective planning and policy directions are needed to improve nursing enrolment and recruitment, and increase the supply of nurses to meet the increased demand:
The Vanuatu MoH must have effective policy and planning directions to improve the number of intakes to 100 each year for at least 10 years to increase the supply of nurses and to meet the demands. (FGD 1, male HRM, age 38 years)
Having an effective succession plan is necessary to identify different age gaps and to train nurses accordingly to fill the nursing gaps:
Within the MoH human resource workforce, there are a good number of nurses with the age range from 20 to 30 and 50 to 55, but very few from the ages range from 40 to 50. Effective succession plan is important to identify gaps and train nurses accordingly to have sustainability of the nursing workforce in the future. (FGD 2, female HRM, age 52)
FGD 3 included the response that proper planning and budget allocation, and increased pay for nurses, are necessary to attract nurses and for job retention:
All the positions in the MoH structure should be budgeted for according to the workforce plan and according to the needs in each cost centre. For job satisfaction, MoH must increase the remuneration package for nurses so that it is attractive, and nurses will be happy and satisfied, in that way we can prevent nurses from leaving their job. (FGD 3, male HRM, age 48 years)
Continuous monitoring and evaluation is necessary at all health facilities as well as of the workforce to identify and relocate nursing staff for fair distribution and to maintain adequate numbers of nurses at each facility:
Monitoring and Evaluation officers in the national level should visit all the health facilities and check accordingly for the required number of nurses in each facility and any facility [that is] overstaffed can be moved to the hospital with less number of staff for fair distribution. (FGD 1; male HRM, age 38 years)
FGD 3 identified that promoting nursing in secondary schools or to the public and on social media to increase awareness of the nursing profession is necessary to attract a young population to enrol in nursing programs to increase enrolment numbers:
A lot of young individuals need to enrol in the nursing program, however they need to have the knowledge about the nursing profession in order to increase their understanding and interest to enrol therefore, and promoting nursing in the secondary school and in social media is a must. (FGD 2; female SCS, age 39 years)
Recruitment of a principal nursing officer as key nursing personnel at the national level is crucial to address the nursing development component and other nursing shortage issues, according to FGD2:
Principal nursing officer is one of the key nursing personnel priority positions within the nursing division and should be recruited and budgeted for to address nursing development, monitor nursing issues and oversee the nurses throughout the country. He/she can be a great influence or part of the planning process in addressing nursing shortage in Vanuatu. (FGD 2; female NM, age 50 years)
Infrastructure and capacity building An expansion of the nursing infrastructure to cater for increased enrolment is crucial to increase the nurse supply. The facility infrastructure and capacity building are also necessary in conjunction with increased enrolment to improve clinical practice:
If the MoH expands the classroom and increases enrolment, it is also important to increase the health facilities infrastructure to cater for the increased enrolment during the clinical practices. (FGD 1; male SCS, age 44 years)
Faculty capacity building for all nursing faculty staff is also necessary to enable them to upgrade to a postgraduate and master level to deliver quality nurse training, according to FGD 1:
All nursing teaching staff should upgrade to higher qualification levels as part of their capacity building to be able to deliver quality training to the nurses. (FGD 1; male SCS, age 44 years).
In FGD 3, a response was that recruitment and training of more senior clinical supervisors for all referral and provincial hospitals are necessary for mentoring and coaching nurse interns:
It is good to recruit and train more SCS in all hospitals to coach and mentor new intern nurses in order to provide quality nursing care. (FGD 3; female SCS, age 51 years)
Effective policies were discussed as necessary to address the infrastructure and to increase capacity building of teaching staff:
To increase infrastructure and capacity building, it is necessary to have effective policies to address them effectively in order to increase supply of nurses in the future. (FGD 1; male HRM, 38 years)
Discussion
The findings from the health professionals in Vanuatu showed the major factors that affect the nursing shortage and the impact on health service delivery for Vanuatu19. The findings also reported the possible interventions to resolve the nursing shortage in the future.
Inadequate planning
There are appropriate number of staff with academic credentials to teach in the Diploma of Nursing program, but the inadequate enrolment of 35 to 40 and poor HR planning have major influences on planning that contribute to the nursing shortage.
Low enrolment numbers at nursing college has implications for the number of trained nurses due to inadequate planning at the national level. Only 35 registered nurses each year and 15 midwives every second year graduated from the only nursing college in Vanuatu due to limitations of infrastructure. With the 50% of clinical nurses who retire each year, the number of workforce affects the nurse-to-patient ratio in the hospitals and other healthcare facilities19. The managers have confirmed that the effect of the shortage nursing workforce is evident. The nurse-to-patient ratio is disproportionate in the Vanuatu health setting: 1:10 to 1:15. The nurse-to-patient ratio in Vanuatu was calculated according to the number of patients admitted in each ward and the number of nurses working on each shift. An approved mandated minimum nurse to patient ratio for each shift is of 1:4 or 1:5, which was first developed in Victoria, Australia in 200026. However, the mandated minimum ratio is not applicable with the current situation in Vanuatu due to the nursing shortage.
Most health managers agreed that inadequate planning and policy direction has significant effects on the nursing workforce and the Vanuatu health system. Managers noted that they hadn’t seen any policy or a succession plan within the HR planning that would effectively address the nursing workforce problems. Poor policy direction from the Vanuatu MoH has shown that the nursing college infrastructure is too limited to accommodate an increased number of nursing enrolments. Furthermore, there are no policies to address capacity to increase the number of students and the faculty staff to contribute to the overall shortage. Various studies support the need to improve infrastructure to accommodate nurse enrolment as well as improve educational and faculty capacity to improve the increasing demand for nursing workforce. Lack of these activities will impact the adequate quantity of nurses in the future27,28.
