Introduction
Acute appendicitis is the most common surgical emergency worldwide1. Generally, most patients with appendicitis (80–87%) present with uncomplicated appendicitis and do not present with gangrene, perforation, appendicular abscess, or phlegmon formation2. Although antibiotic treatment has been proven safe and effective for uncomplicated appendicitis3,4, appendectomy remains the preferred option for acute appendicitis in most cases2,5,6. Increasing severity and worse outcomes of appendicitis have been demonstrated in rural, lower socioeconomic, and Indigenous populations, resulting in more severe economic and social burdens7,8.
The pre-interventional differentiation between complicated and uncomplicated appendicitis is decisive for treatment. However, it is still challenging to make this diagnosis preoperatively. Scoring systems can help in quick diagnosis and decision-making. The Alvarado score is the best-known scoring system based on clinical parameters for the diagnosis of acute appendicitis. The World Society of Emergency Surgery guidelines for the diagnosis and treatment of acute appendicitis recommend the use of the appendicitis inflammatory response score (AIRS) and the adult appendicitis score (AAS)9. Furthermore, the Raja Isteri Pengiran Anak Saleha Appendicitis (RIPASA) score is a scoring system developed for Asian and Middle Eastern populations10. It is reported that certain scoring systems, such as AIRS, have high sensitivity for complicated appendicitis and identify subgroups with low probability of complicated appendicitis or high probability of appendicitis11. It has also been found that incorporating imaging features into clinical scoring models may provide better differentiation between uncomplicated and complicated appendicitis12. However, others have insisted that these scoring systems have limited capability to distinguish between complicated and uncomplicated appendicitis even with additional imaging13.
Economic and social developments are relatively backward in Tibet, and the level of health care is relatively low compared to in coastal China. Several studies have found that the disease spectrum of residents of the Tibetan Plateau differs from that of other regions, especially coastal China and Western countries14-16, which may be related to the high altitude, alpine characteristics, and genetic differences. The Chinese government has established an area-wide basic medical insurance system in Tibet, covering rural areas. Meanwhile, the vast majority of local Tibetan residents are devout Tibetan Buddhists with unique insights on issues such as illness, life, and death. These aspects indicate that Tibet is a region with a unique social and cultural background compared to other rural areas. To date, no studies have examined the clinical characteristics of acute appendicitis in rural Tibetan areas or the application value of risk prediction models. Therefore, using Chaya County as a sample, we explored the clinical characteristics of acute appendicitis and the practicability of these models for rural Tibetan residents.
Methods
Study population and data collection
This retrospective observational study was conducted at the Department of Surgery, Chaya People’s Hospital, Tibet. From 1 April 2018 to 30 September 2021, medical records of consecutive patients complaining of abdominal pain were reviewed, and demographic data, medical history, clinical data, and laboratory features were collected from the clinical records. Patients treated on an outpatient basis and those referred to higher-level urban hospitals without operation on the day of admission were excluded. Standardized data-collection forms were completed by investigators blinded to the study outcomes. The duration of onset was measured from the presence of symptoms to the admission time. The patients’ laboratory values were obtained at the time of the emergency department visit.
Diagnosis
Since establishing the Department of Pathology at Chaya People’s Hospital in late 2019, all surgically excised specimens have been subjected to pathological examination, and the final diagnosis of appendicitis has been pathologically determined. Previously, the diagnosis of surgical specimens could only be determined by the surgeon according to what was observed intraoperatively. Perforated and gangrenous appendicitis and appendicitis with abscess or phlegmon formation are complications of appendicitis.
Moreover, a diagnosis of appendicitis is accepted for non-operated patients when it is reported by using ultrasonography (US) and/or CT, followed by conventional imaging diagnostic criteria. The following US findings indicate acute appendicitis: non-compressible, >6 mm outer diameter, appendicolith, target appearance in axial section, and periappendiceal inflammation with fat stranding17. The following CT findings indicate acute appendicitis: dilated lumen (≥7 mm), appendicolith, periappendiceal fluid collection, and inflamed mesoappendix18.
Appendicitis risk prediction models
The Alvarado score included eight parameters with a total score of 10. The higher the score, the greater the risk of acute appendicitis. It was later modified to seven parameters, and the highest possible score was 919. The AIRS consisted of eight parameters with a maximum score of 1220. The AAS included seven parameters with a maximum score of 2521. The RIPASA score involved 15 parameters with a maximum score of 1510. The obtained data were used to calculate the modified Alvarado score, AIRS, AAS, and RIPASA score. The sums of all the scores were calculated for each patient. According to the results, patients were divided into two groups: the high-suspicion group and the low-and-intermediate-suspicion group.
