Introduction
Depression is the commonest mental health problem during pregnancy1. In low- and middle-income countries (LMICs), 15.9% of antenatal and 19.8% of postnatal women are estimated to have depression1. It can lead to numerous adverse outcomes in the mother, baby and the family, maternal suicides being one of the most devastating1-5. Maternal suicides have been identified as one of the leading causes of maternal deaths across the world6-8. Suicide has been described as 'the tip of the iceberg' because more women would demonstrate self-harm behaviours and experience suicidal thoughts during pregnancy and postpartum8-10.
Maternal depression is more common in LMIC settings, but its prevention and treatment often receive less priority in health agendas1. Help-seeking behaviours of people may also lead to under-recognition and delayed treatment for the condition11-13. Therefore, it is very important to recognise the help-seeking behaviours and possible factors that may shape such behaviours to identify potential strategies to ensure early detection and management of the condition.
Help-seeking first emerged as a concept within illness behaviour. In one of the earliest references, Mechanic described illness behaviour as ‘the manner in which persons monitor their bodies, define and interpret their symptoms, take remedial action, and utilise various sources of help as well as the more formal healthcare system’14. Later, help-seeking evolved to refer to the dynamic process of problem-focused coping, which relied on external assistance from other people, including health professionals and others15. However, the concept of help-seeking is a complex construct and has been used and assessed within heterogeneous definitions.
Rickwood and Thomas suggest, ‘In the mental health context, help-seeking is an adaptive coping process that is the attempt to obtain external assistance to deal with a mental health concern’15. Reviewing the available literature, they came up with a conceptual framework to measure help-seeking for mental health problems. In this model, help-seeking is described under five main constructs: help-seeking process, source, time frame, intention and type of help. Help-seeking process includes three components: general attitude, intention and behaviour. Only the latter two are regarded as representations of the active process of help-seeking. According to planned behaviour action theory, attitudes influence intentions, which influence the behaviours16. Therefore, identifying help-seeking intention would help to predict the actual behaviour. Seeking instrumental support (such as financial assistance, child care help), informational support (such as health-related and referral information), affiliate support (peer support) and emotional support from informal sources (family and friends), semiformal sources (health professionals who do not have a specific role in mental health), formal sources (mental health professionals) and self-help resources are all considered as help-seeking. When preferred help-seeking sources are identified, they can be empowered to provide responsible and empathic responses to a pregnant woman seeking help. Policy changes and modifications to practice guidelines can also be implemented to improve access to appealing sources.
To improve help-seeking, knowledge on factors influencing this behaviour is also valuable. The model suggested by Rickwood and Thomas briefly describes possible influences such as health literacy and identification of symptoms. The Health Belief Model is another popular and detailed model used for understanding why people would engage in health-related behaviours17,18. According to the health belief model, the higher the perceived personal susceptibility and seriousness of a particular health condition, the higher the perceived threat. Higher perceived susceptibility would make people comply with recommended health-related behaviours for prevention, treatment-seeking and control of the said health condition. Similarly, perceived benefits and constraints for the recommended behaviour also affect its uptake. Modifying factors and cues to action are other components shaping a behaviour.
Sri Lanka is a middle-income country with a strong public health infrastructure prioritising maternal health. Despite that, postpartum depression (27.1%) and antenatal depression (10.4–22.8%) are widely prevalent in the country19-22. Maternal suicides are a leading cause of maternal deaths23-27. Suicidal ideation had been reported among 2.9–6.9% of pregnant or postpartum women in remote areas of the country19-21. Anuradhapura district, where 94.1% of the total population is rural, has very high suicide rates, and suicide is reported as the leading cause of maternal deaths27. Despite this, mental health services are limited, and making professional help more accessible and acceptable for pregnant and postpartum women experiencing mental health issues has not been recognised as a priority.
Not receiving appropriate help is a main risk factor for adverse health outcomes of depression and suicidal ideation in pregnant or postpartum women10,28,29. Understanding the decision-making paradigm in help-seeking for maternal depression and suicidal ideation could help design interventions to promote timely, appropriate and effective help-seeking in these issues, which would in turn help prevent the associated morbidity and mortality. Therefore, this study looked at the help-seeking intention, preferred sources and factors influencing help-seeking for depression and suicidal thoughts among pregnant women in rural Sri Lanka.
Methods
A cross-sectional study was conducted in field antenatal clinics in Anuradhapura, Sri Lanka, from 7 August 2018 to 7 September 2018. The district is divided into 20 health divisions under a medical officer of health (MOH). Field antenatal clinics at the village level are conducted through the office of MOH. Attending the clinics at least once was reported by 96% of antenatal women30.
Pregnant women with a gestation period of more than 12 weeks and visiting antenatal field clinics in Anuradhapura district were included as the study population. Women with earlier (<12 weeks) periods of gestations were excluded because morning sickness, which is more common during the first trimester, may have made it difficult for women to participate.
Since help-seeking intention for depression among Sri Lankan antenatal women is unknown, it was assumed as 50% for obtaining the maximum estimation. The minimum sample size required for the study was calculated using the following formula (minimum sample size (n), level of confidence 95% (z) 1.96, precision (d) 5%)31.
n = (z/d)2p(1 – p)
As cluster sampling was intended, design effect was selected as 1.5 as some homogeneity between clusters is expected. A response rate of 95% was applied. The estimated minimum sample size was 606.
Multistage cluster sampling with probability proportionate to size was used to obtain the sample. Five out of the 20 MOH areas in the Anuradhapura district were selected using a random number sequence. The number was limited to five, considering the feasibility. Clusters were selected from field clinics. Cluster size was determined to be 25, based on previous clinic attendance data in selected MOH areas. Based on the cluster size and sample size, 25 clusters were required for the study. All the field clinics (n=43) in the selected MOH areas were listed in alphabetical order. The size of the clinic was determined by the number of second- and third-trimester pregnant women attending each clinic during June 2018. The probability proportionate to size method was used to select 25 clusters. A total of 25 consecutive, consenting pregnant women fulfilling eligibility criteria from each clinic were recruited for the study.
Development of the study tool
Considering the sensitive nature of questions and high female literacy rates (94.6%) in the district32, a self-completed questionnaire was used. A vignette-based approach was selected for the study.
