Introduction
According to WHO, as of 8 June 2022, SARS-CoV-2 (COVID-19) has infected over 530 million people and been responsible for over 6.2 million deaths worldwide1. In response to the relatively high mortality and morbidity of the pandemic, governments internationally have enacted a multitude of public health measures, including mandatory social distancing, mask wearing, self-isolation, quarantine and lockdowns2. At the first peak in April 2020, over half of the global population was under lockdown. Fear, uncertainty, disruption of social interaction and closures of businesses, schools and recreational facilities have had extensive health, economic and social impacts, with the scale of the global economic contraction comparable to the Great Depression of the 1930s3. The COVID-19 pandemic has been associated with poorer mental health and higher psychological distress in cohorts internationally4,5. All of these things also apply to Australia, where the public health measures implemented during the early stages of the pandemic resulted in large scale disruption to work and recreation, contributing to a decline in mental and physical health6,7.
One area requiring further investigation is the impact this changing physical and social environment has had on lifestyle behaviours: smoking, nutrition, consumption of alcohol, physical activity and sleep (SNAPS). It is well known that these highly modifiable lifestyle behaviours are bidirectionally linked to mental health; this likely remains true in the time of COVID-196,7. However, there is a poor understanding of how COVID-19 may have affected these lifestyle behaviours and the relationship between lifestyle and mental wellbeing in this context. An increased understanding of this could provide clinicians and public health organisations with the confidence to target specific behaviours in the prevention and treatment of pandemic-related mental health issues.
An Australian cross-sectional study of an urban population reported decreased physical activity (48.9% of the sample of 1491 adults) and sleep (40.7%), alongside increased smoking (6.9%) and alcohol consumption (26.6%)7. These changes were associated with higher depression, anxiety and stress symptoms, especially negative change in self-reported sleep quality, which had the strongest correlation with depression out of all lifestyle factors examined. Sleep is known to be bidirectionally associated with depression8. Similar cross-sectional studies have been conducted in Croatia and the UK reporting correlations between poorer sleep, diet and exercise and negative mood, but interestingly not alcohol consumption9. However, these studies were limited to urban populations and some had incomplete assessment of lifestyle behaviours.
Rural Australians’ experience of COVID-19 is not yet well represented in the literature. Broadly, the issue of mental illness in rural Australia is exemplified by a high suicide rate, which is up to 40% higher than that of urban areas10. Rural Australians face a range of general barriers to engagement with mental health services, such as increased physical distance and transport, reduced service availability, a culture of self-reliance and reluctance to discuss mental health issues in part due to perceived stigma and reduced anonymity11,12. In contrast, rural areas also benefit from high levels of ‘social capital’, with high rates of community participation and levels of support13. It remains unknown how living rurally may modify mental health in the context of the COVID-19 pandemic. Australian research has demonstrated the development of detrimental health behaviours among rural women during the COVID-19 pandemic, with one study finding that women with children were more likely to report increased alcohol intake14.
Economic disadvantage has been found to correlate strongly with distress, with loss of income strongly associated with the development of mood and substance use disorders15. This may suggest that those with a loss of income are the most affected by COVID-19 and have the highest distress. In addition, in recent years, the rural New South Wales (NSW) population has experienced a drought crisis, with the Millennium Drought lasting between 2001 and 2009 and the recent drought subsiding only in early 2020 as the COVID-19 pandemic began16,17. It is known that drought substantially increases psychological distress and risk of suicide among certain groups, especially males18. However, it is not known how drought affects lifestyle behaviours. Framing this study in the context of both drought and COVID-19 may improve our understanding of patterns of lifestyle behavioural change in response to these two adversities.
This study will explore the relationship between lifestyle behaviours and psychological distress in a drought-affected rural Australian region, in light of the COVID-19 pandemic.
There is a paucity of research involving the use of a clinically applicable lifestyle scoring system. Through this study, a Global Lifestyle Score (GLS) was created in an attempt to correlate lifestyle with the impact of COVID-19 and distress. A holistic and standardised measurement of lifestyle parameters could be applicable in multiple healthcare settings.
Methods
Study design, setting and context
This was a cross-sectional study of the Western New South Wales Primary Health Network (WNSW PHN) Region, which is entirely classified by the Australian Statistical Geography Standard (ASGS) as at least rural based on population and distance to services, and comprises 44% remote or very remote local government areas as well as several larger rural town centres19. The total population is approximately 309 900 people with 12.8% identifying as Aboriginal or Torres Strait Islander, compared to 3.3% nationally20.
While all participants living within the region were eligible, survey distribution targeted two of the largest centres (Bathurst and Orange, Central Tablelands) as well as one remote town (Condobolin) due to ongoing close ties and community goodwill between these communities and the university.
At the time of survey distribution, the state of Victoria was subjected to an enforced strict lockdown, and unlinked COVID-19 cases were appearing in NSW, prompting social distancing measures, partial lockdown and travel restrictions. Social distancing included keeping a space of 1.5 m between individuals, as well as limitations to public gatherings, restaurants, bars and retail stores based on their ability to maintain social distancing. Most schools were returning to face-to-face teaching from online learning, while university campuses were limiting or ceasing face-to-face teaching and placements, transitioning to online learning. Most states had closed their borders to NSW.
Survey participants and recruitment
An anonymous online survey was conducted in September 2020 and distributed to various rural communities via Facebook and local email mailing lists. Eligible participants were adults aged 18 years and over living in the study region. A total of 440 individuals partially or entirely completed the survey. Of these 440 responses, participants with 80% or higher completion rate were included in the analysis, totalling 304 responses (69.1% of total participants who started the survey). The number of accepted responses was slightly lower than the target response number, which was calculated to be 322, based on a sample size calculation with an estimated proportion of the sample reporting COVID impact of 30%, margin of error of 5% and confidence level of 95%. Due to COVID-19 and the difficulty in distributing surveys in person, community engagement was primarily achieved online, by contacting local councils, which distributed a survey link via email and by posting on community Facebook groups for residents of Central West NSW. The survey was accessible on mobile devices and computers. Data collection took place over 1 month in September 2020.
Survey tool
The questions for the survey were developed around the SNAPS lifestyle guidelines of the Royal Australian College of General Practitioners21. To assess mental wellbeing, the Kessler-5 (K5) for psychological distress and the Adult Hope Scale (developed by Snyder et al) for hopeful dispositional traits were incorporated into this survey22. Additional questions around COVID-19 impact, drought impact and demographics were also developed. To access the survey, participants were required to provide consent after reading the participant information statement on the first page of the survey. See Appendix I23-26 for the survey tool and further details.
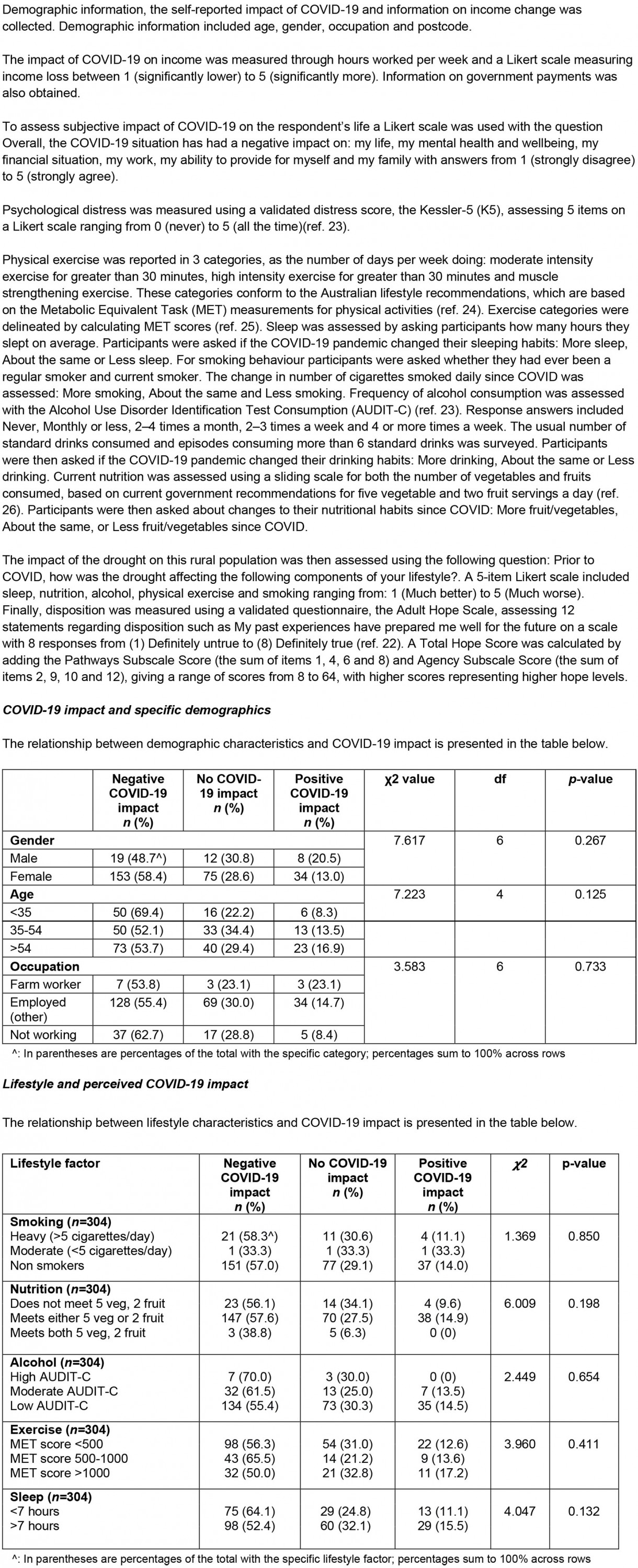
Global Lifestyle Score
A GLS for each respondent was created by grading reported behaviour for each of the five lifestyle items (smoking, nutrition, alcohol, physical activity and sleep) against consensus guidelines, and calculating a composite score ranging from 5 to 15, with higher scores indicating a healthier overall lifestyle profile (Table 1).
