Introduction
Non-communicable diseases (NCDs) are a significant public health burden globally. More than 15 million people aged 30–69 years die prematurely from NCDs annually, with over 85% of deaths occurring in low- and middle-income countries1. To mitigate this severe burden and prevent premature deaths, WHO launched the Package of Essential Noncommunicable Disease (PEN) Interventions for Primary Health Care in Low-Income Settings in 20102. PEN focuses on integrated management of NCDs in primary health centers in resource-constrained settings. It involves implementation of a set of relatively simple and cost-effective interventions, including health education, promotion of healthy behaviors, early diagnosis of NCDs, identification of risk factors, regular follow-up, and timely referrals to larger facilities when necessary2.
The PEN program has been implemented in a number of countries in recent years, including Myanmar3, Kyrgyzstan4, Moldova5,6, Tajikistan7, and Palestine8, providing evidence of impact as well as implementation issues, including gaps in basic service provision at the primary care level8. More evidence on outcomes as well as on implementation is needed.
In Bhutan, a small, mountainous country in South Asia situated between India and China, NCD-related morbidity and mortality have been rising. In 2014, the NCD Risk Factors Surveillance STEPS survey indicated that 39.2% of the population was overweight or obese, while 35.7% had high blood pressure and 6.4% had raised fasting blood glucose9. In 2016, the WHO estimated that 69% of deaths in Bhutan were due to NCDs, with the highest mortality attributed to cardiovascular diseases (CVDs)10. In response, Bhutan adopted the PEN program in 2010. Its pilot program encompassed a set of evidence-based, simple clinical protocols for clinical diagnosis and treatment of the most common NCDs11. The government also developed a Multisectoral National Action Plan for the Prevention and Control of Noncommunicable Diseases (2015–2020), which urged further interventions to address NCD risk factors identified by PEN12. An initial assessment of the program in 2014 indicated positive outcomes, including improvement in blood pressure and diabetes control13. However, a WHO audit in 2016 found implementation gaps, including in health worker adherence to treatment protocols, use of risk-based patient management, and knowledge to modify treatment of hypertension and diabetes. The audit also documented poor standardized screening and follow-up of NCD patients and inadequate follow-up for homebound and other palliative care patients14.
In early 2019, Bhutan’s Ministry of Health (MoH) introduced a new set of interventions building on PEN, called PEN HEARTS. The initiative encompassed six components: healthy lifestyle intervention, evidence-based protocols, access to medicines and technology, risk-based management, team-based care, and systems monitoring (Table 1). PEN HEARTS was introduced in March 2019 in two districts, Punakha and Tsirang, following training of selected health workers employed at the district and basic health unit (BHU) levels15. The program was expanded to two additional districts in September 2019 (Wanguephodrang and Zhemgang). Implementation stressed improving services through a people-centered, integrated approach to NCD management, especially CVD15.