Prior to the development of the tool, a comprehensive literature search was conducted in March 2018 to identify global evidence on help-seeking for peripartum depression. Electronic databases were searched using PubMed, Google Scholar and Sri Lanka Journals Online. In addition to this, a hand search was conducted to identify non-indexed articles. Bibliography of Medical Literature 1980–2005 compiled by Post Graduate Institute of Medicine (PGIM) Library, Colombo, Sri Lanka Medical Index and PGIM repositories were searched to identify local literature. In addition, the titles of theses and dissertations submitted to PGIM were hand searched. Removing duplicates, 192 articles were retrieved, and after the title and abstract review, 87 articles were identified for full-text review. Only one local study regarding the help-seeking for mental health issues in pregnancy could be identified, which looked at the husband's intention to seek help for his postpartum wife. Findings from these studies were combined with the framework for assessing mental health help-seeking suggested by Rickwood and Thomas15, the health belief model17,18 and the planned behaviour action theory16 to develop a conceptual framework for this study (Fig1). This was used to develop the study tool.
A vignette describing the experience of ‘Ama’, a postpartum mother (baby aged 1 month) who was experiencing symptoms of depression (without suicidal thoughts) is given in part A. In part B, the vignette was modified as the same mother was experiencing frequent suicidal thoughts.
To increase the internal validity, a vignette should be constructed following assessment of existing literature, validated by a panel of experts and pretested33. This vignette was designed based on the clinical symptoms described in the Diagnostic and Statistical Manual diagnosis criteria for peripartum depression34. The experience of women with peripartum depression presented in scientific literature and local social media groups also influenced the design of the vignette and the questions. Opinions of reproductive-age females in the same community (n=8), midwives (n=8), and doctors in the public health sector (n=5), were also considered during the process.
Help-seeking intention was measured by asking participants about their intended action if they were experiencing a situation similar to the vignette. Deciding to wait and see if the symptoms would resolve13,35,36, trying self-help strategies such as engaging in religious activities, exercising36-39 and ignoring the symptoms as long as possible37,39,40 had been described in global literature as intended actions when experiencing depression during the antenatal or postpartum period. ‘Just ignore it’, ‘try to figure out a solution by myself’, ‘wait for some time and if it persists, seek help from someone’, and ‘seek help from someone right now’ were the options provided in the current study to identify the help-seeking intention.
Open-ended questions were used to identify the first choice for seeking help for parts A and B. A Likert scale was used to rate the probability of seeking help from selected informal, semiformal and formal sources if a similar situation occurred. Husband35,36,41-45, family (mother, parents in-law)41,42, friends or neighbours35,41,42,46, general practitioners41,47-49, obstetricians38,47,48,50, psychiatrists38,41,45,47,49, traditional doctors13,36,42, internet or social media35,42,43,47,49,51, the public health midwife (PHM)49, the MOH, Kattadiya (‘witch doctors’)13,36,45 and priests36,39,45,52 were selected to be added in the tool based on discussions with local stakeholders and global and local scientific literature on help-seeking for different conditions.
To assess the perceived severity of symptoms, statements on normality (‘It is normal. Almost everybody may feel the same during this period’), spontaneous resolution (‘It is bit abnormal but it will resolve on its own very soon’), the possibility of symptoms of depression being an illness (‘It is possibly a mental disease’) and possible danger of suicidal thoughts (‘It indicates a possible risk for her life’) were provided. These statements emerged from multiple research studies and were adopted for the cultural context35,39,53-56. A five-point Likert scale was used to assess agreement to each statement. Responses of ‘agreed’ and ‘strongly agreed’ were combined to indicate 'having a particular perception'. The perceived probability of respondents having a mental health problem during the antenatal or postpartum period of current pregnancy was marked in an adjective rating scale.
Partner's response is a determinant for the help-seeking behaviour of women45,57. It has been shown that the partner helps women conceptualise their problem and supports seeking information and help58. A partner's encouragement to seek help from family, a midwife, mother support groups and the internet has been described as a facilitator for help-seeking40,59,60. Similarly, lack of support from family and friends has been a barrier to seek help from professionals13. Therefore, this study wanted to assess the perceived benefits and constraints from help-seeking from the husbands, another household member available for helping and the PHM. The perceived response of another family member (when available) was added to the questionnaire because a significant proportion of women in this community were not living with their husbands due to employment issues. The perceived likelihood of receiving selected responses was recorded on a five-point Likert scale. Responses given as ‘likely’ and ‘very likely’ were combined to indicate 'perceived likely'. Responses given as ‘very unlikely’, ‘unlikely’ and ‘neutral’ were considered as 'perceived unlikely'.
Lack of proper knowledge and understanding about peripartum depression13,40,61, and lack of knowledge about available resources and options13,37,61-63, were barriers for help-seeking. Therefore, knowledge on treatment for peripartum depression was also assessed.