Outcome measure
Postoperative hospital stay was defined as the period between operation and discharge. Postoperative hospital stay was recorded as 1 day for patients discharged (transferred) on the same day they underwent the operation. Complications that occurred during postoperative hospital stay were recorded. Hospital costs were calculated by summing all the items enumerated in the hospital discharge summary. The costs expressed in this study were in US dollars. In 2021, US$1 was equivalent to approximately 6.45 Chinese yuan.
Statistical analysis
The data were analyzed by using SPSS Statistics v26.0 (IBM Corp, https://www.ibm.com/products/spss-statistics). Descriptive statistics for categorical data were expressed as numbers and percentages. Continuous variables were presented as medians and interquartile ranges (IQR) and compared by using the Mann–Whitney U-test. Fisher's exact test was used if the expected count of at least one cell was less <5 in a 2×2 table. Variables with p<0.10 in the univariate analysis were selected for a multivariate logistic regression model (method=enter) to analyze the independent predictors of complicated appendicitis. Chi-squared tests were used to compare percentages, and p<0.05 was considered significantly different.
Screening performance characteristics of the scoring system were also measured. Binary logistic regression was applied to calculate the predictive probability of scoring systems for the diagnosis of acute appendicitis. Receiver-operating characteristic (ROC) curves were constructed by using the predictive probability as a covariate. The index of union (IU) method was applied to identify the optimal cut-off value for critical values of risk prediction models. The approach is based on the areas under the ROC curves (AUCs), sensitivity, and specificity values. It defines the optimal cut-off value as the point minimizing the summation of absolute values of the differences between AUC and sensitivity and AUC and specificity, provided that the difference between sensitivity and specificity is minimum22.
Ethics approval
The study was conducted according to the Declaration of Helsinki and approved by Chaya People's Hospital Ethics Committee (202101). Due to the retrospective nature, Chaya People's Hospital Ethics Committee approved informed consent waiver for this study.
Results
Chaya County is located in the Hengduan Mountain area of eastern Tibet, with an average altitude of 3500 m. Chaya People’s Hospital has 85 beds and is the only general hospital in this region. In 2020, it served a population of 76 300 people, of whom more than 95% were farmers and herders, spread over 8300 km2. In 2020, the county’s gross domestic product (GDP) per capita was approximately US$3300 (A$4400).
Between 1 April 2018 and 30 September 2021, a total of 225 patients were admitted for abdominal pain, of whom 132 underwent surgery, including 93 appendectomies for appendicitis. The diagnoses of 93 patients who underwent appendectomy included 55 (59.1%) cases of uncomplicated appendicitis and 38 (40.9%) cases of complicated appendicitis, including 29 (31.2%) cases of gangrenous appendicitis, 7 (7.5%) cases of perforated appendicitis, and 2 (2.2%) cases of appendicular abscess.
Basic characteristics of patients who underwent appendectomy
As shown in Table 1, complicated appendicitis was more common than uncomplicated appendicitis in men (68.4% v 47.3%; p=0.043) and those more than 30 years (68.4% v 41.8%; p=0.012). No significant differences were noted between the two groups regarding ethnicity, occupation, residential altitude, and distance to the hospital. However, for duration of onset, significantly more patients with complicated appendicitis had abdominal pain for >24 hours than those with uncomplicated appendicitis (65.8% v 38.2%; p=0.009).
