Introduction
The health workforce is vital to a country’s ability to address and improve the health of its population1. The allied health (AH) workforce consists of a diverse range of professions, including audiology, dietetics, occupational therapy, pharmacy, radiography, physiotherapy, psychology, podiatry, speech pathology and social work2. Together with nursing and medicine, the AH workforce is essential in addressing society’s current and future health needs3. Being equipped to deal with the complex health issues that arise in rural and remote communities is a key challenge for both AH professionals and the health services that employ them. The latter face additional challenges in recruiting and retaining AH professionals4-6. Comprehensive strategies are needed to support the development and retention of a high-quality rural and remote AH workforce to meet the changing healthcare needs of these communities3,7.
AH professionals working in rural and remote areas require discipline-specific expertise and a diverse generalist skill set to manage the complexity and demand for health care in these areas7. Access to relevant continuing professional development (CPD) that sustains the development of generalist capabilities is a key strategy to support workforce development and the retention of AH professionals in rural and remote areas3,4,7. CPD is the ‘means by which members of health professions maintain, improve and broaden their knowledge, expertise and competence, and develop the personal and professional qualities required in their professional lives’8. A range of activities can be included as CPD, such as education programs, research projects, work-based case studies and audits, mentoring, conference attendance, seminars and workshops as well as self-directed learning activities. Engaging in CPD is essential to meet professional standards and maintain currency and capability in healthcare practice8. For AH professionals new to clinical practice, CPD is essential for successful transition to practice and their retention in the workforce9. Access to CPD in rural areas is often limited owing to a range of factors including geographic constraints, workload commitments, limited organisational support and availability of offerings that have impact, relevance and applicability to the rural context of practice7,10,11.
Online and distance education programs are a means for undertaking CPD and are purported to improve access. However, few evaluations have been published on the impact of online education programs for rural and remote AH professionals11-13. Existing evaluations of online education programs as CPD for AH professionals have focused narrowly on knowledge, and/or technology and program delivery and rarely on practice development or the impact on retention of AH professionals12. The purpose of this study was to evaluate the broader outcomes of an online education program specifically designed as CPD for rural and remote practice, and the impact on the professional development, healthcare services and recruitment and retention of AH professionals undertaking this program.
Methods
Design
A qualitative, exploratory descriptive study design was employed using semistructured interviews. This study formed the qualitative component of a larger convergent mixed-methods evaluation study that explored the reach, quality and impact of an online rural generalist education program (RGP) on AH professionals, which has been reported previously14. The RGP was the formal educational component embedded within the Allied Health Rural Generalist Pathway (AHRGP), a multipronged AH workforce, education and service development strategy aimed at enhancing the quality of AH services in rural and remote areas15. The evaluation included two stages: part A, a process evaluation using enrolment data and surveys, and part B, a mixed-method exploratory descriptive study design involving 6-monthly surveys and semistructured interviews. Qualitative findings reported in this current article were generated from the semistructured interviews in Part B and describe the impact of the RGP in response to the following evaluation questions.
- How did the program build the capability of rural generalist AH professionals?
- What contribution did the program have to rural healthcare services and consumer outcomes and why?
- How did the program influence perspectives on recruiting and building a rural AH workforce?
Online Rural Generalist Program
The RGP is an online education program comprising two levels: a foundational level (level one) for AH professionals new to clinical practice or rural and remote practice; and an advanced level (level 2) for AH professionals who have completed level 1 or who have at least 2 years’ experience in a rural and remote setting. Level 1 consists of 12 six-week modules (22 hours per module), which, when completed, are considered equivalent to two of the eight subjects (six modules per subject) in the advanced level and deemed suitable for recognition of prior learning. Level 2 involves eight subjects (130 hours per subject) leading to a Graduate Diploma in Rural Generalist Practice. As work-integrated learning was a core component of the RGP, participants in the evaluation were required to be concurrently employed in clinical practice in an AH position in a rural or remote area. From 2017 to 2019, the RGP was implemented and evaluated as the formal education component of the AHRGP15. This meant that AH professionals enrolled in the RGP and who participated in the evaluation were incumbents of fixed-term early-career training positions, most commonly 2-year supernumerary positions, with responsibility for a clinical workload and a service development project. These training positions included a formal professional development plan and a minimum of 4 hours of training and supervision per week, supported by a designated profession-specific supervisor15.