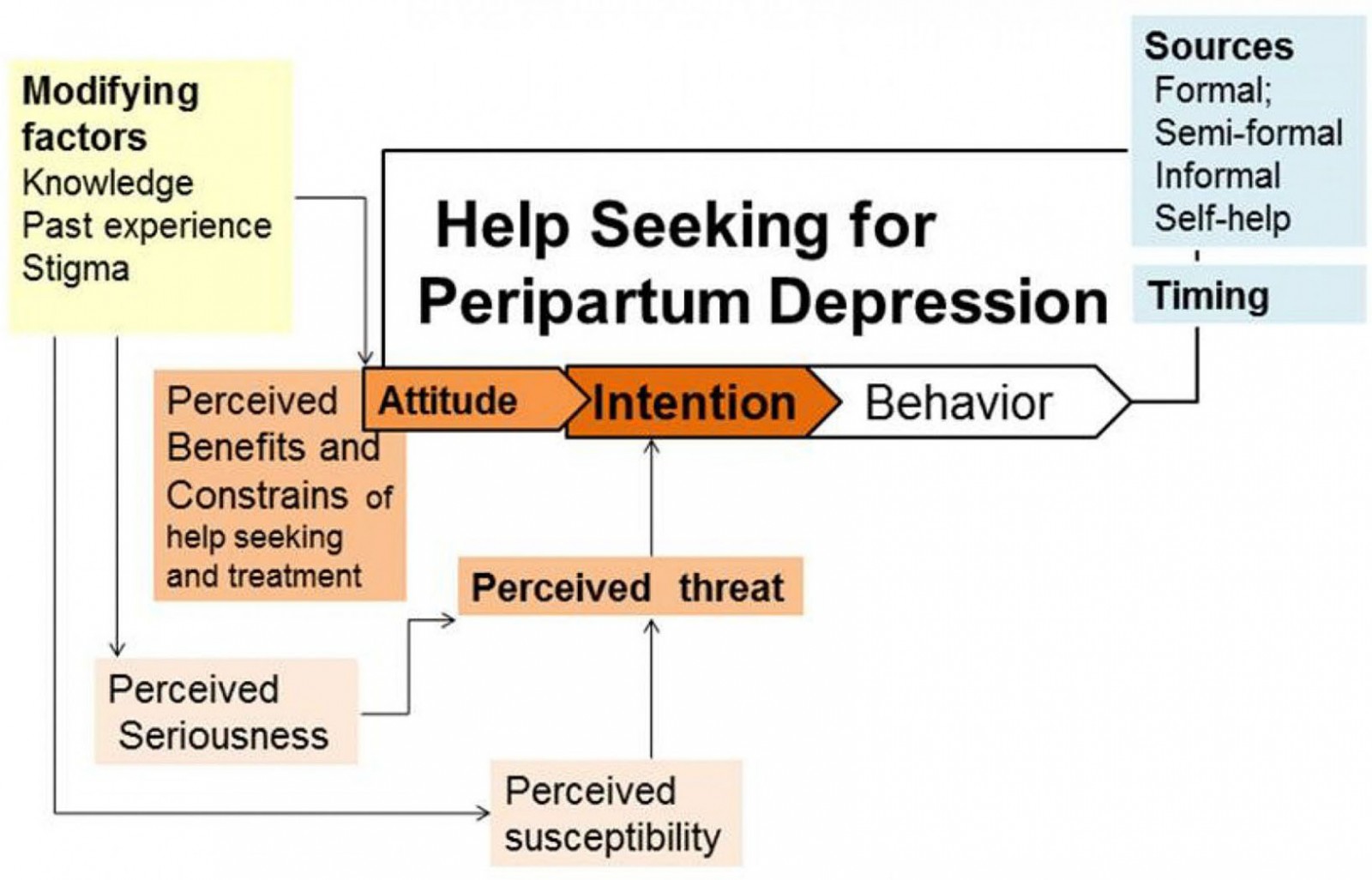 Figure 1: Conceptual framework for predictors of help-seeking intention for peripartum depression among pregnant women in Anuradhapura, Sri Lanka.
Figure 1: Conceptual framework for predictors of help-seeking intention for peripartum depression among pregnant women in Anuradhapura, Sri Lanka.
Validation of the tool
Expert validity for the vignette and the questionnaire was obtained from a panel of experts consisting of a consultant psychiatrist, a consultant community physician, a medical anthropologist, a social scientist, two MOHs and a panel of PHMs. The domains looked at were clinical validity, relevance to the local setting, whether it is comprehensible, and cultural appropriateness.
Cognitive validation of the questionnaire was conducted with 10 pregnant women admitted to the obstetric ward of the Teaching Hospital Anuradhapura, the main hospital for the district, including women from different socioeconomic and demographic backgrounds. Pregnant women were asked to read the vignette and verbally answer questions in the tool. Then the thought process of respondents in giving a particular answer was assessed using probing questions on three aspects: comprehension of key phrases in the question/vignette, the applicability of the question to the community and sensitivity of the question/vignette. Answers were documented, and the questionnaire was changed accordingly. The questionnaire was then pretested among 10 pregnant women admitted to the Teaching Hospital Anuradhapura. Pretesting provided positive feedback.
The original vignette and the questionnaire were developed in Sinhala and were translated to English and Tamil by professional translators. The consensus was obtained from three health professionals whose first language was Tamil regarding the Tamil translation.
Data collection
Data were collected by 10 undergraduates led by an MBBS qualified physician. Data collectors were trained to obtain informed consent and to assist women who needed help filling out the questionnaire. Women who showed signs of distress when filling out the questionnaire and those who mentioned experiencing suicidal ideation were identified and immediately contacted by the physician in a privacy-ensured manner. They were referred for further assessment and treatment depending on the severity of symptoms and the participant's preference. After completing data collection, all participants were provided with a health education leaflet (in their preferred language) about peripartum depression and available sources they could obtain help from, if needed.
Participants were given a structured introduction before data collection to minimise the social desirability bias. They were reassured that identification information would not be collected in the questionnaire and responses regarding perceptions would not be checked when they returned the completed questionnaire. They were also informed about the value of providing responses genuinely representing their perception and thoughts without worrying about being right or wrong. The data collectors assisted participants who could not complete the questionnaire by themselves.
Data were entered with a single-entry method. Physical copies were stored securely, and the database was stored using password protection with the principal investigator.
Data analysis
Data were analysed using the Statistical Package for the Social Sciences v22 (IBM; http://www.spss.com).
Ethics approval
The ethics review committee of the Faculty of Medicine and Allied Sciences, Rajarata University of Sri Lanka, approved the study (ERC/2018/19). Informed written consent was obtained from all participants.
Results
A total of 624 pregnant women aged 17–44 (mean 29, standard deviation 5) participated in the study. The majority were multiparous (n=376, 65.4%) and had heard about antenatal or postpartum depression (n=525, 86.2%). Six reported having frequent suicidal thoughts during the preceding week. Characteristics of the participants are shown in Table 1.
The proportions of participants with help-seeking intention for symptoms of depression and suicidal thoughts, respectively, were 64.1% and 65.3% (Table 2). The intended waiting period ranged from 2 days to 1 year (mode of 30 days) and from 1 day to 2 years (mode 30 days) among those who responded as intending to wait before seeking help for depression and suicidal thoughts, respectively.
The husband was the first choice of help for the majority of respondents, for both depression (n= 284, 56.3%) and suicidal thoughts (n=248, 62.8%). Mother (n=95,18.8%), any other family member (n=21, 4.2%), PHM (n=77, 15.3%), a doctor (n=10, 2%) and others (n=17, 3.4%) were also reported as the first choice of help for depression. Mother (n=80, 20.3%), any other family member (n=23, 5.8%), PHM (n=27, 6.8%), a doctor (n=10, 2.5%) and others (n=7, 1.8%) were reported as first choices of help for suicidal thoughts. The first choice of help being outside the family was significantly lower for suicidal thoughts compared to symptoms of depression (McNemar’s test p<0.001).