Table 1: Basic characteristics of patients who underwent appendectomy in this study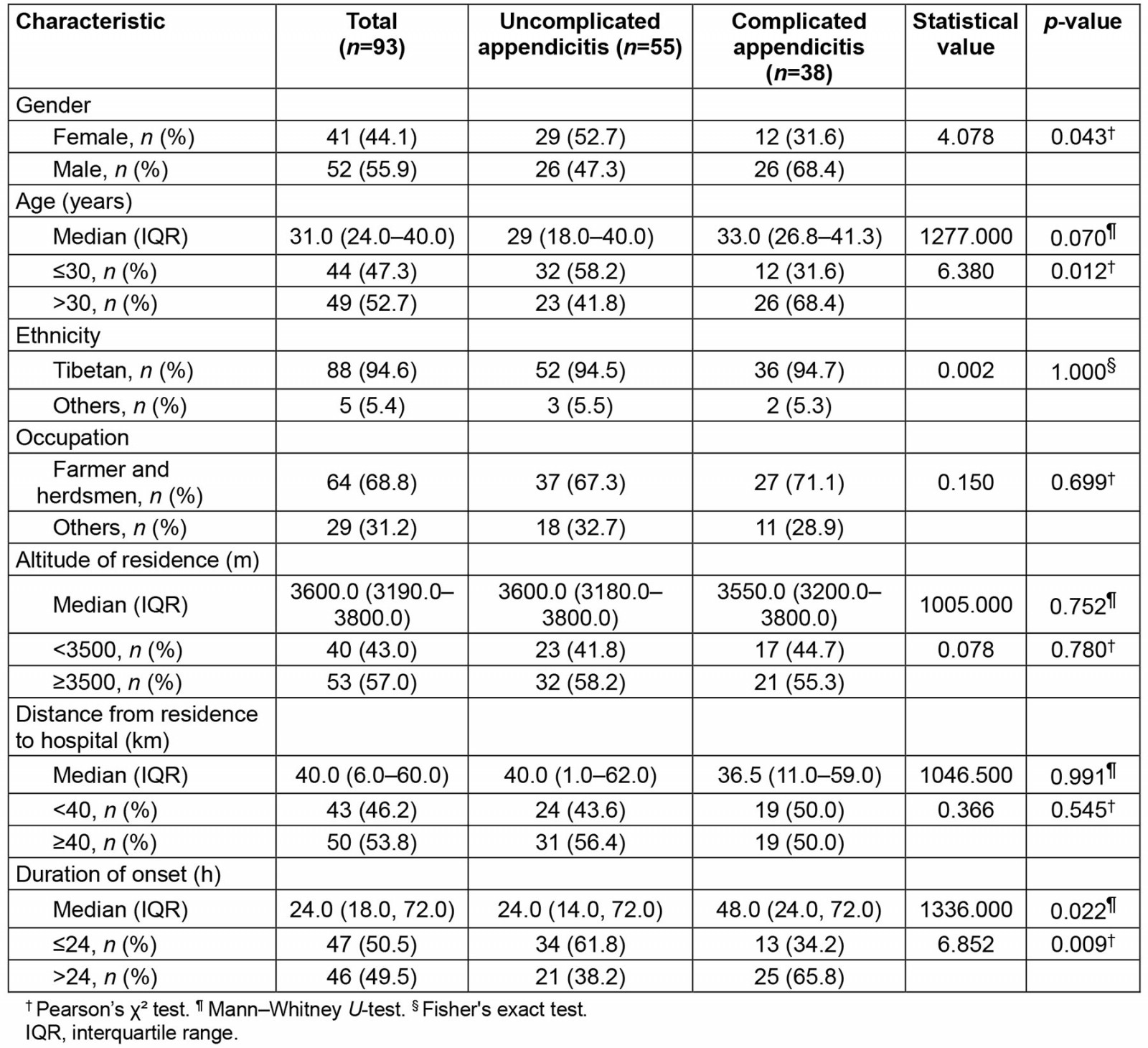
Clinical characteristics of patients who underwent appendectomy
As shown in Table 2, at the time of presentation, the main symptoms and signs (frequency >50%) of appendicitis in patients who underwent appendectomy were right lower quadrant (RLQ) tenderness (100.0%), RLQ pain (97.8%), rebound tenderness (88.2%), nausea or vomiting (75.3%), and migratory pain (59.1%). A higher proportion of patients with complicated appendicitis presented with fever than those with uncomplicated appendicitis (31.6% v 9.1%; p=0.006). No significant differences were found between the two groups for other signs and symptoms. Since RLQ tenderness is physical-exam based and RLQ pain is complaint based, sometimes the two may not be consistent.
Regarding laboratory tests at admission, patients with complicated appendicitis had higher white blood cell counts and neutrophil ratios, as well as higher C-reactive protein (CRP) levels, than patients with uncomplicated appendicitis. Additionally, this cohort showed that the presence or absence of positive findings on ultrasound and CT and whether routine urine test results were abnormal did not differ significantly between the two groups. However, owing to instrument failure or reagent shortage, only 19 patients in this cohort completed the CRP test. Similarly, because of limited technical conditions, only a few patients completed routine urine, ultrasound, and CT tests.
This study found that a higher proportion of patients with complicated appendicitis had a modified Alvarado score of ≥8 than the uncomplicated appendicitis group (31.6% v 12.7%; p=0.027). No significant difference was identified between the two groups of patients regarding whether they underwent open or laparoscopic surgery and the incidence of postoperative complications. Among the 11 patients with postoperative complications, nine cases of wound sepsis were included, and one case each of residual abdominal abscess and incisional bleeding. However, patients with complicated appendicitis had significantly longer postoperative hospital stay (11.0 (IQR 8.8–13.3) days v 8.0 (IQR 6.0–11.0) days; p<0.001) and higher hospital costs (US$2147.2 (A$2855.6) (IQR US$1625.1–2516.6) v US$1487.9 (A$1978.8) (IQR US$1202.6–1809.2); p<0.001) than those with uncomplicated appendicitis.
