Introduction
The Brazilian population is aging rapidly. According to projections of the Brazilian Institute of Geography and Statistics, in 2043 a quarter of the population will be older adults1. This process will have implications for the Brazilian health system2. Therefore, screening older adults at risk for worsening health can provide an opportunity for detection and intervention, thus preventing adverse clinical outcomes and enabling the most efficient use of health resources.
Vulnerability, defined as an increased risk of functional decline or death over 2 years3, is one of the adverse outcomes associated with the aging process and is associated with hospitalization and the use of emergency services4. The literature show different data on the prevalence of vulnerability among older adults. In Ireland it is 12.2%5, in Taiwan 35.8%6, in the Netherlands 51.0%7, and in Israel 83.1%8. Risk factors for vulnerability include female sex9-11, widowhood12, lower income, less education, depression13, arterial hypertension, and diabetes mellitus9.
The identification of vulnerable older adults is carried out using the Vulnerable Elders Survey (VES-13). The VES-13 is a simple tool that since 2014 has been recommended by the Ministry of Health of Brazil for the assessment of vulnerability among older adults in primary care settings14. Although VES-13 was originally developed to identify community-dwelling vulnerable older people, few studies have investigated the prevalence of vulnerability in this population, and even fewer have analyzed its associated factors.
Particularly in rural areas, aging results in greater health needs, in a population that traditionally suffers from a reduced supply of health services15. In most countries, rural areas face transportation and communication difficulties, inequalities in health financing, shortages and uneven distribution of health professionals, with worse working conditions16,17. Developing countries display situations of greater iniquities in rural health18. Brazil, despite the expansion of primary health care in the national territory, still registers strong social and spatial inequality in the provision of services, equipment and health personnel19.
To better understand this older rural population, which is often disregarded in epidemiological studies, it is important to study vulnerability and the factors that influence its development. Therefore, to provide useful insights into vulnerability, and to enhance policymakers’ knowledge of emerging issues and the needs of the growing older population, the present study aims to (1) estimate the prevalence of vulnerability, and (2) identify the associated factors of vulnerability among rural community-dwelling older adults living in the municipality of Rio Grande, Rio Grande do Sul, Brazil.
Methods
Design and setting
This study was a cross-sectional analysis of the EpiRural Cohort Study. The EpiRural Cohort Study is a prospective cohort that investigates and monitors the living conditions, health, and use of health services in a representative sample of community-dwelling older adults (≥60 years) living in the rural area of the municipality of Rio Grande in extreme southern Brazil.
Rio Grande is located 250 km from the border with Uruguay and about 300 km from the state capital, Porto Alegre. It has an area of approximately 2709 km², and an estimated population of 210 000, of which 4% live in the rural area, distributed in approximately 3000 households20. Currently, the definition of urban spaces used in Brazil is given by municipal legislation. The Brazilian Institute of Geography and Statistics, therefore, considers the rural area of a municipality to be outside its urban perimeter.
The baseline study was conducted in 2017. The studied population consisted of older adults living in the rural area of Rio Grande. The baseline sample was based on the 2010 Demographic Census. A selection process was used to select 80% of the inhabited permanent households. All the older adults of the chosen households were invited to participate in the study. The institutionalized older adults (long-term institutions, hospitals, and penitentiaries) were not included in the study. The first follow-up of the cohort was carried out between September 2018 and March 2019. Of the 1029 older adults included in the baseline, 862 were followed up, resulting in a follow-up rate of 83.8%. Further information about the research can be found in the methodological article21.
Procedures
Data collection was performed by six trained interviewers. All the respondents were interviewed face-to-face using structured questionnaires with REDCap (Research Electronic Data Capture)22. Two questionnaires were utilized. The household questionnaire was answered by the head of the household and aimed to characterize the household and family income. The individual questionnaire was answered by the older adult or their caregivers and investigated health issues, use of health services, lifestyle and behaviors. The anthropometric parameters evaluated were weight, knee height and calf circumference, standardized according to the method of Habicht et al23.