The WHO and Bhutan’s MoH collaborated with Boston University to conduct an initial assessment of PEN HEARTS in 2019–2020. The purpose was to investigate implementation progress and explore evidence of impact on care, treatment, and outcomes to inform further program roll-out in Bhutan (see Table 1 for program elements). It addressed two main questions: was implementation of the PEN HEARTS delivered as planned? Were there measurable impacts of the PEN HEARTS program on provision of care for NCDs and patient outcomes? (Detailed subquestions are shown in Table 2.)
Table 1: Overview of PEN HEARTS components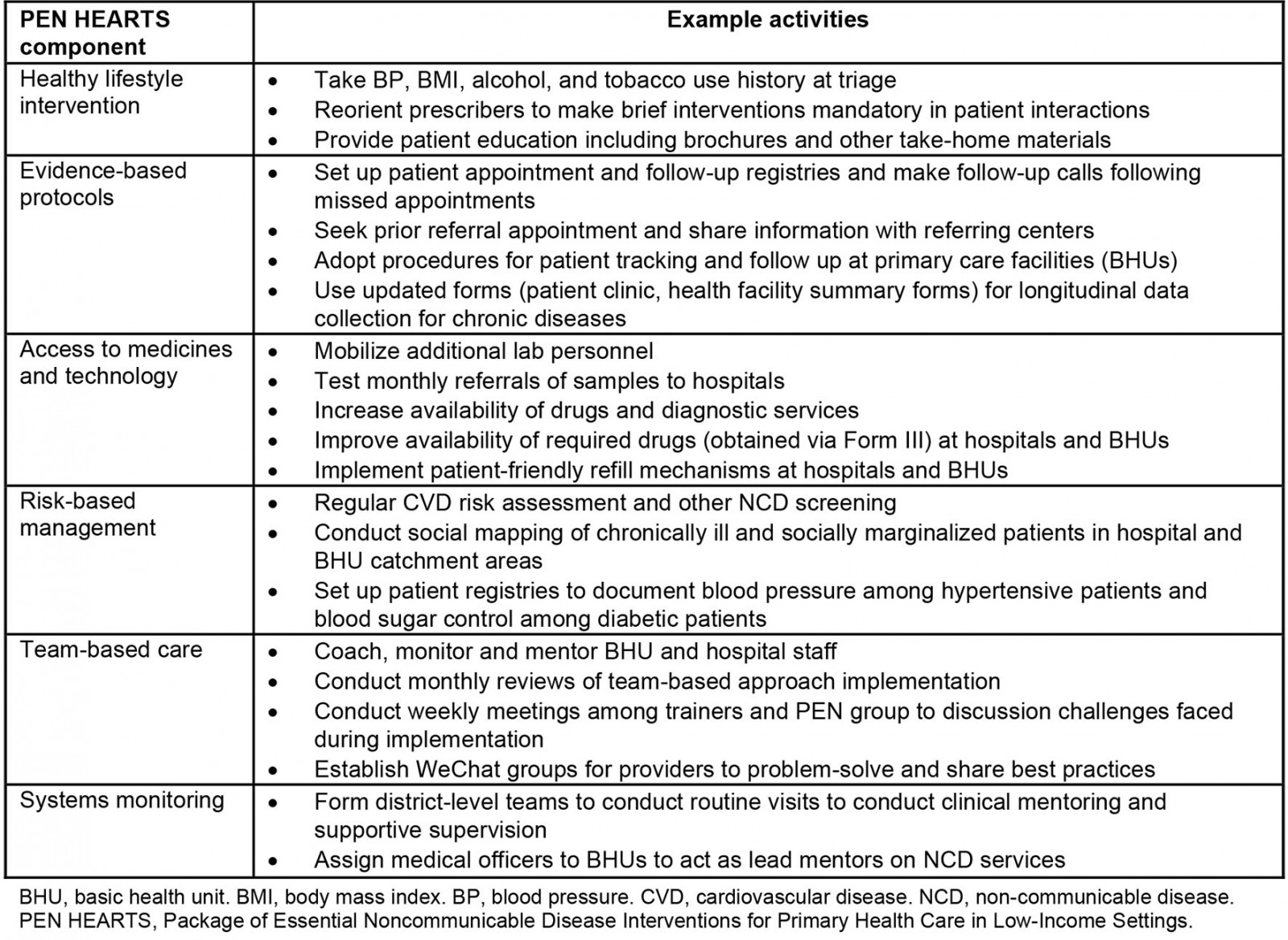
Table 2: Evaluation questions, indicators and data sources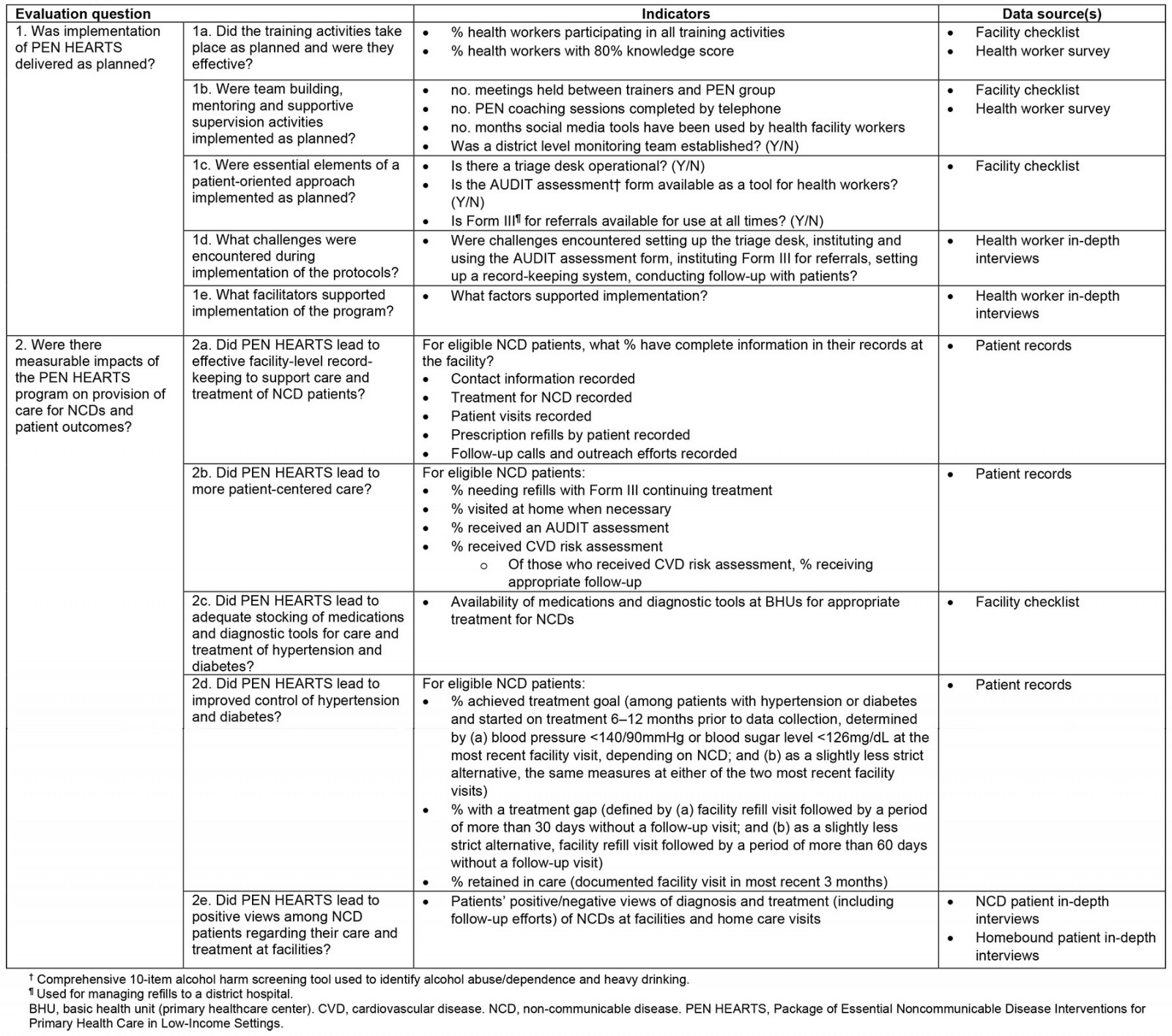
Methods
Study design
Given the complexity of the evaluation, time constraints, and the desire to incorporate views of a wide spectrum of stakeholders, a cross-sectional, convergent mixed-methods design was chosen that would utilize quantitative data for key assessments as well as qualitative data to inform and enrich those findings (Table 2). This involved the collection and analysis of quantitative and qualitative data in parallel, an approach employed frequently for program evaluation16. Quantitative data aimed to evaluate program implementation components including training, team building, mentoring and supervision, and patient-centered care; and program impact components including record-keeping, adherence to PEN guidelines, and medication supply. Qualitative data aimed to explore challenges and facilitators of implementing PEN HEARTS, and program impact via patients’ views of their care. The research team planned a second round of data collection 1–2 years subsequently to investigate longer term effects, but the COVID-19 pandemic paused those plans.
Study sites
Data were collected from three groups of districts (Fig1), two intervention groups, and one comparison group. Group A comprised Tsirang and Punakha districts, the ‘early starters’ that initiated PEN HEARTS in April 2019. Group B encompassed the late starter districts of Wangduephodrang and Zhemgang, which began implementation in September 2019. Group C included Trashi Yangtse and Lhuentse districts, where PEN HEARTS was not scheduled to be implemented until 2020.
Data were collected at each district hospital in study districts (six in total), as well as a random sample of three BHUs in each district. Hospitals were similar in infrastructure and human resource patterns, as were BHUs. The hospitals contained 20 beds staffed by doctors with basic diagnostics and treatment facilities, and two or three ambulances for patient transfer. BHUs employed community health assistants and other auxiliary health professionals, offering routine daytime and urgent services but no ambulances.
BHUs were selected using a stratified random selection process. Districts were stratified as urban, remote, and semi-urban with the goal of selecting one BHU per category in each district. If two BHUs of the same category were selected, another was selected until each category was included. Due to time constraints, qualitative data collection was limited to Punakha (group A), selected by flipping a coin.
