Introduction
Every year, an estimated 15 million infants are born preterm worldwide and it is the leading cause of approximately 1 million deaths in children under the age of 5 years1. Preterm birth is when an infant is born before 37 completed weeks of gestation. Infants born at 28–32 weeks gestation are considered very preterm, and less than 28 weeks gestation extremely preterm1,2. The prevalence of preterm birth in Australia rose from 6.8% in 1994 to 8.7% in 20203,4.
Women residing in rural and remote areas (RRA) of Australia experience increased rates of adverse perinatal outcomes and are at almost twice the risk of having a preterm infant than women residing in major cities5,6. RRA health services are not equipped to provide the specialised level of care required for preterm infants, thus mortality and morbidity rates are higher for preterm infants born in non-tertiary centres7,8. In addition, the closure of many RRA hospitals in Australia over time has led to metropolitan tertiary and some regional centres now providing the bulk of maternity services9. This means that women in RRAs who have preterm births can only access specialist neonatal services by travelling great distances, often by emergency aircraft or ambulance, to metropolitan tertiary centres10. For Australian residents, there are no costs incurred by families for the care and treatment of their infant while admitted to a neonatal intensive care unit (NICU). This burden lies with the Australian Government’s Medicare system. Most NICUs in Australia offer subsidised accommodation to women from RRAs, which is financially supported by state or territory governments and usually obtained through assistance by the social worker. Not all accommodation is within hospital grounds, and cooking or laundry facilities can be limited.
People in RRAs generally face a range of stressors unique to living outside major cities when it comes to accessing healthcare services6,11. However, the additional impact of having a preterm infant in an NICU on women from RRAs is not well known. A previous study undertaken almost 30 years ago involved interviews with parents from RRAs, targeting specific questions about access to and involvement in their infant’s care, as well as verbal or written communication from the neonatal team12. However, the psychosocial impact on the woman and her family was not examined. A more recent literature review on the topic of parenting the preterm infant in the NICU found only one study on the experience of RRA parents and highlighted the lack of knowledge in the RRA population group including Aboriginal and Torres Strait Islander Peoples. A recent study examining the experiences of parenting a premature infant found a lack of knowledge in this area and highlighted the importance of further research to understand the experiences of women from RRAs13. This study aimed to understand the experiences of women from RRAs of Australia who have had a preterm infant in an NICU.
Methods
Study design
A qualitative descriptive approach was used, drawing on the lived experiences and perspectives of women through their stories, giving a deep, rich understanding of the experience of having an infant admitted to the metropolitan NICU setting while residing in a rural area.
Participants and settings
Using non-random convenience sampling through two Australian preterm infant organisations, women were invited to take part in the study by an online advertisement, which directed them to complete a brief eligibility questionnaire. The inclusion criteria were women residing in a rural or remote area, aged more than 18 years and had birthed an infant at 32 weeks gestation or less who had received care in an NICU within the previous 6 months. Five women who met the inclusion criteria consented to participate in this study.
Data collection
Demographic information was collected in the screening questionnaire. Prior to the interviews, participants were provided with a consent form and participant information sheet outlining the aims of the research and expectations of participating to gain informed consent. A list of 17 semi-structured, open-ended questions based on the literature and study objectives was developed by the researchers. The questions were pilot tested with one mother who had a preterm baby in NICU, to identify potential biases, and some minor refinements were made. Each interview lasted up to 90 minutes, and all interviews were conducted using Zoom video-conferencing software. Interviews were audio-visually recorded and transcribed verbatim.