Sampling: study sites and participants
Purposive sampling was used to select the study sites and participants to ensure representation of the interests of both health sector stakeholders and AH professions16. Ten sites were selected: seven from Queensland and one site each from Western Australia, Northern Territory and New South Wales. All sites were in a rural or remote location as determined by the Australian Standard Geographic Classification, Accessibility/Remoteness Index of Australia Plus17. Across the 10 sites, eight AH professions were represented: dietetics, occupational therapy, pharmacy, physiotherapy, podiatry, radiography, social work and speech pathology. Study participants included AH professionals enrolled in the RGP and their designated work-based supervisors and senior managers who provided operational management from each of the 10 sites. All RGP participants were employed on a full-time basis and enrolled in level 1 and/or level 2 of the RGP administered by James Cook University.
Data collection and analysis
To promote consistency and retain a neutral perspective, data collection and analysis were conducted by one researcher, who was independent of the RGP’s development and implementation. Data were generated from individual semistructured interviews with consenting participants recruited by email and telephone. Interview topics, based on the evaluation questions, were developed to explore the experiences of RGP participants, and their managers and supervisors of the program, and their perception of the impact of the RGP on themselves, the healthcare service and the broader community. Using a semistructured approach allowed flexibility to adapt interview questions to specific participant groups and probe for further depth and detail in the topics being explored.
The interview topics were:
- allied health participants’ experience of being part of the rural generalist program
- improvement in rural generalist knowledge and skills
- improvements in the effectiveness, efficiency and accessibility of rural and remote services
- barriers, enablers in implementing rural generalist service strategies
- rural generalist program outcomes: successes and challenges
- impact/influence on allied health participants’ intention to stay.
Interviews were conducted by video or telephone during the RGP participants’ last 12 months of completion of the program. With participant consent, interviews were audio recorded and transcribed verbatim. Participants were assigned a unique identifier to ensure anonymity of participants and sites, and to provide an audit trail. Each study participant was allocated a specific identifier to distinguish their role within the study. Postgraduate AH professional enrolled in the RGP were allocated a ‘P’, with supervisors allocated an ‘S’ and managers allocated an ‘M’. This provided clarity in using participant quotes when reporting results, while still maintaining study participants’ confidentially and anonymity. NVivo v12 (Lumivero; https://lumivero.com) data management software supported data analysis.
Interview data were thematically analysed site by site, then across sites using a systematic six-phase approach18. Initially a set of provisional codes were applied to the interview data, based on the evaluation questions. In the first two phases of analysis, patterns, codes and unique ideas relevant to the questions were identified in the transcripts. After initial coding of data, a member of the evaluation team conducted intercoder agreement. Codes were then compared, contrasted and collapsed into secondary, more advanced codes in phases 3 and 4. This iterative process continued through the final two phases where major themes and subthemes were developed18. The final step of analysing data across sites, using the same approach, maintained consistency in the analysis and strengthened the reliability of findings18,19. This systematic approach aimed to engender rigor in managing and theming the large volume of data generated, while allowing the flexibility to deepen the analysis within each coding segment18,19.
Ethics approval
Ethics approvals were granted by James Cook University Human Research Ethics Committee (HREC) H7025; the Top End Health Service and Menzies HREC for the Northern Territory site HREC 2017-3008 and the Townsville Hospital and Health Service HREC/17/QTHS/200 for sites in Western Australia, New South Wales and Queensland.
Results
A total of 50 study participants were interviewed across the 10 sites between January to December 2019. This included 17 participants enrolled in level 1 and six enrolled in level 2 of the RGP, and 27 participants who were their managers and/or supervisors (Table 1). Interviews were conducted by telephone (n=39) and videoconference (n=11) and ranged between 30 and 75 minutes in duration.