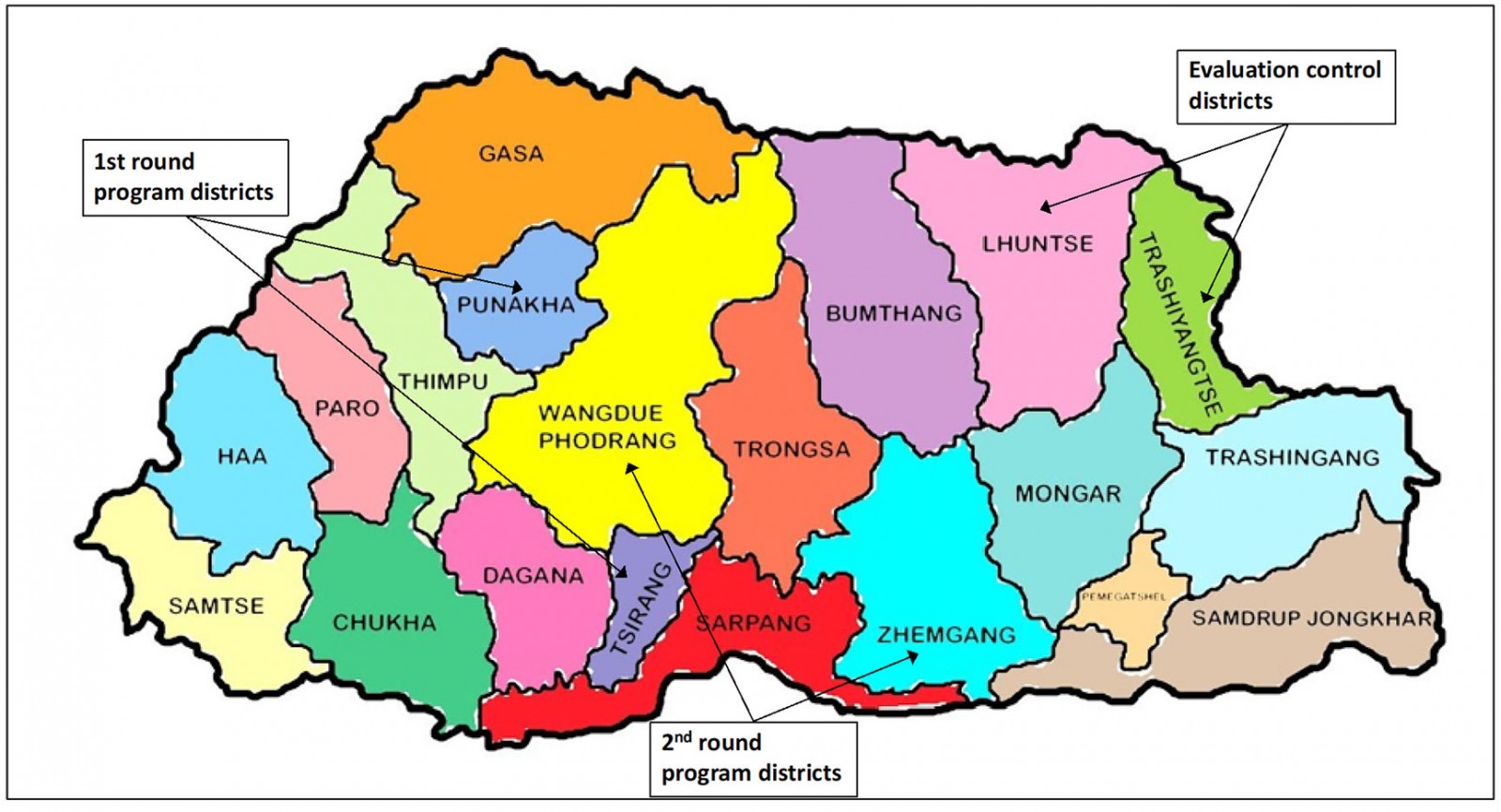 Figure 1: Evaluation sites
Figure 1: Evaluation sites
Data collection
A two-day training was held for enumerators, including detailed review of the protocol, informed consent, qualitative research methods, and study instruments. Study instruments were piloted in Punakha, followed by a full-team review of study tools. Enumerators were then grouped into four teams consisting of a supervisor (with master’s-level education or above) and two or three enumerators (bachelor’s level education). Enumerators collected data for 1–3 days per study facility, depending on size. Table 2 contains detailed information on data collection activities and indicators used to address specific evaluation questions.
Quantitative data collection: All quantitative data were collected on pre-printed, pre-numbered forms. The supervisors recorded data collection outputs in real time using logbooks for their respective study districts. The data were entered into Kobo Toolbox, a web-based data organization tool. Quantitative data collection included facility checklists, by which data were collected from health workers about program-specific supplies and/or available equipment; health worker surveys to assess knowledge of PEN HEARTS protocols, measured by 17 questions (a combination of true/false, multiple choice, and patient scenarios that asked about appropriate sequencing of care activities) based on training content, developed in consultation with local PEN HEARTS trainers; patient record abstraction – NCD patients, for data on record-keeping, patient care and treatment, and outcomes for patients who met specific diagnosis and treatment criteria; and patient record abstraction – homebound patients, for similar data as collected for NCD patients.
Qualitative data collection: In-depth interviews (IDIs) were conducted in Dzonghka or English according to participant preference. Activities included: (1) health worker IDIs – to describe program implementation; NCD patient IDIs – to understand patients’ views of the program and possible changes made because of PEN HEARTS; and homebound patient IDIs – to elicit homebound patients’ views of PEN HEARTS.
Sampling approach
Participants for surveys and record reviews: Participants were recruited by evaluation enumerators. For the health worker survey, sampling strategies differed for hospitals and BHUs. At hospitals, health workers were selected randomly by hand from a list of staff present on the day of data collection. When the number of health workers was less than the target sample size, all were selected. At BHUs, selection was done on a convenience basis due to the small numbers of health workers at these facilities (typically one to three people). Inclusion criteria included being aged 18 years or above and supporting NCD treatment at a study district hospital or BHU as a doctor, nurse, physicians’ assistant, pharmacist, or lab technician. Informed consent was obtained prior to administering the survey.
For patient record abstraction, enumerators created a sampling frame at each facility to include eligible patients, who were then selected randomly by hand. As with health workers, the number of eligible participants at some facilities was less than the number eligible, in which case all were selected. Eligibility was determined by being age 18 years and above, diagnosed with hypertension or diabetes, started on treatment between 1 May 2018, and 1 May 2019, and attending a study district hospital or BHU for follow-up care. Informed consent was not obtained for patient data abstraction because records were reviewed retrospectively, without collecting identifying information.
Participants for IDIs: Health workers were selected randomly at the Punakha hospital, using the survey sampling frame, and by convenience at BHUs (whoever was present when the study team visited). Inclusion criteria were the same as for the health worker survey. NCD patients were recruited on a convenience basis from facility waiting rooms on the day(s) of data collection. Inclusion criteria were the same as for the NCD patient record abstraction, including currently attending a study district hospital or BHU.
A convenience sample of homebound patients was recruited to participate in IDIs conducted in their homes. Inclusion criteria were being age 18 years and above, receiving care managed from a study district BHU or hospital, being unable to physically visit the hospital or BHU due to being terminally bedridden, elderly, or ill; and being visited at home in the previous 6 months by a health worker.
All IDI participants provided informed consent prior to beginning an interview.
Analytic approach
Sample sizes: For the health worker survey and patient record abstraction, sample sizes were determined based on feasibility/timeline and the ability to detect meaningful differences in key indicators between district groups. For the survey, a sample size of 29 per district (58 per group) was estimated to provide a minimum of 80% power at a two-sided alpha of p=0.05 to show specified differences in proportion with at least 80% knowledge (correct scores). For the patient record abstraction, a key indicator was proportion with complete (100%) patient information. A sample size of 30 per district (60 per group) was chosen because it could provide a minimum of 80% power at a two-sided alpha of p=0.05 to detect a difference of approximately 25% in this indicator. This number was also sufficient to detect a 25% difference in disease status (Table 2). The sample size for record abstraction of homebound patients was smaller due to fewer numbers of such patients at facilities. Twenty per group was estimated to allow detection of a 35–40% difference, depending on the proportion found in control districts.
The sample sizes for IDIs were determined by feasibility and timeline. Given prior experience of the study team and expert opinion suggesting that saturation may be achieved with 15–20 participants17, the aim was to recruit 14 health workers (eight/hospital; two per BHU), 20 NCD patients (five per hospital; five per BHU), and 10 homebound patients (up to 10 across all facilities). Although these numbers were relatively small, the evaluation team was confident the IDIs would provide rich, supplemental data.
Analyses: Quantitative analyses covered all indicators presented in Table 2. Continuous variables were summarized using their mean and standard deviation or median and interquartile range. Categorical variables were expressed as percentages. To assess health worker knowledge, correct answers were summed over the 17 survey questions and expressed as a crude score (number correct/17) for each provider, and mean scores per group were derived. The proportion with ‘high knowledge’ was defined as 80% correct. Disease control was define in two ways: the strict measure estimated the proportion of patients with hypertension who had BP<130/80mmHg at the last recorded visit or patients with diabetes who had a fasting blood glucose <126mg/dL at the most recent recorded visit. The alternative measure of disease control considered blood pressure or blood glucose at either of the last two recorded visits.