If they were to seek help for symptoms of depression, 90.5% (n=555) said they would probably or definitely seek help from their husbands. While family members showed a high acceptance rate as a help-seeking source, a PHM was more acceptable than any doctor (Table 3). If seeking help for suicidal thoughts, 71.1% (n=406) of the participants said they would probably or definitely seek help from their husbands (Table 3). The intended process for seeking help from a doctor or midwife for symptoms of peripartum depression is shown in Table 4.
The possibility of themselves developing a mental illness during the current pregnancy or postpartum period was perceived as impossible (n=379, 65%), may be possible (n=177, 30%), possible (n=19, 3%) and highly possible (n=8, 2%). Only half of the participants believed that the vignette described a possible illness (n=296, 49.9%) or that suicidal thoughts could be life-threatening (n=269, 48%). A total of 45.3% agreed with both these possibilities. More than a third also believed that the symptoms (n=222, 37.6%,) and suicidal thoughts (n=196, 34.6%,) are normal and a common experience during the pregnancy and postpartum period. Perceptions of spontaneous resolution of symptoms (n=35, 59.3%), and suicidal thoughts (n=256, 45.5%) were also widely prevalent (Fig2).
Positive responses for help-seeking were perceived as likely by the majority. Only a smaller proportion of women perceived that negative responses were likely to be received if they sought help from their husband, family members or a PHM (Fig3).
Regarding the treatment for peripartum depression, 120 (21.2%) believed that there is no cure and lifelong treatment is needed, 265 (45.5%) believed that it requires admission to hospital, and 68 (11.9%) believed that breastfeeding has to be stopped during the treatment period. A total of 412 (70.7%) believed some women are very strong so that they can control the symptoms without treatments.