Data analysis
Thematic analysis using Braun and Clarke’s six-step framework was undertaken14. Following transcription, the primary researcher reviewed the recordings to ensure accuracy of the transcripts. This was followed by a familiarisation process of reading the transcripts several times over. Initial ideas were also noted. The second phase involved generating initial open codes or patterns in the data. The coding used was formed from two approaches: semantic, where coding and theme development reflected the explicit content of the data; and inductive, whereby coding and theme development were directed by the data content14. Codes were also written in a notebook for later stage analysis. The third step involved identifying potential themes from the data. This involved examining the codes for broader patterns. The other researchers reviewed at least one interview each to identify themes. The fourth phase involved the primary researcher reviewing the themes and checking the candidate themes against the data set, to ensure they were able to answer the research question. The fifth step was to define and name the themes. Again, this required consultation with all researchers to assist in deciding on an informative name for each theme. The final step in the framework was to produce the final report.
Ethics approval
This study was given approval by the Southern Adelaide Local Health Network Human Research Ethics Committee (SSA/19/SAC/13.9 HREC/19/SAC/14). All data has been de-identified and pseudonyms have been used throughout.
Results
Participants were five women aged between 29 and 36 years (mean age 30.2 years), and the average age for Australian women giving birth that same year was 30.7 years4. All were working three or more days a week prior to giving birth to their preterm infant. All women described themselves as Anglo-Australian, from a tertiary-educated and middle socioeconomic background, living in rural areas of Australia in the states of Victoria, New South Wales, Western Australia and Queensland. The women’s infants were born between 24 weeks and 3 days gestation and 31 weeks gestation. One woman birthed her infant in a regional health centre and was transferred to the metropolitan NICU shortly afterwards. The remaining women birthed in a metropolitan tertiary centre after being transferred from a regional hospital antenatally. The type of birth, parity, marital status and distance of residence to their respective NICUs is shown in Table 1.
Four major themes were identified from the thematic analysis: emotional trauma, social displacement, external coping resources and craving continuity of care. External coping resources consisted of a further three subthemes: desiring emotional support, requiring practical support and needing peer support.
Table 1: Study participant demographics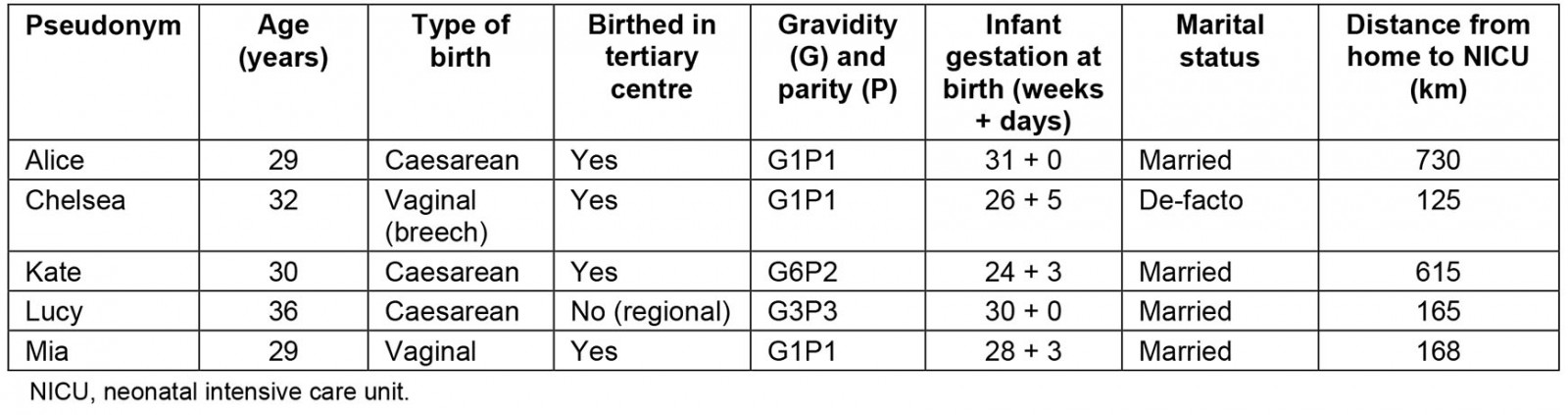
Emotional trauma
Participants described their experience as traumatic. Participants used words such as ‘stressful’, ‘scary’, ‘shock’, ‘chaotic’, ‘surreal’, ‘awful’, ‘helpless’, ‘traumatic’, ‘guilty’, ‘anxious’, ‘sadness’ and ‘failed’. The inability to take on the primary caregiver role led to strong feelings of ‘frustration’, ‘helplessness’ and ‘disappointment’.