Table 1: Global Lifestyle Score scoring rubric27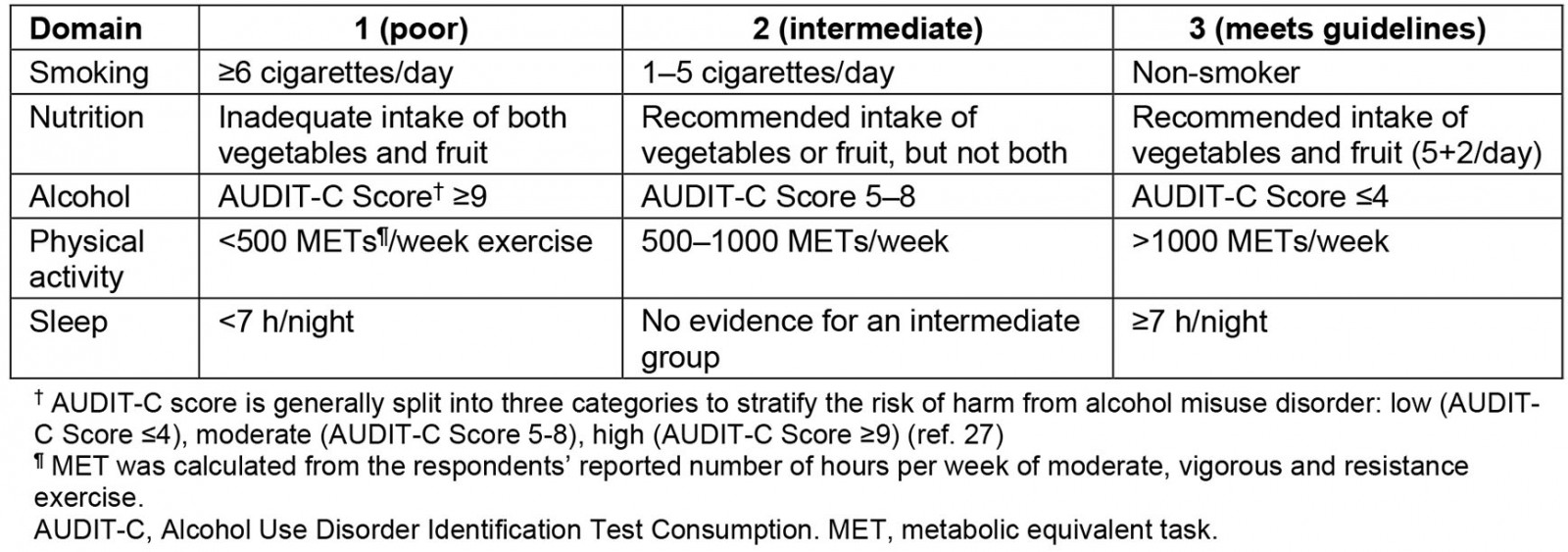
Data analysis
Statistical analysis was performed on SPSS v27 (IBM International; http://www.spss.com). Before analysis, Likert scale responses for overall COVID-19 impact, drought impact and impact of COVID-19 on income, smoking, nutrition, alcohol, physical activity and sleep were recoded into subcategories of negative impact (1), neutral (2) or positive impact (3) in order to maximise power. Descriptive statistics were generated, including frequencies and percentages for categorical variables (eg demographic variables and COVID-19 impact scales), and means and standard deviations (SD) for continuous variables.
K5 and the Total Hope Score (a standardised score calculated from addition of agency and pathway subscales on the Adult Hope Scale) were compared between groups based on demographics, overall COVID-19 impact and COVID-19 income impact using independent samples t-test or ANOVA with Posthoc Tukey tests. For the age-versus-COVID-19 impact analysis, age was re-categorised into ages <35 years, 35–54 years or >54 years. K5 psychological distress was also correlated with the GLS and Total Hope Score using Pearson correlation.
The association between overall COVID-19 impact and demographics and reported impact of COVID-19 on individual lifestyle factors was determined using χ2 tests. Appropriate statistics (Pearson’s r, t, F values, degrees of freedom (df)) were reported for all tests. P-values were considered significant if less than 0.05.
Participants’ qualitative comments were analysed by brief thematic analysis to identify key themes regarding the impact of the COVID-19 pandemic on lifestyle based on Braun and Clarke’s approach28. Participants’ qualitative statements were assigned codes; similar codes were assigned subthemes, and subthemes were aggregated into themes that represented broad, overarching ideas.
Ethics approval
Ethics approval was obtained from Western Sydney University Human Research Ethics Committee (H13796). All participants were provided with written informed consent prior to participation. The article contains no identifying information.
Results
Participant demographics
The sociodemographic characteristics of participants are reported in Table 2. The majority of participants were female (262, 86.2%), aged 35–64 years (194, 63.8%) and employed in non-agricultural industries (232, 76.3%).
Table 2: Sociodemographic characteristics of participants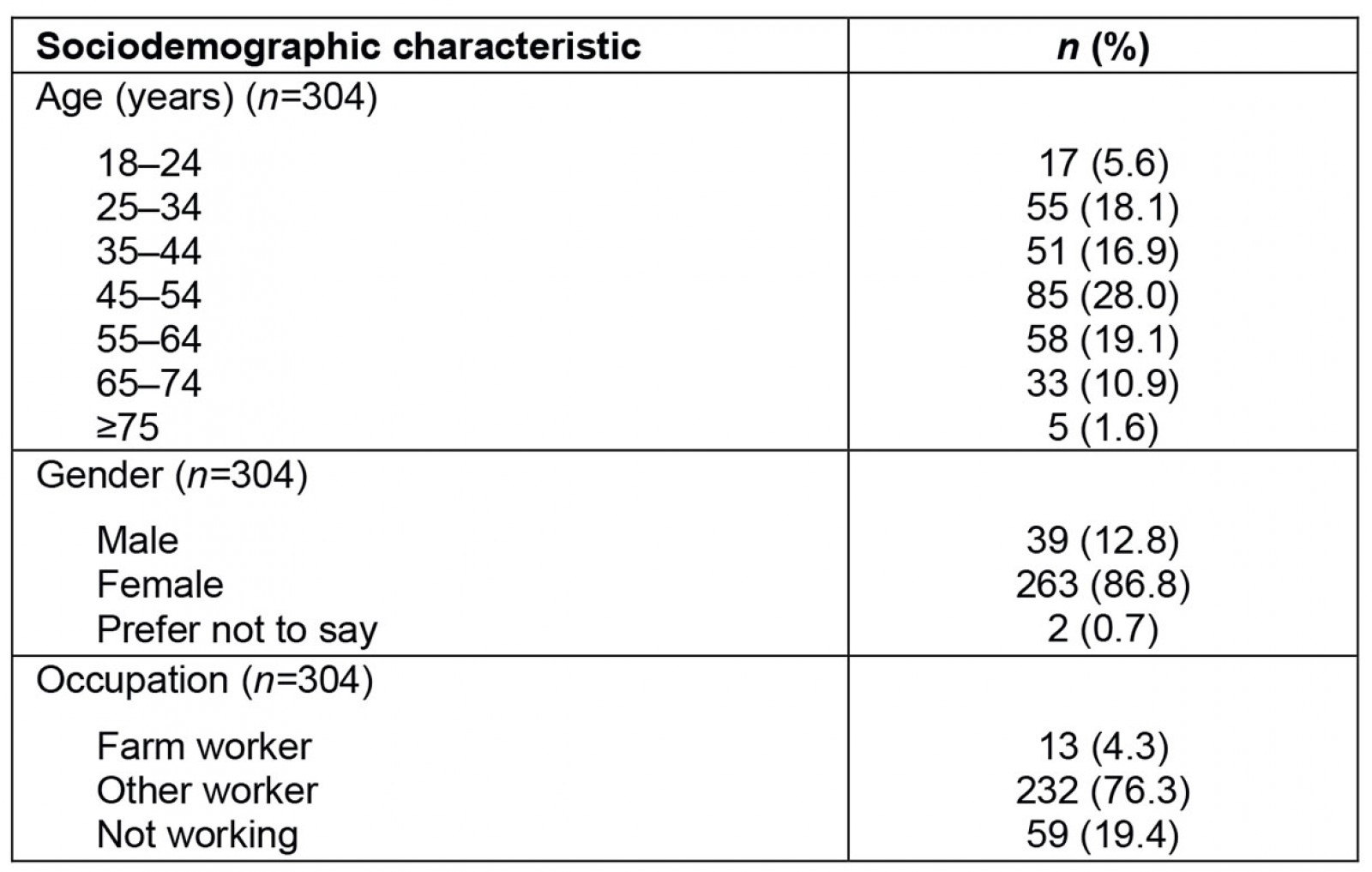
Mood and disposition
The K5 was used to measure psychological distress, with scoring either categorised as low–moderate (5–11) or high–very high (12–25). The mean±standard deviation (SD) K5 score in the participants was 10.39±4.48. High distress on the K5 scale was present in over one-third of participants (n=95, 33.7%) with the remainder in the low–moderate category. The Adult Hope Scale was used to measure hopeful disposition. The mean±SD Total Hope Score, derived from the Adult Hope Scale (n=266), was 44.08±10.78.