Vulnerability
Vulnerability was assessed using the VES-13. The VES is a 13-item questionnaire that considers age (one question), self-rated health (one question), physical function (six questions), and functional dependence (five questions). Scores range from 0 to 10, and scores of 3 or more classify older adults as vulnerable3.
Covariates
The assessed covariates were as follows: sex (male; female); marital status (without a partner; with a partner); education, in complete years of study (none; 1–4; 5–8; ≥9); presence of hypertension (no; yes); diabetes (no; yes); rheumatism/arthritis/arthrosis (no; yes); osteoporosis (no; yes); depression (no; yes); history of ischaemia or stroke (no; yes); fall in the past 12 months (no; yes); use of continuous medication (no; yes); sarcopenia (no; yes), assessed using the Strength, Assistance with walking, Rise from a chair, Climb stairs and Calf Circumference (SARC-Calf); max. 20 points, with a score ≥11 indicating sarcopenia24; and cognitive impairment (assessed through the Mini Mental State Examination (MMSE), with a maximum score of 30, where >23 points indicates normal cognition, 19–23 indicates mild cognitive impairment and ≤18 indicates moderate/severe cognitive impairment)25.
Statistical analysis
Data were analyzed using Stata v13 (StataCorp; http://www.stata.com). The sample description was performed by obtaining the proportion of individuals in each category of variables. Descriptive statistics were used to estimate the prevalence of VES-13 items (absolute and relative frequency). The prevalence between the categorical variables was verified through Pearson’s χ2 test. Crude and adjusted analyses were performed using Poisson regression, with robust adjustment for variance, prevalence ratios (PR), 95% confidence intervals (95%CI) and p-values. The adjusted analysis was performed using the