It was pretty traumatic … that mourning process of not having that attachment, having to … care for your baby in a humidicrib, was very different to what you thought would happen … seeing how vulnerable they are … but it’s all out of your hands. (Chelsea)
Lucy became emotional when describing her experience. As she was about to be transferred from the regional hospital to the city with the emergency transport team, she explained:
I said goodbye to my husband, … when heading out the door … I said, NO! He’s coming now … we’re not going to make it. They thought I was having a panic attack. We went back in [to the regional hospital] and I was fully dilated … it happened so quick. It was horrible. (Lucy)
Participants felt that being separated from their infant was ‘not natural’ and ‘didn’t feel right’.
I got quite emotional … The whole ‘it’s not fair’, why do I have to go through this. It’s not what it’s meant to be. Just sadness and anxiety that I had to leave my baby there. It’s just not a natural thing to do. (Alice)
Guilt was a major emotion that resonated with all the participants and was particularly evident when they were required to leave their infant. Kate said, ‘I should be at the hospital in case something happens’. Mia also described her trauma of leaving her baby, ‘It’s … terrible, so hard. Guilty … how dare I go and enjoy a good night sleep’. Similarly,
It was a month before I went home for a visit. I was so stressed something would happen and I was anxious that he’d notice I was gone … he might open his eyes and I’m not here. (Chelsea)
The emotional trauma experienced by the women was interconnected with social displacement, due to leaving their newborn infant or family behind.
Social displacement
Given their impending preterm birth, participants were recommended to transfer to the closest metropolitan tertiary centre to enable the care required to reduce the morbidity and mortality risks for their infant. The need to transfer to the tertiary centre was a somewhat forcible displacement for the participants from their rural communities. After the birth of their infant and discharge from the postnatal unit, it was through the innate values and moral obligations of motherhood that the displacement continued, as the participants chose to temporarily live close to their baby while in the NICU. This was to establish bonding, the role as the primary caregiver, and to provide breastmilk for their infant’s nutrition and growth. As such, participants were required to adjust to motherhood, while living in unfamiliar surroundings and being thrust into the foreign environment of the NICU setting, routines, rules and regulations.
Participants also expressed concern for their other children due to the separation from the family. Lucy spoke of how she felt ‘torn’, particularly on birthdays and Mother’s Day.
We didn’t have our other two children … they were with their grandparents … that was really hard being away from them … felt like I wasn’t being a good mum to them … I just felt really bad. I was so far away. (Lucy)
On being separated from her toddler, Kate also expressed a similar feeling, ‘… it just felt like I was being ripped in two different directions’. This displacement caused much disruption to the participants’ lives and there was a great desire for all women to return home to their normal lives.
Socially it’s been hard … only having contact with my husband and mum … being away from them for so long and not having them be able to come and have those social catch ups took its toll after a while. (Alice)
External coping resources
‘External coping resources’ was the overarching theme describing the unique responses to the way the women coped with various stressors related to their infant’s admission to the NICU. It incorporates three subthemes: desiring emotional support, requiring practical support and needing peer support.
Desiring emotional support: All participants reported relying heavily on their partners for comfort, care and reassurance, and to discuss their fears and anxieties. This support was sometimes impaired due to partners not being able to accompany the participant or having to return to work. In the absence of their partner, women turned to their own mothers for emotional support. Kate recalls being transferred 615 km to the tertiary centre to give birth:
We both are really good at being able to talk to each other or when we need to reach out for help. But it was pretty scary. My husband wasn’t allowed on the flight. He had to drive, so he drove through the night. (Kate)
Chelsea said, ‘my partner stopped working for three weeks just to support me, because I guess for me, my anxiety was quite high’. Despite Alice staying in the hospital’s hostel at no cost, the hostel was for women only and her husband was not allowed to stay with her. Alice explained, ‘It wasn’t ideal staying by myself, I’d rather be with my husband. Without my husband or without my mum being there, you know, that was a bit stressful’.