Perceived impact of COVID-19 and drought
Over half of participants reported negative COVID-19 impact (n=173, 56.9%) (Fig1). A total of 46 (15.1%) reported a loss of income due to COVID-19. Almost half of participants reported a negative impact of the drought on their life (n=144, 49.0%).
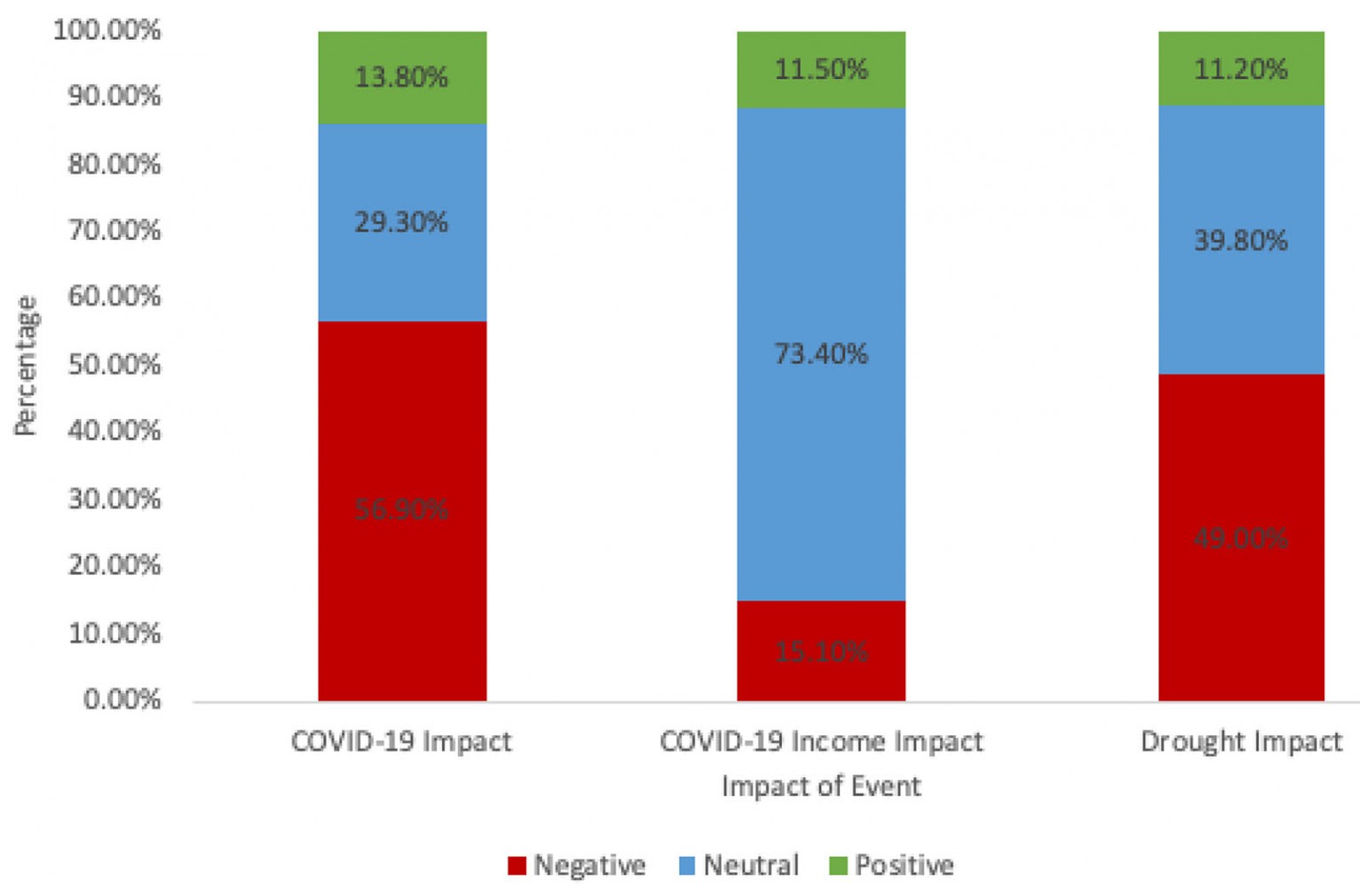 Figure 1: Perceived impact of COVID-19, impact of COVID-19 on income and perceived drought impact.
Figure 1: Perceived impact of COVID-19, impact of COVID-19 on income and perceived drought impact.
Lifestyle behavioural change due to COVID-19
All participants (n=304) answered questions regarding the impact of COVID-19 on their lifestyle factors (smoking, nutrition, alcohol, physical activity and sleep) (Fig2). Most participants (n=220, 72.4%) were active drinkers and about one-eighth (n=39, 12.8%) were active smokers. Across all lifestyle factors, the most common response was no impact.
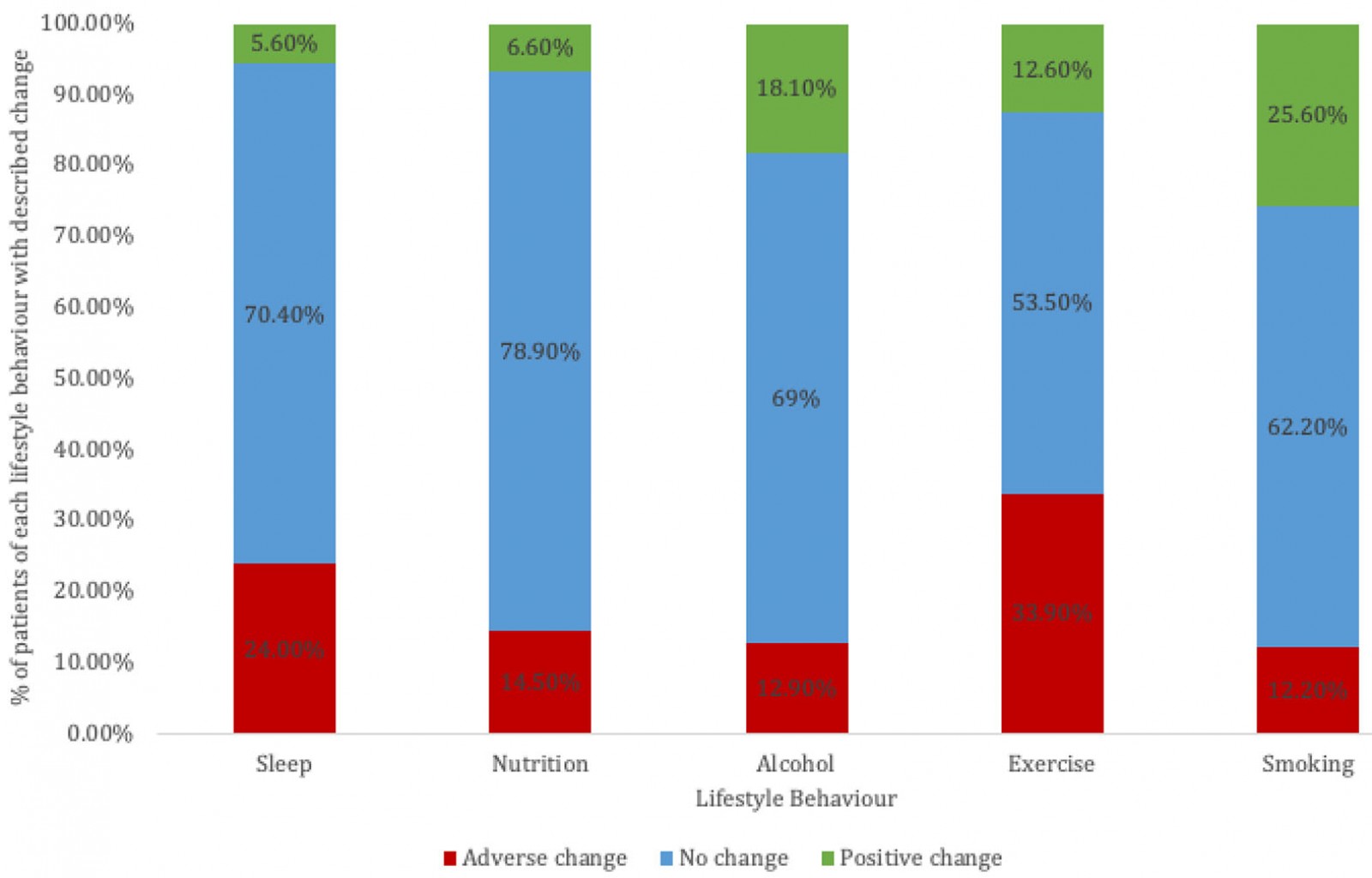 Figure 2: Self-reported changes in lifestyle behaviour due to COVID-19.
Figure 2: Self-reported changes in lifestyle behaviour due to COVID-19.
Association between psychological distress, lifestyle and disposition at time of survey
Current lifestyle behaviour at the time of survey alongside distress levels is summarised in Table 3. The GLS calculated based on these lifestyle factors ranged from 7 to 15 in the cohort. The mean±SD GLS was 11.28±1.63.
A significant negative correlation was found between distress and the GLS (r = –0.293, p<0.001), with those having a higher positive lifestyle score reporting lower distress.
Distress was significantly higher in participants who slept fewer than 7 hours per night (p<0.001). Similarly, a statistically significant correlation was found between distress (K5) and cigarettes smoked (p=0.006). Posthoc tests showed heavy smokers were significantly more distressed than non-smokers. There was a significant correlation between participants with a MET (metabolic equivalent of task) score >1000 having lower levels of distress (lower K5 scores) than those with a MET score of 500–1000 (p=0.032) (Table 3). No correlation was found between distress and nutrition or alcohol intake.