hierarchical level model, in which the variables were adjusted for the same level, in addition to those of the previous level in the model. Those variables with p<0.20 were kept for adjustment, and this method was repeated for the other levels. For ordinal exposures, the p-value of the linear trend test was reported; for the other variables, the Wald test of heterogeneity was used, and p<0.005 was considered to indicate significant associations.
Ethics approval
The EpiRural Cohort Study was approved by the Research Ethics Committee of the School of Medicine of the Federal University of Rio Grande (protocol no: 51/2017; protocol no. 154/2018). Participation was voluntary, and informed consent was obtained. All participants voluntarily signed an informed consent form.
Results
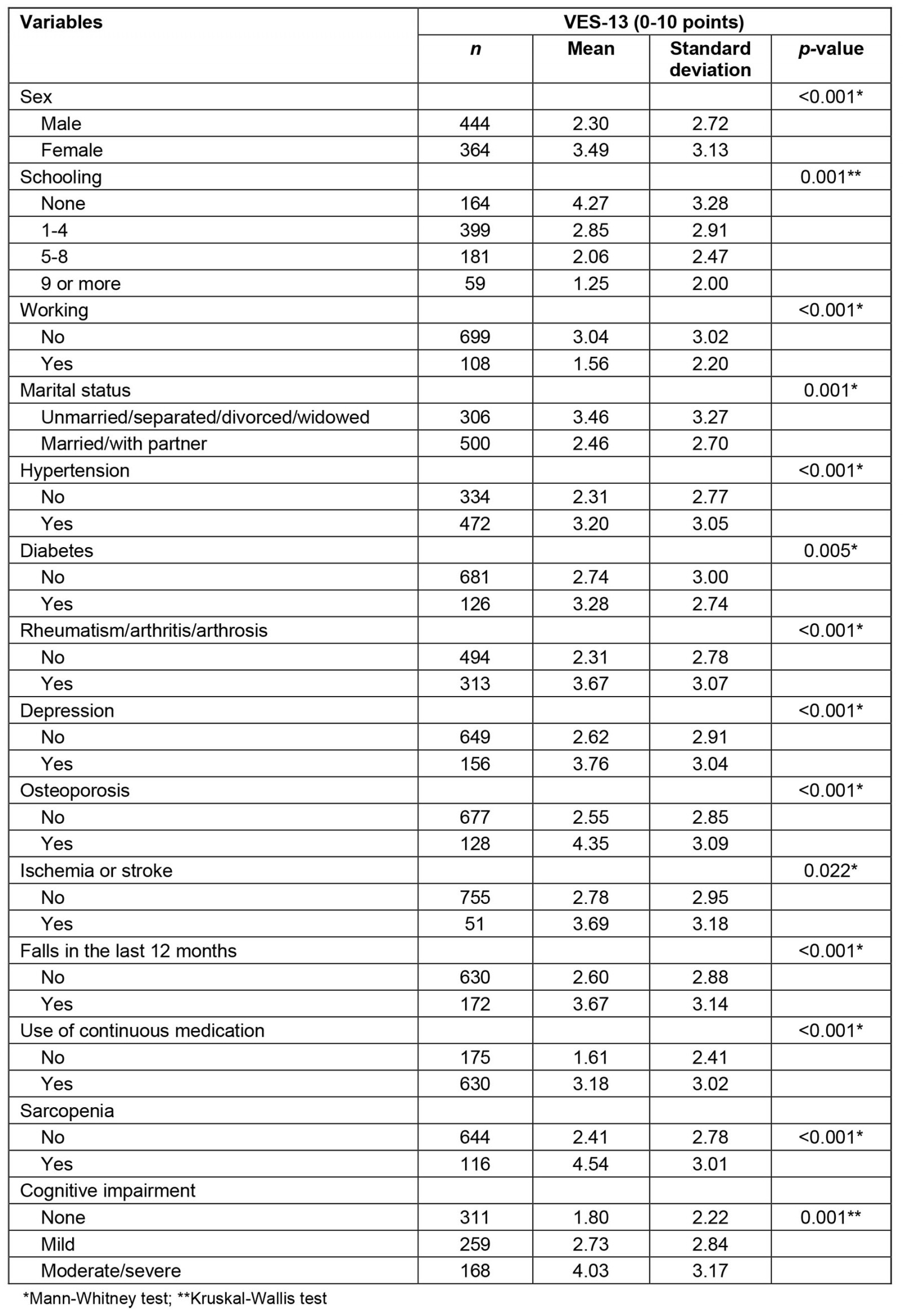
Out of 862 older adults followed, 808 fully answered the VES-13 and were included in the analysis. A majority of the participants were male (55%), with 1–4 years of schooling (49.7%), had monthly family income between 2.0 and 2.99 minimum wages, and were married or living with a partner (62%). Only 13.4% of the older adults worked. A total of 58.6% reported hypertension, 38.8% reported rheumatism/arthritis/arthrosis, 19.4% reported depression, 15.9% reported osteoporosis, 15.6% reported diabetes and 6.3% reported history of ischemia or stroke. A total of 21.4% of the older adults reported falls in the last year, 78.9% reported continuous medication use, 15.3% reported sarcopenia, and approximately 35% had mild cognitive impairment. The prevalence of vulnerability was 40.8% (95%CI 37.5-44.3) (Table 1). The mean VES-13 score was 2.84 points (standard deviation of ±2.97), and the median was 2.00 points. Details of the mean and standard deviation of the VES-13 according to the independent variables are presented in Supplementary Table S1.