Table 2: Clinical characteristics of patients who underwent appendectomy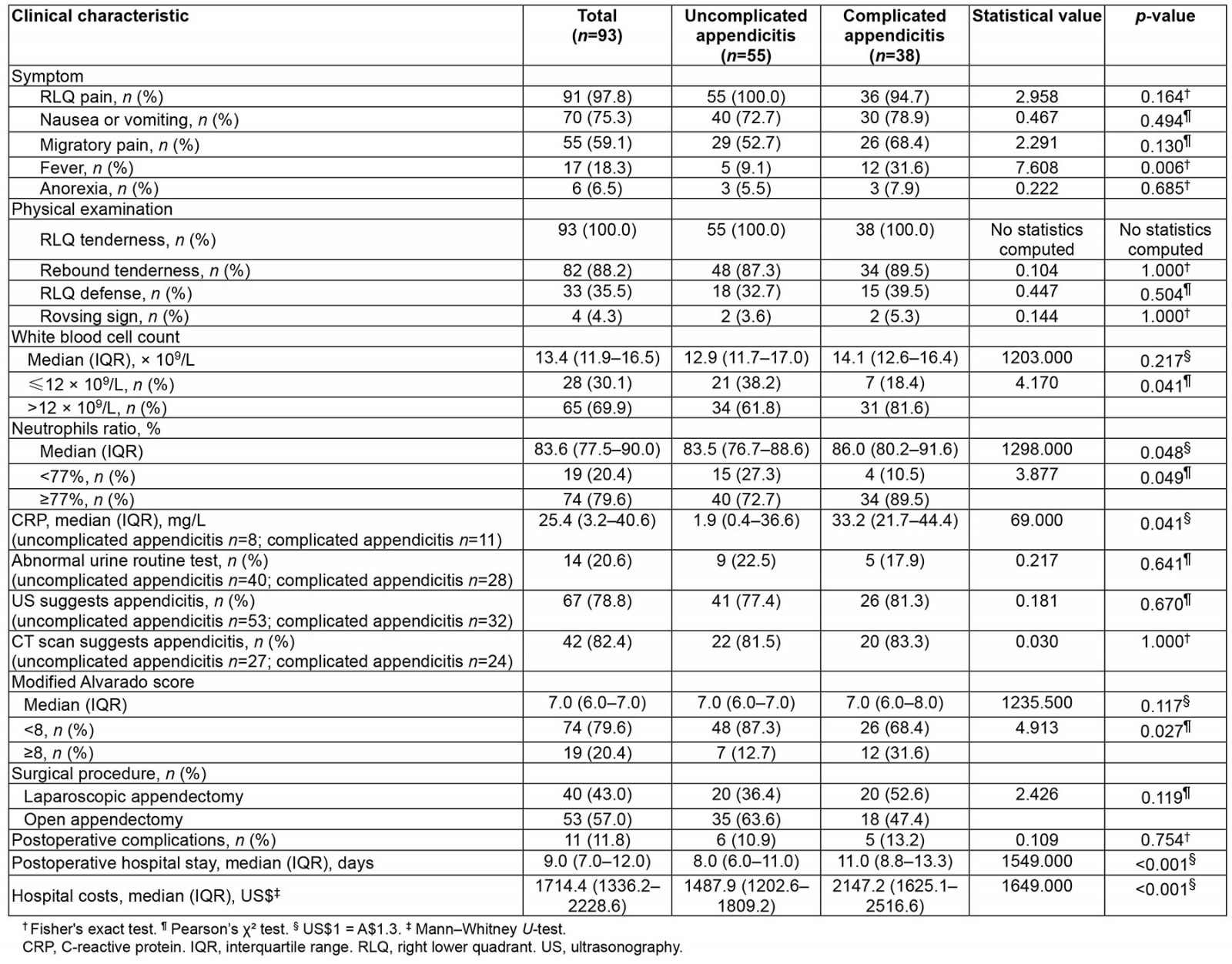
Multivariable analysis of factors associated with complicated appendicitis
Complicated appendicitis imposes greater social and economic burdens on patients than uncomplicated appendicitis does. Therefore, this study aimed to explore the risk factors associated with complicated appendicitis. As shown in Table 3, multivariable analysis revealed that duration of onset >24 hours, age >30 years, and male sex were independent risk factors associated with complicated appendicitis.