Table 3: Lifestyle behaviours correlated with distress at time of survey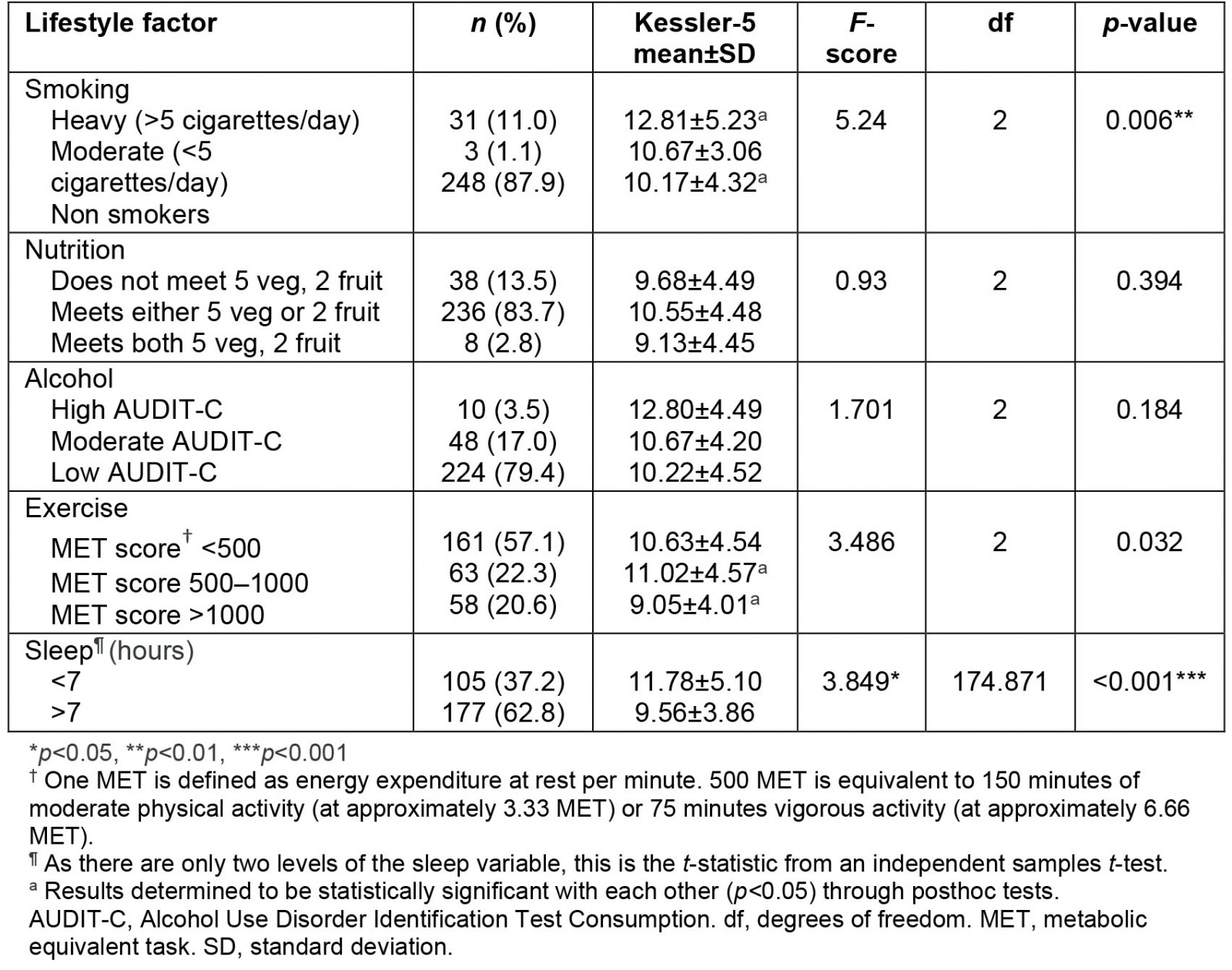
Association between psychological distress and change in lifestyle behaviours, income loss and greater perceived COVID-19 impact and hopefulness
Psychological distress was associated with changes in all lifestyle factors except alcohol (Table 4). Participants who reported either increased or decreased sleep were significantly more distressed than those who had no change to their sleeping habits. Those reporting less exercise were significantly more distressed than those with no change to their amount of exercise. Those reporting better nutrition were found surprisingly to be significantly more distressed than those with no change to their nutrition. Those who reported more smoking were significantly more distressed than those reporting no change or less smoking. No significant correlation was found between K5 and change in alcohol consumption.
Participants who saw a reduction in their income during COVID-19 had significantly higher distress than those whose income was unaffected or who had an increased income. Similarly, those who reported a negative COVID-19 impact were also significantly more distressed (Table 5).
A less hopeful disposition (low Total Hope Score) was also significantly correlated with higher distress (r = –0.364, p<0.001)
Those who reported a negative COVID-19 impact and no COVID-19 impact were significantly less hopeful (with lower Total Hope Scores) than those who reported a positive COVID-19 impact (Table 6).