Table 2 presents the descriptions of the VES-13 items. A total of 66.4% of the elderly people were aged between 60 and 74 years, and 59.0% self-rated their health as very good/good. Regarding physical function items, 69.0% reported no/little/some difficulty performing heavy housework such as scrubbing floors or washing windows, more than 70% reported no/little/some difficulty in stooping, crouching or kneeling; in lifting, or carrying objects as heavy as 10 pounds (4.5 kg); and in walking a quarter of a mile (400 m). A total of 87.0% had no/little/some difficulty reaching or extending arms above shoulder level, and 94.9% had no/little/some difficulty writing, or handling and grasping small objects. For the functionality items, 74.8% of the older adults had no difficulty shopping for personal items; 76.9% had no difficult in managing money, 89.2% responded that they had no difficulty in doing light housework, and more than 90% had no difficulty walking across the room and bathing or showering.
In the adjusted analysis, female sex (PR=1.45; 95%CI 1.23–1.71), not working (PR=1.70; 95%CI 1.17–2.45), living without a partner (PR=1.26; 95%CI 1.07–1.47), medical diagnosis of diabetes (PR=1.23; 95%CI 1.03–1.48), rheumatism/arthritis/arthrosis (PR=1.22; 95%CI 1.03–1.46), depression (PR=1.21; 95%CI 1.02–1.42), and osteoporosis (PR=1.38; 95%CI 1.15–1.66) were associated with vulnerability. An inverse association was observed between education and vulnerability (p<0.001). Sarcopenic older adults had a 67% greater probability of vulnerability than non-sarcopenic older adults (PR=1.67; 95%CI 1.38–2.02), and cognitive impairment was directly associated with vulnerability (PR=1.39; 95%CI 1.08–1.81 and PR=1.77; 95%CI 1.34–2.34; p<0.001) (Table 3).
Table 1: Descriptors of the sample of older adults residents in the rural area of the municipality of Rio Grande, Rio Grande do Sul, Brazil, 2018–2019 (n=808)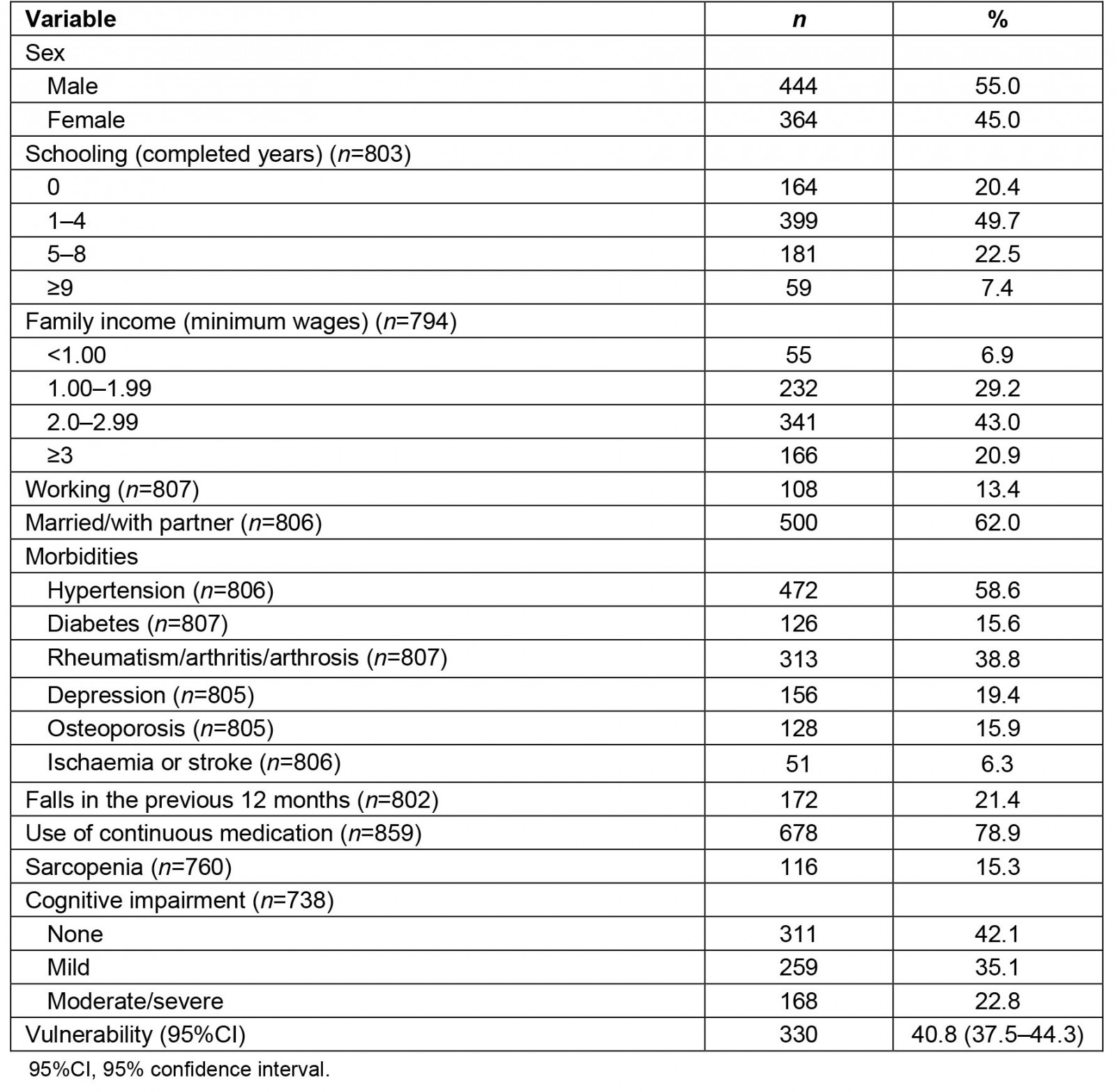
Table 2: Description of Vulnerable Elders Survey items. EpiRural Cohort Study (2018–2019), Rio Grande, Rio Grande do Sul, Brazil (n=808)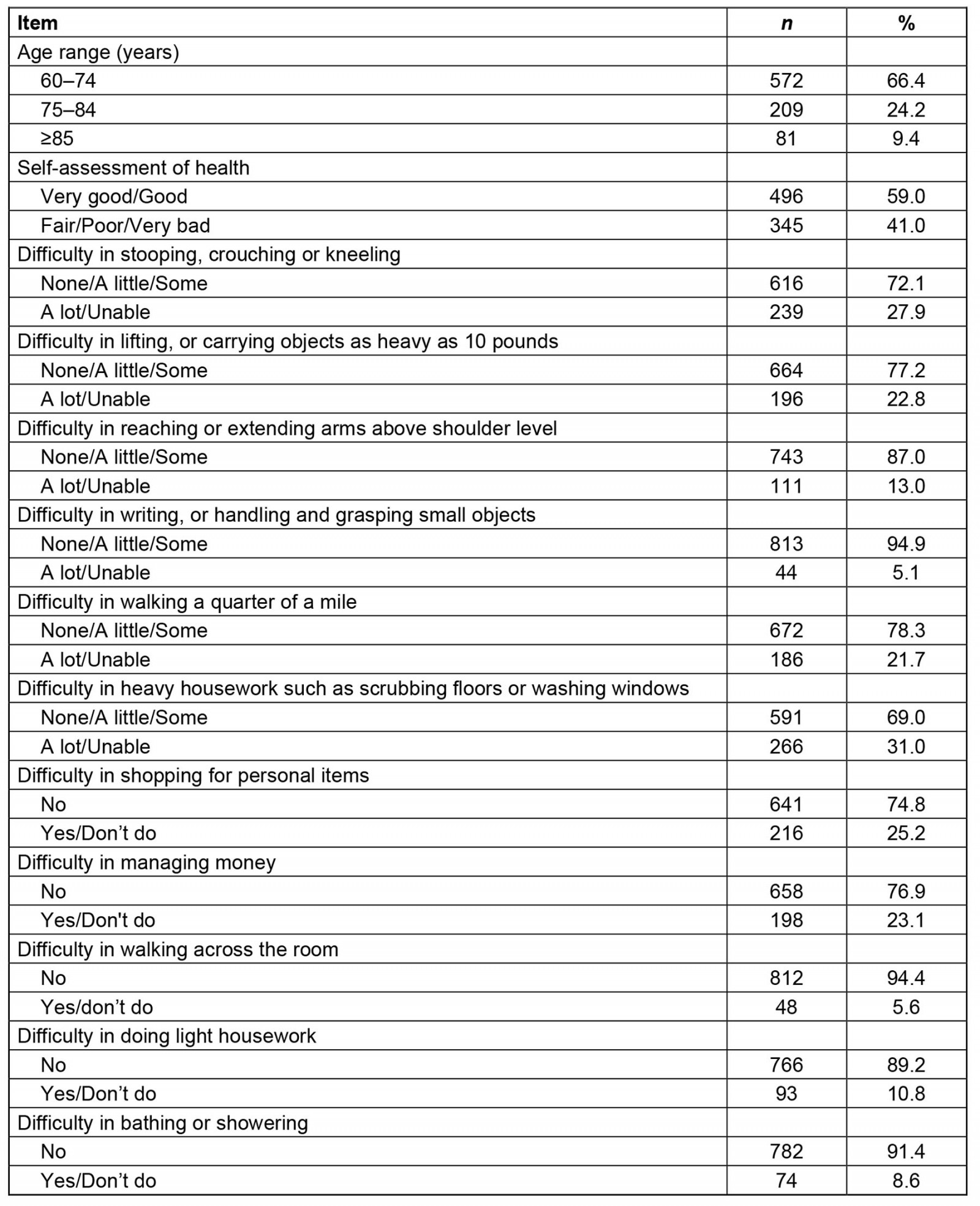