Three key themes related to the perceived impacts of the RGP were identified:
1. Building capability as rural generalist AH professionals
2. Recruiting and building a rural workforce
3. Enhancing healthcare services and consumer outcomes
Table 1: Characteristics of interview participants: RGP participants, managers and/or supervisors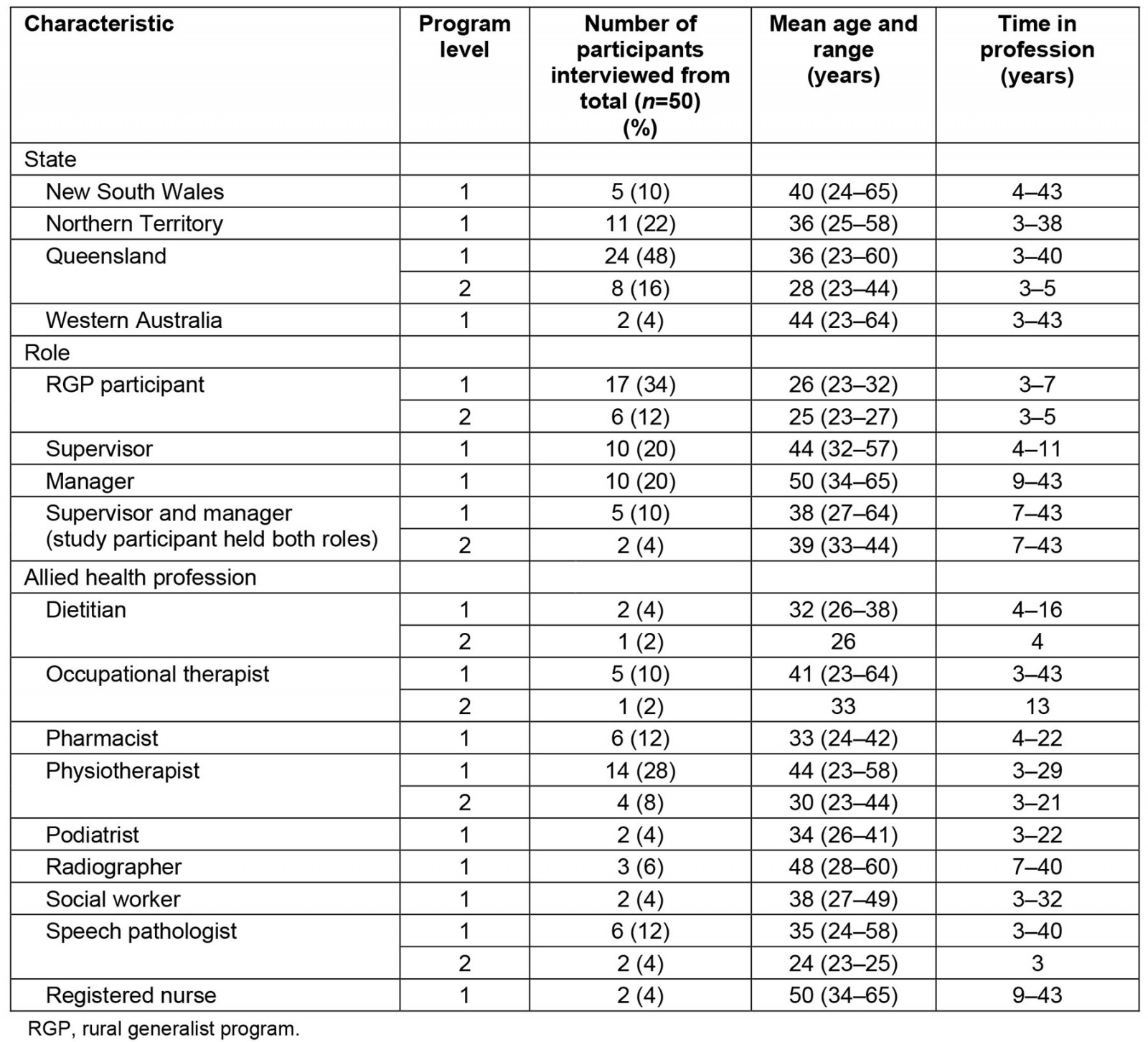
Theme 1. Building capability as rural generalist allied health professionals
The RGP provided AH professionals with an opportunity for supported professional development as rural generalist AH professionals. The majority of RGP participants and their managers and supervisors expressed how the program helped facilitate learning and development in all areas of healthcare practice, with professional development observed beyond clinical skills.