Table 1: Participant characteristics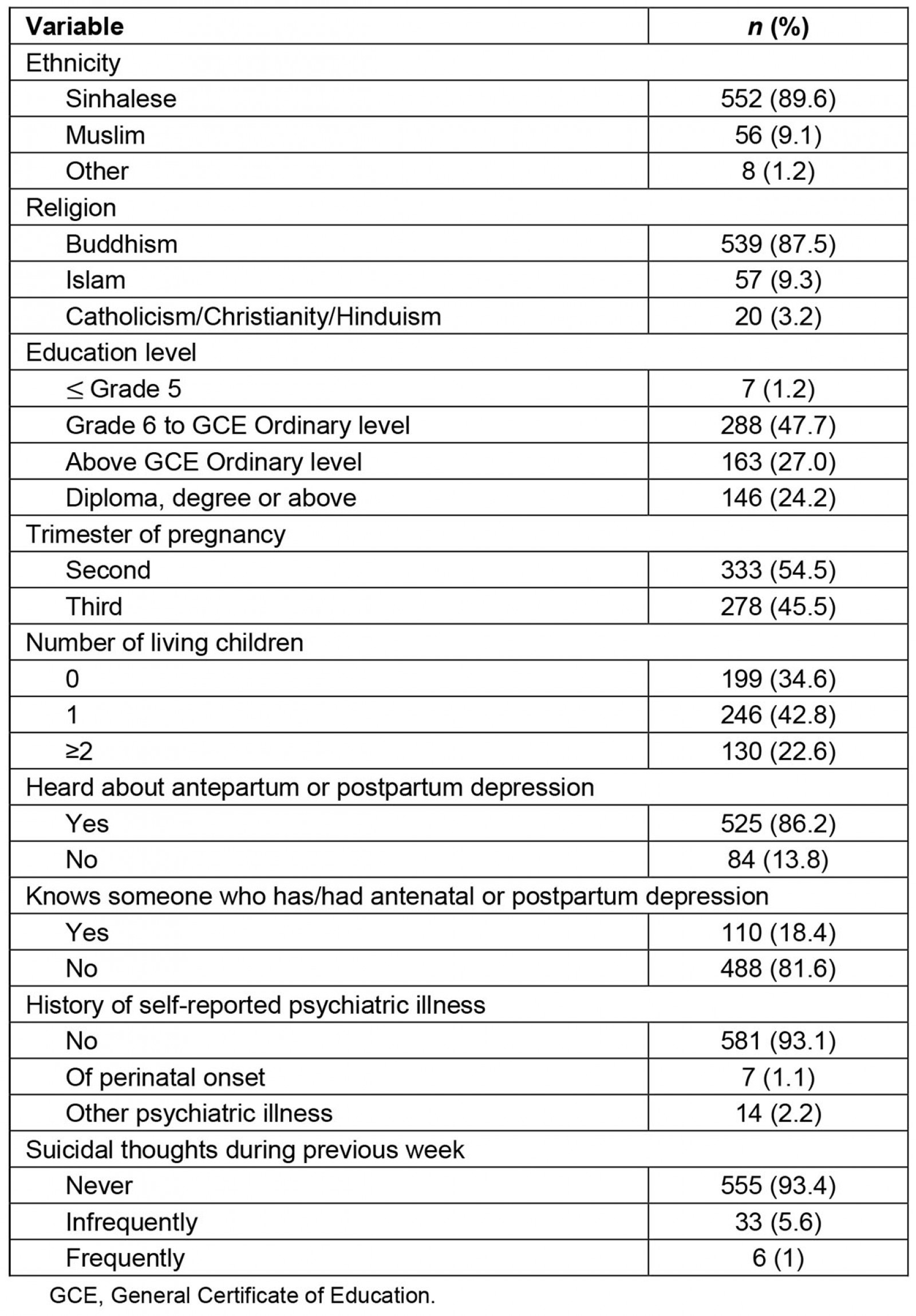
Table 2: Help-seeking intention for symptoms of peripartum depression and suicidal thoughts among pregnant women in Anuradhapura, Sri Lanka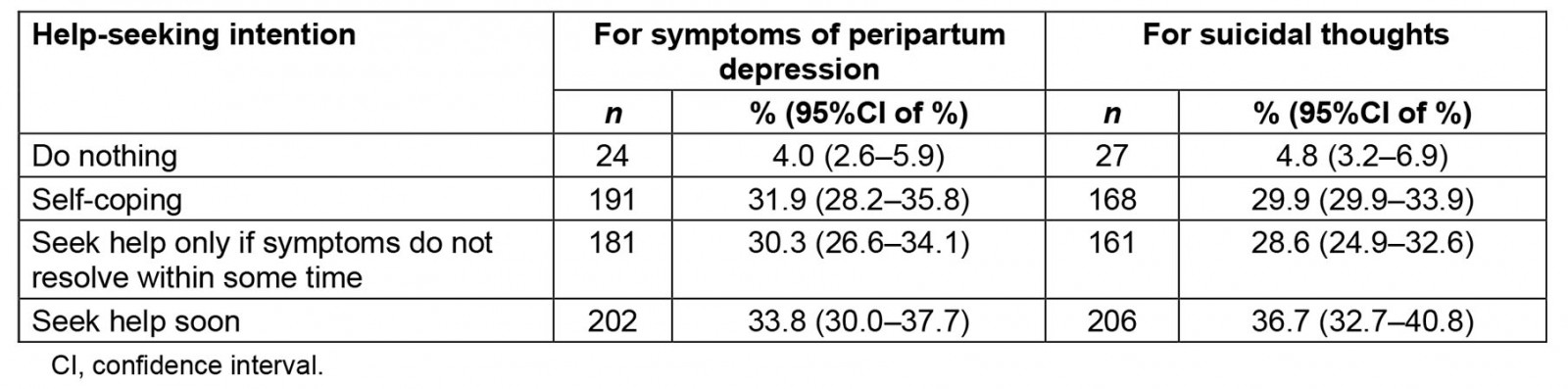
Table 3: Probability of seeking help for symptoms of peripartum depression and suicidal thoughts from selected sources among pregnant women in Anuradhapura, Sri Lanka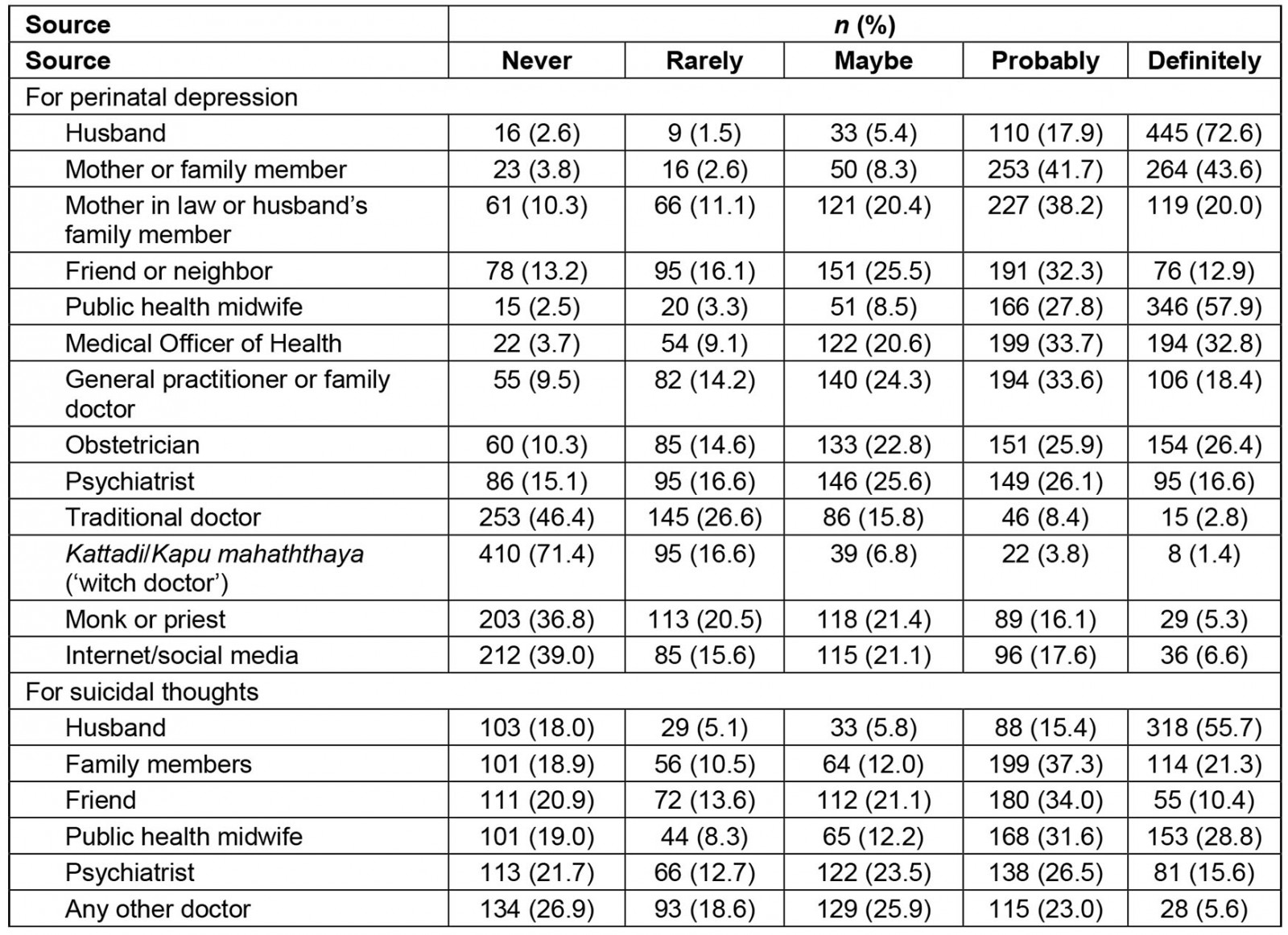
Table 4: Intended process for help-seeking from a doctor or midwife for symptoms of peripartum depression among pregnant women in Anuradhapura, Sri Lanka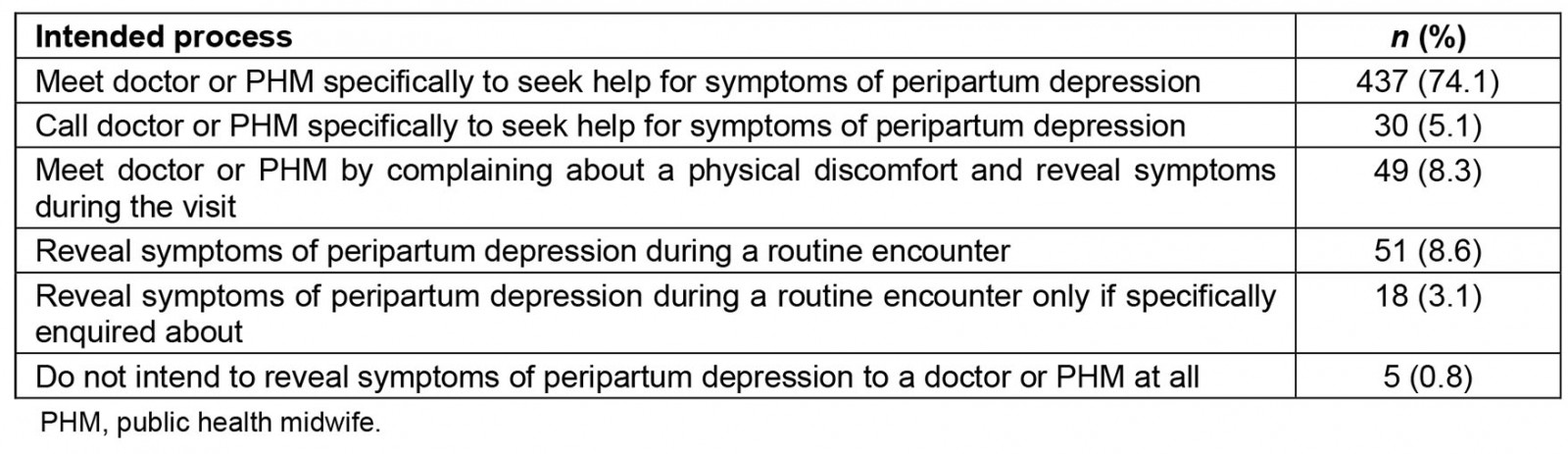
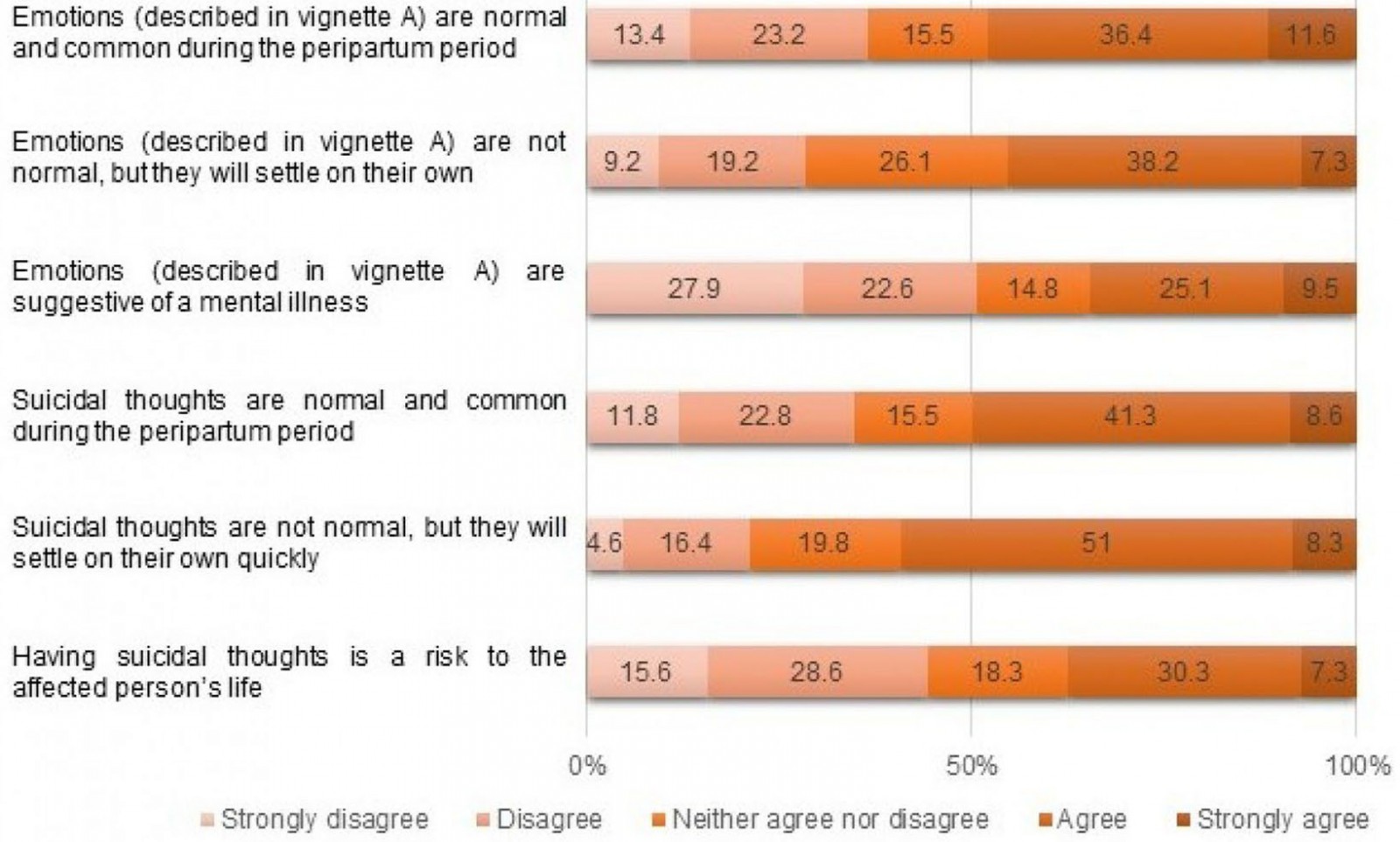 Figure 2: Perceptions regarding symptoms of peripartum depression and suicidal thoughts among pregnant women in Anuradhapura, Sri Lanka.
Figure 2: Perceptions regarding symptoms of peripartum depression and suicidal thoughts among pregnant women in Anuradhapura, Sri Lanka.
