Introduction
Background
Randomised controlled trials (hereby referred to as ‘trials’) are the gold standard method for evaluating health and care interventions including medicinal products, and services1 Recruiting participants to trials can be extremely difficult2, and can make or break the success of a trial. Recruiting fewer participants than is needed to answer the research question can result in an underpowered trial that fuels the significant problem of research waste2.
In recent years the focus of the trials community has shifted from simply recruiting participants to recruiting the right participants to ensure that trials are designed explicitly for the patients that stand to benefit most from their results.
The INCLUDE Project3, funded and led by the UK’s National Institute for Health and Care Research, identified a variety of groups that are routinely underserved by health research; characterised by lower inclusion in research, high healthcare burden that is not matched by research volume, poorer health outcomes and lower engagement with healthcare interventions compared to other groups4. These underserved groups varied by demographic factors, social and economic factors, health status and disease-specific factors4.
The experiences of people living in rural and remote areas are complex and multifaceted, and although they are named explicitly in INCLUDE’s list of groups by social and economic factors, their experiences intersect with those of several other underserved groups, such as people at age extremes, those in full-time employment and people experiencing digital exclusion/disadvantage4.
People living rurally face health inequities fuelled by social exclusion, access to and awareness of health services, and poor transport links5. In comparison to people living in urban areas, mortality rates for asthma are higher6; cancer is diagnosed at a later stage7. leading to increased mortality8; intervention rates for heart disease are lower9; and patients are admitted to hospital less frequently10. The mean age of rural people is rising rapidly11, fuelling the complex health needs of this population12. In addition, the rationing of healthcare resources may have impacted rural patients disproportionately13,14. The nature of rural living produces a complex set of challenges that lead to increased socioeconomic disadvantage in older populations15; those experiencing socioeconomic disadvantage are also a group underserved by health research16.
To ensure that health and care interventions are acceptable, accessible and applicable to people living rurally, it is important that researchers are able to effectively recruit rural participants into their trials. Recent systematic reviews have sought to quantify the effects of recruitment interventions with the aim of giving trial teams an evidence base to work from17,18 when planning their recruitment strategies, but as yet none of this work has focused solely on people living rurally.
This systematic review will quantify the effects of randomised evaluations of strategies to recruit rural participants to trials. Our findings will contribute to the evidence base to support trial teams to recruit a participant population that represents society as a whole, informing future research and playing a part to alleviate health inequalities between rural and urban populations.
Objectives
In this review, we will explore trial recruitment methods being used to target participants living rurally. Our objective is to answer the question ‘Does the use of these trial recruitment methods increase the proportion of rural participants recruited to randomised controlled trials?’ We will include randomised evaluations of recruitment methods with at least one comparator.
Criteria for considering studies for this review
Types of studies: These studies include a comparison of two or more interventions to improve recruitment of people living rurally to randomised controlled trials. These comparisons must be randomised: they should randomly allocate participants to intervention or comparison groups.
The context of the included host trials is likely to be health care, and we will include trials set across all stages of health care, including collaborative care taking place within more than one healthcare context (primary, secondary, tertiary, end-of-life care, within the community). Strategies evaluated within other trial contexts (eg public health interventions in schools) will also be included in this review.
We will not include studies where potential participants are asked whether they would take part in a hypothetical trial.
Types of participants: Participants will be individuals living rurally who are involved in a trial. Due to the diverse nature of rurality and the way that rurality is defined in various global contexts, we will not use a fixed definition of rurality. A location that we define as rural in our own context (our study team all reside in Scotland, UK), will be very different to a location defined as local in Tanzania, Canada or India, for example. The UK’s Office for National Statistics Rural Urban Classification defines areas as rural using population19; settlements with a resident population of more than 10 000 are rural in the UK context. In contrast, the Indian government defines rurality using a combination of population, population density and employment20; defining a rural area as one with a population of less than 5000, a population density of less than 400 per square kilometre, and where more than 25% of the male working population is engaged in agricultural pursuits.
We will rely on study authors, trusting that they know the context that they are working within and are able to work within an appropriate definition of ‘rural’.
We anticipate a fairly low number of included studies due to the targeted nature of this review. Therefore, we have decided to include studies where ‘rural’ is explicitly referred to, even if the study authors have not included details of the definition they are working with.