Table 3: Crude and adjusted analysis of associations between vulnerability and independent variables, Rio Grande, Rio Grande do Sul, Brazil, 2018–2019 (n=808)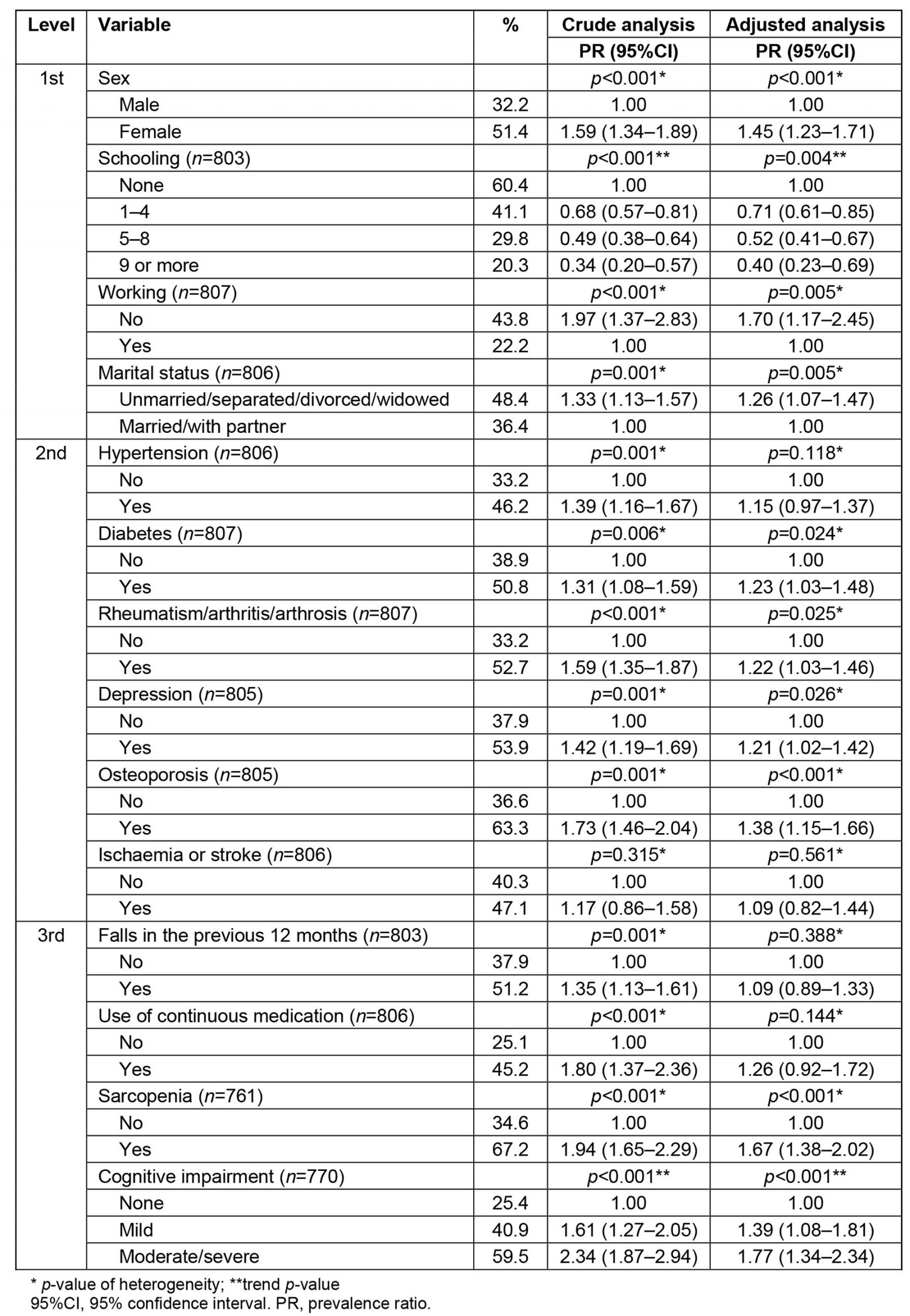
Discussion
This study evaluated the prevalence of and factors associated with vulnerability among rural community-dwelling older adults in Rio Grande, Brazil. Approximately 4 in 10 older adults were vulnerable. Female sex, living without a partner, not working, having a medical diagnosis of diabetes, rheumatism/arthritis/arthrosis, depression and osteoporosis, and having positive screening for sarcopenia and cognitive deficits were associated with a higher prevalence of vulnerability. Higher education was associated with a lower occurrence of the outcome.
Although health and lifestyle indicators may differ between older adults living in urban and rural areas26, the prevalence of vulnerability found in this study was similar to that reported in other studies. Studies carried out in different populations of urban older adults in different locations, such as the US27,28, Canada29, Ireland30,31, France32 and Taiwan6, reported prevalences ranging from 30% to 50%. In Brazil, studies have reported a similar prevalence of vulnerability, of approximately 50%12,33.
The association between sex and vulnerability identified in this survey was also observed in other studies. In Ireland, women were 50% more likely to be vulnerable10. In Brazil, two studies found a higher prevalence of vulnerability among women9,11. The feminization of aging is already well established, but in our study we did not find any difference in the mean age between men and women. A possible explanation for our findings is that, as they are more concerned with their health, women have more acute perceptions of the signs and symptoms of diseases34.
Our findings are similar to those reported in studies that also demonstrated an inverse relationship between education and income and vulnerability. Higher levels of education imply better living conditions and a greater ability to take care of one’s health35. In addition, higher income and education are related to greater access to basic infrastructure and health services36, favoring a more assisted aging process and, consequently, reducing the occurrence of vulnerability.