Bivariate analysis was performed using χ2 tests of association or Fisher’s exact test for categorical independent variables and t-tests or Wilcoxon tests of association for continuous variables as appropriate. Pairwise comparisons were conducted among groups.
Qualitative data were audio-recorded, transcribed, and translated into English by the Bhutan study team. Transcripts were sent to Boston via a secure transfer system for analysis. Transcripts were entered into NVivo v12 (QSR International; https://www.qsrinternational.com/nvivo-qualitative-data-analysis-software/support-services/nvivo-downloads) and analyzed using thematic content analysis with inductive coding. Two members of the Boston team read the transcripts, discussed, and organized the themes and subthemes. One researcher coded all transcripts. Direct statements of participants were selected to illustrate themes.
Following analysis, quantitative and qualitative data were integrated using a weaving approach across the main thematic elements of the evaluation16. This approach is consistent with a convergent mixed-methods design, which in the present study allowed data from IDIs to enrich and elucidate key quantitative findings, while incorporating the views of key stakeholders in their own words.
Ethics approval
This study was approved by the Research Ethics Board for Health (REBH) (REBH/Approval/2019/075) in Thimphu, Bhutan and the Institutional Review Board of the Boston University Medical Campus in Boston, MA (Protocol #H-39376).
Results
Data were collected on 14–28 November 2019 from six district hospitals and 18 BHUs. A total of 153 health workers participated in the knowledge survey; all selected agreed to participate (no refusals). Health workers had similar background characteristics across districts, although a higher proportion of those in group A were below the age of 30 years; more than half (52.3%) were male, while nearly 30% were health assistants and 30–40% were doctors or nurses. The median years of experience as a health worker was 3.5–5.8 (Table 3). IDIs were conducted with 13 health workers, 18 hospital or BHU patients, and four homebound patients (Table 3). A total of 121 NCD patient records were reviewed.