Table 3: Multivariable analysis of factors associated with complicated appendicitis in this study. A multivariate logistic regression (method=enter) was used in this model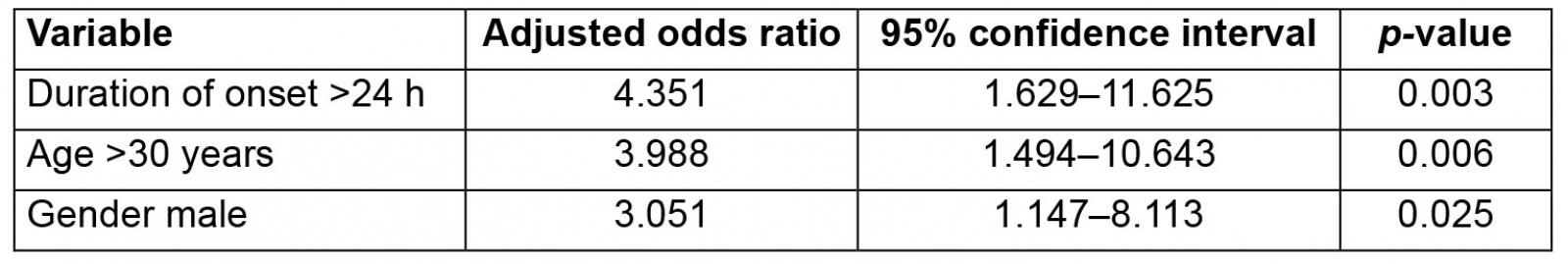
Evaluation of appendicitis risk prediction models
This study then evaluated the diagnostic value of the widely used appendicitis risk-predictive models for this cohort. In total, 127 patients complained of right lower abdominal pain, of whom 96 were treated surgically (including 91 with proven appendicitis), and 31 were treated non-operatively (including 22 with ultrasound or CT findings of appendicitis). Of these 127 patients, 113 were considered to have appendicitis, and 14 did not have appendicitis. Based on the clinical data collected, the predictive scores for appendicitis were calculated for each patient. Because of the lack of CRP tests in 92 patients and routine urine tests in 29 patients, the modified Alvarado score was finally calculated for 127 cases, the AIRS and AAS for 35 cases, and the RIPASA score for 98 cases.
As shown in Table 4, a modified Alvarado score ≥6 had the best diagnostic value, with an IU of 0.091, AUC of 0.760, sensitivity of 80.5%, specificity of 71.4%, and accuracy of 79.5%. An AAS≥13 had the best diagnostic value, with an IU of 0.046, AUC of 0.727, sensitivity of 70.4%, specificity of 75.0%, and accuracy of 71.4%. The best diagnostic value was achieved with an IU of 0.028, AUC of 0.764, a sensitivity of 77.8%, a specificity of 75.0%, and an accuracy of 77.1% for an AIRS≥6. The RIPASA score ≥7 had the best diagnostic value, with an IU of 0.042, AUC of 0.812, sensitivity of 79.1%, specificity of 83.3%, and accuracy of 79.6%. Overall, the AIRS showed the best performance among the four prediction models evaluated in this study.