All participants reported that they felt reassured by the consistency of the same nursing staff caring for their infant and that it provided them with the opportunity to build rapport with staff. This helped to relieve some anxiety when they left the NICU each night:
They knew what our baby needed. It worked well doing shared care as they also knew us. I didn’t have to re-explain myself to new nurses. (Alice)
Participants did however feel let down with the lack of emotional support offered by staff in the NICU. Three participants mentioned a lack of privacy, and that overhearing bad news being delivered to other parents affected them emotionally. Despite these experiences, the NICU staff did not counsel them about their distress. Chelsea recalled having to put on a brave front, then going off and ‘crying in the expressing room’. Similarly, Lucy explained:
There were days where we had pretty bad days … I had to just take things up with my own doctor. (Lucy)
Mia explained that, despite having a pre-existing mental illness, no additional support was offered through a perinatal psychiatrist or psychologist. She responded:
… I was open about it from the beginning, which I sometimes hesitate to do … and they knew I had a history of anxiety and depression. It was very much, ‘oh goodbye, you’ve had your baby, we’ll look after her [baby] and all the best’. I had to call the hospital asking for a debrief. (Mia)
Requiring practical support: All participants reported that having accommodation close to the NICU, along with practical and financial support, was highly valued once discharged from the postnatal unit. After weeks of separation from her toddler, one participant was eventually able to have a family room:
We are most grateful for having somewhere to stay so close. It has taken a huge chunk of financial burden from us. If we had to stay in a place far away from the hospital, it would just add another level of stress. (Kate)
Some of the accommodation facilities did not have free parking, cooking facilities or fridges, which forced participants to buy take-away food or eat out in restaurants, which was expensive given the long-term requirement for their displacement.
We have to pay [for parking] … I think with things like that, probably there could be some leniencies or sympathy. We didn’t have any cooking facilities in the place we were in. Even if I were to make a meal, I couldn’t store it anywhere. We did have savings, but we blew it all. The money was a bit of a stress to be honest. (Chelsea)
Participants relied heavily on their parents for practical support, which included financial assistance, and taking care of their other children. There was also stress associated with the maintenance of property and the care of animals back in their rural home town while temporarily living in the city. Participants found themselves relying on family, and even neighbours, to perform these roles in their absence. Alice explains:
We do have animals, that was a bit stressful ... having to ask someone to mind your animals for three months. We did consider popping them in a kennel, but it was going to be thousands and thousands of dollars. (Alice)
With all participants planning to work much longer into their pregnancy, they found that maternity leave was inflexible and did not take preterm birth into consideration:
I had to take my computer in to hospital to work, as I didn’t have any paid leave. There should be more flexibility around leave. People just don’t understand that premmies are not the same as a term baby. (Mia)
Needing peer support: All the participants reported that connecting with other mothers in the NICU was pivotal in supporting their journeys. Although they acknowledged the care and concerns conveyed by their friends and extended family, they felt that other mothers who were going through a similar experience were better able to empathise and comprehend what they were going through:
When we first got there, we became friends with a lady … so she kind of paved the way for us in our expectations … it’s been really good to have someone else going through it. Another couple have just moved into the accommodation the last couple of weeks [from a rural area] … so I feel like we’re kind of paving the way in their expectations which has been nice. (Kate)
Women felt that a mentor program in the NICU would have been helpful. Two women found great support from women who also had an extremely preterm baby:
It was nice to have someone that understood the language of the NICU … the NICU code. It’s nice to almost have, I guess, a mentor through the process. There’s not a lot regionally once you get home, it’s all city based. Having someone that’s been through it before, even if it’s just a messaging service, just as reassurance. I think that would be a benefit as well. (Alice)