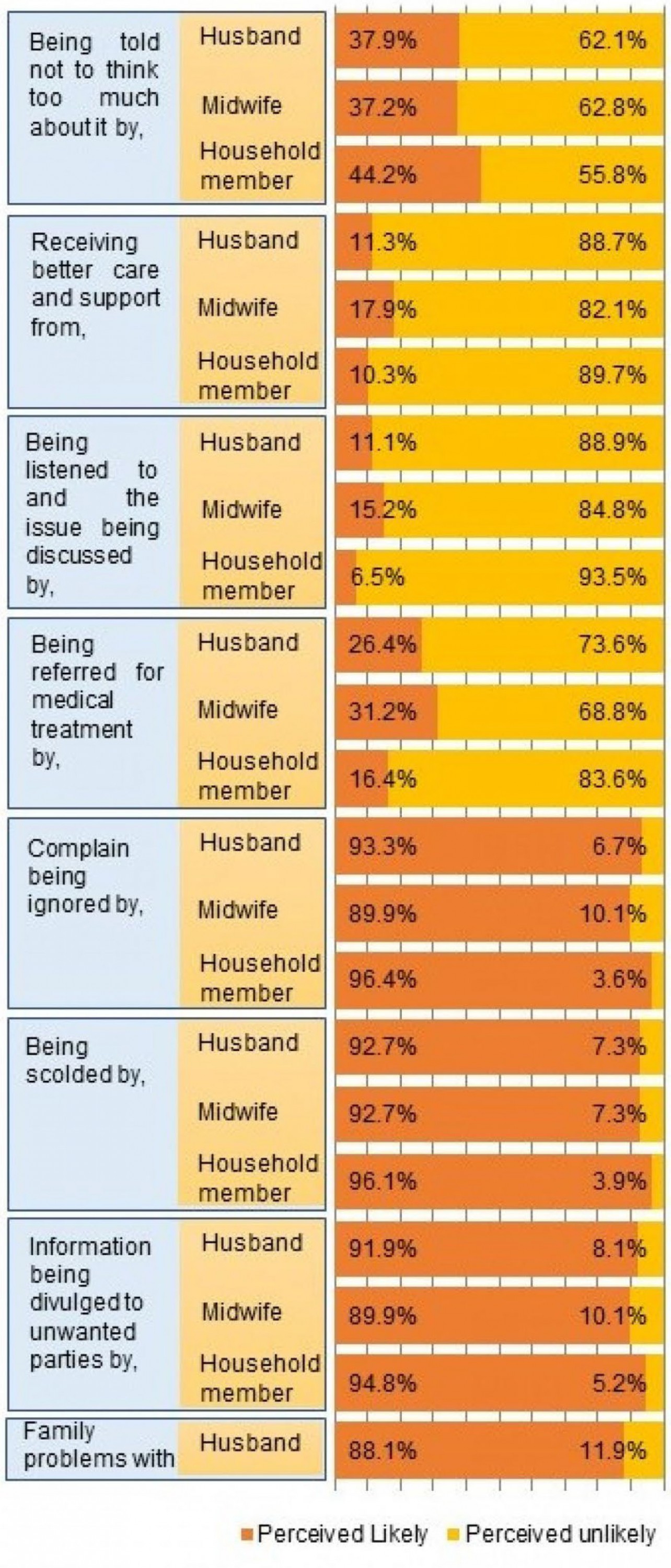 Figure 3: Perceived likelihood of selected responses to help-seeking for symptoms of peripartum depression from husband, another household member and public health midwife among pregnant women in Anuradhapura, Sri Lanka.
Figure 3: Perceived likelihood of selected responses to help-seeking for symptoms of peripartum depression from husband, another household member and public health midwife among pregnant women in Anuradhapura, Sri Lanka.
Discussion
Maternal suicides and depressive disorders are leading causes of maternal deaths29,64. Suicidal ideation, depression and being less likely to be receiving any active treatment at the time of death are strong predictors of suicide during the perinatal period10,28,29. Screening to identify these risk factors and making appropriate referrals would reduce the associated morbidity and mortality because appropriate care can be provided for those who need it49,54. However, maintaining universal availability, feasibility and timely accessibility of such interventions is challenging, especially in resource-constrained rural settings9,65. Prompting help-seeking by affected women and empowering their lay and formal reference networks to respond effectively would be helpful in such settings.
Help-seeking intention
This study shows that 64.1% of the pregnant women intended to seek help for symptoms of peripartum depression. Similar rates have been described in other studies41. Reported help-seeking behaviour for peripartum depression range from 65.5% (in Australia)66 to 10–12% (in India)67.
About half (n=181) of those with help-seeking intention would wait some time for symptoms to disappear on their own before help-seeking. Another 31.9% (n=191) had reported intending to try self-coping methods for symptoms of depression. Similar delay of help-seeking has been reported in other settings as well13,35-39,42,47,68. Interestingly, the intention to seek help immediately did not increase significantly, even when suicidal thoughts were added to the vignette. Delaying help-seeking prolonged the period the affected women are exposed to the health risks from depression during the antenatal and postnatal period.
Sources of help
Lay reference systems are crucial in help-seeking. Preference for family and friends over professionals when seeking help for depression during peripartum period has been reported in almost all relevant studies around the world35,41-43,46,48,49,55. The present study shows that this is even more the case in relation to seeking help for suicidal ideation. The majority of women mentioned that they would first seek help from their husbands for both symptoms of depression and suicidal thoughts. However, local evidence suggests husbands may not adequately understand these conditions and may not provide better care or take their wife for professional help69. Therefore, it is crucial to equip family members of pregnant women with the ability to recognise the danger associated with these symptoms. Families should be empowered to act empathically, increasing their care and support and to facilitate women to seek help from professionals.
A home visiting health worker has been reported as a useful source to seek help for depression during pregnancy and postpartum46,49,55,61. PHMs are the grassroots health workers who are the key source of health information, care and support to pregnant women, especially in rural Sri Lanka. This close relationship is reflected in a preference for the midwife over any other formal or semiformal sources and as a likely source for help-seeking. However, why some participants reported that they would never or rarely seek help from their midwife if they were to experience peripartum depression (5.8%) or suicidal thoughts (27.3%) needs to be investigated in further studies as this may act as the main barrier for effective care provision. Lack of training and understanding about mental health conditions and self-harm, and the lack of a proper guideline regarding these issues, are challenges for PHMs in providing responsive care for help-seeking women, which must be addressed urgently70-72.