Table 4: Identification and validation of optimal thresholds for risk prediction models in this study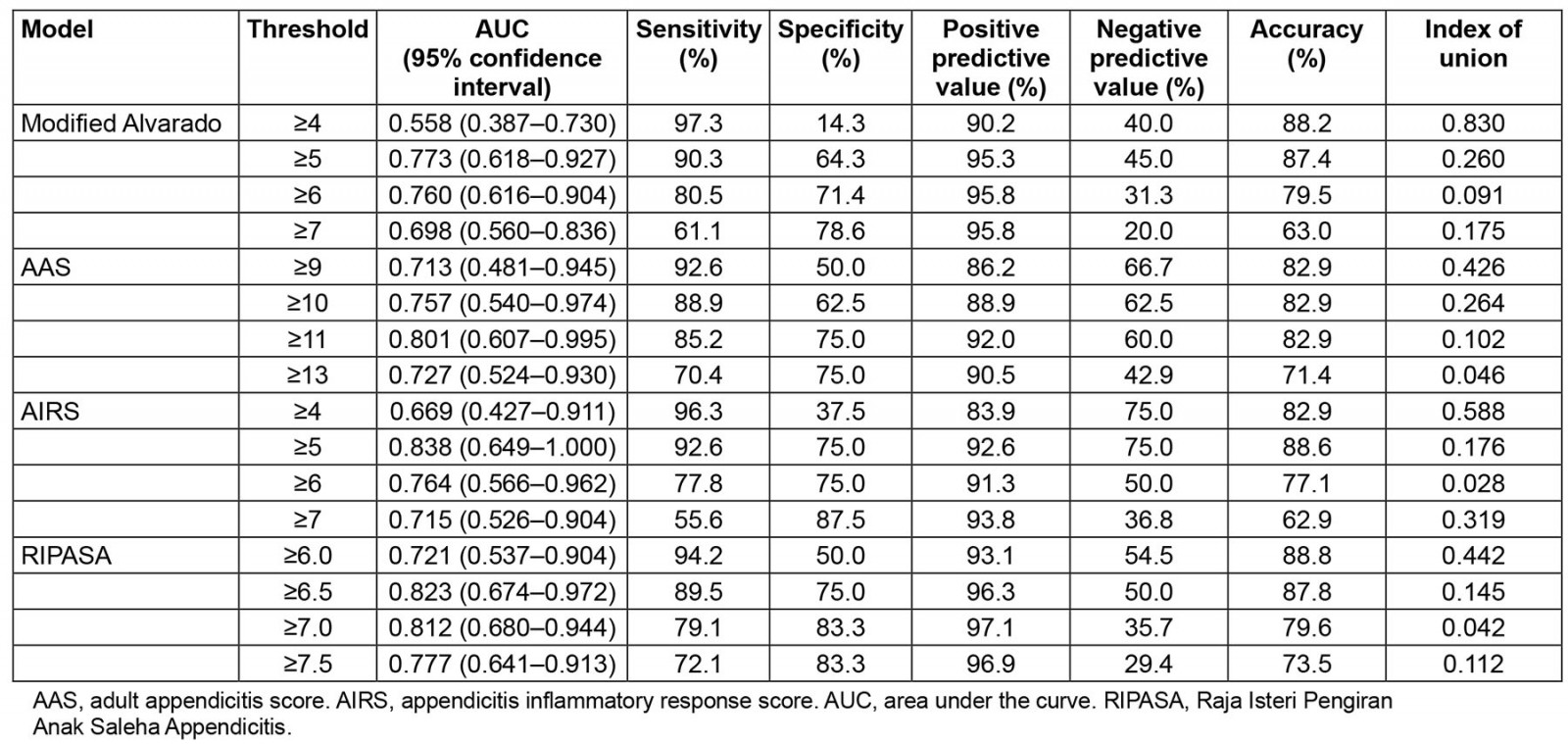
Diagnostic value of scoring systems combined with imaging examinations
First, this study evaluated the diagnostic value of CT and US for acute appendicitis in this cohort. A total of 132 patients were diagnosed definitively by surgery, 82 of whom underwent CT scan and 124 of whom received US examination preoperatively. Therefore, the diagnostic values of CT and US were evaluated separately in this study. As shown in Table 5, the IU, sensitivity, specificity and accuracy of CT in diagnosing acute appendicitis were 0.112, 82.4%, 93.6% and 86.6%, respectively. The IU, sensitivity, specificity and accuracy of US in the diagnosis of acute appendicitis were 0.135, 78.8%, 92.3% and 83.1%, respectively.
Finally, this study evaluated the diagnostic value of the risk-predictive models integrated with CT and US for acute appendicitis. As shown in Table 5, the integration of CT or US with the risk-predictive models improved their diagnostic value in most cases, as evidenced by the better IU values obtained. However, for most risk-predictive models, combining with imaging features did not further improve their predictive value. Only the combination of AAS≥13 and CT had an IU value of 0.044, which was slightly better than 0.046 for AAS≥13 only.