Types of interventions: Any intervention, strategy or approach aimed at improving or supporting recruitment of participants nested within randomised controlled trials performed for purposes unrelated to recruitment may be considered. Included interventions could be aimed at any trial stakeholder group (eg research ethics committees, trial recruitment staff or trial participants). Examples of such interventions include, but are not limited to, the use of different methods to remind participant of appointments, use of different types (including both method of information delivery and content) of participant information leaflets, changes to the staff member making the approach to potential participants, where and/or when the initial consent process takes places, financial incentives, specific transport connections to the study site and use of different data collection methods.
Included studies will include at least one intervention and one comparator. The comparator may feasibly be ‘nothing’, meaning the intervention is compared against taking no special measures to improve recruitment.
Types of outcome measures: Our primary measure will be the proportion of individuals recruited into a randomised controlled trial. Where study authors report the proportion of individuals recruited as well as the proportion of individuals randomised, we will extract and report both of these data and consider potential differences between them.
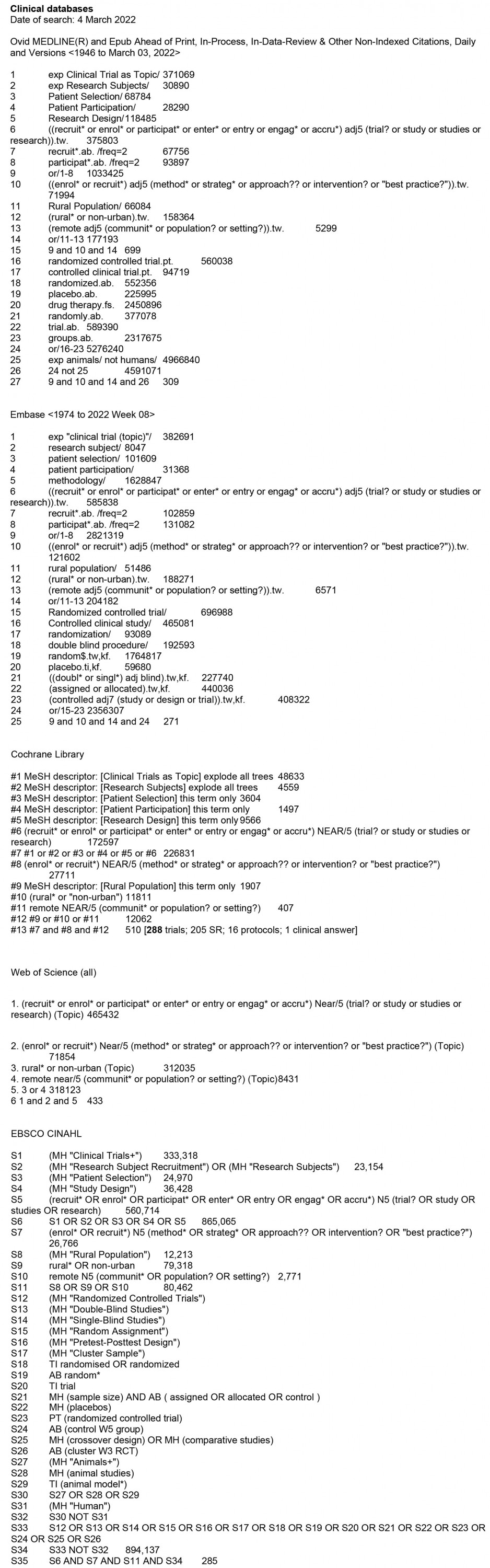
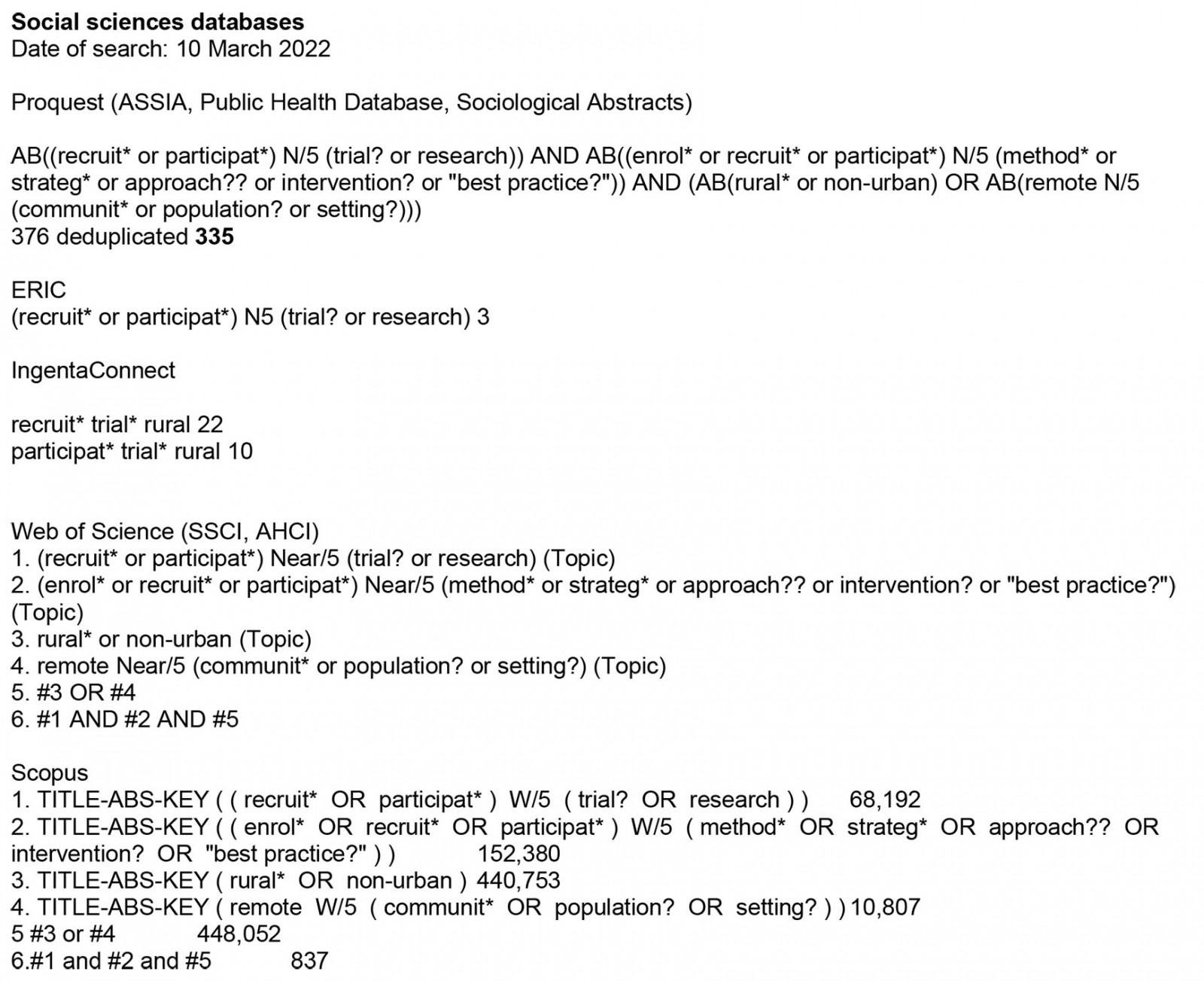