Table 4: Lifestyle behavioural change due to COVID-19 correlated with distress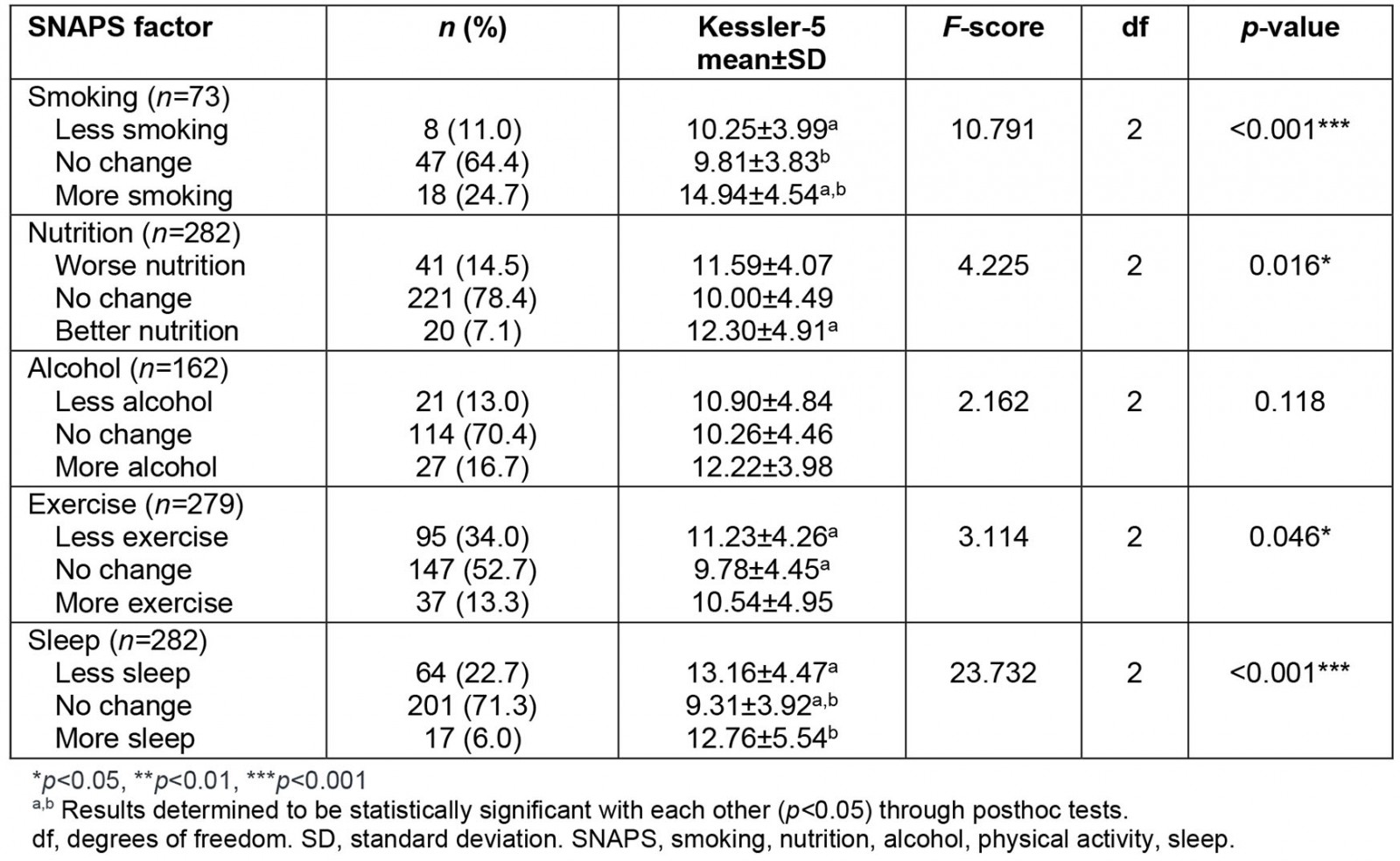
Table 5: Income change due to COVID-19 and perceived COVID-19 impact correlated with distress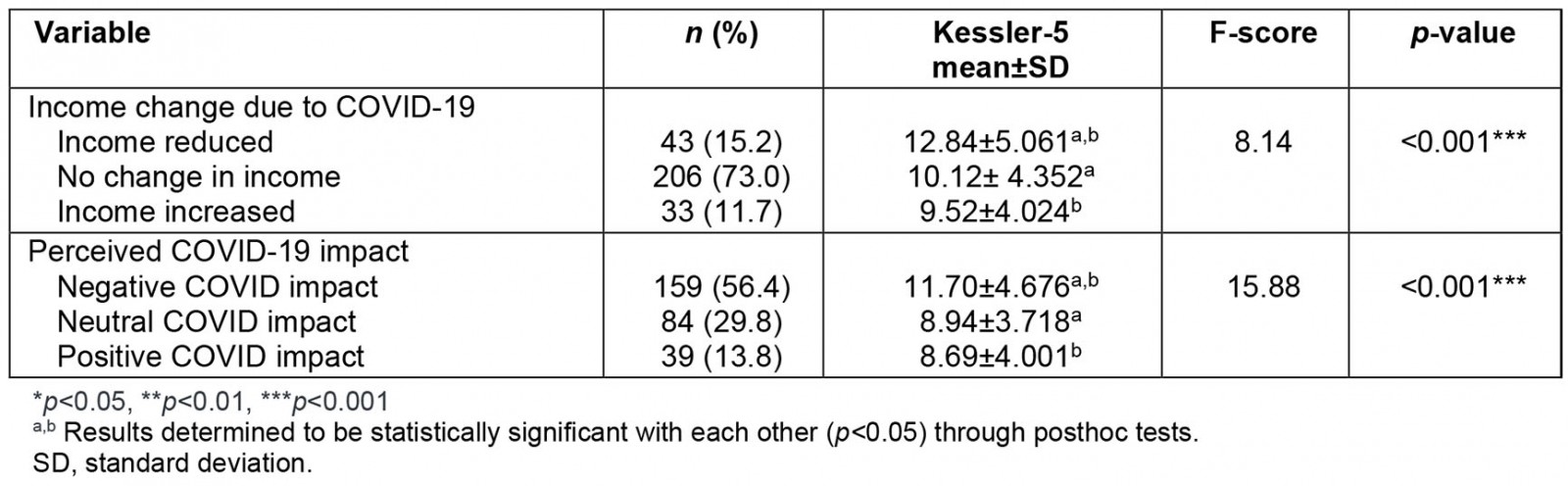
Table 6: Perceived COVID-19 impact correlated with Total Hope Score22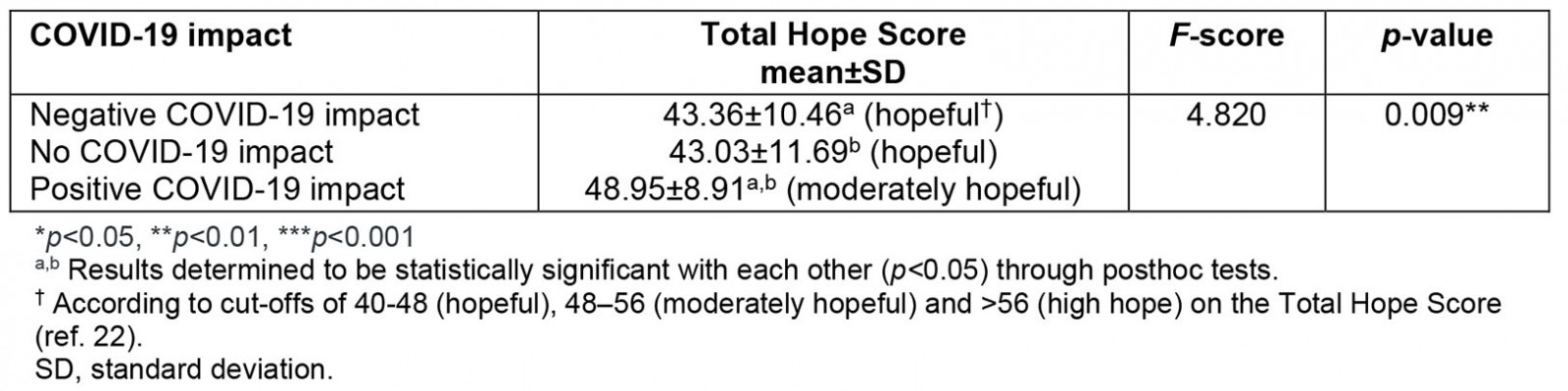
Association between subjective COVID-19 impact and lifestyle change, disposition, income loss and drought impact
There was no significant correlation between self-reported COVID-19 impact and gender (χ2=7.617, p=0.267), age (χ2=15.523, p=0.214) or occupation (χ2=12.946, p=0.373).
Current lifestyle was not significantly correlated with perceived COVID-19 impact, as measured in both individual lifestyle factors and the composite Global Lifestyle Score (F=2.130, p=0.121).
There was a significant association between subjective COVID-19 impact and sleep (Table 7). Interestingly, participants who reported decreased and also increased sleep were more likely to report a negative COVID-19 impact than those who reported no change, with the proportion highest in those reporting more sleep. The proportion reporting positive COVID impact was highest in those reporting more sleep. No other changes in lifestyle domains, including changes in nutrition, smoking and alcohol consumption, were associated with COVID-19 impact.
Notably, income change was significantly correlated with COVID-19 impact (df=4, n=304, χ2= 21.173, p<0.001), with a greater degree of income loss associated with a greater self-reported negative COVID-19 impact (Table 8, Fig3)