All participants felt they needed to connect with women in their local region who had also experienced very or extreme preterm birth for support and guidance, especially after discharge. Participants felt that women who had given birth to infants born only a few weeks preterm were unable to understand their concerns or relate to their experience in the NICU:
I did try to connect with a mothers’ group here actually [in the rural setting after discharge]. I asked if anyone else had a prem baby and someone said, ‘yes, a thirty-six-weeker’. I was like NO! That’s not prem! I mean, I know everyone is on their own journey, and it probably was [a preterm infant] to her. But it’s a very different support network [to connect with women with very preterm infants]. (Chelsea)
There were some disadvantages of building a support network with other mothers from the city. This was due to participants returning home to their rural areas and becoming separated from their city support networks. After discharge, when the time came for the participants to catch up with the other mothers from the NICU in person, distance then became a barrier:
A lot of women were from there [the city]. I think that’s hard, because they are living in that area, it’s not so easy for me to like, just catch up for a cup of coffee with a few of those mums for half an hour … that’s been difficult keeping up those connections. (Chelsea)
Lucy did not have the opportunity to talk with other mothers in the NICU, since there were no structured times to facilitate this, and she said ‘I really wish I had spoken to other mums more in the unit [NICU] … like people who have gone through similar experiences … a networking thing I think would be good’.
Craving continuity of care
Participants reported a lack of coordination and communication in their infant’s transition from the NICU to either a lower level nursery or regional health service when discharged from the tertiary service. These periods of transition were stressful, and participants felt they were not provided with referrals to appropriate specialists for their infant’s follow-up and that health professionals in the regional health services did not have the knowledge to provide appropriate care and support:
Going from such specialised staff back to where they barely know what they are doing, it was really tough. They just weren’t as careful … I had to keep a close eye on things … that was a whole lot of other stress. We didn’t have that same level of trust in the staff. (Mia)
Participants voiced that local community services and support groups in the rural and regional areas did not have experienced healthcare workers who understood the neurodevelopmental aspects of the very preterm infant.
… once you’re discharged, that’s kind of it … you’re sent off into the oblivion. I felt like NICU mums get sort of forgot … some gaps around that support once the babies are no longer fragile anymore … when they get close to getting home, everyone sort of takes their foot off. I mean, I’ve now got my council mothers group with babies who were born when [baby] was born, but they were developmentally 3 months ahead of her … a really big oversight by the council groups. The things they were saying or suggesting for us to do with her [baby] were not appropriate. It would be great if they even just connect you with the same gestation with the premmie mums. (Mia)
Three of the participants reported that they had to organise follow-up paediatric care for their infant’s medical issues themselves after discharge. This included private specialist paediatric appointments and having to pay for a private lactation consultant to be able to continue breastfeeding successfully. They were not linked in with any specific preterm birth supports or specialised services on discharge home:
Once we got home, the contact with them [tertiary hospital] stopped. We were linked in with our local infant health service, but I just lost all confidence when we went there because they don’t see a lot of prems and any of the questions I had, they couldn’t answer. It just made me withdraw from their support … so I did lots of ‘Googling’. (Alice)
Due to the lack of experience by the medical profession with regards to very preterm infants in their rural and regional areas, participants returned to the tertiary centre for their infant’s investigations and procedures. Although it was an inconvenience (a 14-hour round trip twice for one participant), they felt ‘more comforted’ by this, given the appropriate experience of the staff in the city.
Discussion
This study aimed to understand the experiences of women from RRAs in Australia who have a preterm infant at 32 weeks gestation or less in an NICU. Although the findings from this study support existing literature15-18 some specific elements unique to the women from rural areas compounded their emotional trauma. These were associated with the social displacement experienced by all participants due to tertiary centre transfer and being separated from their partners, children and extended family.