Search methods for identification of studies: We searched clinical databases (Ovid MEDLINE, Embase, Cochrane Library, Web of Science All, EBSCO CINAHL) and social sciences databases (Proquest, ERIC, IngentaConnect, Web of Science SSCI and AHCI, Scopus). All searches were conducted on the same day: 4 March 2022. We applied no restrictions to language or publication date. Full search strings used for each database are available in Appendix I.
Methods
Data management: Search results from all included databases will be merged into the reference management software EndNote, and duplicate records removed using the EndNote de-duplication tool. We will then use a master spreadsheet to record all study inclusion and exclusion decisions. This spreadsheet will enable us to create a Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) flow diagram21 after the screening process is complete.
Extracted data will be collected on specially designed forms (see ‘Data extraction’ section) and data entered into the Cochrane RevMan tool (Cochrane; http://tech.cochrane.org/revman) when data are complete enough to make this possible.
Identifying studies: Two reviewers will independently screen the titles and abstracts of all search records. Full texts will be sought for studies that look as if they meet the inclusion criteria, and two reviewers will independently screen them to determine if they meet our inclusion criteria.
Any disagreements between reviewers will in the first instance be discussed to explore why different decisions have been made, and if this does not resolve the issue then a third reviewer will be called in to moderate and make a final decision on inclusion.