Interestingly, individuals who reported a negative COVID-19 impact were also more likely to report a negative impact from the drought pre-COVID-19 (χ2=30.361, p=0.005) (Table 9).
Table 7: Perceived COVID-19 impact correlated with changes in lifestyle behaviour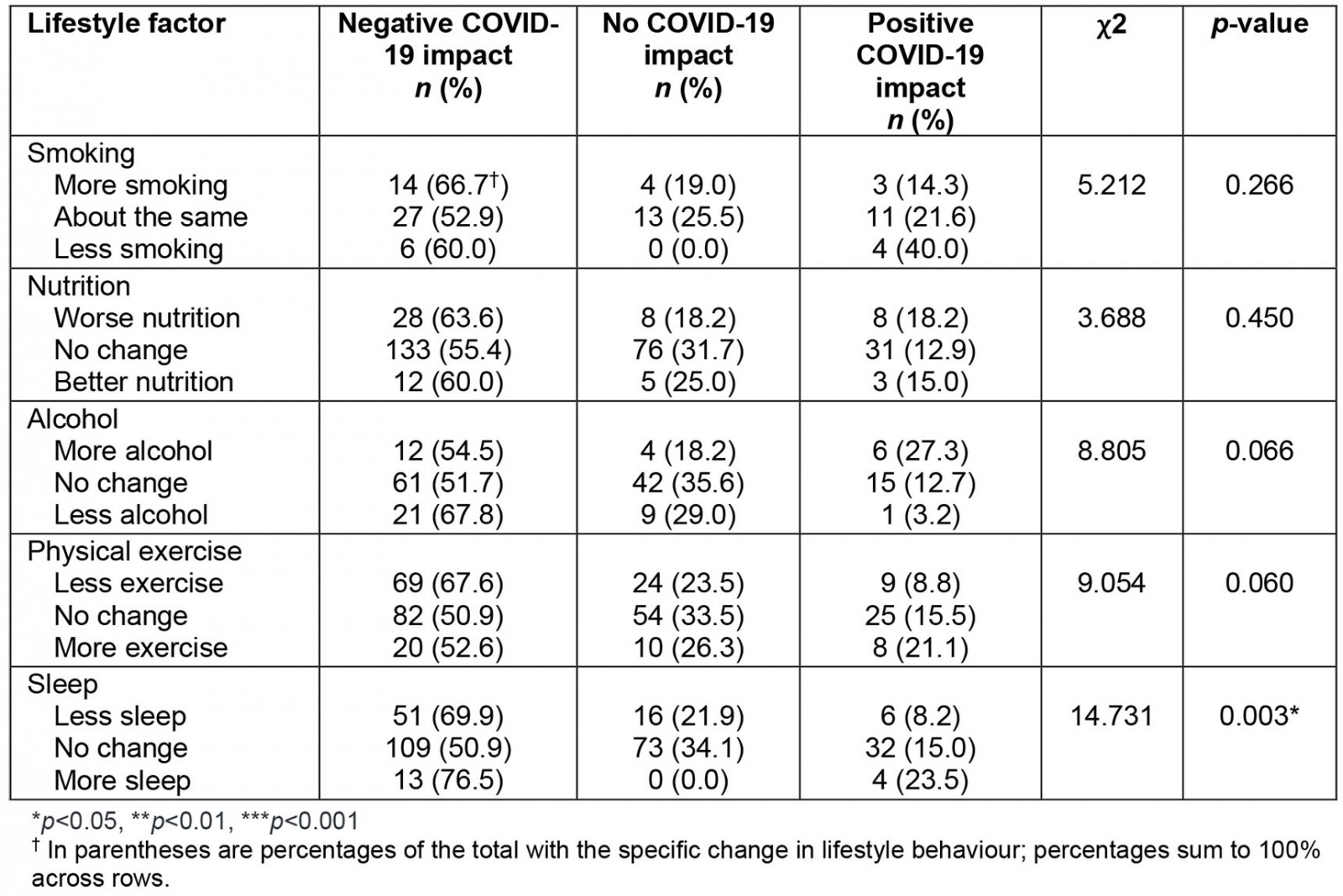
Table 8: Perceived COVID-19 impact correlated with income change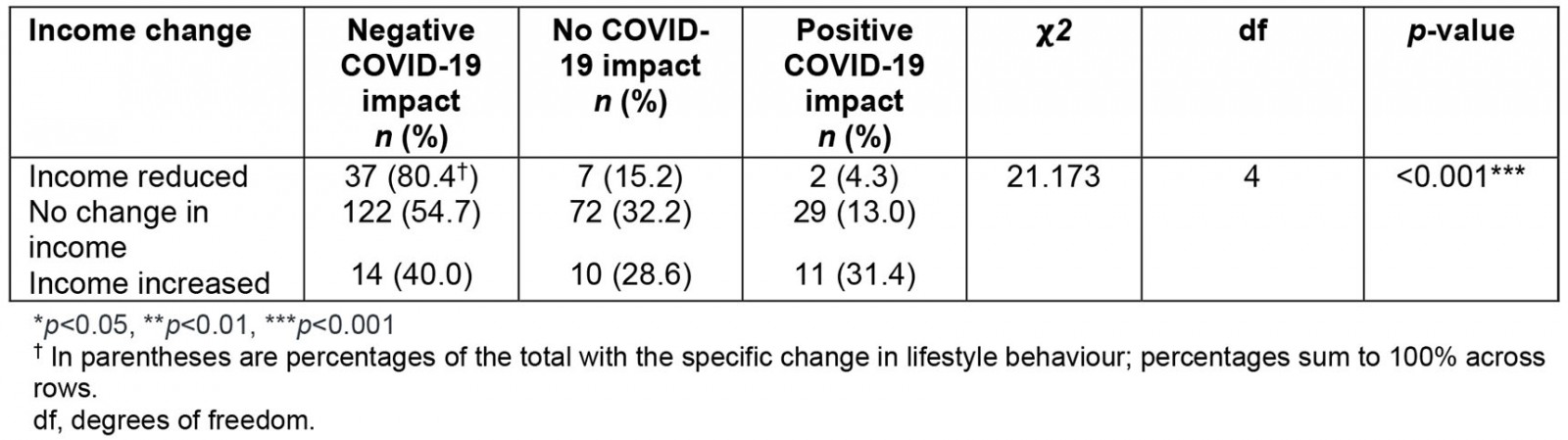
Table 9: Perceived COVID-19 impact correlated with perceived drought impact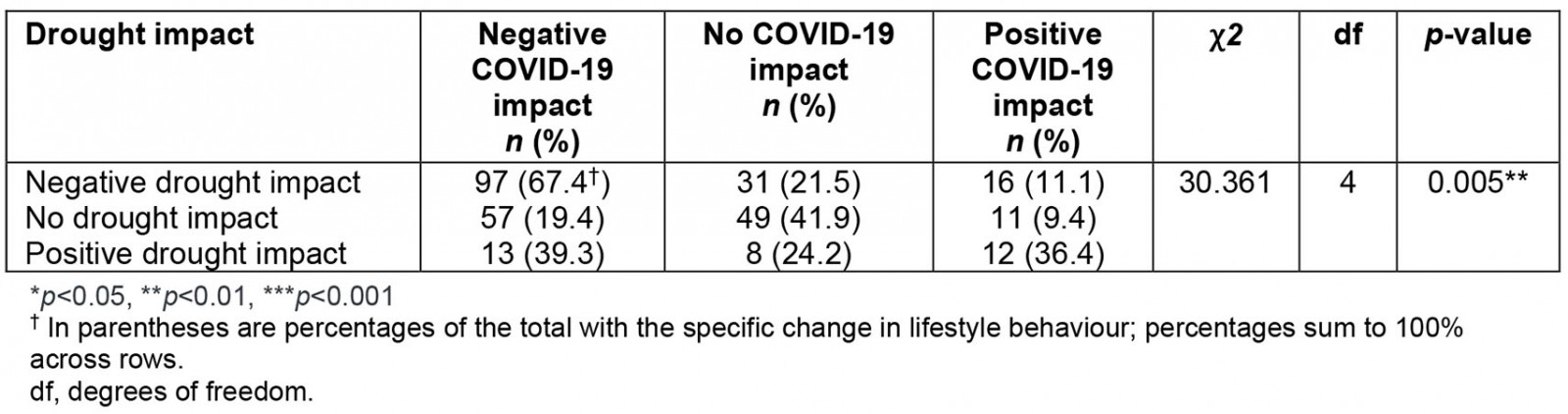
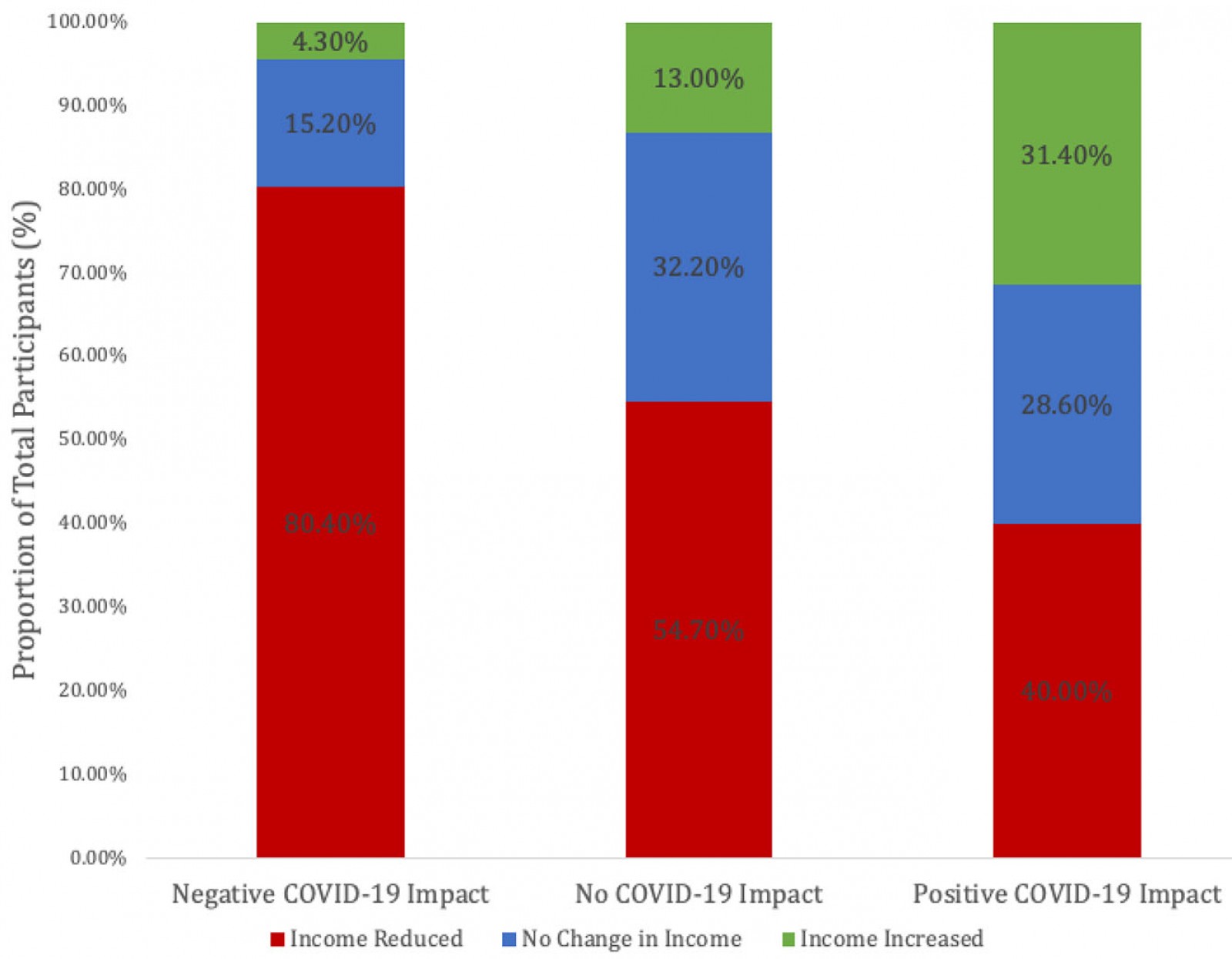 Figure 3: Perceived COVID-19 impact correlated with income change
Figure 3: Perceived COVID-19 impact correlated with income change
Association between cumulative subjective COVID-19 and drought impact with distress
The relationships of psychological distress with subjective impacts of COVID-19 and drought appeared to be cumulative (Table 10). As expected, the most distressed group reported adverse impacts from both COVID-19 and drought and were significantly more distressed than those who reported no adverse impact by either, or adverse impact by drought alone.
Participants who reported adverse COVID-19 impact were significantly more distressed than those who did not, both in the context of adverse drought impact and no adverse drought impact.
Participants who reported adverse drought impact were numerically but not statistically significantly more distressed than those who did not, regardless of their reported COVID impact.