Emotional trauma, compounded by social displacement, may predispose women from RRAs to longer term mental health conditions. If not managed appropriately, this could contribute to poor outcomes with regards to the long-term psychosocial development of their infants19. Griffiths described how forcible displacement embodies feelings and emotions of a ‘refugee condition’ (p. 99)20. By leaving their home, arriving in an unfamiliar location, and adjusting to a new environment, people are left in a state of uncertainty, indefinite waiting and imperfect knowledge of the situation, with feelings of fear, threat and anxiety20. Although participants in this study were somewhat forcibly displaced, they were not fleeing their home permanently due to political or civil unrest as is often the case with refugees in the current displacement research20,21. Hirani and Richter explained that being in a ‘refugee condition’ can still leave a woman experiencing psychological issues, having adjustment difficulties to the parental role and feeling vulnerable to exploitation21. This may be similar for a woman from an RRA transferring to a tertiary centre for preterm birth, as their life transforms from a place of familiarity and security to one of disruption and apprehension. This was certainly the case for the participants in this study, and this was not evident in previous literature12,22. Further research into the social displacement experience for women with preterm infants from RRAs – to avert any long-term negative sequelae – is warranted.
While the effects of social displacement are concerning, RRAs are not equipped to deal with high-risk birth populations and must be transferred to a tertiary centre for ongoing care23. Participants were aware to some degree of the maternal and neonatal capability in their region and of the understanding that tertiary centre care was crucial for the best outcomes for their infant. They also knew they would eventually return home, even though an indefinite time frame led to anxiety and frustration. Regardless, the short-term disruption to their ‘normal lives’ created many psychosocial challenges. Health professionals must understand the impact of emotional trauma and displacement on the wellbeing of women from RRAs with a preterm infant in the NICU.
Within the NICU, the family-integrated care model has been adopted internationally and forms part of the clinical practice framework for midwives and nurses24,25. Family-integrated care incorporates a range of services and activities – including educational, psychosocial and behavioural – that aim to place the family central to care planning, care delivery and decision-making for the infant26. Participants in this study described a range of support needs, including emotional support, practical (or instrumental) support and peer (or network) support. In relation to desiring of emotional support, the findings from this study concur with other studies that highlight women’s partners as the primary providers of emotional support18,19. However, this study also added to the existing literature that, in the absence of partners, women from RRAs utilised their mothers to meet their emotional needs. This is an important consideration, since four of the women in this study found themselves alone when their partners had returned to their rural communities for work.
People living in RRAs generally have lower incomes than those in urban areas but pay higher prices for goods and services27,28. Although socioeconomic status was not assessed in this study, having a preterm birth placed financial constraints on the families, and at times the women reported receiving financial assistance from extended family. Participants also relied heavily on extended family, friends and neighbours for practical support, including taking care of other children, property and animals while they were away. However, not all extended families may be in a financial position to do this.
Subsidised accommodation close to the NICU was valued and it relieved some of the financial burden for participants; however, there were other associated expenses. For RRA families, a short outpatient appointment or a small procedure with a specialist could mean a round trip of 2 or 3 days – involving travel, accommodation and food costs29. None of the participants in this study identified as Aboriginal or Torres Strait Islander; however, a study with Aboriginal Peoples from RRAs found that travelling to a city hospital was a significant barrier for them – financially and in terms of time and distance29. The time and cost of travel back and forth to the NICU was not recognised as burdensome by the healthcare system. Although the Australian Government subsidises some travel expenses for people accessing specialist care through urban outpatient clinics, barriers created by distance – including lack of public transport, poor communication and unfamiliar hospital processes – can be difficult to overcome30.