Risk of bias of individual studies: Two reviewers will independently assess the risk of bias in all included studies using the Cochrane risk of bias tool22. As recommended, we will consider:
- random sequence generation (selection bias)
- allocation concealment (selection bias)
- blinding of participants and personnel (performance bias)
- blinding of outcome assessment (detection bias)
- incomplete outcome data (attrition bias)
- selective reporting (reporting bias)
- other sources of bias.
Reviewers will resolve any disagreements in risk of bias assessment through discussion; where this is not possible a third reviewer will be brought in to adjudicate. The level of risk of bias within each of these domains will be presented clearly within the final review.
Data extraction: Two authors will independently extract data from all included studies using specifically designed data extraction forms. Disparities in data extraction will be resolved during discussion and, if necessary, the involvement of a third reviewer. Data will be extracted on three categories – intervention, participant and setting – using the Template for Intervention Description and Replication (TIDieR) checklist as a guide23.
- Intervention: any rationale or theory to the intervention, details of the materials and procedures used to deliver it, who provided the intervention and how, and, if assessed, whether the intervention or comparison changed throughout.
- Participant: eligibility criteria for the host trial, characteristics of the participants recruited and if these characteristics differed between intervention and comparison groups.
- Setting: the country and context in which the host trial was conducted, and details of where the intervention was delivered.
Results
Data analysis
Studies will be analysed according to the type of recruitment intervention being evaluated (eg method of communication such as use of SMS reminders, changes to the delivery of participant information; or content of communication such as language variations, use of video or illustrations to portray participant information). Studies will be further categorised should we find the same intervention applied to more than one trial setting, intervention type or participant group.
The latest update to the Cochrane review ‘Strategies to improve recruitment to randomised trials’, published in 2018, included 68 trials evaluating 72 comparisons17. With this in mind, we do not anticipate a significant volume of studies as we are focusing specifically on recruitment of rural participants. We will present results as risk difference with the associated 95% confidence intervals. As recommended by the Cochrane Handbook, we will calculate prediction intervals when more than 10 studies are included within any one category and there is no clear funnel plot asymmetry24.
Where there are insufficient data to conduct statistical analyses, we will present a descriptive analysis of the interventions being evaluated.
Dealing with missing data: We will attempt to contact the corresponding authors of studies where details about the participant population, the intervention and/or outcome data are missing. Data will be analysed as reported, and loss to follow-up will be reported and assessed as a potential source of bias in our risk of bias assessment.
Assessment of heterogeneity: Where data allow, heterogeneity between the studies will be assessed using the χ2 test for heterogeneity, and the degree of heterogeneity will be quantified using the I2 statistic. As we have noted previously, we do not anticipate a significant volume of included studies; we will therefore include 95% confidence intervals to express the uncertainty associated with I2 estimates25.
Where substantial heterogeneity is detected (I2 ≥ 50%), possible explanations will be explored between reviewers and the data summarised using a random-effects model if appropriate.
Assessment of reporting bias: We will investigate reporting (publication) bias for our primary outcome where there are 10 or more studies of the same participant populations, intervention types, and for which outcome measures are available. To do this, we will use a funnel plot and take care when interpreting any asymmetry, as publication bias is not always the root of this.
Confidence in cumulative estimate: Where possible, we will bring studies together that have comparable participant populations, intervention types and outcome measures. Pooling these studies will enable us to apply the GRADE approach26 to give an overall assessment of the certainty of the evidence presented to us. Certainty will be considered as:
- high: further research is very unlikely to change our confidence in the estimate of an effect, and is unlikely to change the estimate
- moderate: further research may have an important impact on our confidence in the estimate of an effect, and may change the estimate
- low: further research is likely to have an important impact on our confidence in the estimate of an effect, and is likely to change the estimate
- very low: further research is very likely to have an important impact on our confidence in the estimate of an effect, and is very likely to change the estimate.
Two reviewers will independently apply GRADE to studies to determine the certainty of the evidence within each comparison.
Conclusion
This systematic review will quantify the effects of randomised evaluations of strategies used to increase the representation of rural participants in clinical trials. The results of this review have the potential to influence the design and conduct of future clinical trials, working to highlight the unmet health needs of rural communities. Specifically, our findings will inform trialists of evidence-based recruitment strategies that can be used to increase rural representation and reduce disparities between rural and urban populations.
This work is part of the Trial Forge initiative to improve trial efficiency27.
References
You might also be interested in:
2015 - Determinants of an urban origin student choosing rural practice: a scoping review