Table 10: Association between COVID-19 impact and drought impact correlated with distress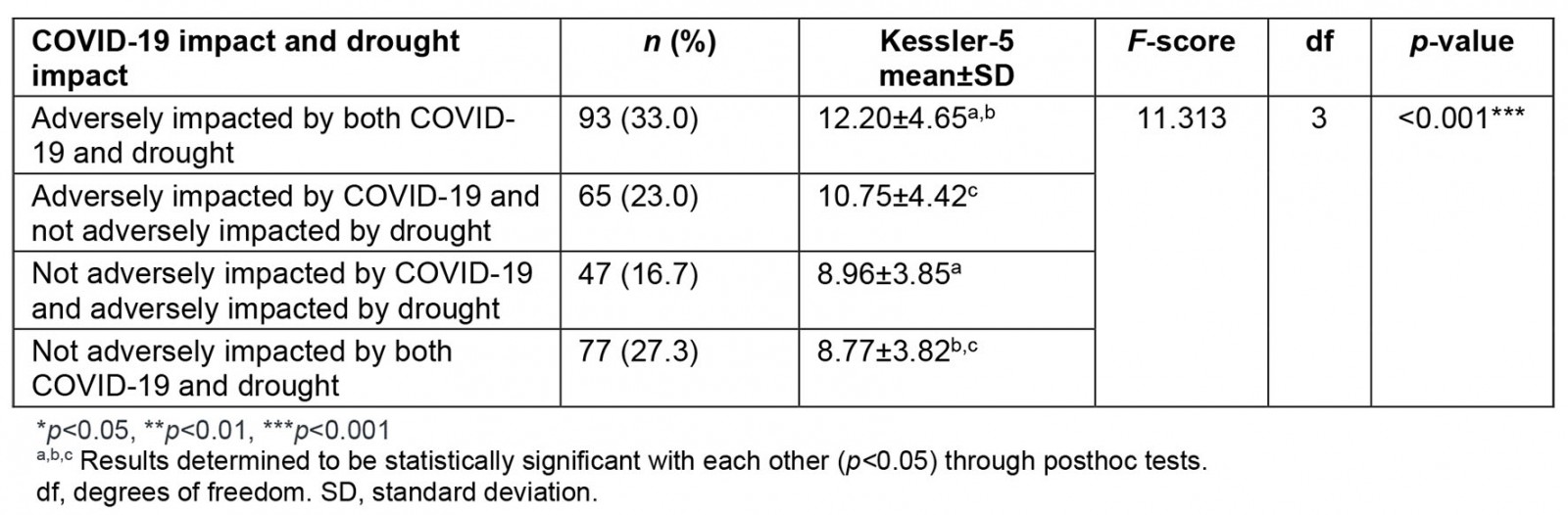
Participant comments
A total of 143 respondents (47.0%) provided qualitative responses to open-ended questions enquiring about the impact of COVID-19 on the respondent’s lifestyle domains of smoking, nutrition, alcohol, exercise and sleep, and life generally. Thematic analysis was performed, with themes, subthemes and representative quotes presented in Table 11.
Table 11: Thematic analysis of qualitative survey responses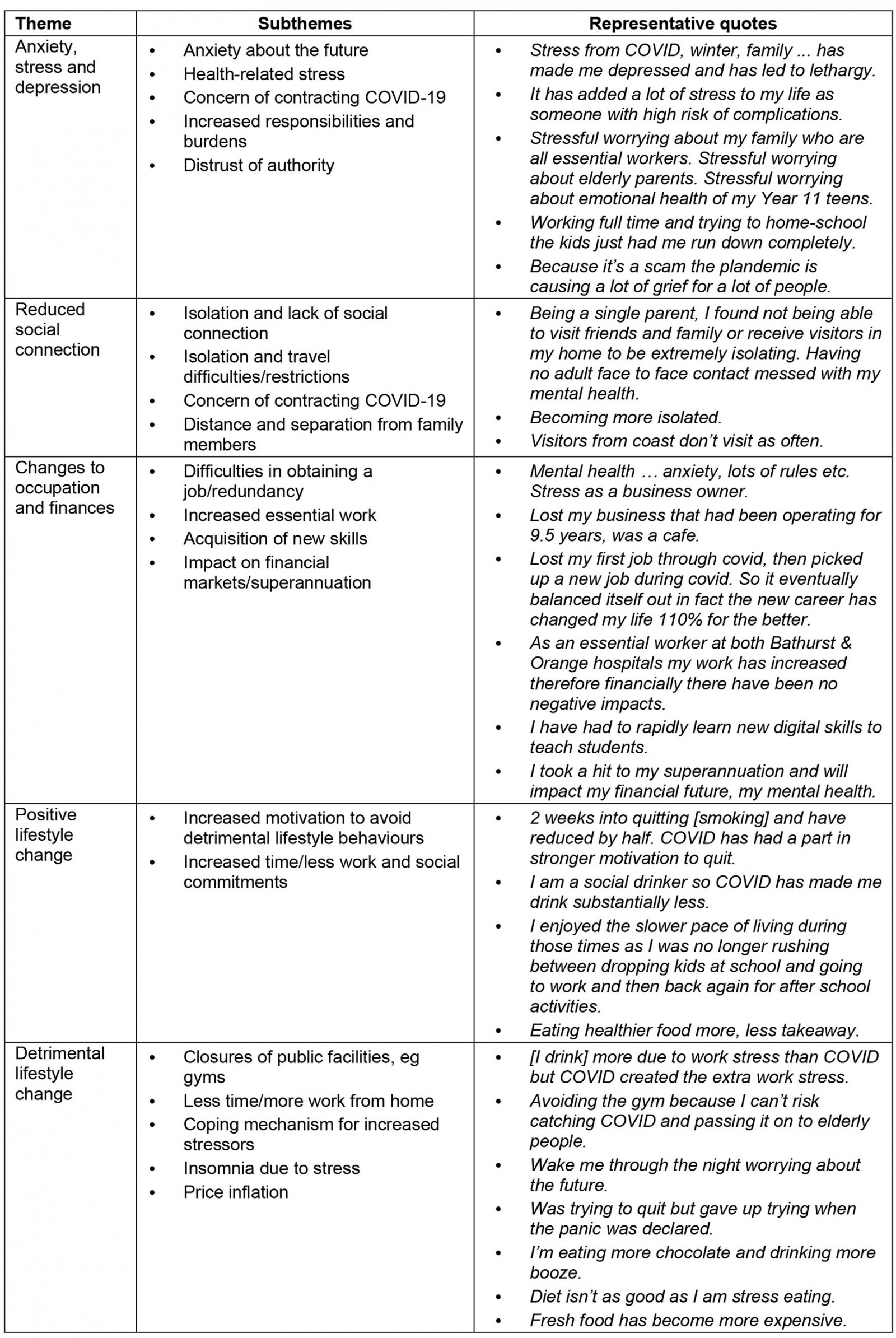
Anxiety, stress and depression: This theme incorporated five subthemes: anxiety about the future, health-related stress, concern of contracting COVID-19, increased responsibilities and burdens, and distrust of authority. Many identified an increased level of stress and anxiety due to work or COVID-19 restrictions, which among some respondents was amplified by health-related stress related to fear of complications from COVID-19. Increased responsibilities, such as the increased need for home-schooling children, were also identified as a salient factor underlying increased levels of stress. A small number of participants expressed a distrust of authority, with their responses often embracing conspiracy theories about the pandemic being fabricated, and about excessive control.
Reduced social connection: This theme incorporated four subthemes: isolation and lack of social connection, isolation and travel difficulties/restrictions, concern of contracting COVID-19, and distance and separation from family members. The general feeling from respondents was a negative impact on relationships and socialisation, partially due to public health restrictions on in-person gatherings, activities and venues, and concern of contracting COVID-19. Even though many restrictions were eventually eased, such as local and regional travel, some participants reported being separated from more physically distant family members for extended periods, and interstate and international travel remained restricted. Respondents identified a reduced sense of connection and support, which was occasionally related to increased feelings of depression.
Changes to occupation and finances: This theme incorporated four subthemes: difficulties in obtaining a job/redundancy, increased essential work, acquisition of new skills and impact on financial markets/superannuation. Most responses under this theme illustrated a negative impact of the pandemic on their employment and/or finances as it was associated with loss of occupation, reduced superannuation and mental stress surrounding pandemic-related restrictions. Some reported an increase in the hours of work they undertook, particularly those in essential roles such as in health care. Another occupation-related change was the acquisition of new skills, including digital skills and digital presentations, particularly in the field of education.
Positive lifestyle change: This domain incorporated two subthemes: increased motivation to avoid detrimental lifestyle behaviours, and increased time/less work and social commitments. Some respondents described a decrease in detrimental lifestyle behaviours, such as smoking and alcohol intake and the consumption of unhealthy food, driven by COVID-related shutdowns of social events and restaurants. Some participants attributed increased levels of exercise and a more relaxed pace of living due to increased time from less work and fewer social commitments. Some reported longer, better sleep and more naps while working from home.
Most respondents did not smoke; however, COVID-19 did provide one individual with the impetus to quit; one participant reported relapsing during COVID-19, but this may or not have been a causative relationship, and no respondents described taking up smoking. Most respondents viewed COVID-19 as negatively impacting their exercise, with the most significant limiting factors including fear of leaving home and closures/cancellations (eg of gyms).
Detrimental lifestyle change: This theme incorporated five subthemes: closures of public facilities, less time, coping mechanisms, insomnia due to stress, and price inflation. Participants reported that closures of public facilities like gyms and outdoor recreational spaces and fear of contracting COVID-19 from these spaces were direct contributors to reduced exercise, and this is consistent with the present survey’s findings that exercise was the most impacted lifestyle domain. Some participants had increased work burdens and hence less time for exercise and self-care. Other participants insightfully described actively turning towards maladaptive lifestyle behaviours as a coping mechanism, such as stress eating, drinking and smoking. Finally, several participants reported insomnia due to stress and anxiety, and some reduced their intake of fresh fruit and vegetables due to unaffordability.
In summary, the experiences of COVID-19 were variable and dependent on individual circumstances. This survey largely captured impacts on mental health, social isolation, occupation and finances, and both positive and detrimental lifestyle changes.
Discussion
This study examined the association between lifestyle behaviours (smoking, nutrition, alcohol, physical activity and sleep), lifestyle behavioural change during COVID-19, psychological distress, disposition, income and the reported perceived impact of COVID-19 in a rural Australian population.
At the time of survey, over a third of participants reported high–very high distress, substantially higher than the national average of 13% in 201829. Those with more detrimental lifestyle behaviours (lower GLS) reported higher levels of distress during the pandemic, particularly in relation to sleep and smoking. Given the well-established relationships between the SNAPS lifestyle domains and mental health, both detrimental current lifestyle behaviours and the adoption of new detrimental lifestyle habits during COVID-19 were expected to correlate with higher psychological distress, and vice-versa. However, exercise, inadequate sleep and active smoking were the only lifestyle behaviours found to be significantly correlated with psychological distress.