Background information on NCD patients was limited to what was in the records, but was sufficient to indicate few major differences in the patient populations across districts. Overall, 53.7% were hypertensive, 44.6% were diabetic, and 1.7% had both conditions (Table 4). Over half (57.9%) received care at BHUs. A slightly higher proportion in group C were hypertensive compared to groups A and B. Just over half overall (51.2%) were male, although there were more females (62.5%) in group A districts and more males (68.6%) in group B districts. The mean age was 50–60 years across all districts.
Table 3: Background characteristics of participants: health worker surveys and in-depth interviews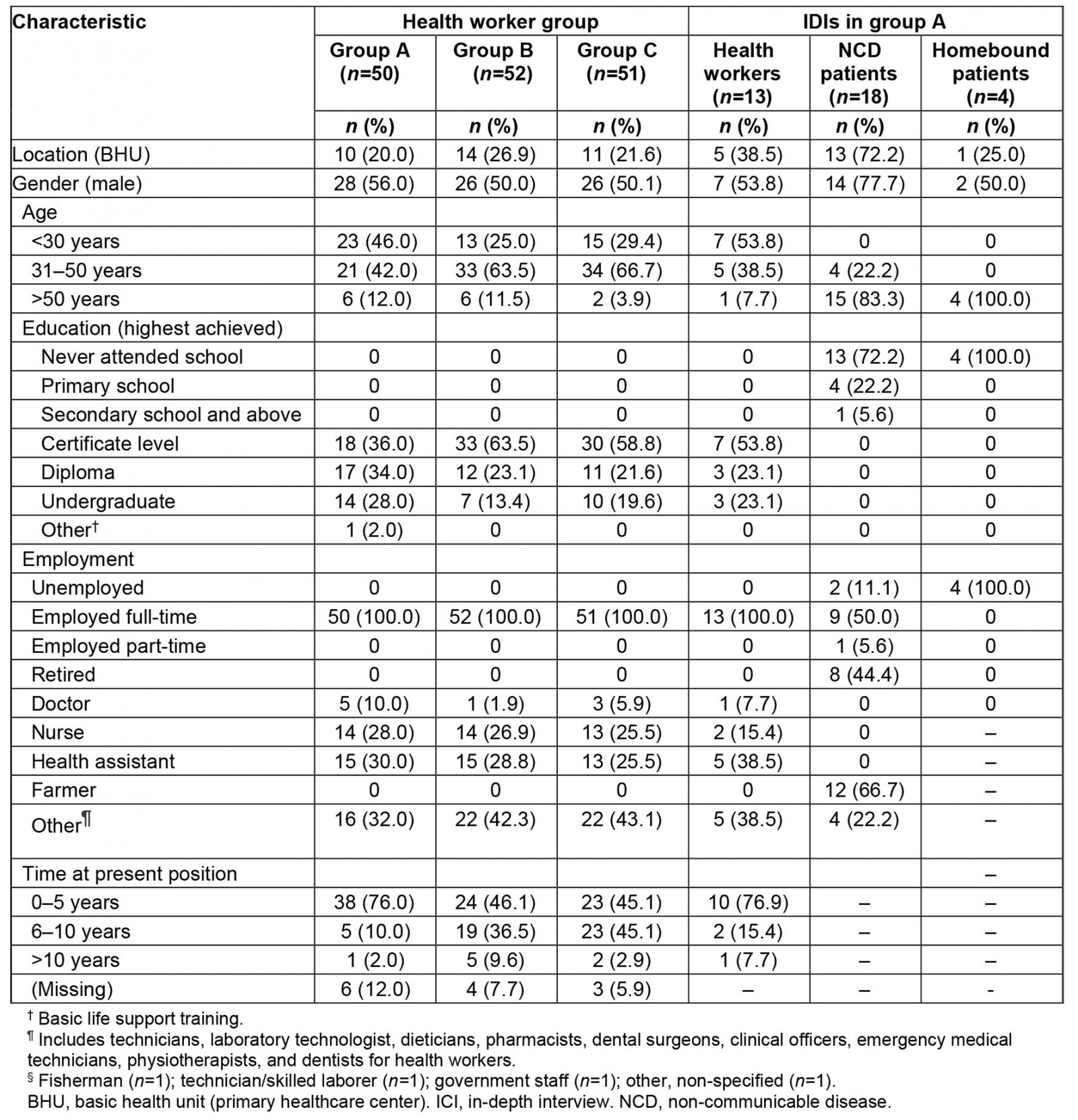
Table 4: Background characteristics of NCD patients selected for record review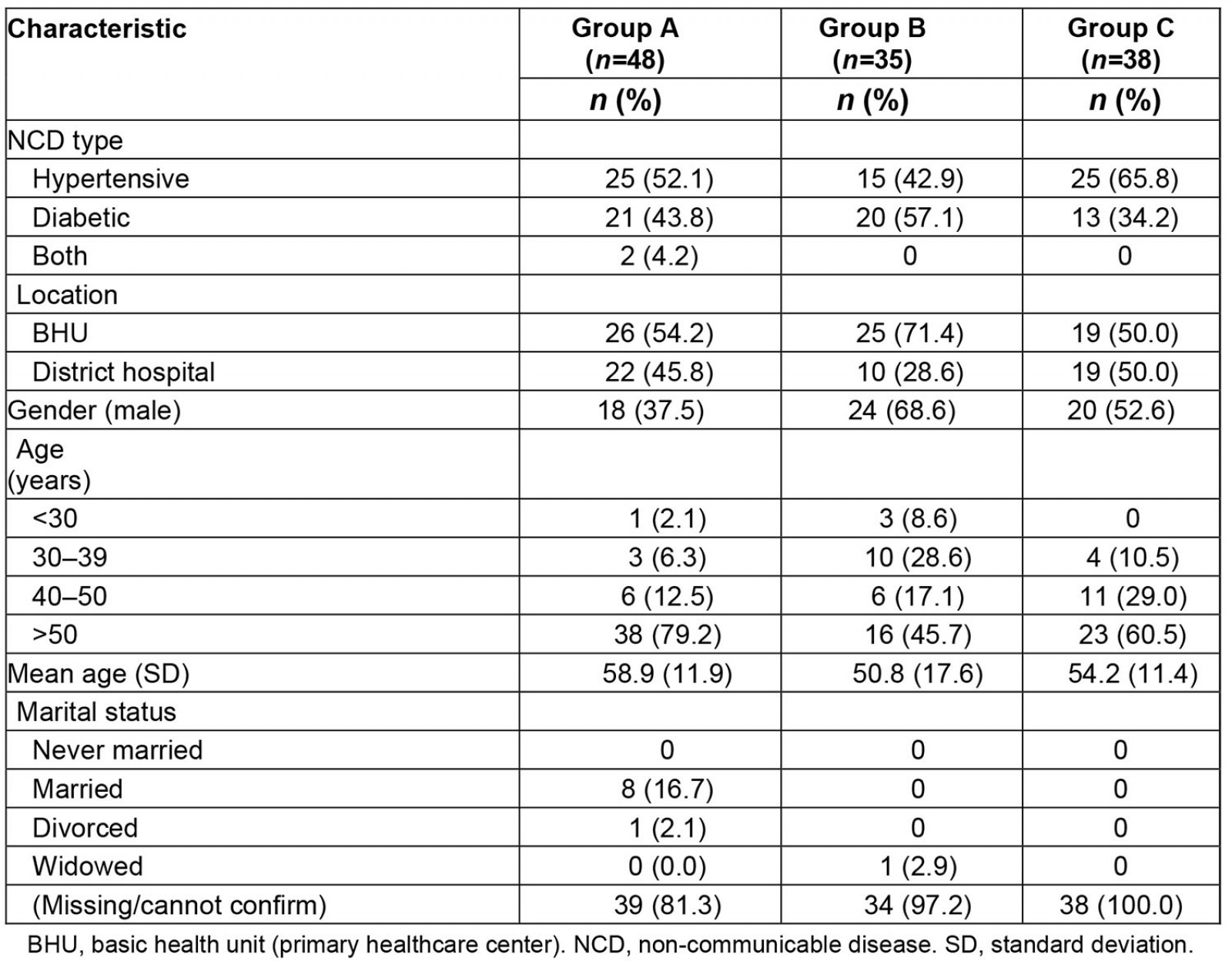
Implementation outcomes
All quantitative implementation indicators are reported in Table 5. Key findings are summarized below and integrated with qualitative findings.
Training status and social media use: Most (95%) health workers in group A districts were trained in PEN HEARTS protocols. By comparison only 9% of health workers were trained in group B districts. Health worker staff in group A used social media for team-based care much more than group B (5.3 mean months of use in group A v 0.4 in group B).
Table 5: Implementation Indicators for intervention districts (groups A and B)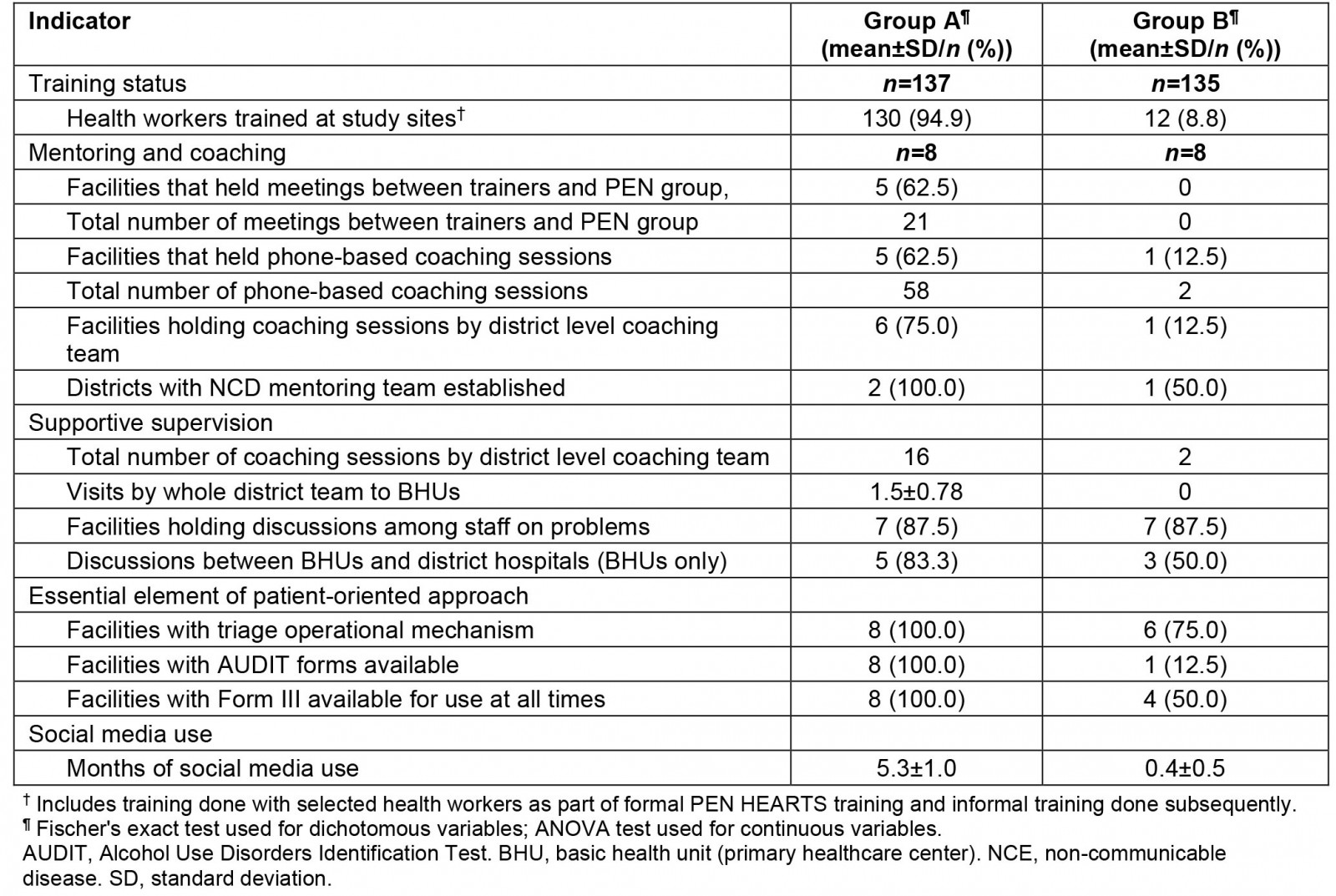
Mentoring, coaching, and supportive supervision: Among the three groups, group A recorded higher team building, mentoring, and supportive supervision activities. Both districts in group A had established a district-level mentoring team. Five out of eight facilities within group A had meetings between trainers and the PEN HEARTS group, as opposed to none in group B. These same five health facilities also hosted 58 phone-based coaching sessions. By comparison, group B recorded only two phone-based coaching sessions. None of these activities occurred in group C districts.