I’ve found [it] really useful … all the generalist ways of practice. Like telehealth and skill sharing and partnerships … (11PB)
[The health professional has]... grown … into a very skilled passionate calm clinician who’s done a really good job up here and made an impact on people’s lives. (29SE)
All study participants described gains in relevant, generalist knowledge. Study participants explained that undertaking project management, quality improvement and health service delivery education modules, concurrently with the responsibility of implementing a service project, provided for significant professional development. RGP participants found that applying the theory and practical aspects of the modules to a service project enhanced their understanding of the healthcare system, service development, governance and healthcare teams. Implementing a project meant RGP participants needed to work within organisational processes and teams to effect change. As a result, RGP participants deepened their knowledge and understanding of how the health system and organisation functioned. As one manager described, this increased AH professionals’ ability to lead and manage service projects, understand their role within a team and their ability to work more effectively and efficiently in the healthcare service.
… so the training really does help them get more perspective on … how they can be as efficient and as effective in their role as they potentially could be. (61MSD)
Simultaneously studying while working presented RGP participants with an opportunity to develop time-management and decision-making skills. Managing study commitments alongside clinical caseloads and a health service project prompted them to be organised and decisive to meet competing timelines. At times, when a staff member had left or was on leave, RGP participants were the only AH professional available in their health service. This increased the need for them to manage caseloads and work independently, think critically, prioritise and make decisions with distance supervision.
You have to deal with a lot of different things concurrently, even just having the mental capacity to like step back and say okay I can’t do everything at once. This is what I need to prioritise now, and that kind of thing was really good. (24PC)
Managers, RGP participants and their supervisors noted that a key outcome from the program was RGP participants’ increased capability for autonomous, independent practice. Managers and supervisors also noted a distinct increase in RGP participants’ confidence in taking ownership of their role to independently manage not only complex clinical caseloads but clinics and services.
… they’ve just – they’ve gone from somebody very junior who’s been in a large team to a sole practitioner who’s able to manage service across a number of sites. (33MG)
Improving communication and confidence was reported to enhance RGP participants’ interprofessional practice and teamwork. Managers and supervisors observed how well RGP participants interacted with others across the organisation when providing consumer care. RGP participants described feeling more confident to have professional conversations with senior staff, team members and consumers.
… So, it [the RGP] has majorly increased my confidence... I would have been very unconfident to speak to someone like a head of department about persistent pain at the [X hospital] previously and try and convince them to do something that I wanted them to do. And now I’m a lot more sure of myself. (03PD)
Conversely, a small number of RGP participants indicated that some components of the RGP had limited impact on their learning and development. This mainly related to the non-clinical aspects of healthcare practice. Some RGP participants commented that completing study modules and project work took them away from clinical practice, which they found frustrating and demotivating. Others found specific program modules too basic for their learning needs; they were seeking more challenging or profession-specific content that would extend their learning and development, and clinical practice skills.
I found that a lot of the general sort of non-clinical subjects were a bit irrelevant and not very useful either … it just didn’t seem very relevant or a good use of my time, considering I had so many clinical demands. (63PI)
Theme 2. Recruiting and building a rural workforce
Study participants expressed that having the RGP embedded within the broader AHRGP provided the essential framework needed to recruit early-career professionals and equip them with the foundational capabilities and confidence for generalist practice in rural areas. As illustrated by the following RGP participant’s comment, this influenced participants’ perspectives about the factors that would contribute to decisions to work in and remain working in these contexts.
I think the skills that you do learn would build up confidence and competence in being able to do work in a remote location a lot better than people that just go out and have no idea what they’re doing. (11PB)
The findings indicate that the RGP was a valuable component of the AHRGP pathway for recruitment and retention. When asked about the recruitment and retention of AH professionals, the majority of study participants described the RGP as a positive incentive for both. As one manager emphasised:
We’ve now got people who want to stay [in rural and remote areas], and you know outside of these contracts – it has to be a positive. (33MG)
Managers and supervisors spoke of the challenges experienced with recruiting staff to work in their organisations. They explained that because the RGP was embedded within the broader AHRGP initiative, participation in the RGP was supported with health service funding and formal supervision structures and that these elements augmented recruitment to the respective health service sites. Lack of ongoing funding and structures to support AH positions were acknowledged as potential limitations of the RGP that would affect recruitment and long-term retention.