The study finding that those who had a high level of physical activity as measured by MET had a lower distress suggests that exercise may be a protective factor in the context of the COVID-19 pandemic. Physical activity has been shown in other studies to have an effect on reducing psychological distress30. Similar to these findings, Stanton et al found that sleep had the strongest correlation with depression out of all lifestyle factors7. Sleep is strongly associated with depression and the relationship is bidirectional, with sleep disrupted by depression, and sleep deprivation a major risk factor for developing depression8. The COVID-19 pandemic has been associated with widespread poor sleep among the general population, with healthcare workers strongly affected31. The positive association between smoking and psychological distress is expected, as there is a known bidirectional relationship between these two entities involving shared environmental causes and neurophysiological changes32.
Previous research has indicated that COVID-19 has had a significant impact on lifestyle behaviours, and this study confirms this in the rural population studied. It was found that a significant proportion of participants reported changes in each lifestyle domain, ranging from 21% with nutrition to 46% with exercise. More people reported negative rather than positive change across all domains. Exercise was also the most impacted domain in Stanton et al’s cohort in April 2020 during lockdown, with a total of 69% of respondents reporting both a positive and negative impact7.
As expected, negative lifestyle change in some domains (increased smoking and less exercise) were associated with increased psychological distress. Interestingly, both an increase and decrease in sleep were linked to increased distress. Unexpectedly, participants who improved their nutrition had significantly higher distress compared to those whose lifestyle remained unchanged. As with Ingram et al’s UK cohort study, no correlation between change in alcohol consumption and mood status was found, unlike other lifestyle risk factors, possibly confirming their hypothesis that this may reflect the positive effect that alcohol has on mood under certain social circumstances9. The unexpected increase in distress found among those that adopted healthier behaviours, particularly for nutrition, may reflect how some individuals with high distress perhaps attempted to improve their anxiety through lifestyle changes as a form of self-medication. Another theory borne out in the literature suggests that the process of adopting and maintaining a healthier lifestyle may itself cause distress33. However, this result contradicts Hu et al’s cohort where decreased vegetable, fruit and breakfast intake during the pandemic was associated with a lower subjective wellbeing34. Although more sleep may be positive for some individuals, the association between both an increase and decrease in sleep with distress is congruent with the well-established sleep disturbances of both hypersomnolence and insomnia in mental health conditions such as depression35. Sleep may have a unique relationship with distress.
Regarding perceived COVID-19 impact, over half of participants reported an overall negative impact on their life. This question was intended to capture the perceived overall psychological burden of the pandemic, including the effects of mandated restrictions on lifestyle, work and education, broader social changes and fear of contracting the disease itself. Those who felt negatively affected by the COVID-19 pandemic had higher distress levels. This is consistent with a large longitudinal study that reported that people without mental health disorders reported an increase in symptom severity on scales used to measure mental health compared to pre-pandemic levels, consistent with the hypothesis that COVID-19 may have directly caused poorer mental health outcomes36. Current lifestyle did not correlate with perceived COVID-19 impact, either as measured individual behaviours or as a composite global lifestyle score. This finding suggests that other factors such as reduction in income may be more dominant. Nonetheless, since detrimental lifestyle behaviours correlates with overall psychological distress, it remains important for mental health even in the context of additional stressors. Changes to sleep habits correlated with perceived COVID-19 impact, with participants reporting increased sleep also reporting the highest proportion of positive COVID-19 impact as expected, but there was also a significant signal for both decreased and increased sleep with negative perceived COVID impact, and this is consistent with the study’s finding that both decreased and increased sleep correlated with increased psychological distress. It is likely that a few chronically sleep-deprived participants who encountered reduced constraints of work and daily life on their sleep experienced a net positive effect, but generally participants reporting increased sleep were, if anything, more likely than their peers to also report negative COVID-19 impact, and this may reflect greater disruption to other aspects of waking life, or poorer sleep quality despite increased time in bed as has previously been reported37. It is notable that changes in other lifestyle behaviours (nutrition, alcohol and physical activity) both during and ostensibly due to COVID-19 did not correlate significantly, suggesting that these behaviours are not as strongly prioritised.
Notably, loss in income was correlated with both higher distress and greater self-reported COVID-19 impact. Economic recessions have been shown to have a devastating effect on mental health and, at the time of this survey, over 206 000 Australians were unemployed due to COVID-1938. A reduction in income was associated with increased distress and a greater negative self-reported COVID-19 impact in the participants. A recent large prospective, longitudinal study of over 34 000 participants found that patients who reported a decrease in income over a 3-year period were 30% more likely to develop a mood or substance disorder15. Furthermore, significant financial stress has been associated with increased interpersonal stressors, greater psychological distress and lower levels of psychological wellbeing39. Government policy directed towards financial prosperity of older women has been shown to improve mental health outcomes40. Government payments such as JobKeeper and JobSeeker may have protected against more severe impacts on mental health.
The association between perceived COVID-19 impact and drought impact within the same population suggests that there are common mechanisms or vulnerabilities that may impact rural populations, including impact of external stressors on income. Farmers in NSW throughout the drought experienced significant distress about the effects of the drought on themselves, their families and their communities18. Specifically, farmers who experienced financial hardship or were isolated from their communities by virtue of working in remote areas were at particular risk of drought-related stress18. Similar risk factors may have been triggered by the COVID-19 pandemic in 2020, resulting in the found correlation between drought-related stress and self-reported COVID-19 impact.
This study found that COVID-19 is independently associated with higher levels of distress among people having previously experienced drought. Some international data suggest the exposure to multiple disasters can adversely affect physical health, mental health and wellbeing, greater than the impacts seen in those who have only been exposed to one disaster41. This was borne out in the present study, with participants reporting adverse subjective impact from both events being the most distressed, more so than those reporting adverse impact from either event alone. However, only negative COVID-19 impact was statistically significantly associated with cumulatively greater distress; the weaker non-significant numerical trend seen for negative drought impact may reflect the healing and recovery process in action compared to the active challenge of COVID-19.
Disposition (low hope) was also correlated with higher distress and greater perceived COVID-19 impact. Distress is a complex phenomenon and lifestyle, lifestyle changes, perceived COVID-19 impact, income loss and disposition were identified as correlates. Analysing their relative independent significance would be a direction for future research.
Strikingly, when lifestyle factors were pooled into the composite GLS, more detrimental lifestyle behaviours were associated with higher levels of distress. This strongly supports the hypothesis that a GLS may have utility in predicting known correlates of lifestyle behaviours, including psychological distress. The GLS has potential utility in providing an overall lifestyle assessment. It may assist health professionals treating those with negative COVID-19 experiences and those with other mental health issues in offering targeted lifestyle interventions.
Study limitations and future directions for research
The limitations of this study included the small sample size, predominantly composed of participants from one rural town in Australia with access to the internet on a smartphone or computer. There was a large skew towards older female participants, which is not reflective of the rural Australian population as a whole. The inability to distribute the survey in person limited the study population because the online groups surveyed had a relatively inactive younger population, and the authors note that only 73% of households in the region have home internet access, which is the lowest level nationally20. It also excluded individuals without access to the internet. Furthermore, the study design did not differentiate between varying social and demographic subgroups, including parental status; for example, Glenister et al, studying rural women in 2020, during COVID-19 reported an increase in alcohol only among women with children at home as opposed to those without14. Not taking these subgroups into account may have confounded the correlations between lifestyle behaviours and COVID-19 impact as it may have obscured underlying correlations in opposite directions. Future research into the impact of COVID-19 on younger Australians and other subgroups should consider this. A further limitation of this study is that pre-existing mental health conditions were not assessed.
While the focus on Bathurst and Orange (Central Tablelands region) and Condobolin is a non-representative sample of the Western NSW region and rural Australia more broadly, the university has strong community goodwill in these communities, making the results largely locally applicable, and these communities also had relatively similar exposures to drought, which may not have been true of a larger but more heterogeneous target population.
A further limitation of this study is that it relied on self-reported data that may have been incorrectly recalled or exaggerated and cannot be independently verified. In addition, cross-sectional studies such as these make it difficult to delineate cause and effect. For example, lifestyle change and COVID-19 impact may work bidirectionally to influence each other. Future research may consider a longitudinal study to address these limitations.
Drought-affected populations may have unique vulnerabilities. As those with perceived increased drought impact were more likely to report increased COVID-19 impact, a direction for future research is the extent to which drought relief initiatives may build resilience within communities to prepare them for future crises.
The correlations of Total Hope Score with distress and perceived COVID impact, while statistically significant, may not be clinically significant as it was analysed as a continuous variable without using previously validated categories. On the other hand, these categories have not been validated in this study population.
As part of this research, a GLS was developed on evidence-based findings in each of the five lifestyle domains. This scoring system has not been validated outside of this study. Future research could therefore refine the GLS into a clinically useful scoring system that could be applied to other established lifestyle-dependent conditions, from psychological conditions to physical health conditions such as cardiovascular disease and diabetes. Another avenue for research is whether modification of lifestyle factors is a useful intervention for reducing distress in the context of a stressor such as the COVID-19 pandemic.
Conclusion
This study found disproportionately high rates of distress among rural Australians during the COVID-19 pandemic, linked to low GLS, worsening lifestyles and loss of income. Common vulnerabilities may drive distress given the correlation between negative impact from disparate stressors of the recent drought and COVID-19.
The GLS has been shown to have utility in predicting distress and may have further clinical applicability for primary healthcare settings if validated against physical and psychological parameters.
These findings may have important implications for health professionals in providing a greater understanding of COVID-19 and its effect on mental health and lifestyle among patients, and to direct their management accordingly to improve patient outcomes.