Essential elements of patient-oriented approach: All eight group A facilities were reported as having the essential elements of a patient-oriented approach: use of a triage system and having AUDIT and Form III forms (used for patient referrals and to obtain medications for patients) available. By contrast, among group B facilities, six of eight had an operating triage system, one of eight had AUDIT forms available, and four of eight had Form III available.
Challenges encountered during implementation: The qualitative data indicated that health workers experienced implementation challenges in four main areas: human resources, medicine shortages, equipment failure, and record-keeping.
Human resources Health workers described being often short-staffed, with duties and priorities that prohibited them from spending adequate time with NCD patients. As one explained:
The biggest challenge is staff shortages and the multiple responsibilities we shoulder ... we don’t get enough time to fill up forms and concentrate fully on PEN HEARTS. If additional staff is provided, the services can be improved further.
Medication shortages Most health workers noted that the process of requesting pharmacy refills was lengthy, often resulting in patients not receiving medications at the time of their visit:
If there are new cases, we need to fill up the form again and send it to the hospital, which takes time. We end up using drugs from our old clients for the new ones and this has caused drug shortages.
Equipment failure Health workers highlighted that frequent failure of equipment to check blood pressure and blood sugar was discouraging, and prevented them from delivering the program as planned. For example:
It’s very challenging … we fell short of glucose strips and sought support of 100 strips from a BHU and recently the dysfunctional weighing scale could not be repaired, so we requested a BHU to mobilize a weighing scale.
Record-keeping Health workers revealed mixed views on the acceptability and utility of the new record-keeping system. While some described an improved ability to track and manage patient disease and refills, others felt the process was burdensome:
The challenge we face is that when more programs are initiated, most of our time is consumed in record management and treatment.
Facilitators to implementation: Health workers described support, supervision, and mentoring from senior leadership as integral to implementing PEN HEARTS. Support consisted primarily of frequent communication and timely feedback via social media (eg WeChat) and in-person visits. This support was viewed as contributing to patient care and improving personal work satisfaction. For example:
These days, we have time to time monitoring and supervision visits from district hospital. They come, check our documentation, and write remarks in the visitor’s register. They also praise us and give us compliments for the changes we made. We are happy they notice and appreciate our work.
Impact outcomes
Differences in healthcare worker knowledge of hypertension and diabetes management and facility management practices are reported in Table 6. Table 7 highlights the differences in clinical outcomes by district. Key findings are summarized below, integrated with qualitative findings.
Table 6: Health worker knowledge and facility practices by district group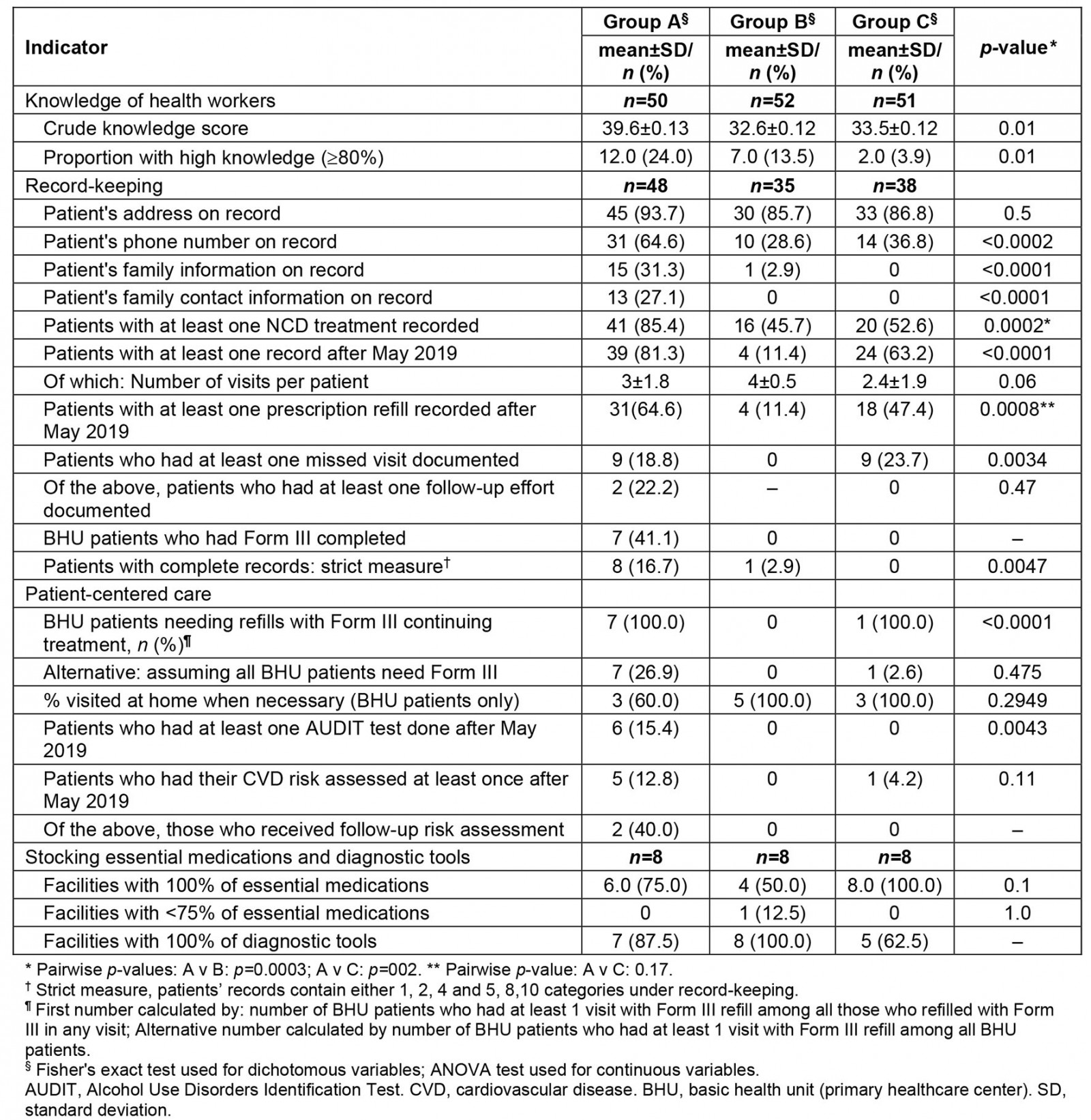
Table 7: Clinical outcomes by district group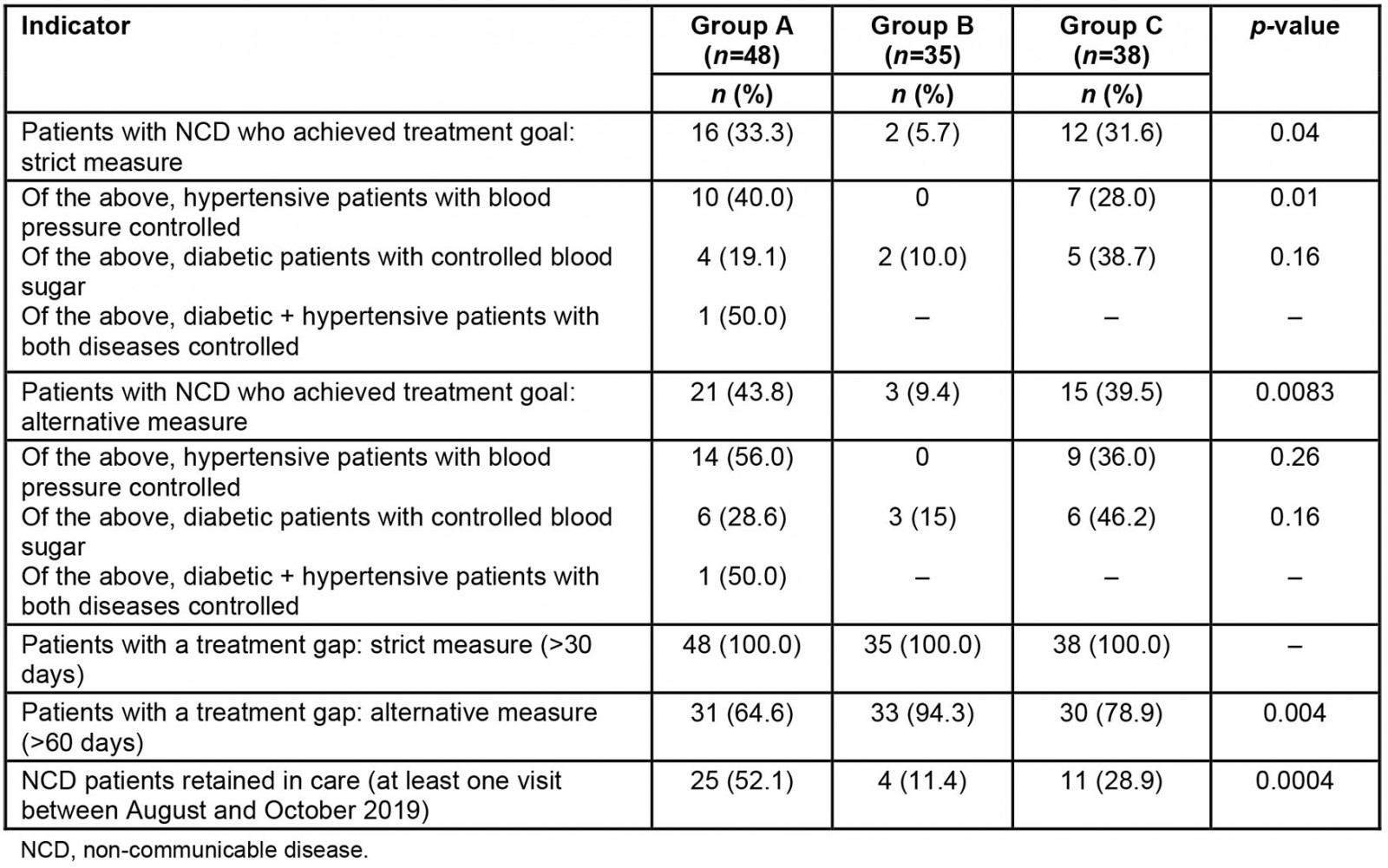
Knowledge of health workers: Group A health workers demonstrated significantly higher mean knowledge scores than groups B and C (p=0.01). At the same time, there were notable gaps in knowledge across all groups, particularly around sequencing of activities when an NCD patient failed to attend a refill visit, referral procedures, and the components of patient-centered care.
Improvement in record-keeping, refill, follow up and referrals: There were higher levels of complete patient record documentation in group A (16.7%) compared to group B (2.9%) and group C (0%) (p<0.001). Among the BHU patients, 65% in group A had at least one prescription refill and 41% had a refill using Form III recorded. The two other groups had significantly fewer prescription refills (p<0.001). Where records in group A indicated a follow-up appointment was necessary, only 22% documented that a referral was made. Overall, the study showed improvements in collecting contact information; major gaps persisted related to records on missed visits and follow-up calls.