Inadequate human resource planning has significant effects on the current nursing workforce, where there is inadequate distribution of new nurses after their internship program. This can be prevented if workforce planning at the national level ensures a fair distribution of nurses in all facilities. A study in Fiji shows that nurses were distributed according to the level of need and not necessarily according to equal numbers across the provinces. Challenges have been experienced with unequal nurse distribution across all the islands and provinces29. Upgraded versions of databases are necessary to ensure a fairer nursing workforce distribution and to identify workforce trends to strengthen the health system12. However, the database used by the Vanuatu MoH needs to be upgraded and to adopt the experience of other countries to improve the workforce distribution.
Increased population growth
The increased population is a common reason for complaints by nurses, causing increased trends of diseases, which result in increased work demand.
Vanuatu has an annual population growth of 2.3%. It faces the burden of non-communicable disease, which is a leading cause of morbidity, with a growing number of inpatient admissions, of around 18 000 per year. This has placed additional pressure on the Vanuatu economy as it seeks to accumulate more nurses to keep up with the needs of increasing population19. The increased population growth also causes significant effects on workload, especially in the hospital setting due to increased demand for care services.
A major contributing factor to the nursing shortage is a rapid increase in the retirement age of the current nursing workforce. Replacement of an ageing workforce is more challenging as many young people are not interested in enrolling in nursing. A study confirmed that the nursing shortage has significantly impacted all operational levels in the hospital setting as the demand for nurses increases30. If the recommended strategies to resolve the nursing shortage are implemented in Vanuatu within the next 2 to 3 years, the recommended ratio will likely be achieved by 2030.
The supply of nurses from the nursing college is not keeping pace with population growth and increased disease. Moreover, with the increased number of patients, special facilities are required address various diseases effectively, and such facilities would need trained, specialised nurses. Studies have shown that diseases associated mainly with population and with other risk factors such as obesity and smoking lead to non-communicable diseases31,32.
Nurse turnover
Nurse turnover is one of the themes that emerged from the managers’ perspectives from increasing absenteeism and increased medical problems of nurses due to increasing workload.
Findings identified that, in Vanuatu, unresolved salary anomalies and poor working environment are the main contributing factors for job dissatisfaction . The managers witnessed the effects of job dissatisfaction due to poor working conditions, continuous absenteeism and lack of punctuality, which results in nurses leaving the profession to look for other employment opportunities. The findings from nurses’ perspectives also confirmed that lack of motivation is another reason for nurse turnover. Studies have shown that dissatisfaction is the reason for nurses’ absenteeism and turnover, which later impacts the nursing workforce33,34.
Health and medical conditions such as injuries are common issues among nurses who work in busy and overcrowded health facilities, and that cause poor nurse attendance. The findings discovered that most nurses have experienced injuries, mostly back injury from handling patients in the workplace and issues affecting their physical health.
On the ratio of nurses in Vanuatu, there are more female than male nurses. Consequently, more female nurses are likely to experience straining injuries, which can lead to longlasting medical problems and reduce productivity. Studies have shown that pressure of work is the most contributing factor, which can lead to back pain from patient handling35,36.
Proposed strategies to resolve the nursing shortage
Effective planning and policy are crucial to improving nursing enrolment and recruitment, and to increase the supply of nurses to meet increased nurse demand. Findings show that enrolment is one of the driving factors to ensure an adequate nursing workforce, which needs more attention and focus in order to meet the increased nurse demand. Greater investment should be made to increase enrolment of student nurses in nursing programs to 100 compared to the current enrollment of only 35 to 40 for the Diploma of Nursing and 15 for the Graduate Diploma in Midwifery each year. Furthermore, it is necessary to have an increased number of nurses in order to improve working conditions and patient quality of care37. To increase enrolment, it is also necessary to promote nursing in secondary schools as well as increase public awareness to increase understanding about the nursing profession. This may attract the younger population to enrol in nursing so that, after their training, they will be able to replace ageing nurses. This is one of the best strategies to address the nursing shortage. It was one of the practices in the past but needs strengthening to increase the public’s understanding of the nursing profession. Studies support the belief that it is necessary for a health system to invest in nursing education to increase the number of nurses enrolled. In this way, nurses’ working conditions as well as the quality of patient care will improve accordingly34,38.
Facility infrastructure and capacity building are also necessary in conjunction with an increase in nurse enrolment to improve clinical practice, according to findings. A study has shown that nursing training facilities is important to ameliorate the quality of training. Other countries have similar problems to Vanuatu, with budget constraints that restrict expansion and improvement of nurse training infrastructure39.
Conclusion
The present study has identified many key factors that contribute to the current shortage in the nursing workforce in Vanuatu as well as the recommended strategies to address a projected shortage. Studies have shown inadequate planning, increased population growth and nurse turnover as being the cause for shortage of nursing workforce. The findings may be helpful to policymakers at the decision-making level to address and resolve the nursing workforce shortage and improve nursing performance in the future.
Acknowledgements
We would like to thank all the study participants and those who were very supportive with their valuable time and participation in the FGDs. We also thank Mrs Julie Sutherland for valuable editing assistance.
References
You might also be interested in:
2021 - Tuberculosis in the Torres Strait: the lady doth test too much
2016 - Outreach programs: an adjunct for improving dental education
2015 - Indonesian medical students' preferences associated with the intention toward rural practice