… It’s more been local [positioned] for two years which was facilitated by the course – the funding for my position coming for this [program] has allowed me to be out here and I love rural practice now. (73PB)
Where the AHRGP training positions were supernumerary positions, having an additional capable staff member provided service coverage to accommodate staff leave and professional development opportunities. Being able to fill long-term vacancies cultivated service stability and some organisations’ abilities to progress activities that had previously been on hold due to staffing levels. Managers, supervisors and RGP participants reported that these changes enhanced staff morale and job satisfaction.
… prior to all this happening we had such a high turnover … that could never get any, anything running and, you know, and keep it running because there was always, people would stay for a year or two and then, you know, two years was the kind of max... (54SD)
Managers and supervisors suggested the RGP has the potential to support succession planning that would benefit rural healthcare. The organisational, team and clinical knowledge gained from participating in the RGP while working in a clinical role established foundations to move more seamlessly into more senior roles.
Like if we’re looking to fast track people to more senior level positions, then teaching them about quality improvement and, you know, that the way that the team runs and the strategic levels of how the systems within the health service work and that kind of picture, I think there’s a lot of value in that. (02MSB)
The RGP participants reported developing a greater appreciation and understanding of AH practice in rural and remote contexts. The variety and challenge of generalist practice, and the diverse communities that they worked within, influenced RGP participants’ passion to continue working in rural and remote contexts, now and/or in the future. This passion for rural and remote practice was also observed by supervisors and managers.
… [they have] become very passionate about rural and remote health and I think that passion is sort of infectious with the rest of the team and sort of talking about the work she’s been doing and everyone getting a lot more interested and those kinds of things which, um, yeah, I think does have an impact on our retention rate certainly our recruitment. (211SC)
The RGP, when embedded within the AHRGP, was considered a valuable mechanism for supporting and building a rural workforce. However, some managers and supervisors suggested that the rural context and workload may not be appropriate for all young clinicians. Concerns were raised about the isolation and limited infrastructure associated with rural and remote locations for those in the early stages of their career.
In some ways it’s, it’s almost too early for the, for their early careers because they’re kind of consolidating their skills, they’re almost so new that it’s, um, it’s a lot for them to take on even though they’ve managed. (54SD)
Some RGP participants echoed this finding. Although they perceived the RGP was an incentive, they felt it was too early in their career and life to choose to work in rural health.
I think that in terms of what another rural job directly after this would do for my career, I think it would be a negative choice because it would then limit me pretty much exclusively to rural practice, to go out and do another two or three years in, in a rural town. (73PB)
Theme 3. Enhancing healthcare services and consumer outcomes
As RGP participants’ capability and confidence to independently manage their caseloads increased, service efficiency was enhanced because they did not have to rely as heavily on others.
I can go down to the ward and do all of that myself, I’m much more confident with that now … so that service is better because I don’t have to rely on going back to the supervisor. (52PD)
As service efficiency increased, more outreach services could be accommodated. Managers and supervisors reported increased consumer access, decreased waiting times, and increased continuity of care with more effective discharge, follow-up at home and ongoing support.
… it’s been earlier discharge because there’s a physio available on a daily basis rather than, like, normally I would be on outreach for a few days, three, three weeks out of four. So that slows things down and slows down discharge … we’ve been able to offer greater outreach. (54SD)
RGP participants, managers and supervisors alike, reported improvements in service delivery approaches as a result of RGP participants sharing information and ideas generated though the RGP. For example, RGP participants developed useful organisational and community relationships that were reported to enhanced service delivery and they enjoyed sharing information with supervisors and managers receptive to new initiatives.
My team and like, all the colleagues that I work with … love it when I come across stuff that I’m like, ‘Oh, this is probably really helpful, let me just send out an email for anyone that wants to read it’. (11PB)
The RGP was designed to align with service improvement projects. RGP participants found that program modules supported them to carry out these projects, and that they were able to simultaneously learn about and work more effectively within their workplace and community contexts. Collectively, the RGP modules fostered RGP participants’ ability to understand service delivery, identify service gaps, and implement projects that contributed to service enhancements.
… it’s made service delivery better... clients previously did not have that service at all, and now, through – indirectly through my program, they have that service … (03PD)
Service improvement projects resulted in the introduction of additional healthcare services and quality improvement activities. Projects across study sites varied and included new outpatient and outreach services, education programs and streamlined discharge planning processes. Service expansion added value in terms of what healthcare organisations could offer local communities. Improvement activities were reported to save time and cost through improved referral systems, streamlined administrative processes and onsite service provision. The capacity of health services increased in terms of the types of health care offered to consumers, and communities previously underserviced.