Patient-centered care: Potential gaps were present in patient-centered care, although conclusions are limited by low levels of record-keeping. The number of patients needing refills with Form III was high (100%) in groups A and C, compared to 0% in group B (p<0.001). Records also suggested that use of AUDIT tests and CVD risk assessments was low: 15.4% of patients in group A received an AUDIT test (0 in the other districts), and 12.8% of patients in group A received a CVD risk assessment (0 in group B, 4.2% in group C).
The IDIs suggested that care may have become more patient-centered in ways difficult to measure given the state of patients’ records. Both health workers and patients described avenues by which PEN HEARTS facilitated improvements to patient-centered care. Health workers conveyed a better ability to track and manage patient disease and refills, and to provide outreach to improve services in a timely manner:
The changes have [been] obvious [in their] impact on the quality of care we provide for our patients ... if we have records it helps us to follow up on their subsequent visit, and we get to know more on their treatment, medication and efficacy of prescribed medicine.
Patients described how health workers were attentive to their needs, provided clear information about medications and their illness, and facilitated methods for obtaining medications (eg home delivery or reminder calls to pick up refills). For example, one homebound patient explained:
I can experience and see some changes … lately we have some health workers come to our doorstep to provide services and even provide medication if necessary. The home care visits are very advantageous, and I feel that this service will benefit us.
Improvement in stocking of medications and diagnostic tools: Nearly all facilities had >75% of essential medicines and diagnostic tools, although gaps were evident at some facilities. Of note, all eight group C district facilities had essential medications, as opposed to 75% of group A and 50% of group B facilities. Regarding diagnostic tools, 100% of group B facilities were fully stocked, as compared to seven of eight group A facilities, and five of eight group C facilities.
In the interviews, patients expressed mixed responses when asked about consistent access to medications. Some stated that all medications were consistently available while others noted frequent stock outs (items not available in the facility). Patients elaborated that while stock outs occurred more frequently at BHUs, they were generally still able to access their medications at the hospital. According to one NCD patient:
… I have seen a change in way that I get all my medicines from here and I don’t have to travel to hospital. I am very happy that this service is available, and I can save Nu [money].
Improvement in clinical outcomes: There were encouraging results regarding clinical outcomes, even with gaps in record-keeping. The proportion of patients who achieved their treatment goal was significantly higher in group A than group B (33.3% vs. 5.7%) but similar to group C (31.6%). Due to incomplete record-keeping, treatment gaps were assessed using a definition of gap >60 days. This measure indicated a significantly lower proportion of patients with a treatment gap: 64.6% in group A districts compared to 94.3% and 78.9% in groups B and C, respectively (p<0.001). The proportion of patients retained in care, as defined by at least one facility visit in the most recent 3 months, was also significantly higher in group A districts (p<0.001).
Qualitative data from patients support these findings. When asked about positive changes from the PEN HEARTS program, patients perceived that control of their disease had improved. They described better medication adherence, diet management, and overall improved health and wellbeing because of the changes over the previous 6 months at both hospitals and BHUs. As one NCD patient said:
In the past six months, they have made the new initiative of telling me and other patients like me about what is good and bad for my body and blood sugar. They also tell me to eat [the right] kinds of vegetables and fruits too.
A homebound patient added:
For last few months, I have received my medicines without a single break from the hospital and I have not missed a single day in the last few months. The reason is it’s getting delivered.
Patients’ perceptions of PEN HEARTS: Data from interviews with NCD and homebound patients indicated a strong positive response to PEN HEARTS. Both groups described positive experiences regarding their care and treatment. They depicted health workers as kind, compassionate, and knowledgeable about their disease and medication. As one NCD patient explained:
I am comfortable visiting the BHU for services. The health workers provide good treatment with the right attitude. They focus more on adherence to treatment, alcohol and tobacco cessation, control salt and fat intake, and daily exercise.