MOHs are another potential source for professional help, easily accessible for perinatal mothers. Nevertheless, 12.8% of participants would never reveal their emotional problem to an MOH, which is a valuable opportunity lost. Improving the acceptability of MOHs as a source for help-seeking for peripartum depression may be valuable, especially in rural and resource-poor settings.
In contrast to observations from other settings36,44, only 16.6% and 15.6%, respectively, of women in this community reported definitely seeking help from a psychiatrist if they developed depression or suicidal thoughts during pregnancy or postpartum. This may be due to a poor understanding of mental health services and poor accessibility to such services in this community, which needs to be explored further. (At the time of the study, psychiatrists were available in only one hospital in the district.)
Using an obstetric setting for managing mental health issues in pregnant women is an interesting possibility, as susceptible women are regularly in contact with their obstetricians47,50,57. More than half (52%) of the participants reported a definite or probable likelihood of seeking help from obstetricians if they developed depression in the peripartum period. Therefore, paying attention to facilitating mental health-related help-seeking at obstetric settings may help to improve maternal health status in the country.
Previous studies have reported that Ayurvedic alternative medicine, traditional medicine practitioners and Kattadiya are sources of help for mental health issues in Sri Lankans73,74. Seeking help from complementary or alternative medical practitioners, Kattadiya and religious leaders has been reported in studies among Indian13, Saudi Arabian45, American42,48, Vietnamese American37, British-Caribbean39 and Nigerian women36 with peripartum depression as well. However, only a small percentage of participants in this study reported intention to seek help from such sources.
Internet and social media have been reported as sources of help for peripartum depression in other settings35,42,49,59,75. Despite the study setting being a mainly rural community, nearly a quarter of participants in this study also reported that they would at least probably use these sources for help-seeking. Exploring methods to utilise these modern options to quantitatively and qualitatively increase maternal health provision is worthwhile.
Intended process for help-seeking
While the majority of respondents reported that they might see a doctor or midwife specifically for help-seeking, 11.7% reported that they would reveal their problems only during a routine encounter with health providers, while a third said they would first need to be asked about emotional problems. Therefore, it is important to enquire about emotional wellbeing and facilitate women to speak of their emotional concerns during clinic and domiciliary visits.
Perceived threat
According to the health belief model, perceived severity and perceived susceptibility would determine the perceived threat, which is a main factor in predicting a health behaviour76. The perceived threat from symptoms of depression and even suicidal thoughts seems to be low in this community as many believed that these are normal emotions during pregnancy and the postpartum period, and that these would resolve on their own and were unlikely to be pathological. A total of 86.2% of participants had heard about antenatal or postpartum depression previously. Alarming rates of inability to recognise the seriousness of symptoms are likely to be a huge barrier for help-seeking in the event of experiencing a similar scenario. Therefore, urgent health education strategies are needed to empower pregnant women to recognise mental health 'red flags' in their lives.
Vignette-based studies have shown that the ability to identify symptoms of depression as a mental health problem is high among young Sri Lankans77,78. This is not reflected in this study, possibly due to the complex nature of the scenario where depression occurs on top of many significant changes to the lifestyle. The dilemma about abnormal emotions and normal emotions in the peripartum period has been a key challenge for women seeking help35,39,53-56. Inability to relate these symptoms with a possibility of a mental illness may be due to stereotyping presentations of mental illnesses as rather severe and psychotic. Difficulty in conceptualising symptoms has been associated with a lack of shared experience in several cultures39,60. Only 18.4% of participants knew someone having the condition, which may partly contribute to the inability to identify the vignette scenario as a mental illness. Relating real-life experiences and scenarios during health education and reducing barriers to sharing experience of survivors would help this community to identify symptoms early.
Perceived susceptibility to mental health conditions during the pregnancy or postpartum was also low among the study participants. This could be related to their beliefs and stereotypes about mental illnesses and motherhood. For example, women in some cultures thought that their mothers were ‘super women’ who returned to work the following day after giving birth. They felt that ‘strong women’ of their ethnocultural background could deal with the stresses and would not get depression like other women39,46. Whether the local communities hold similar or different perceptions on illnesses and motherhood needs to be studied further.
Attitudes towards help-seeking behaviour
Expectations about positive and negative sanctions can be used as proxy indicators for normative expectations. The majority of respondents perceived that positive consequences (such as receiving better instrumental and emotional support, and facilitation of further help-seeking) were likely and that negative consequences (such as being scolded, family problems, being ignored and breach of confidentiality) were unlikely if they sought help from their reference network (husband, other household member and PHM). Therefore, it may be assumed that pregnant women in this community have positive normative expectations about help-seeking for depression.
Perceptions about treatment
The stereotype that strong women did not need treatment to cope with symptoms of peripartum depression was held by 70% of respondents. A fifth believed this condition could not be cured. These beliefs could negatively affect help-seeking from semiprofessional and professional sources.
Conclusion
The study uses a vignette of peripartum depression. This approach was adopted to overcome the problem of lay people not being familiar with disease names, especially in relation to mental illnesses. The use of a vignette allows assessment of how participants construct meaning for common symptoms of a particular disease – whether they can identify a possibility of a disease when its symptoms are noticed. Efforts were undertaken to maintain the internal validity of the vignette. Anonymity techniques and a structured introduction during data collection were used to reduce the social desirability bias.
The study describes the help-seeking intention of pregnant women. The intention may not always correctly reflect the behaviour because many factors, including self-efficacy, structural and health system barriers, will also come into play16.
While suicidal ideation can occur independently of depressive symptoms, and peripartum depression includes antenatal depression, the vignettes focused on a mother experiencing depression during postpartum period and associated suicidal ideation to avoid confusing the participants with too much detail and length.
Intention and timeliness of help-seeking for peripartum depression and suicidal thoughts are suboptimal among pregnant women in this Sri Lankan community. The perceived threat from symptoms of peripartum depression and suicidal thoughts is also low. Ending preventable maternal deaths in this population requires more social innervations to improve the understanding of mental health during pregnancy and postpartum. Strategies to empower families and grassroots level healthcare workers to help mothers identify and seek treatment for mental illnesses also need prioritising.
References
You might also be interested in:
2021 - Designing and managing distributed learning: we’re all in this together