No other studies were found that assessed the association between work and vulnerability. A possible explanation for our findings is that, as functional capacity is one of the components of the VES-13 and as work activity presents challenges that encourage the maintenance of functionality among older adults37, it is likely that older adults who work are more independent. Another hypothesis for this finding is the fact that the work activity in the area is more manual. Thus, it is assumed that older adults living in rural areas may have less loss of functionality because they remain active for longer.
The absence of a partner increased the probability of vulnerability by 26%. This association can be explained by the greater attention and care received from a partner, which would lead a person to seek more health services and, thus, increase the chances of diagnosis of health problems and receiving treatment, thus protecting the individual against vulnerability34. Previous research has shown that the absence of a partner can lead to isolation and reduced concern with health, causing worse clinical outcomes among older adults38.
Previous studies carried out in Brazil have shown the association between diabetes, osteoporosis and rheumatism/arthritis/osteoarthritis and vulnerability9,12. It is possible that the greater vulnerability of older adults with these conditions is due to the greater risk of complications and limitations resulting from the processes of disease progression8.
The association between depression and vulnerability corroborates an Irish study in which older adults who reported depressive symptoms were 4.8 times more likely to be vulnerable10. Psychiatric disorders, including depression, are often attributed to the losses of physical and mental functions that accompany the aging process39.
The strong association between continued medication use and vulnerability was lost in the adjusted analysis. On the other hand, a study carried out in Lima, Peru, with the objective of evaluating the pharmacological quality of hospitalized older adults, found that the mean number of medications per patient was 2.940. Other studies have shown that the use of medication may be associated with a decline in functional status in older adults41.
Sarcopenia is characterized by the progressive and generalized loss of skeletal muscle mass and muscle function, which can lead to adverse outcomes such as reduced ability to perform daily activities42. Consequently, sarcopenia generates functional dependence, which is one of the items evaluated by the VES-13. However, it is important to emphasize that the association between sarcopenia and vulnerability was expected, as some items are common to both instruments. However, consistent with our findings, loss of muscle mass was associated with the presence of vulnerability in institutionalized older adults. In a study of elderly Polish subjects, participants with sarcopenia scored three or more points on the VES-1343.
Older adults with greater cognitive impairment become vulnerable as they stop performing the most complex activities of daily living44,45. The performance of activities of daily living depends on satisfactory cognitive ability, and a reduction in cognitive ability or a cognitive impairment will compromise the activities of daily living that are assessed as part of the VES-13 construct.
Our study has some limitations. First, the cross-sectional design does not allow the analysis of the temporality of events, making these susceptible to reverse causality in some associations, such as for the variables of work, depression and sarcopenia. Second, the VES-13 is a simple method for identifying community-dwelling vulnerable older adults, defined as those at increased risk for death or functional decline. Thus, there is no gold standard for vulnerability. However, its cultural adaptation was performed, and the VES-13 proved to be a reliable instrument with regard to the stability and internal consistency of its measurements46.
Despite these limitations, VES-13 is promoted in an official document from the Brazilian Ministry of Health, which favors its use, especially in primary care settings. Furthermore, as it is a simple tool that does not require technological resources and that can be applied by any primary care professional, its use is recommended and opportune. To the best of our knowledge, most previous studies have assessed vulnerability as measured by the VES-13 as an exposure, and ours is the first population-based study to assess vulnerability in a rural setting. We believe that our results can improve knowledge about the health characteristics of rural areas.
Conclusion
The results of this study showed a high prevalence of vulnerability among rural community-dwelling older adults, mainly among females and those who did not live with a partner, had less schooling, diabetes, rheumatism, osteoporosis, depression, sarcopenia and cognitive impairment. This study highlights the groups of older adults with characteristics associated with vulnerability who can be assessed in primary healthcare settings, identified in an active search, and monitored to prevent the development of worse outcomes.
References
Supplementary material is available on the live site https://www.rrh.org.au/journal/article/7714/#supplementary
You might also be interested in:
2021 - Not just simple cellulitis: a case report of polymicrobial Aeromonas infection from rural Queensland