The availability of peer support in the NICU was clearly important to all participants in this study. The lack of structured opportunities for mothers to share stories and support each other was limited. This supports a recent study where mothers were asked about how improvements could be made to their care31. Hall et al concurred with these findings and provide insight into how comprehensive family support programs and designated areas where mothers can meet should be implemented in the NICU as part of family-integrated care32. They explained how trained mentors should be assigned to new parents within 3 days of an infant being admitted32. Mentorship is a concept that needs to be explored further within the NICU setting, to determine how it may benefit the psychosocial wellbeing of women from RRAs in the long term.
The specific needs of families of preterm infants does not simply end on discharge from the NICU. Women from RRAs craved continuity of care after discharge. Although they sought trusted health providers in their local area who had experience with very preterm infants, these did not exist. These findings are similar to those of Shepherd and Woodgate11, who also found that parents living in rural communities emphasised the importance of having a local healthcare provider that they trusted and that knew their child’s condition. The parents found that being able to get in contact with their healthcare provider at the tertiary centre after discharge was reassuring11. On discharge from the NICU, it may be reassuring for women in RRAs to have access to a phone or messaging service within the tertiary centre for support. Having early referral and access to appropriate city-based specialists via telehealth could potentially reduce the need for further episodes of displacement33,34.
The lack of appropriate community support led women to withdraw from local rural health agencies, as women felt health providers were unable to provide answers or correct advice about their preterm infant’s condition. This highlights a gap in knowledge of some rural health service providers expected to provide ongoing follow-up care of preterm infants after discharge. Yet existing literature emphasises the importance of referring women and preterm infants to appropriate health agencies post-discharge from the NICU as, without this care, women are placed at greater risk of postnatal depression and infants at greater risk of poor neurodevelopmental outcomes12,23,35. The women in this study, although struggling to find appropriate health and support services, did not receive any follow-up regarding their mental wellbeing as recommended by the Australian Perinatal Mental Health Guideline36. This was a concern given that one participant had a pre-existing mental illness.
Limitations
While the concept of ‘saturation’ is commonly used in qualitative methodology, experts explain that researchers should not be locked into a specific sample size, but rather obtain an understanding of the depth and richness of the data being investigated37,38. The concept of ‘information power’, rather than saturation, has been proposed to guide adequate sample size for qualitative studies, particularly when a low number of participants provide information relevant for the actual study39. Although it was difficult to recruit a larger sample size due to the vulnerability of the target population, the sample size – although illustrative – is not representative and may require further confirmation.
The initial plan to recruit participants within the NICU setting and for face-to-face interview was not possible due to the COVID-19 pandemic restrictions imposed at that time. The online recruitment method via social media may have attracted women who were already comfortable using social media platforms. However, it does demonstrate that some women are in search of support via online support groups. Lastly, it is not known how RRA experiences might differ from those of women residing in urban areas. Examining experiences of both groups is an important next step in providing quality care in the NICU and beyond.
Conclusion
Women from RRAs with a preterm infant in the NICU reported experiencing emotional trauma impacted by social displacement. Funding should be considered for the extended family to stay in appropriately equipped accommodation facilities with the woman, for ongoing psychosocial and financial support during the infant’s NICU admission. Women from RRAs highly valued peer-to-peer support from other mothers in the NICU; however, these relationships were difficult to maintain once they returned home. Further research into RRA support groups for women with preterm infants may be considered; however, facilitation and logistics would need to be explored to ensure they meet the needs of these women. Women sought continuity of care by appropriate health professionals in their local community who understood their experience and the neurodevelopmental concerns of their preterm infants. Additional training for health professionals in RRAs in the follow-up of preterm infants may assist in build trusting relationships between women and health professionals, and potentially minimise the burden of returning to the city for follow-up appointments. Further research into the psychosocial aspects of social displacement in the NICU of women from RRAs is warranted, and it is recommended that Aboriginal and Torres Strait Islander women are also represented. The experience of women from RRAs may assist health professionals in NICUs and RRAs as a guide to develop and implement appropriate services and resources in the future for women in RRAs with a preterm infant.