We had increased the number of paediatric clients we were seeing, we decreased admin time recalling patients and we’d decreased the number of failed to attend. (57PA)
Projects conducted by RGP participants that led to new services or processes such as telehealth, which linked healthcare services from major to remote centres, were acknowledged as beneficial to both consumers and to the host service. Reductions in staff travel time provided more timely and efficient services for consumers. In some instances, this changed clinical outcomes and expedited the transition of consumers back to communities. Having services offered in a local area supported consumer engagement, support and welfare.
You’ve got kind of increased accessibility to the service obviously for the patients and for the clinicians, so the local GPs and the doctors within the hospitals, got a more efficient service … so you don’t have to transport patients externally … the waiting list is, reduced. (71PF)
Discussion
The qualitative findings of the RGP evaluation presented in this article suggest that engaging in the RGP contributed to the professional development of AH professionals and had positive outcomes for rural and remote healthcare organisations and consumers. The development of the RGP was underpinned by sound pedagogy that aimed to scaffold RGP participants’ professional development within a work-integrated approach to learning. Findings indicate that this approach potentiated the development of capabilities AH professionals require for rural and remote practice.
The design of the RGP utilised the principles of adult learning20 to draw on RGP participants’ experience and provide opportunities for self-directed, authentic application of new knowledge within participants’ own workplaces. Teaching and learning strategies within the RGP were developed using experiential and constructivist approaches to learning to allow RGP participants to incorporate new knowledge and skills through active engagement in relevant, real-life activities21-23. Embedding the RGP within the AHRGP increased the opportunity for structured experiential learning that was authentic and meaningful. The combined effect of aligning the RGP program, clinical practice experiences and engagement in a service improvement project, cultivated deep, meaningful learning that led to the significant professional development of self-directed, independent AH professionals. Findings revealed benefits for early-career AH professionals, including increased confidence and capability for independent practice, improved knowledge about generalist practice and enhanced clinical practice. While not all RGP participants experienced all of these outcomes, the majority found the experience beneficial to their professional development and career.
These findings add to the substantial evidence supporting the efficacy of immersive placements and work-integrated learning practices for professional development and socialisation24. Such experiences have a positive impact on work readiness and employability25. Work-integrated learning is considered an effective workforce development strategy for preparing AH professionals for the workforce and, in this instance, influenced RGP participants’ desire to work in rural locations26. The duration and type of work-integrated learning experience, together with alignment of curriculum and healthcare experience can affect outcomes25. Our findings suggest that work-integrated learning, or experiential learning, needs to be intentionally integrated with structured, formalised education and support to enhance the quality of outcomes for the learner.
The suite of support focused on the AH professional’s individual needs and contexts may be a reason for the success of the RGP. Somewhat similar findings have been reflected in other studies3,4,7, including a systematic review27 that examined the experiences of early-career AH professionals and doctors in rural and remote environments. Both AH professionals and doctors reported increased skills and confidence from the support they received, particularly from supervisors and managers27. Importantly, when support was perceived to be inadequate ‘both groups of participants reported challenges to their confidence, feeling overwhelmed and lacking satisfaction in their roles’27. Early-career AH professionals and doctors in this review also reported that having access to professional development opportunities to support skill development, career advancement and maintain competence necessary to meet registration requirements was a positive factor for working in rural and remote contexts27. This builds on earlier research that found that access to support and CPD was seen as a priority and an essential factor for AH professionals in rural practice7,10,11. Reasons for this included consolidation of clinical skills and development of more advanced knowledge and skills. Perhaps not surprisingly, inadequate access to CPD and/or limited opportunity for career advancement were seen as deterrents to AH professionals remaining in the rural health workforce.
The RGP was described as an incentive for recruitment that could influence short-term retention, highlighting its potential as a strategy for building a rural and remote AH workforce. AH professionals’ engagement with the RGP may have enhanced their integration and assimilation within the rural and remote context and thus their sense of belonging and desire to remain in their roles. A sense of belonging and worth, and the ability to make a difference and contribute to community are elements that lead to learning and promote professional and personal socialisation24,25,27. In rural and remote locations, these factors are known to increase job satisfaction and retention3. Evidence also suggests that the opportunity to work collaboratively with health services on projects with clear goals and responsibilities, and to communicate outcomes with a range of audiences, supports AH professionals’ development25,28. Moreover, experiences that facilitate connectedness in the workplace, coupled with education that promotes independence and autonomy for practice, are considered important factors in AH professionals’ preparation for their professional role29 and early-career transition experiences27.