Table 5: Diagnostic values of computed tomography and ultrasonography, as well as combined with prediction models, for acute appendicitis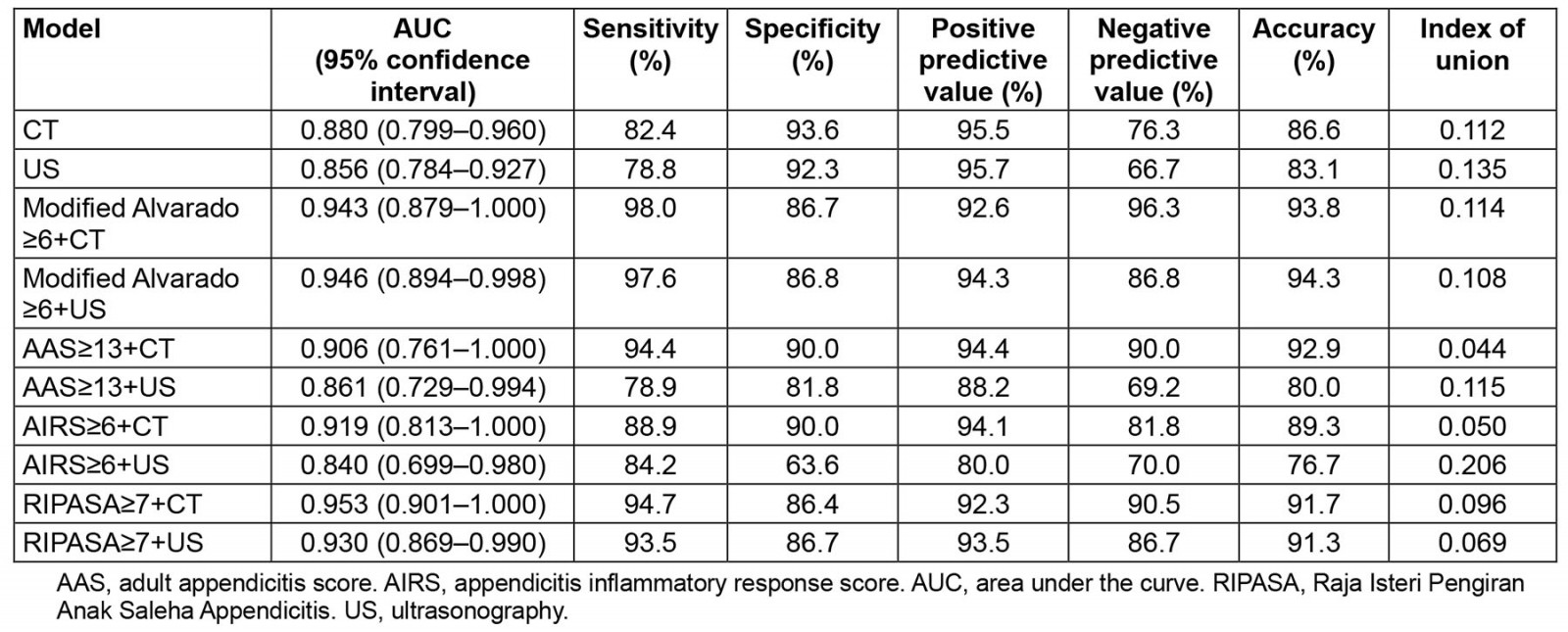
Discussion
This study showed that acute appendicitis was the most common abdominal surgical condition in rural Tibet, represented by Chaya County, accounting for 70.5% (93/132) of patients who underwent surgery for abdominal pain. In addition, patients with acute appendicitis in rural Tibet are generally younger, with a median age of 31 years, and have a higher disease severity, compared to data presented in other literatures, with a proportion of complicated appendicitis of 40.1%.
As reported in the literature, 5–28% of patients develop complications after appendectomy23. The rates of surgical incision infection after appendectomy observed in low and middle human development-index countries are much higher than in high human development-index countries24. However, the incidence of complications after appendectomy was not substantially high in rural Tibet, consisting of only 11.8% of patients in this study. Even in cases of complicated appendicitis, complications after appendectomy did not increase significantly compared to in cases of uncomplicated appendicitis.
The low incidence of surgical incision infection after appendectomy in our findings may be related to the unique environment in Tibet, such as high altitude, low temperature, atmospheric pressure, dry climate, and intense ultraviolet radiation. In addition, the unique lifestyle and diet of native Tibetans may have shaped the gut microbiota differently from that of populations living at lower altitudes. Moreover, the number and abundance of antibiotic-resistance genes are significantly higher in the gut microbiota of Han Chinese than in native Tibetans25.
This study showed that hospitalization costs for complicated appendicitis surgery were high, exceeding two-thirds of the local GDP per capita, resulting in heavy social and economic burdens. Identifying the risk factors associated with complicated appendicitis is crucial to improving the level of health care in Tibetan areas and the quality of life of local people. Studies have shown that complicated appendicitis has been linked to extremes of age, racial and socioeconomic disparities, public insurance, and remote residency7,26. Complicated appendicitis is more commonly seen in racial/ethnic minorities, low-income groups, and children27,28. In particular, the distance patients travel for their definitive surgical care correlates with higher rates of complicated appendicitis29-31. Geographic barriers affect the receipt of surgical care among children, particularly with regard to transplantation, congenital cardiac surgery, and appendicitis32. Racial disparities in the incidence of ruptured appendicitis may be more related to access to care and timely referral than disparities in care once the patient reaches a hospital.