Patients also described how health workers called them to remind them to refill their medication and/or to check on the status of their condition. They expressed appreciation for health workers who made home visits, and for those who spent time teaching them about disease management. For example, one homebound patient said:
For the last six months or so, health staff have been coming to check my blood and [to] bring the medicines. They have advised me on my blood sugar control and accordingly adjust the medicines.
Some patients also indicated opportunities for improvement. They described the shortage of staff at BHUs and felt services would improve if more health workers, doctors, and services were available. When asked about hospitals, patients highlighted the long queues for services which often forced them to spend the entire day away from home. As two NCD patients said:
… if the government could deploy [a few more] health workers and essential equipment, that would be great, and would have a greater impact on quality of health care.
With large numbers of patients availing the same services, the waiting time exceeds more than an hour or two. This really bothers me.
Discussion
This evaluation provides important evidence regarding early implementation of PEN HEARTS and its impact on NCD management in Bhutan. Most elements of the PEN HEARTS program were implemented as planned, including monitoring and supervision. Use of social media for communication appeared to be particularly popular. The evaluation allowed identification of several critical areas for improvement: training, record-keeping, and use of AUDIT and CVD assessments. It also revealed signs that the program was impacting disease control positively. Several other findings highlight gaps that may affect sustained effectiveness, offering lessons for further scale-up of PEN HEARTS in Bhutan as well as program implementation in other resource-constrained settings.
Training
While healthcare providers were trained in the PEN HEARTS protocol, many appeared unfamiliar with key details. Notable knowledge gaps were identified, particularly around sequencing of activities when NCD patients fail to attend refill visits, referral procedures, and components of patient-centered care. This was particularly evident in group B facilities, where process indicators were notably worse than in group A. These gaps could be due to challenging survey questions, or may reflect incomplete training at the time of data collection, since training took place in waves – starting with formal training of selected individuals and continuing informally in facilities over time. They might also indicate less intensive training practices over time, less follow-through on training by management, less supportive supervision, or a combination of all three.
The take-away lesson, for Bhutan and other countries, is that strengthening knowledge of health workers requires multiple activities over time. Refresher trainings and alternative forms of both formal and informal training could be employed, including use of mobile technologies18-23. Reinforcement of team-based peer coaching, mentoring, and supportive supervision between and within teams in future training and implementation would also be beneficial.
Record-keeping
The evaluation revealed limited changes in record-keeping practices. It found inadequate record-keeping in patient visits, follow-up calls, and medication refills, and limited use of Form III for referrals to critical services. Overall, less than 20% of sampled records were complete, excluding Form III. This is worthy of stakeholder attention because good records foster better care, monitoring, and evaluation. Importantly, data for evaluation can only be as reliable and thorough as records themselves. Incomplete record-keeping limited the ability to measure a range of indicators such as follow-up procedures after missed visits and disease control. The lesson here is that improving the quality of record-keeping should be a key priority, both for disease control and program evaluation24.
The evaluation did not provide reasons for poor record-keeping but anecdotal evidence and discussions among the study team suggested that inadequate staffing given the patient load may limit the time health workers have to maintain records, both at BHUs (where two or three health workers typically handle all activities) and at hospitals (where medical staff are more numerous, but none are dedicated to NCD care). This suggests that structural changes to increase medical staff may be critical.
Additional tools for health workers, such as standard patient record templates (including those recommended by the PEN HEARTS technical package) may be useful in this regard. Piloting a new system using referral slips with multiple (self-carboning) copies could also be employed to address issues monitoring patient retention in care. One copy would remain in the referring facility medical record, and a second copy would be carried by the patient and given to the receiving facility. A third copy with the referral result and instructions could be taken back to the first facility by the patient, thereby ensuring communication across all facilities providing care to the patient. This system is both comprehensive and yet sufficiently simple to be appropriate in a range of settings.
Use of AUDIT and CVD assessments
Use of AUDIT and CVD assessments are priorities for PEN HEARTS that need more promotion. It is unclear why poor use of behavior-related assessment tools was so prevalent, but over-burdened medical staff may again play a role. Aside from re-balancing the staff-to-patient ratio, potential strategies to address this gap include a systematic monitoring system to ensure regular checks on degree of compliance with key features of the program, as well as continued and strengthened emphasis on risk-based assessments and holistic care including brief interventions to reduce the effects of tobacco and alcohol.
Essential medications and diagnostic tools
Maintaining access to essential medications and tests is critical for long-term care of NCD patients. One surprising finding was that the group C districts had better supplies of medications than group A districts (100% v 75%). There is no obvious explanation for this difference, but it may reflect disparities up the supply chain in Bhutan’s districts or, conversely, varying demand from communities. It may also result from a combination of medication distribution (perhaps based on size or type of facility) and actual prescribing practices or drug usage. Further investigation of this unexpected finding and incorporation of additional follow-up could be explored in subsequent evaluations.
Impact of PEN HEARTS on disease control
The evaluation provided early evidence that PEN HEARTS was impacting disease control positively. Disease control was close to 50% in group A districts (using a measure pertaining to the most recent two patient visits) and significantly higher than the other districts. Study findings on retention were similarly positive, with over 50% of patients in group A districts retained in care compared to much lower proportions in other districts. The data on treatment gaps in group A were less positive overall but, regardless of measure, such gaps were significantly fewer than what was observed in other districts. These findings provide the strongest evidence that PEN HEARTS, even over a 6-month timeframe, was making a difference in NCD control. To understand longer term and spatial effects of the program, another round of data collection focused on implementation and impact of PEN HEARTS is recommended. It is worth noting that strengthening record-keeping prior to further evaluation would add to confidence in the data, underscoring the importance of this element of PEN HEARTS.
Limitations
There are several limitations to this study. First, sample sizes were small; however, findings revealed statistically significant differences across a range of key indicators. Additionally, the study design was limited to data available in patients’ records. As discussed above, this remains an area in urgent need of improvement. A population-based sampling approach would have been more rigorous, and mitigated selection bias, but time and budget constraints prevented such a design. Finally, the IDI data, as with any qualitative data, may be biased due to the desire of participants to please enumerators. The ability to triangulate data across different groups (patients and health workers) may have helped mitigate such bias.
Conclusion
This evaluation provided preliminary data to guide further implementation of PEN HEARTS in Bhutan, with lessons for other countries as well. It revealed gaps in health workers’ knowledge that highlight a need for improved and sustained training activities. It also illuminated inadequate record-keeping and use of behavior assessment tools, suggesting a need for structural reforms to reduce patient burden for medical staff.
The evaluation also found some evidence of improved disease control in intervention districts, suggesting that PEN HEARTS has the potential to impact NCD burden in resource-constrained settings. Given the limitations of timing and scope, sweeping conclusions are not possible; rather, they point to the importance of further evaluation to better assess the potential for a simple set of initiatives such as PEN HEARTS to make a difference for NCD patients in Bhutan and similar settings.
Acknowledgements
The authors thank the non-communicable disease control program, the Department of Public Health, Ministry of Health, Bhutan, for facilitation and support. This evaluation was conducted collaboratively by KGUMSB and Boston University with financial support provided by World Health Organization – South-East Asia Regional Office.
References
You might also be interested in:
2021 - AzoresDiab model: the risk prediction of type 2 diabetes in the Azores
2013 - Prevalence of eye diseases among school children in a rural south-eastern Nigerian community
2013 - Transforming rural health systems through clinical academic leadership: lessons from South Africa