Challenges associated with health professionals’ transition to independent practice have been highlighted in previous studies9,27,30. For early-career AH professionals working in rural contexts, the challenges of this transition can be compounded9. Isolation from family and friends coupled with working and living in an unfamiliar environment can be daunting. AH professionals new to rural practice without mechanisms to assist their integration, sense of belonging and transition are likely to leave31. Our findings indicated that connecting with other AH professionals undertaking the program provided a supportive network for sharing experiences. It was also clear that there were reciprocal benefits of having dedicated supervisors to partner new employees during their entry to rural practice. This included interprofessional learning and development of supervision skills, which are factors known to influence retention of rural AH professionals32,33.
To improve recruitment and retention of AH professional in rural areas, our findings reinforce that structured educational strategies need to be embedded within broader support strategies that cultivate a sense of belonging and professional socialisation. In addition, future workforce development strategies need to engage AH professionals in organisational activities to support community and workplace socialisation. As an online program, most RGP participants engaged with and enjoyed the content and delivery. Engaging in education is known to promote safe practice and improve consumer outcomes, help reduce professional isolation, and enhance recruitment and retention12,13. Careful consideration of the design, delivery and content of online programs, to ensure sustained engagement, is essential if these advantages are to be realised12. Findings from this study suggest that designing online programs with learning activities that promote both online and offline interaction in the workplace are important inclusions that offer timely support and have authentic, practical relevance and application in the workplace.
Relevance for practice
Health professionals in rural and remote locations face challenges accessing ongoing professional development, most notably due to geographic location and staff shortages. Attending CPD programs is often limited by costs and finding additional staff to cover workloads12. Online education is seen as a potential solution and, with improvements in technology, is now growing in popularity. During 2020 and 2021, the COVID-19 pandemic propelled education providers to move from face-to-face and blended modes to online delivery, which highlights potential opportunities for the delivery of professional development in rural and remote practice. Creating educational approaches that can meet different learning needs can help address differences in learning modes and technological inequities that can often challenge the delivery of CPD and health care in rural areas34. Such approaches could enhance the access and availability of CPD for rural AH professionals and, subsequently, workforce development.
Limitations
This study may be limited by study participants’ ability to discern the distinct impact of the RGP because of how it articulated within the AHRGP. Future evaluation of workforce development programs may consider realistic approaches that investigate for whom and under what circumstances these types of programs work35. Further insight into the experiences of participants within each study site will allow deeper understanding of location-specific experiences.
Conclusion
The value of educational programs that align with AH professionals’ needs, and provide authentic experiences for sustained learning and development, are evident from this evaluation of the RGP. Postgraduate education can be provided online in rural areas to promote professional development and is conducive to recruitment when coupled with broader workforce strategies, including access to supportive experts and service development initiatives. This approach may inform governments and health organisations of the conditions in which workforce development, aimed at meeting consumer needs, will be most successful.
Acknowledgements
The study was funded by the Allied Health Professions Office of Queensland, Department of Health, Queensland Government. The authors would like to thank Professor Jenny Sim, Associate Professor Natalie Ciccone, Dr Desley Harvey and Ilsa Nielsen for their contribution to the evaluation project; Jennifer Carr, Katrina Bird and Leisyle Blanco for their assistance with data collection; and Dr Karen Cheer for her assistance with data analysis. The authors would also like to thank those who participated in the study: managers, supervisors and RGP participants from throughout Australia.
Publication disclosure
This article reports on the qualitative findings from a larger convergent mixed-methods evaluation study that has been previously published in part elsewhere14.
Conflict of interest
Four of the six authors are employees of the two universities offering the RGP.
References
You might also be interested in:
2014 - Rural emergency medical technician pre-hospital electrocardiogram transmission
2008 - Rural nurse job satisfaction
2007 - 'Perimeteritis' and rural health in Manitoba, Canada: perspectives from rural healthcare managers