However, in the present study, only demographic factors (age, sex) and duration of illness were confirmed to be independent risk factors associated with complicated appendicitis, whereas social (eg ethnicity, occupation) and geographical factors (eg altitude of residence, distance from residence to hospital) did not affect the occurrence of complicated appendicitis. One possible explanation is that residents were mostly devout followers of Tibetan Buddhism and often chose to pray first after the onset of illness or seek help from the monastery, where the lamas judged the need for hospital visits and even the choice of surgery needed to be ruled by the lamas. Therefore, the increased duration of the illness (delayed hospital visits) may have led to a higher incidence of complicated appendicitis. Importantly, local health workers have to find the best balance between religious beliefs and professional services for residents.
Moreover, this study found that the best cut-off values previously reported in the literature for the commonly used risk prediction models for appendicitis, whether the Alvarado score, the AAS and AIRS recommended by the World Society of Emergency Surgery guidelines, or the RIPASA score specifically for Asians, did not apply to patients in the Tibetan region. For example, for the Alvarado score, the best critical value reported in the literature is seven compared with five in our study; for the AAS, reported in the literature is 16 compared with 11 in the present study; for the AIRS, reported in the literature is 933 compared to 5 in the present study; and for the RIPASA score, reported in the literature is 7.5 compared with 6.5 in the present study. There may still be some specificity in the clinical presentation of patients with appendicitis in rural Tibet compared to other areas.
Although the AIRS demonstrated the best diagnostic value in this study, the Alvarado score seems simpler and more convenient to apply, making it easier to promote its use in remote rural areas of Tibet unless a more practical model is developed in the future. Several studies had described the capability of the AIRS and Alvarado score to discriminate between uncomplicated and complicated appendicitis12. The present study finds that the modified Alvarado score may be useful as a guide for differentiating between complicated and uncomplicated appendicitis. However, these results need to be confirmed through further investigation.
Many studies suggest that diagnostic imaging is recommended in suspected acute appendicitis patients, to confirm the diagnosis and to differentiate complicated from uncomplicated appendicitis34. This study showed that most of the patients with acute appendicitis in Tibet have typical symptoms and signs. Therefore, a definite diagnosis can be obtained by careful physical examination and inquiring about the patient’s history. Although imaging findings such as CT and US show high diagnostic value in acute appendicitis1,35, the varying skills of technicians in rural and remote areas may lead to a decrease in the accuracy of diagnosis. In this study, the sensitivity of CT for the diagnosis of acute appendicitis was only about 80%, which is lower than the 90–95% reported in most of the literature36,37. However, the specificities for both CT and US are above 90%, suggesting that CT and US have significant advantages for diagnosing non-appendicitis and help to reduce the rate of non-essential surgery. Furthermore, this study shows that incorporating imaging features in the prediction models may provide better diagnostic value for appendicitis. Therefore, integration of commonly used scoring systems, such as RIPASA, with CT or US findings may become a more suitable diagnostic model for acute appendicitis in rural Tibet.
This study had some limitations. First, the small population in the study area meant that few cases were involved in the study. Second, the technical conditions of the hospital led to the inability to complete some examination items, which may also interfere with the data analysis. Third, because this was a retrospective study, records of comorbidities were incomplete and therefore were not collected. In fact, due to the lower level of medical care in rural Tibet, most patients were unaware of their comorbidities prior to their visit. A well-designed multicenter prospective randomized controlled study may effectively address these issues and achieve more convincing results.
Conclusion
This study demonstrated the clinical characteristics of patients with acute appendicitis in rural Tibet and the application value of risk prediction models through a retrospective case analysis. If rural Tibetan people encounter RLQ pain, medical practitioners can make a relatively definitive diagnosis of appendicitis with the AIRS model, even without better technical conditions (such as CT scan).
Acknowledgements
We would like to thank Dr Hua Chen, a former biostatistician of Oklahoma Medical Foundation, for her valuable consultation on the statistics section of this article.
Funding
This work was supported by grants from the Science and Technology Benefiting People Program of Xiamen, Fujian Province, PR China (3502Z20184010).
Conflict of interest
The authors declare that they have no competing interests.
Data availability
The datasets analyzed during the current study are not publicly available but are available from the corresponding author upon reasonable request.
References
You might also be interested in:
2014 - Rural emergency medical technician pre-hospital electrocardiogram transmission



